Editor's note: This text-based course is a transcript of the webinar, Aging And Vision: The Occupational Therapy Role, presented by Subah Gupta, MHS, OTR/L, SCLV, CBIS.
Learning Outcomes
- After this course, participants will be able to:
- List the common conditions where visual deficits are encountered.
- Identify screening for visual deficits in geriatrics.
- List appropriate intervention strategies for older individuals with visual deficits towards independence in ADLs and IADLs.
Introduction
Welcome, everyone. I am glad to be here. Today, we will talk about aging and vision and the role of occupational therapy.
Is Vision Only 20/20?
Anatomy of the Eye
Is vision only 20/20? We all know that the answer to that is no. The visual system is comprised of the interior structures of the eye, as well as posterior structures (Figure 1).
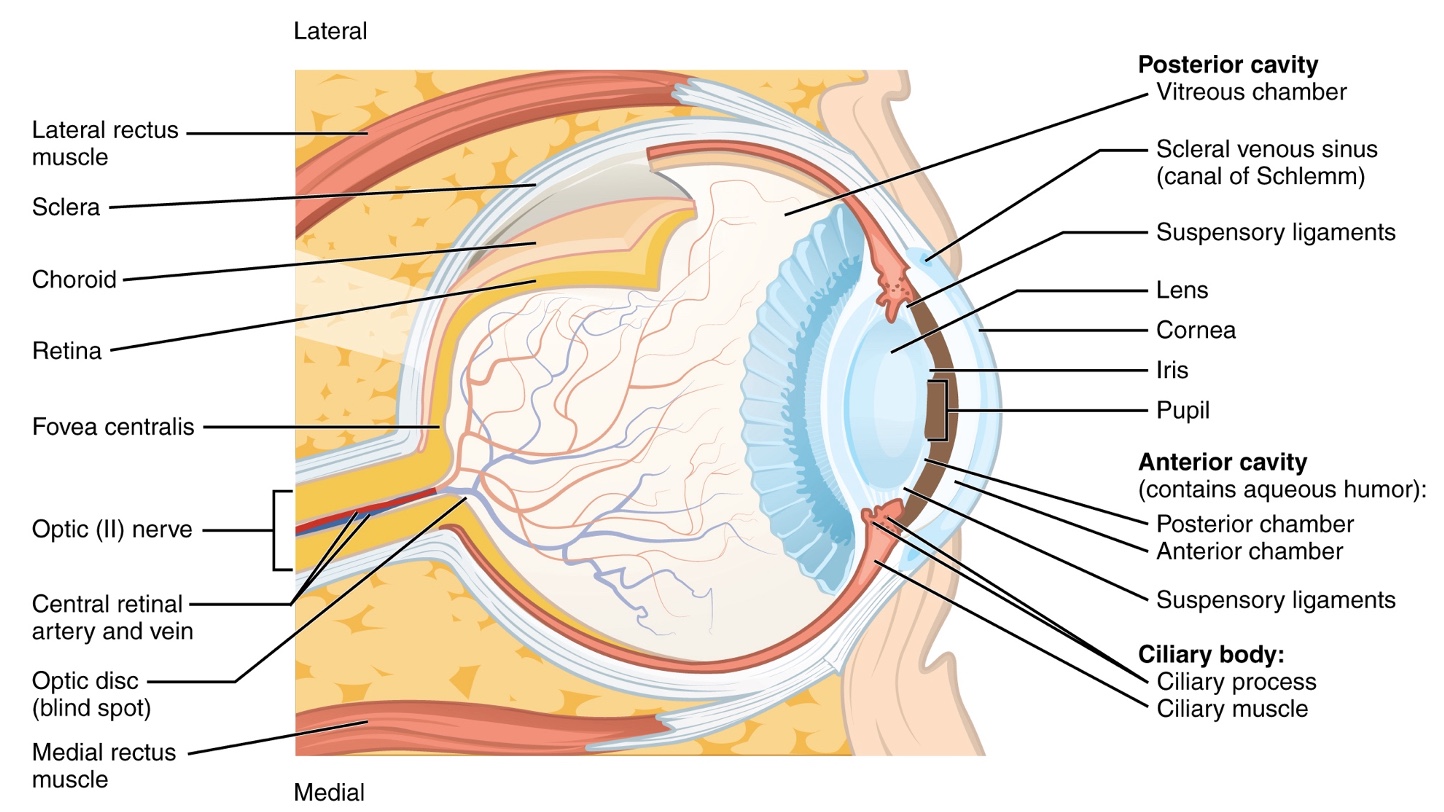
Figure 1. Anatomy of the eye. Click here to enlarge the image.
The anterior structures of the eye are the bony orbit, eyeball, and optic nerve. The posterior structures involve the geniculocalcarine tract, the lateral geniculate nucleus, and the visual cortex.
The interior structures capture the image of whatever we view and transmit it to the brain. It is common to hear that the brain sees, not the eyes. Once the image reaches the visual cortex, it is integrated with information, such as language, memory, emotion, and information received from other senses. This information creates a plethora of visual images that the frontal and prefrontal cortex accesses, leading to motor output and cognition.
For today's talk on vision and aging, we will limit our conversation to the interior structures of the eye. When light rays enter the eye, they hit the cornea, aqueous humor, lens, and vitreous humor. Then these light rays are going to converge on an area that is called the fovea. The fovea is part of the macula, part of the retina, and the inner coating of the eye. What is essential about the macula and the fovea is that they have the highest concentration of photoreceptor cells responsible for giving us detailed vision and appreciation of the size, form, color, and boundaries of what we see. It helps recognize that particular image when processed in the brain.
WHO Levels of Visual Impairment
- Low vision – A condition that cannot be corrected by medical or surgical intervention or by glasses: it allows some usable vision but is severe enough to interfere in completing daily activities (NEI)
- Legally blind – visual acuity is 20/200 in the best-corrected eye or a visual field of 20 degrees or less in the better eye (NEI)
In the visual world, there are two terms that we often hear, low vision and legal blindness. Low vision is a condition that cannot be corrected by medical or surgical intervention or by wearing glasses. There is some usable vision, but the deficit is strong enough to interfere with daily living activities.
Legal blindness, on the other hand, is a term that signifies visual acuity of 20 by 200 in the best-corrected eye or a visual field of 20 degrees or less. There are two different terms used in two different settings because low vision is a term that we use for billing to Part B.
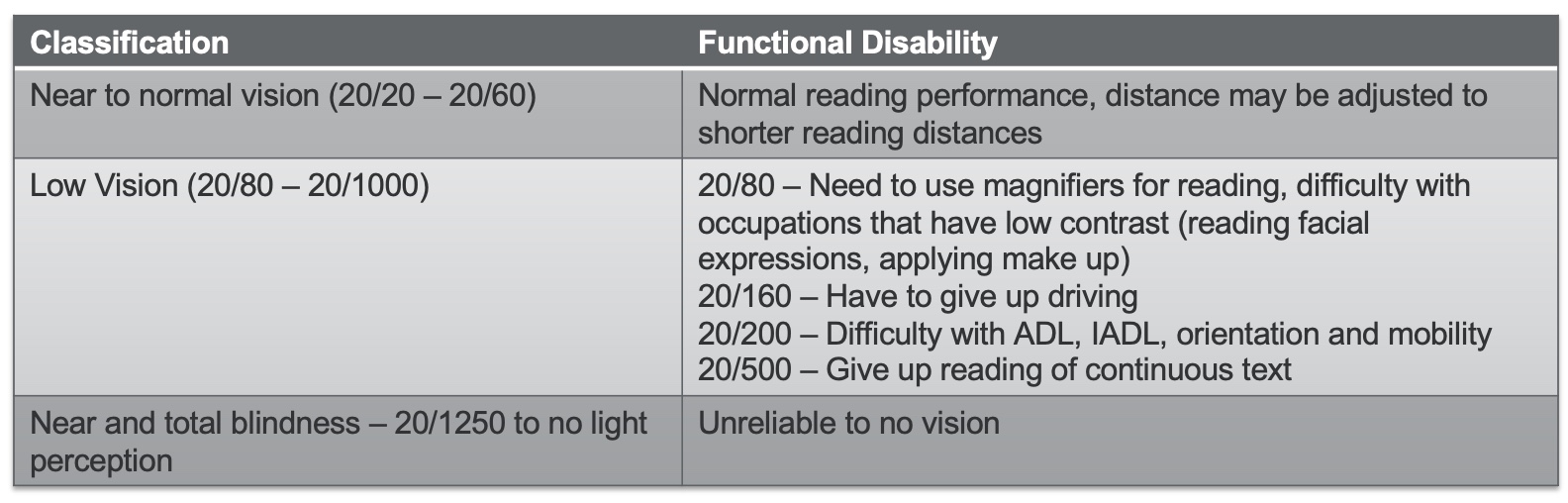
Figure 2. Vision classification and functional disability chart. Click here to enlarge the image.
It has a classification of 20/80 to 20/1000, which is the visual acuity range, meaning if an individual has a visual acuity of 20/80, they may need magnifiers for reading. If it is 20/160, they may have to give up driving. If it is 20 by 200, there may be difficulty with ADLs and IADLs. If it is 20 by 500, the individual may have to give up reading continuous text.
Legal blindness, on the other hand, is a term coined by the government which allows the individual to receive or be eligible for government services and benefits.
Aging Leads To:
- Cognitive Decline
- Motor Decline
- Sensory Decline
- Psychological Decline
Normal Aging and Vision as per SKI Study
- Presbyopia
- Floaters – Strands of protein in vitreous
- Dry Eye – Poor quality of tears or insufficient tears produced by the lacrimal glands
- Increased need for light – An 80-year-old will need 10 times more light as compared to an average 23-year-old
- Increased susceptibility to glare
- Reduced dark/light adaptation
- Reduced contrast sensitivity – A 75-year-old needs 2 times more contrast, and a 90-year-old will need 6 times more contrast
A study by the Smith-Kettlewell Institute, called the SKI Study, focused on vision function for performance in ADLs and IADLs. There were a few conditions that they identified.
Presbyopia. It is an age-related accommodative decline in accommodative amplitude. It means when we, as individuals, hit the age of 40 and above, and I am right there, we will need glasses to read.
Floaters. These are stands of protein in the vitreous. These may look like cobwebs or worms when looking at the sky. It reflects those proteins onto the retina because the vitreous is not as dense. The vitreous gets more fluid-like as one gets older.
Dry eye. Dry eye is not a serious medical condition but can be very debilitating. There is poor quality or insufficient tears produced by the lacrimal glands. If the client tells me they have dry eyes or if I read this diagnosis in the medical chart, I immediately jump to the 20/20/20 rule. For every 20 minutes of sustained near vision tasks like looking at a screen (which has been our life during the pandemic), the individual needs to look 20 feet away for 20 seconds and blink. Blinking stimulates the lacrimal glands to secrete tears.
Increased need for light. There is a high need for light as we age. And that is because the pupil diameter gets smaller and smaller as we age—an 80-year-old needs 10 times more light compared to an average 23-year-old. There is increased susceptibility to glare because the cornea and the lens are losing their smoothness.
Reduced dark/light adaptation. There is diminished dark light adaptation because the neural impulse is generated when light strikes the photochemicals in the photoreceptors, which must be reinstituted. When there is a delay, we have reduced dark and light adaptation. Again, if you walk into a dark theater, it takes you a few minutes to get accommodated, and vice versa when going into the light. This adjustment gets longer over time with reduced dark/light adaptation.
Reduced contrast sensitivity function. A 75-year-old needs two times more contrast, and a 90-year-old needs six times more contrast.
Limited Vision Occurs Because Of:
- Injury/trauma
- Diseases
- Aging
- Any/all of the above
Limited vision occurs because of injury, disease, aging, or all of the above. When I worked in a hospital outpatient setting, most of my low vision clients were all of the above. For example, it could be a 70-year-old post-stroke. A stroke is an injury that could also have comorbidities like macular degeneration or glaucoma. Now that I am in private practice, I see more of the disease and the aging combination. So it depends upon what setting you treat.
Commonly Seen Conditions in the Older Adult
In the interest of time, I will not discuss the pathophysiology or the pathogenesis of vision issues as that information is on your slides. Instead, I want to examine the symptoms, treatment, and our role.
Cataracts
- Causes
- Lens opacity that interferes with light transmission
- Opacification begins in the periphery and gradually moves towards the center; old fibers in the nucleus of the lens become compressed and dehydrated
- Treatment
- Criteria for removal of a cataract is when reduction in visual acuity is 20/50 or less
- Intra-ocular lens procedure (IOL) is completed, where the lens is replaced with a plastic implant
- Covered by Medicare and the procedure has great outcomes
Cataracts are a condition that affects the lens of the eye. In the United States, an individual or a patient is eligible for cataract surgery as soon as their vision is 20/50 or less. Cataract surgery has excellent outcomes, and OT is typically not involved. If I encounter someone, I may give them some strategies when looking at light if the individual has not come to that conclusion.
- Symptoms
- Greater effect on central vision
- Blurred vision
- Visual distortion
- Reduced Contrast Sensitivity Function (CSF)
- Decreased color discrimination
- Glare sensitivity
- Functional Limitations
- Difficulty driving
- Difficulty reading
- Difficulty watching TV
The symptoms of cataracts have a more significant effect on central vision. There is blurred vision, visual distortion, reduced contrast sensitivity function, reduced color discrimination, and glare sensitivity. Cataracts can lead to difficulties with driving, reading, and watching TV. Typically, I adjust their lighting at a working distance or give them a few other strategies concerning mobility. Figure 3 is what a grocery store would look like if you are viewing it through an eye with cataracts.

Figure 3. An image of a grocery store aisle with a cataract.
The visual image is blurred, not detailed, and with reduced contrast.
Age-related Macular Degeneration (ARMD)
Age-related Macular Degeneration is a condition that affects the photoreceptor cells in the macula.
- Dry AMD
- Higher incidence (90%)
- Pathogenesis is balding of the retina where there is a gradual destruction of cone and rod cells (atrophy)
- Drusen (fatty protein) found on the retina where atrophy is occurring
- Often unilateral, slowly progresses to the other eye
- May convert to the wet form in later stages
- Cause – Unknown
- Vitamins may help slow down the progression
- Neo Vascular (Wet) AMD
- Lower incidence (10%)
- Pathogenesis is hemorrhaging (cells in RPE breakdown, vascular endothelial growth factor (VEGF) stimulates new blood vessels which are fragile and leak, causing hemorrhaging)
- Usually bilateral and aggressive
- Often there is rapid vision loss
- Cause – Genetic
- Anti-VEGF injections may help
Macular degeneration occurs in the area of the retina that houses the fovea, which has the highest number of auto receptor cells. The fovea, opposite the pupil, is where light rays converge, and the image of what you see is transmitted to the brain. There are two types of macular degeneration, dry and wet, and the pathophysiology of each is on your slide.
- Symptoms
- Scotoma (blind spot) in the central visual field
- Difficulty to see detail
- Difficulty with color discrimination
- Difficulty discriminating contrast
- Functional Limitations
- Never results in blindness
- Reading span is affected
- Without is read as with
- Unable is read as able
- If the scotoma is less than 5 degrees, the brain will fill in the picture – perceptual completion
- If the scotoma is more than 5 degrees, the client will not see a black hole, but a misaligned, blurred, distorted picture or has the inability to focus
The symptoms of wet and dry macular degeneration are the same. The hallmark of macular degeneration is a blind spot in the central field, also called a scotoma. Clients have difficulty seeing detail, contrast, and color discrimination. If the scotoma is small, less than five degrees, the brain fills in that information called perceptual completion. As the disease progresses, the scotoma gets bigger and bigger, and that is when you start to see a blind spot. A word of caution is a blind spot. It is not necessarily a big black blind spot, but rather, they see a distorted image that is blurred and misaligned.
With macular degeneration, I work the most on reading. It is not uncommon to come across a reading span being affected, seeing the word "without" and only reading "out." This condition never results in blindness. Figure 4 is a picture of a healthy eye. You can see the macula and the optic nerve in Figure 4.

Figure 4. Image of a healthy eye.
Figure 5 shows macular degeneration of the eye with drusen (yellow and white spots of lipid-protein). With the drusen, there is a distortion right in the center.
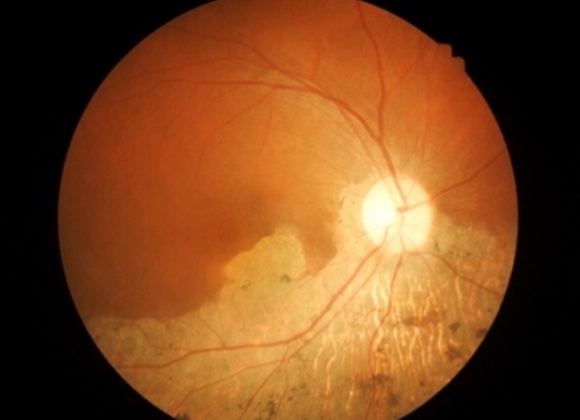
Figure 5. Image of an eye with macular degeneration.
Figure 6 shows how this might look.

Figure 6. Images showing a distortion from macular degeneration.
Glaucoma
- Causes
- An increase in intraocular pressure occurs due to build up of aqueous in the anterior chamber, the only outlet is the optic disc leading to increased pressure along the nerve and loss of blood flow
- Causes the nerve fibers to die
- Could be because of scar tissue, surgery, microscopic changes in the trabecular meshwork, and anatomical aberration (narrow-angle between cornea and iris)
- Treatment
- Eye Drops
- An increase in intra-ocular pressure occurs due to build up of aqueous in the anterior chamber, the only outlet is the optic disc leading to increased pressure along the nerve and loss of blood flow
- Causes the nerve fibers to die
- Could be because of scar tissue, surgery, microscopic changes in the trabecular meshwork, and anatomical aberration (narrow-angle between cornea and iris)
- Surgical procedures
- Eye Drops
The next condition is glaucoma which is a disease of the optic nerve. Some researchers classify this as a brain disease because the optic nerve connects the eye to the brain. As soon as I see the glaucoma diagnosis, I have the patient show me how they are administering their eye drops. I use an empty vial of Xalatan, a glaucoma drug, in my mobile kit. If it is not time for the patient to administer their eyedrops, I have them simulate that. I am looking for them to lower their eyelid, tilt their head back, and put in the eye drop. Once these steps are completed, does the individual close their eye or gently press? If so, that will prevent Xalatan, or whatever medication, from being drained into the tear ducts, and it will allow for the med to stay in the eye to do its work. Many clients have more than one prescribed eye drop. If that is the case, you must wait five minutes between the two medicines because you do not want the second medicine to wash off the first and render it useless. I complete this education with all of my glaucoma patients.
- Symptoms
- Visual loss starts in the periphery (hence easy to miss)
- With progression, scotoma develops in the macula
- Can lead to blindness
- Functional Limitations
- Affects mobility, a high risk of falls, collisions, and disorientation
- These individuals are afraid to leave home
- Affects driving
- Isolation and depression
Visual loss starts in the periphery, and it is easy to miss. It is a hidden or silent condition. As it progresses, there are blind spots that develop in the central visual field, and they are usually eye-shaped. As such, this is a condition that can lead to total blindness. Visual loss starts in the periphery, so functional mobility is affected. These are individuals who are afraid to leave home. Remember, when an individual is inside the home, they are in a static environment where furniture and items are all stationary. They may have a spouse or a pet moving, but the home is usually a static, familiar environment.
In contrast, the grocery store is an unfamiliar dynamic environment where they must navigate many obstacles (carts, people) to be safe or not embarrass themselves. These individuals prefer to stay at home, leading to isolation and depression. Glaucoma also affects driving. Figure 7 shows a picture of a healthy eye and one with glaucoma.
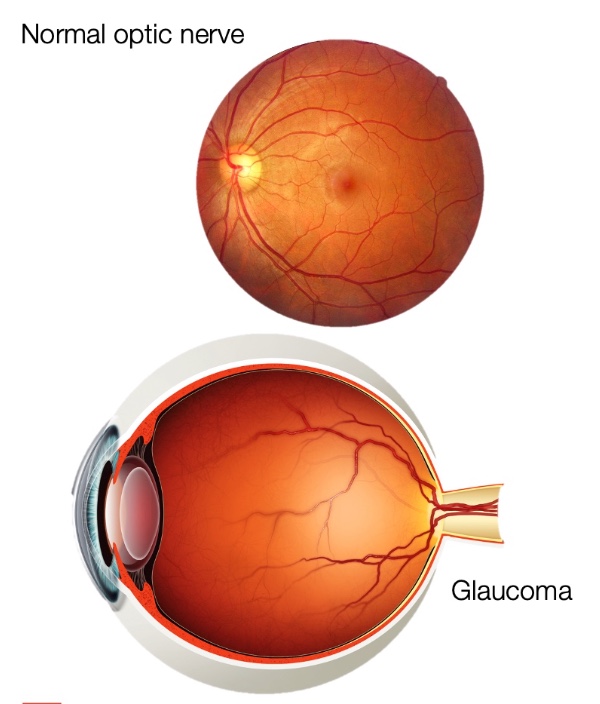
Figure 7. Comparison of a healthy eye and one with glaucoma.
Figure 8 shows what this may look like, including the restricted visual fields in the periphery.

Figure 8. Example of glaucoma.
Diabetic Retinopathy
- Causes
- High levels of blood sugar destroy the small blood vessels; they leak fluids and lipid on the retina
- Macular edema with drusen and dot and blot hemorrhage leads to …
- Oxygen deprivation….. leads to neovascularization; these vessels break and bleed too
- Contraction of the vitreous leading to possible retinal detachment and blindness
- Treatment
- Controlling blood sugar and blood pressure
- Anti-VEGF injections
- Laser treatment
- Corticosteroids
- Vitrectomy
- OT role – self-management
Diabetic retinopathy is a disease of the small blood vessels, with the hallmark symptom being fluctuating vision. While working in outpatient, I had a patient come to PT and OT for vertebroplasty. I saw a history of diabetes and diabetic retinopathy during the medical intake as comorbidities, but I did not think much of it. I was focused on getting the patient independent in ADLs with adaptive equipment and looking at their biomechanics. During the evaluation, the patient told me they could only see the big E on the Snellen Chart. As vision was an interest of mine, I realized he was at 20/2200, but I continued to focus on their orthopedic issues. He came back 48 hours later, and all he had was light perception and no other vision. Immediately, I changed tracks and started addressing vision over 45 minutes of the session and 15 minutes addressing his ortho issues. I needed to ensure that he was independent in managing his diabetes to prevent other complications.
- Symptoms
- Fluctuating vision
- Glare sensitivity
- Reduced contrast sensitivity
- Visual field deficits
- Functional Limitations
- Depends on the visual field deficit; if it is central – difficulty with reading and object identification; if it is peripheral – difficulty with mobility
- Can cause total blindness
The hallmark of diabetic retinopathy is fluctuating vision, glare sensitivity, reduced contrast sensitivity, and visual field deficits, depending on where the blood vessels have been affected. They may have issues with seeing in their periphery, central visual field, or both, and it is a condition that can lead to total blindness. Figure 9 shows some examples of the damage and how it would look to a person affected.
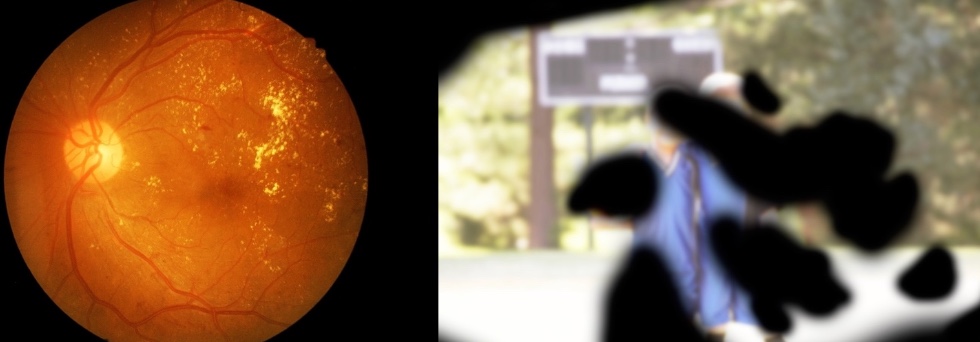
Figure 9. Examples of diabetic neuropathy.
Charles Bonnet Syndrome
- Hallmark is visual hallucinations.
- There is no noise.
- Client knows what they are seeing is not there.
- No agreement on the cause (still being researched)
- One theory is – CBS is like a phantom limb sensation
- Usually, clients see cats, flowers, dogs, bagpipers, etc.
Another condition I see often is Charles Bonnet Syndrome, where there are visual hallucinations. The client knows that what they are seeing is not there. There is no agreement on the cause, but what is suspected is that for 65 to 70 years, the client has had intact or some vision with visual sensory feedback going to the visual cortex. Now, whether it is glaucoma, diabetic retinopathy, or macular degeneration, there is a significant visual loss, and the brain is seeking that visual input. Hence, the brain comes up with visual hallucinations (like cats, flowers, et cetera) to fill that gap. It is akin to the phantom limb sensation. Over the years, I have learned to ask the client if they see anything like this, and I preempt it by saying, "It is common to see things that are not there. Do you see things that are not there?" More often than not, the patient gives a sigh of relief and relaxes, saying, "Yes, I do, but I never told anybody because I did not want to be labeled crazy." So addressing vision and helping with the psychosocial element is huge.
Other Conditions
- Retinitis Pigmentosa
- Optic Neuritis
- Ocular Albinism
- Retinal Detachment
- Achromatopsia
Other common conditions include retinitis pigmentosa, optic neuritis, and ocular albinism. Ocular albinism is a condition lacking melanin, so the iris is flooded with light. There can be glare sensitivity and visual acuity issues. One good thing about ocular albinism is it is a stable condition, and they are great candidates for bioptic driving. We are not going to dive deep into bioptic driving because it is not for an entry-level webinar. The State of Pennsylvania passed bioptic driving passed last year. All of us in the low vision world are excited about it. Retinal detachment is an emergency because the retina separates from the pigment epithelium, and there is no blood supply, so there can be cell loss. It happens in diabetic retinopathy and if a client has severe myopia.
Low Vision Services Are Being Provided By:
- Ophthalmologists
- Optometrists
- Occupational Therapists
- Teacher of the Visually Impaired
- Certified Low Vision Therapists
- Certified Orientation and Mobility Specialists
An ophthalmologist and an optometrist provide low vision services, where we often get referrals. In an ideal world, they will complete a low vision exam; however, it can also be provided by OTs, teachers of the visually impaired, certified low vision therapists, and certified orientation and mobility specialists.
Service Delivery
- Need a prescription from the referring MD or OD
- Can be provided in any setting covered by Medicare and/or private insurances
- Conditions of coverage are outlined in May 2002 program memorandum
- Any OT can provide low vision services
- There are 2 certifications available
- SCLV (By AOTA) – Used to be a portfolio-based competency, available since 2006
- CLVT (By ACVREP) – Certified Low Vision Therapist
Low vision services can be provided if you have a script from a physician. You may not get the detailed evaluation, but we can proceed. Medicare and private insurance cover these services. If anybody is interested, conditions of coverage are outlined in the May 2002 program memorandum, or feel free to reach out to me, as I am happy to share these with you.
Any OT can provide low vision services. When I gave you the example of the client who had vertebroplasty, I did not have my SCLV certification, but I was still providing low vision services. Regarding certification, there are two: the SCLV, which AOTA offers, and the CLVT. The SCLV certification is only for OTs, while the CLVT certification is for OTs and related vision providers.
When billing Medicare part B for low vision services, we use primary visual impairment as the primary diagnosis code, which means the ICD-10 code for 20 by 80, 20 by 100, 20 by 200, or whatever their visual acuity is. The secondary diagnosis code could be diabetic retinopathy, glaucoma, or the condition causing visual impairment.
Frequency and Duration
- Frequency: 1-3 times per week
- Length of session: 30-60 minutes
- Duration:10-12 sessions or less
- Sessions can be spaced out because homework is provided in between sessions.
Frequency and duration are typically one to three times a week, with sessions lasting anywhere between 30 to 60 minutes. The duration is 10 to 12 sessions, but those 10 to 12 sessions do not usually end within six weeks. This is because as therapy is administered, a lot of homework goes on, so the length of low vision therapy services can extend up to three to four months.
Our Role
- Is to determine what usable vision remains and teach a client to use this vision effectively as opposed to sensory substitution (blind) approach
- OT Practice Framework states, "Occupational therapy services are provided for habilitation, rehabilitation, and promotion of health and wellness for clients."
Our role as OTs is to determine what usable vision remains and to teach the client to use this vision effectively, compared to the sensory substitution approach, which is the approach you use when an individual is blind.
Low Vision OT Assessment
- Ideally, all clients should have a low vision examination by an ophthalmologist or an optometrist before OT evaluation.
- Include a depression screen
- Be mindful of cognitive deficits
- Always be knowledgeable about other health conditions
- Low vision interventions should not exacerbate chronic health conditions
- Like any other OT evaluation document medical history, onset date, medications, assistive equipment patient has, and family support
All clients should have a low vision examination by an ophthalmologist or an optometrist before an OT evaluation, but that does not always happen. When I was in a hospital outpatient setting, therapists were the ones identifying visual deficits and referring them to low vision specialists. I worked closely with an optometrist back then who would do the eval, and we would share our findings. Now that I am in private practice, I have an optometrist do a low vision eval first. It depends on what setting you are working in, but having the low vision exam before OT is preferable.
It should also include a depression screen. The Geriatric Depression Screen is a free download and public domain. Please include this to assess if there is a psychosocial impairment. We also want to be mindful of cognitive deficits. I cannot stress this point enough. Visual deficits can get masked as cognitive deficits. If an individual cannot see well, they are probably not going to attend to or engage or participate in tasks, which can be interpreted as a cognitive deficit, especially for individuals who are 70 and above. I like to use the Mini-Mental State Exam (MMSE), Montreal Cognitive Assessment (MoCA), Addenbrooke's Cognitive Examination- III (ACE), Executive Skills Questionnaire (ESQ), or whatever tool you have to measure cognition. If I do not have one of these in my mobile kit, I use paragraphs of text. I have the client read and then answer questions. Then, I will speak another set of texts and have the client answer questions. If they do better answering questions by listening than by answering questions by reading, then I know it is probably not a cognitive deficit but a visual deficit.
It is also essential to be knowledgeable about other health conditions. This scenario happened to me a few days ago. I am seeing a client who has diabetic retinopathy, glaucoma, and macular degeneration. For this client, her workstation was a desk built into the wall. She worked at the computer four to six hours a day while running her own business and had a scanner to her right. She needed access to the scanner at least six to eight a day. I gave this client a floor lamp and placed it behind her right shoulder because she was right-eye dominant. I adjusted the height, ensured she could see her screen and left. Two days later, when I returned for our next session, she complained of severe backache. I discovered she had to duck below the floor-length lamp to access her scanner. I had to remind myself that vision is only a tool in our toolbox. We have to look at the patient holistically and be knowledgeable about what other health conditions they have to intervene accordingly. It should not exacerbate chronic health conditions.
As with any other OT evaluation, document the patient's medical history, onset date, medications, assistive equipment, and family support. It is not uncommon for me to find a drawer with tons of magnifiers and other equipment the client has used over the years. So it is important to document what assistive optical equipment the client has.
Clinical Observations
- Difficulty recognizing faces
- Unusual head movements
- Leaning forward or away when trying to read
- Frequent falls or bumping into furniture
- Decreased attention
- Social isolation
- Lack of eye contact
Individuals may have difficulty recognizing faces due to low contrast. For example, a nose may look the same as a cheek or a forehead. It is also difficult to read emotions on a person's face with low contrast sensitivity. There may also be unusual head movements because an individual is trying to move that blind spot away to view the image. They may look forward or away when trying to read when adjusting the focal distance. They may fall frequently or bump into furniture because of impaired peripheral vision.
We talked about decreased attention. If someone cannot see well, they will not attend. They may be socially isolated as they prefer static environments. There can be a lack of eye contact. This is unlike those with autism, who have limited eye contact due to difficulty understanding social cues. In this instance, the lack of eye contact is because the client is trying to see either above, below, left, or to the right to gain a clear image. They look at you from a pseudofovea, which we will briefly discuss here.
Spectacle Prescription
- OD – Right Eye
- OS – Left Eye
- OU – Both Eyes
- -1.75 Myopia corrected by concave lens
- -2.00 Astigmatism correction needed
- 20 Orientation of the toric lens
- +2.50 Reading add
If they have a spectacle prescription, I have them give a copy because it gives me a lot of information. "OD" means the right eye, "OS" means the left eye, and "OU" means both eyes together. For example, the first number above is -1.75, which tells me the client is myopic or nearsighted. The glasses that they are wearing are going to help them see far. The number -2.00 tells me they have astigmatism, and the cornea or the lens is not round. Instead, it may be shaped like a football. The number 20 is the orientation of the lens to correct astigmatism. Lastly, the reading add number (+2.50) means the client may need bifocals. They will be viewing near items from the lower part of their glasses, and they will be viewing far from the top part of their glasses.
In the earlier example, the vertebroplasty patient would have had "LPO," light perception only, HMO, "hand movements only," or "CF," count fingers.
Test Eye Dominance
- Have the client find a target at a distance; give them the paper towel roll and ask them to view that distant target through the paper towel roll
- Have them look at a near target through a hole in the card
- Whichever eye they take the paper towel roll or the card to is the dominant eye
We should always test eye dominance. The dominant eye usually leads the scanning and the fixation, the two things that happen when reading. Knowing the dominant eye helps us put lighting in the right place. Remember, I put the lamp towards the right eye because the right eye was dominant, but she had a backache because it impacted her functionally.
Another reason to know eye dominance is an individual will use the magnifier with their dominant eye, and the prescription should match this.
To test eye dominance, have a client use a paper towel roll to focus on an item in the distance. Have them look at a near target through a hole in a card for near vision. Whatever eye they use for the paper towel roll or card is the dominant eye. Document and record it.
Visual Acuity
- Clarity or sharpness of vision
- Measured as a Snellen fraction – Distance over Letter Size
Visual acuity is described as the clarity or sharpness of vision and measured as Snell fractions. For 20 by 20, the upper 20 refers to the distance, and the lower 20 refers to the letter size. OptiType is a fancy word for the size of the numbers, letters, or symbols on an eye chart. What an individual should see at 20 feet is clear at 20 feet (20/20 vision). Twenty by 100 means that what I should see clearly at 100 feet is not clear, and the person has to come to a distance of 20 feet for it to be clear.
- Distance/Intermediate Visual Acuity
We test visual acuity using a Snellen Chart (Figure 10), which most of us have seen.
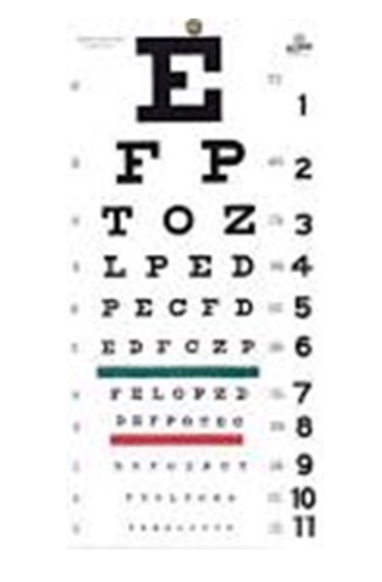
Figure 10. Snellen chart.
We have to use something different in the low vision world as the Snellen caps at 20 by 200. If you go back to the WHO classification, low vision can go from 220 to 1,000. Low Vision Lea Numbers Chart is an example of a test we can use, as shown in Figure 11.
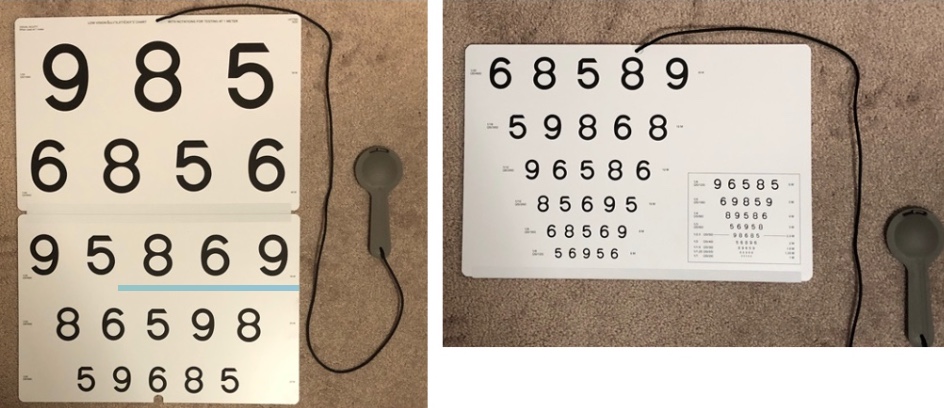
Figure 11. Low Vision Lea Numbers Chart.
There are many low vision assessments. The testing distance for the Low Vision Lea Numbers Chart is one meter. This outcome measure also gives you numbers between 20 by 100 and 20 by 200, which Snellen does not. Thus, it allows you to discover nuances in visual acuity.
- Things to keep in mind:
- Light source to be directed from behind the client
- Charts need to be held at the specified distance
- Chart needs to be evenly and adequately illuminated
- Test dominant eye first, nondominant eye second, then both eyes together
- Test with glasses on if prescribed
The light source should be behind the client, so the light is not shining into their eye. The charts must always be held at a specific distance and adequately illuminated. When testing distant visual acuity, you test the dominant eye first, the nondominant eye second, and then you test them both together. As OTs look at function, we should also test a client with their prescription glasses if applicable.
Accommodation
- The ability of the eye to view objects at near distances without visual blur. It requires:
- Lens to thicken
- Pupils to constrict
- Eyes to converge
For accommodation, the lens needs to thicken, pupils need to constrict, and eyes need to converge. We start to lose this ability after the age of 40, and that is why people often need reading glasses.
Near Acuity Charts
A near acuity chart is Rosenbaum, a pocket screener, shown in Figure 12.
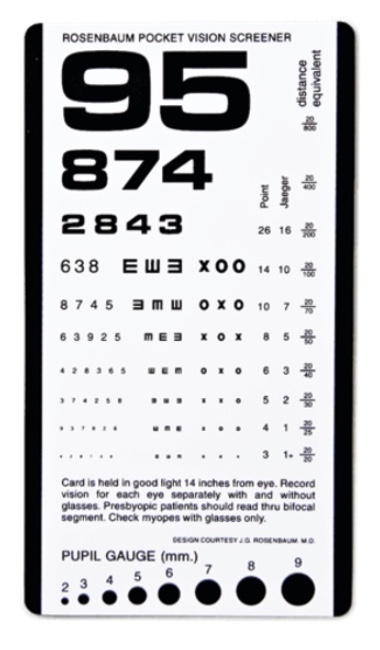
Figure 12. Rosenbaum Vision Screener.
Many annual eye exams include this screener. Again, in the low vision world, we must step it up using something like a Warren Text Card (Figure 13).
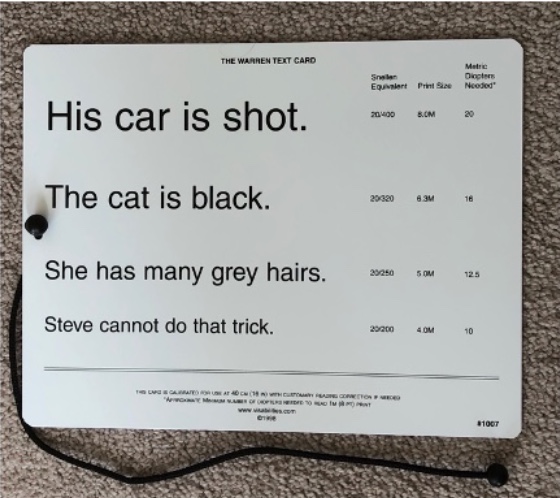
Figure 13. Warren Text Card.
The Warren Text Card is used at 16 inches, and the sentences are at fifth-grade reading level. This card is available in English and Spanish. When looking at reading, we want a measure that tests near vision and reading because we rarely functionally read letters in isolation. The reading chart has to be in their primary language.
- Select a reading chart in their primary language
- Select a chart at an appropriate reading grade level
- Test is completed using both eyes
- Client wears glasses if prescribed
We also want to select a chart at an appropriate reading grade level. One of the intake questions in my eval is, "Did you graduate high school?" If so, I know they have a reading proficiency up to the seventh or eighth-grade level. We mostly read with both eyes, so this is completed with both eyes open. And if the client wears bifocals, hopefully, they are reading through them.
Allowances That Can Be Made
- Is it this or that?
- Allowed to match
- Can respond by saying: Yes or No
- Can display a single optotype
- Can read only 1 optotype per line until the client reaches a line where they struggle, asked to read all optotypes
- Clients with central scotoma, can turn their heads but cannot lean forward
Certain allowances can be made when testing an individual with the Warren Text Card. It is okay for us to say, "Is it six or a nine?" Going back to my neurological background, I often test low vision in 70-year-olds with receptive aphasia, expressive aphasia, and/or dysarthria. I would give them the numbers, and they would match them. They can respond by saying yes or no. It is also okay to display the first letter of the chart and hide the rest to reduce fatigue. Fatigue will set in at some point, and you want to delay that by having them only read the first letter until they get to a line where they start to struggle. Then, you want to ensure they can read at least 50% or more, usually three out of five words. Clients who have that central blind spot can turn their heads to find an area they can see but cannot lean forward.
Contrast Sensitivity Function
- Contrast sensitivity is a measure of how faded or washed out an image can be before it becomes indistinguishable from the uniform background
- Common tests available:
- Pelli-Robson Contrast Sensitivity Test
- Mars Contrast Sensitivity Test
- Low contrast ETDRS Test
Contrast sensitivity measures how faded or washed out an image can be before it is indistinguishable from its uniform background. These three tests above are available in the OT vault. Most OTs prefer the Lea Number Low Contrast Chart because it has a functional interpretation. This can be seen in Figure 14.
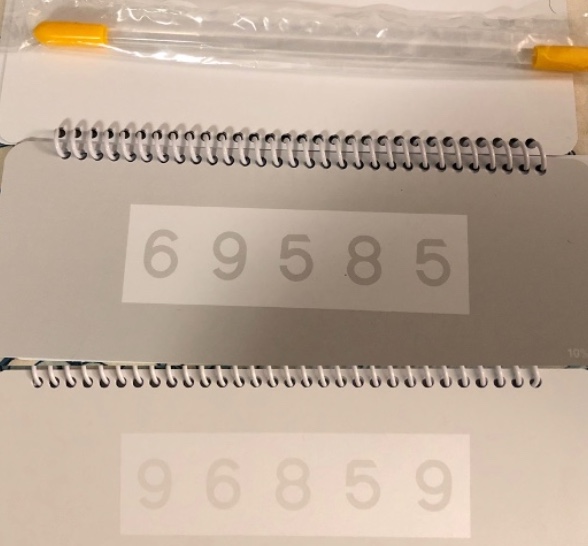
Figure 14. Lea Number Low Contrast Chart.
- Functional Interpretation of Lea Contrast Number Chart
- Does not see any numbers – CSF is extremely limited, and enhancement of contrast is needed for the client to function. The client may require assistance to ambulate safely in environments. Ability to resume driving is highly questionable and should be carefully evaluated.
- Client sees numbers only at 25% level – Client may require assistance to ambulate safely in environments. Driving performance should be carefully evaluated, especially with regard to night driving and driving in cloudy conditions.
- Client sees numbers up to 10% level - Client likely will have difficulty detecting subtle changes in the support surface, reading materials printed in low contrast formats, seeing black and white photographs, facial features, water, and other low contrast materials. Magnification and increased illumination may assist the client to recognize low contrast features. Driving performance should be carefully evaluated, especially with regard to night driving and driving in cloudy conditions.
- Client sees numbers at 5 and 2.5% level - Client likely will have difficulty seeing facial expressions and recognizing friends across the street. They may have difficulty detecting curbs and other low-contrast drop-offs. Increased illumination may assist the client to recognize low contrast features, and modifying environment to increase contrast is recommended.
We, as OTs, live and breathe function, so any chart that gives a functional interpretation is typically what we use. In the Lea Number Low Contrast Chart, there are numbers. They are 10M OptiTypes and listed in different intensities: 25%, 10%, 5%, 2.5%, and 1.2%. What you see in Figure 14 is 10 and 5%. And then this is the five. You can see the difference in the intensity of the numbers. The chart is placed at a reading distance of 40 centimeters or 16 inches, and you have the client read the first OptiType. The chart should also not reflect light.
Let's take an example. The client can read all the numbers at 25% and 10%, but the client cannot read the numbers at 5%. The functional interpretation is that they will have difficulty detecting subtle changes in support services, so mobility outdoors may be affected. They may have trouble reading materials printed in low-contrast formats like newspapers or have difficulty with facial features. They may also have difficulty identifying water on the floor, a fall risk. They may have difficulty driving at night or in cloudy conditions. Magnification and increased illumination will help this client to recognize low-contrast features. As illustrated, the chart sets you onto the treatment path based on the results.
Color
- Client matches the color cards at any distance
- Informal screen
- Score it as percentage accurate
Figure 15 shows the color cards that I got from Home Depot.

Figure 15. Color paint cards from Home Depot.
This is an informal screen of matching colors. You can score it as a percentage of accurate responses.
Visual Fields
Visual fields are an area that is seen without moving the eyes, as shown in Figure 16.
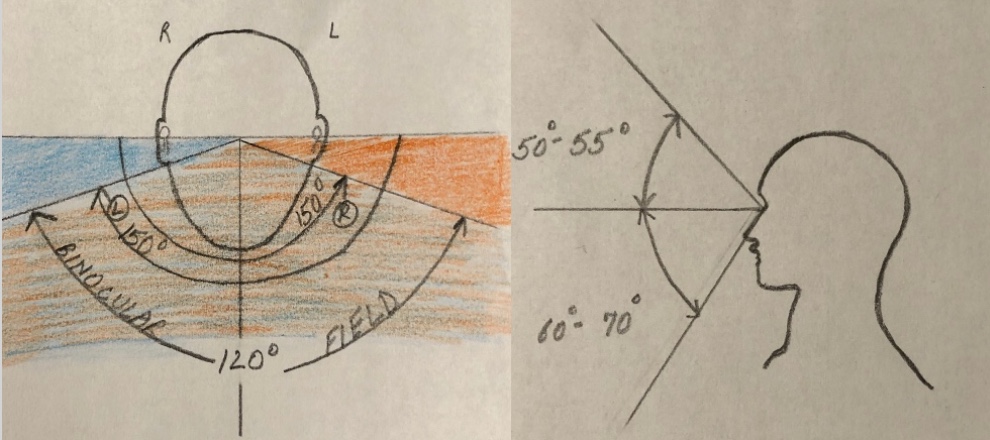
Figure 16. Visual field testing.
Horizontally, each eye will have a visual field up to 150 degrees. In the middle is the binocular field. The visual field extends superiorly 50 to 55 degrees and inferiorly 60 to 70 degrees.
Confrontation Testing
- Patch one eye
- Have the patient fixate on a central target
- Approach the patient from front, "Tell me when you see my finger and how many are there?"
- Move it right to midline, left to midline, top to midline, and bottom to midline.
- Record approximately where the patient reported seeing the stimuli, can compare with your own
I assume you have heard about this, done it, or at least seen it done. The client's one eye is occluded, and the patient fixates on the therapist's nose. You have them identify how many fingers you hold up to the right, left, top, and bottom of the midline. This is not one of my favorites because it is so easy to cheat on this test. It is an informal screen that is commonly used.
Two Person Kinetic Test
We should also test peripheral visual fields using the Two Person Kinetic Test, as seen in Figure 17.

Figure 17. Two Person Kinetic Test.
I usually use a family member as the second examiner. The family member sits with a target like a pen, and the client fixates on the object. You go behind the client and move an object like a pen light and move it in an arc. The client tells you when they first spot it. The other eye is patched. Again, you will do the right to left, left to right, top to the midline, bottom to the midline, and then document your findings. Peripheral visual fields are a function of rods sensitive to motion and light, so using a pen light is a great target.
Scotoma Testing
How do we figure out if the client has a blind spot? It is not uncommon for me to walk into a client's home and find this taped onto the fridge or the wall. Figure 18 is an image of an Amsler Grid.
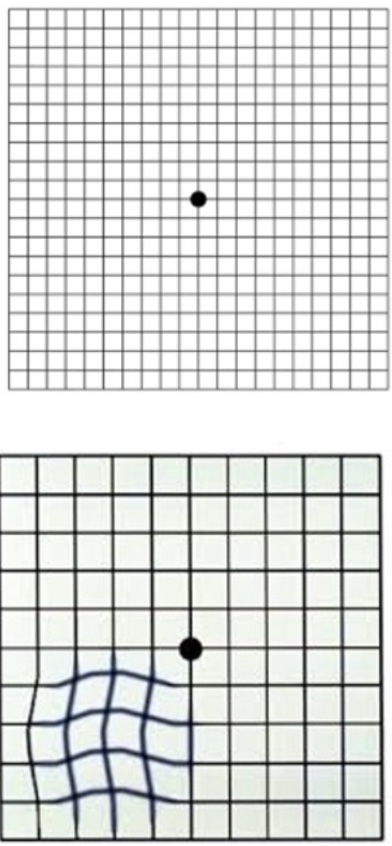
Figure 18. Amsler Grid.
If the client sees crooked lines, the disease is now symptomatic. As part of my assessment, I use the Face Field Method, as shown in Figure 19.
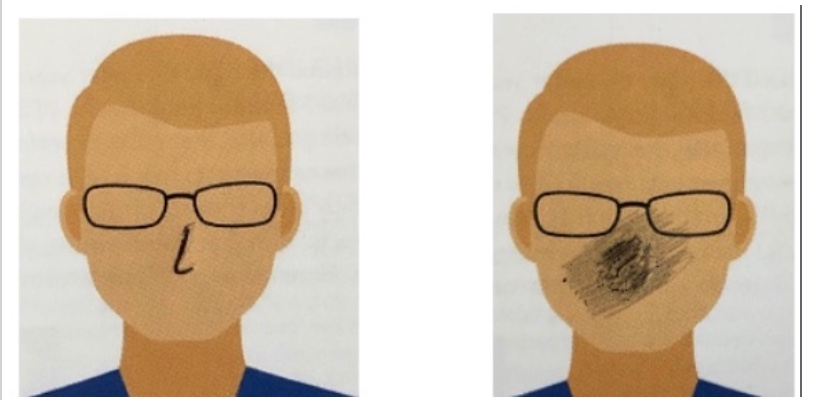
Figure 19. Face Field Method.
The client has a patch on one eye, and I have the client fixate their vision on my nose. I then ask them if any part of my face is missing, blurry, or distorted. If the client says, "Yeah, your left eye is distorted," that will be a distortion or blind spot in the visual field. Their blind spot is in the middle if my nose is distorted.
You can do another method called the Clock Method, which uses a paper target (Figure 20).
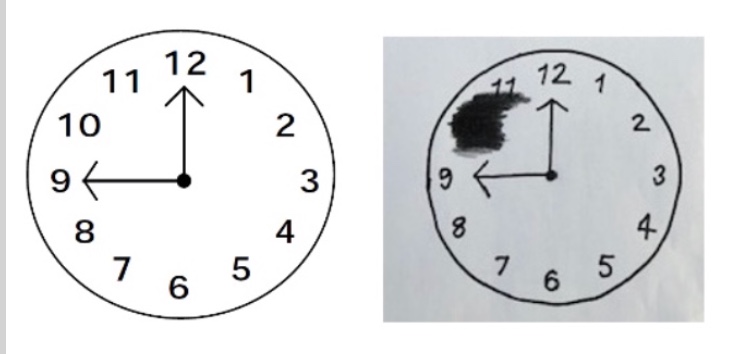
Figure 20. Clock method.
The client looks at the clock's center, and you ask, "Are there any blurry, distorted, or missing numbers?" The client may say, "Yep, the ten is missing."
We use these methods because we typically do not have access to something called microperimetry, which is the test done in the eye doctor's office to find the scotoma. Once we determine a blind spot, how do we treat it?
Preferred Retinal Locus (PRL)
- When scotoma covers both fovea, the brain, within 24 hours, develops a pseudo fovea to complete all tasks, including reading
- This scotoma is going to be at different locations in different patients
- A very important part of OT training is to find this PRL and to use it effectively and automatically to view a target and read
Any time a scotoma or a blind spot is covering the fovea of both eyes, the brain, in 24 hours, will develop a pseudofovea view. Again, the client with unusual head positions or limited eye contact is trying to access the pseudofovea to see. Our job as OTs in the low vision world is to help the client find this pseudofovea and use it for function. I am not going to go too in-depth about how we do it because that is an advanced level, but I just want you to be aware that a centric viewing or finding the preferred retinal locus is one of the areas we look at in detail.
- Finding the PRL
- Use the clock
- Client looks above the card, below the card, to the right of the card, to the left of the card until a location is identified that provides the clearest image of the target.
One of the ways we find that pseudofovea is by using the clock picture. I put my fingers at the 12, have the client look at my fingers, and ask, "Did the ten come back into your vision?" You can then put your fingers at the nine and see if that vision is clearer for them. By doing this, you are helping them to find the pseudofovea.
Functional Assessment for Reading and Writing
- 1 minute read aloud test (150 – 200 words for average readers)
- Reading Endurance – 5 min intervals
- MNRead
- Pepper Test
- SK Read Test (Non-standardized)
- Low Vision Reading Comprehension Assessment (Morgan)
- Collins Writing Assessment (Free Tool)
Once we have administered all these tests, it is vital to measure function. Here are a few things that help towards that. One is the One Minute Reading Test. An average reader can read anywhere between 150 to 200 words aloud. In my mobile kit, I carry two copies of the exact text. I give it to the client and time while they read it. And at the end of one minute, I count how many words they read.
Another thing you can look at is reading endurance at five-minute increment levels. Again, I have two copies of a text, and they read while I time them. At the end of five minutes, I ask them what word they finished. I know if they are reading aloud, but if they are reading it silently, they tell me. I then circle that. The client may need a few minutes to recover before you start the second five-minute increment. You compare the times between both, giving you an idea about sustained reading. If they read a medicine bottle, that is spot reading, while a book is sustained reading.
MNRead and Pepper Test are the two tests we will review.
MNRead Test
- 2nd - 3rd-grade reading level
- Five versions
- White on black and black on white
- Test both eyes together
- Client sits 16 inches from the chart
- Wear glasses if prescribed
- Available in multiple languages
- Has an iPad version available
The MNRead or the MN Read Test is leveled at a second to third-grade reading level. It has five versions, which helps because I can give version A upon evaluation and version B upon discharge. It is an outcome measure. It has black print on a white background and white on a black background. With the white background, there is always going to be glare. If glare bothers the client, then performance on the test with the white background will be poorer than when a black background is used.
As this is a near-vision reading test, we test both eyes together at a distance of 16 inches. They wear glasses if prescribed. The neat thing about this test is that it is available in multiple languages and has an iPad version. If anybody is interested in this, please feel free to contact me. I experimented with this version during the pandemic. I do not have any research to back it up, but I am happy to share my experiences.
When working in a hospital outpatient setting, I had tons of Burmese patients who were not fluent in English, and I had no test to measure reading performance. If you reach out to the creators of MNRead, they will develop a test for you in that language. Unfortunately, I did not know that at the time.
This is what the MNRead looks like in Figure 21.
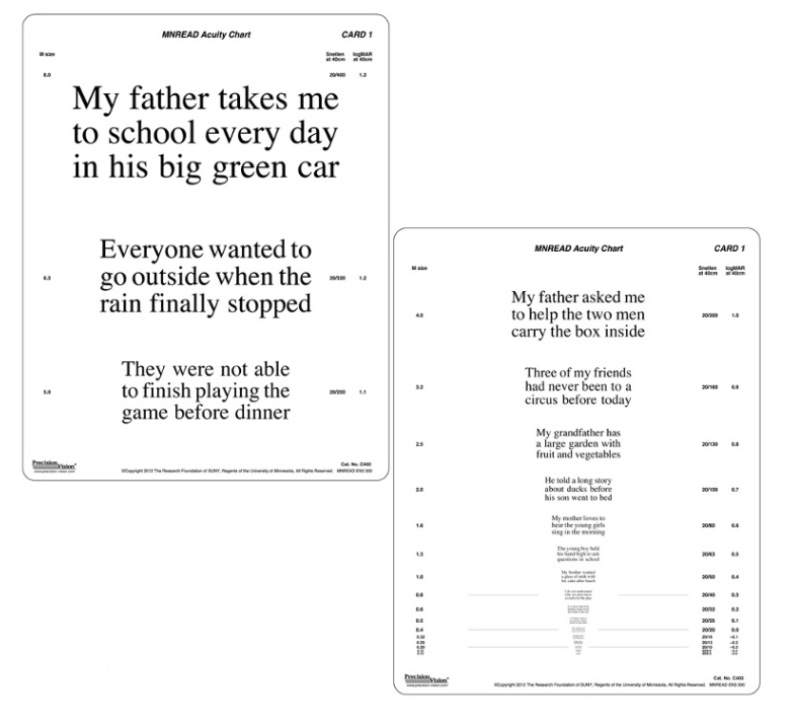
Figure 21. Example of MNRead.
The client reads the sentences, and you document the read time. This test may or may not give an idea about the scotomas that are there.
- Reading Acuity - The smallest print that a person can read without making significant errors.
- Critical Print Size - The smallest print that a person can read with maximum speed.
- Maximum Reading Speed – A person's reading speed when reading is not limited by print size.
This gives you reading acuity, whether 20/40, 20/60, or 20/100 for near vision, and it gives you the critical print size, the smallest print that a person can read with maximum speed. As a clinician, this helps me determine if a client needs enlarged font or a magnifier. For example, if I know the critical print size is four M, which corresponds to roughly 33 font size, I know that all my handouts and educational material must be that size. I also know that all my email communication in this digital-friendly world has to be in that large 33 font. I share this information with the rest of the team.
This test also gives us the maximum reading speed. If their maximum reading speed is around 8M, which is 66 font, it will be difficult for that client to read continuous text. And if that is their goal, I may jump to the electronic magnification at that point. I do not have any financial relationship with the authors or publishers of any of these tests. What I am sharing today is from my experience.
Visual Skills for Reading (Pepper) Test
- 6th to 8th-grade reading level
- 3 versions in 5 print sizes (1M,1.6 M, 2M, 3.2M, 4M)
- Non-contextual, no semantic clues
- No specific test distance, select the card 1-2 sizes above their near acuity
Another test is the Pepper Test, shown in Figure 22.
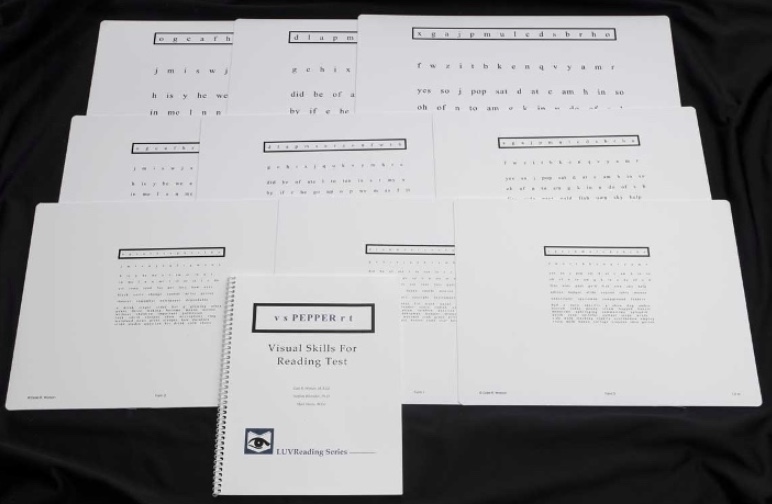
Figure 22. Pepper Test.
The Pepper Test is leveled at sixth to eighth-grade reading level and comes in three versions so that you can give one upon evaluation and discharge. It has different print sizes to accommodate font needs (as determined by MNRead) and provides a reading rate and accuracy. I can say, "The client's reading accuracy upon evaluation was 60%, and upon discharge was 80%, with a reading rate of 86 words a minute at eval and 150 words a minute at discharge." This documentation can help to support reimbursement for my services to Medicare.
Another thing about this test is that it has a series of unrelated letters and words, and sentences in this test. When clients read, they cannot bank on contextual or semantic use. An example is the word "remember" in one of the versions. If the client has a blind spot to the left, the word "remember" can be read as member, which may make sense as the word is in isolation. You do not have the centennial meaning of the sentence helping you figure out what the word should be. You are reading how you see it. The authors, Watson and Wright, have done a terrific job choosing words accordingly.
Another example is the word "theater." If you have a ring scotoma, a donut-like shape obliterating vision, "theater" may read as "heat," totally changing the meaning. "I went to the theater" is very different from "I went to the heat," but because the word is in isolation, the client does not even pick up on the fact that what they are reading is wrong or missing letters.
Sensitivity to Glare and Light
- When glare modulation is affected, photophobia (increased visual sensitivity to intensity of ambient lighting) is very common.
- Ask the client verbally about glare sensitivity and/or observe for behaviors where they always have shades on, use a wide-brimmed hat indoors, and/or window blinds are always pulled down
For informal observations of light or glare sensitivity, you are looking for behaviors like always having their shades on or wearing a wide-brimmed hat indoors. Are they always fiddling with their window blinds?
Assessments
- As vision impairment affects IADLs more than basic ADLs, some of the clinical outcome measures are -
- Revised Self-Report Assessment of Functional Visual Performance (R-SRAFVP)
- National Eye Institute Visual Functioning Questionnaire – 25
Here are two assessments that are used to assess ADLs and IADLs. They are free; the links to these two assessments are in your resources. We will talk about the first one, and you can look at the second one on your own. They are both similar to interview formats and subjective rating questionnaires.
The first is "Revised Self-Report Assessment of the Functional Visual Performance." Please acknowledge the authors if you are using this resource (Figure 23).
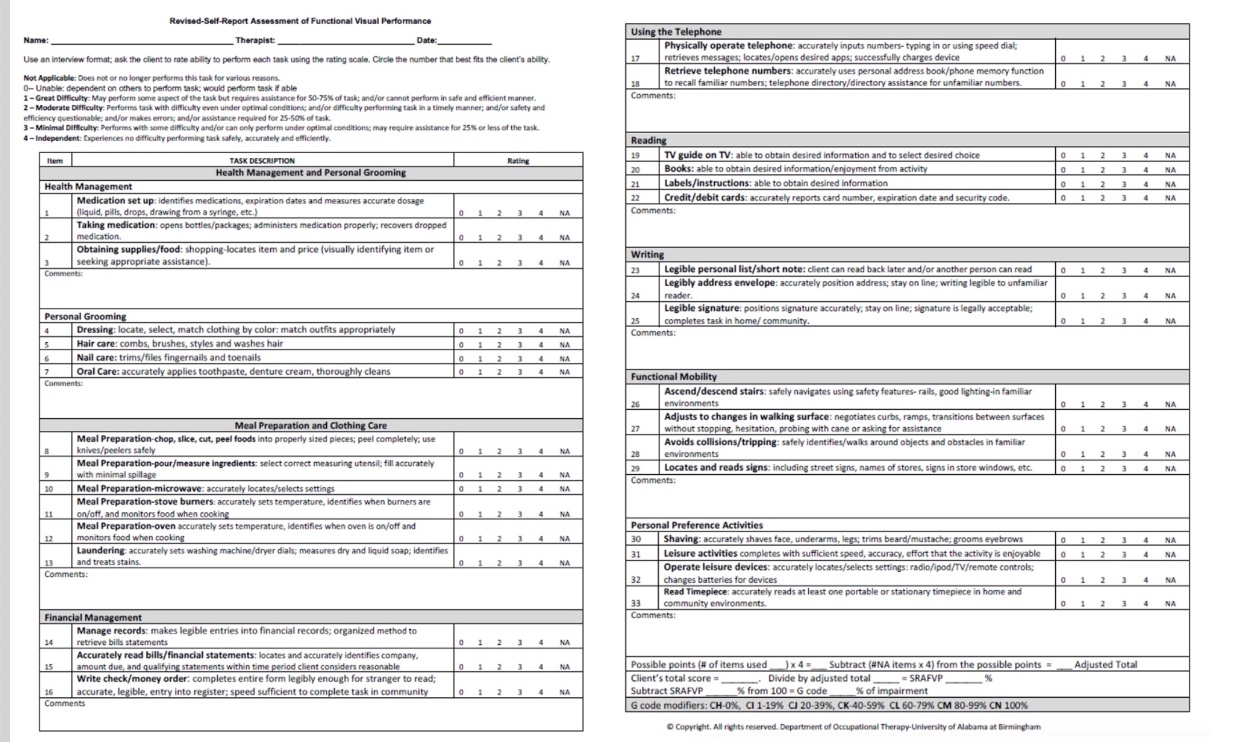
Figure 23. Revised Self-Report Assessment of Functional Visual Performance. Click here to enlarge the image.
This test looks at ADLs and IADLs like health management, meal prep, grooming, writing, and reading. The client scores it on a scale of zero to four. Zero is unable, and four is independent. At the very end, you get a percentage of impairment, which correlates to the G codes for all those practicing in the acute hospital environment.
This tool is handy, and this tool also has an app. I am old-fashioned, I have always used the paper version, but because it is available as an app, you can easily score this on your phone. The only thing to be aware of is that you cannot save the file. You have to download it as a PDF and send it to a secure email address for it to be a part of the electronic medical record.
Goals
- Client will be able to read a menu, financial statements, and bills with 90% accuracy using LVAD consistently towards independence in ADLs and IADLs in 3/3 trials.
- Client will be able to complete simple meal preparation with the minimum assistance of one where he/she is able to set the dials on the oven, read a simple recipe, use the microwave and manage the stove controls with 75% accuracy in 2/4 trials.
- Client will be able to demonstrate complete independence and 75% accuracy in modifying his/her screen to improve her reading tolerance from 3 to 6 minutes without visual fatigue using the teach-back method.
We justify intervention by achieving goals. Above are some sample goals.
OT Intervention
- Focus is on management and prevention of vision loss, NOT cure
- There are no magic pills, optical aids, or glasses that will cure the disease
- OT focus should be to help them "successfully age in place"
- Client education is critical
The intervention focuses on managing and preventing vision loss, not a cure. It may take a few sessions and earning the trust of the patient to even start with intervention. No magic pills, optical aids, or glasses will cure the disease. OTs' focus should be to help them successfully age in place, and client education is critical.
Light
- Rule of thumb is to increase lighting (task as well as ambient) but avoid/minimize glare
One rule of thumb is to increase both task and ambient lighting. Task lighting is the central lighting, while ambient lighting is the lighting in the room. As we increase lighting, we want to avoid or minimize glare. Figure 24 shows a light meter.

Figure 24. Example of a light meter.
You can use a light meter on the work surface, whether that is the countertop in the bathroom, next to the microwave, by the stove, or on the table where the print is like a magazine or document. You do not want to place it next to the light source but rather on the work surface. This Lux Meter, or the light meter, is pretty inexpensive. You can find one for less than $20. It is handy to have in your tool kit.
- The ratio between the page/electronic device, the desk, and the room should be 5:3:1
Figure 25 shows recommendations by ISNA, the Illuminating and Engineering Society of North America.
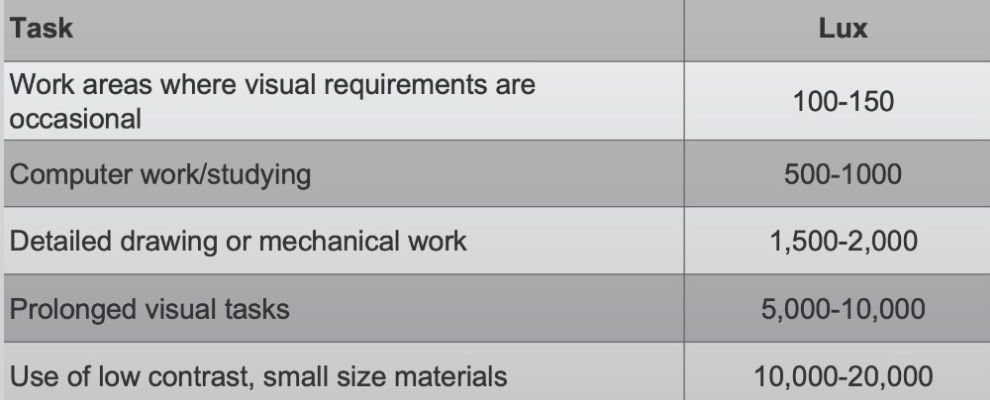
Figure 25. Light recommendations by the ISNA.
The term Lux is a measurement for illumination. These recommendations are for a healthy eye.
There have been studies concerning light recommendations with macular degeneration, and there is a wide range from 2,000 Lux to as high as 7,000 Lux just for general viewing.
I have learned over the years not to get stuck on those numbers but to increase lighting and assess function. Is the client able to read effectively? Can the client give me 150 to 200 words a minute with the light we put into place? I am happy to share research information in this area if anyone is interested.
- Ambient lighting
- Should be even, flicker-free, and devoid of shadows
- Task Lighting
- Always have reading light placed behind the dominant eye. Light should not be shining into the eyes
- Use the inverse square law for lighting
- Use gooseneck or swing arm lamps to adjust the height
Ambient lighting should be even, flicker-free, and devoid of shadows. We place task lighting behind the dominant eye. So if I use a floor-length lamp, like an OttLite, I want to put it behind the dominant eye. Please keep the holistic nature of OT in mind. We do not cause back pain, and light should not be shining in their eyes.
You can use the inverse square law for lighting. If anybody is interested in the mathematical side of it, I would be happy to discuss that with you at the end of the seminar. The inverse square law of lighting means that as you move the light closer to the surface, there will be disproportionately more light at the surface. A table lamp with that gooseneck, as in Figure 26, provides more light.

Figure 26. Example of task lighting.
If you do not have a gooseneck, look for table lamps with swing arms. Besides the OttLite, there is Stella, Verilux, and Tektronix. There are quite a few names, but you are looking for brightness, which you can measure with the light meter. Once we have addressed the brightness of the light, we look at the quality of light.
Five bulbs are out there; Incandescent, fluorescent, full spectrum, LED, and halogen. We will not be talking about incandescent because those are being phased away. Let's start with fluorescent, which will be the cool light.
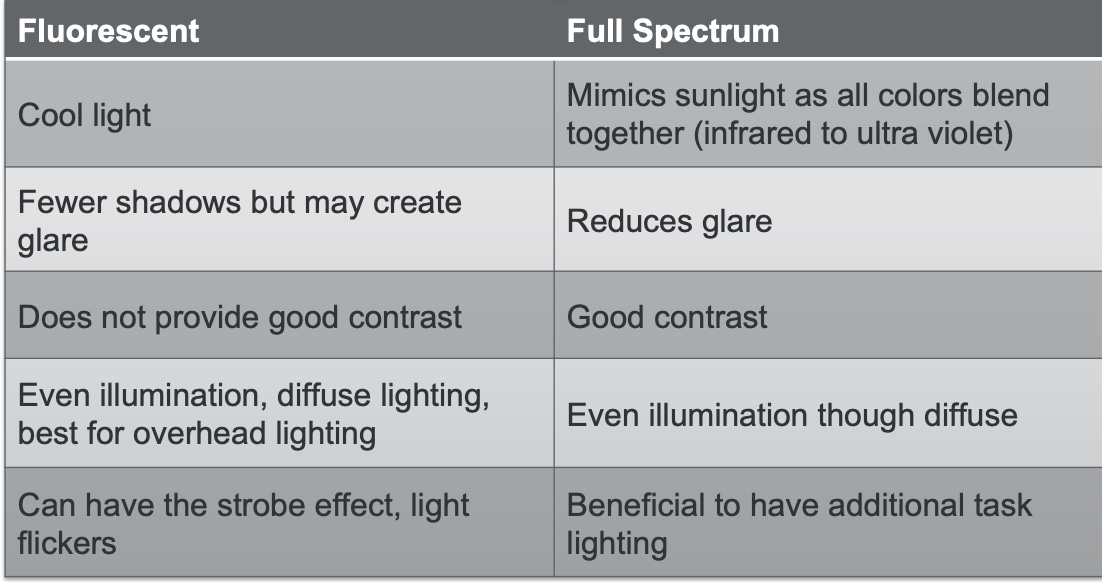
Figure 27. Fluorescent bulb characteristics.
Fluorescent bulbs are cool, white light. Fluorescent has fewer shadows, but it can create glare. It also does not provide good contrast, but it is cheap. This is what you see in most public places. It is best for overhead lighting, although it is diffused. It can also have a strobe effect with flickering that may be bothersome to our clients with pathophysiology.
Full spectrum lighting is light that mimics the sunlight, and all colors are blended, which reduces glare. There is good contrast and even illumination, just like the fluorescent, and it is beneficial to have as an additional task light. As we are talking about these bulbs, there is not going to be rhyme or rhythm to what bulb will match the patient's eye, other than the fact that it allows the patient to choose the light that is best for them for viewing or reading. You can use different light colors and decide what light is best for them. As vague as it sounds, patients do it instinctively in a matter of minutes, and they will tell you. "I dislike the red light (or white or yellow). It is just a matter of doing one or two sets, and they will immediately tell you which they prefer.
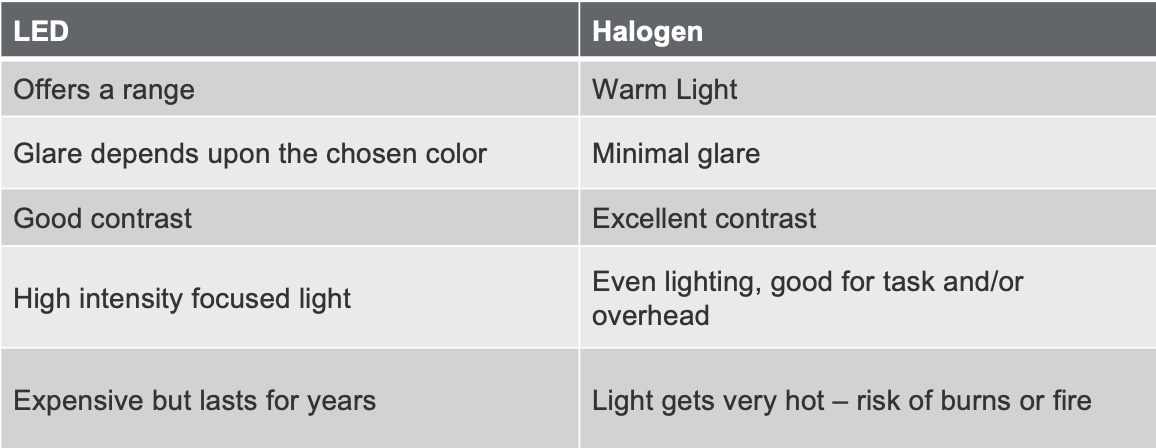
Figure 28. LED vs. halogen.
The next one is the LED which offers a range. One lamp will give you warm white light and the sunlight or blue light. Not only does it give you a range of colors, but it also gives you different brightness settings. This is why LEDs are starting to be a favorite, other than these lights last for years. LED offers good contrast, and it is a high-intensity focused light. Figure 29 shows another example of task lighting.
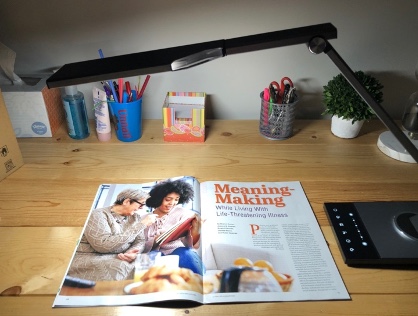
Figure 29. Example of another task light.
Halogen is still my favorite, but it is difficult to get. I do not like using halogen with the aging population because the light gets very hot, and there is a risk of burns or fire. For example, if you have a curtain next to a halogen table lamp, you run the risk of the curtain catching fire. Halogen lights offer excellent contrast. There is minimal glare, but the color tone for halogen will usually be amber, yellow, and red.
Choosing a light is going to be very subjective. It is going to be on a case-by-case basis.
Computer Screen
- Eyes should be resting on the upper 1/3 rd. of the screen
- If there is a window, ensure that the client's back is towards the window and that there is no glare on the screen
- Adjust blinds throughout the day to ensure good lighting around the task area
- Choose a wider monitor for increased field of view; flat screens are preferable
- Monitors with LCD crystal display reduce glare
- Decrease pattern density by spacing text and increasing size
We have to talk about computer screens in the COVID world. Their eyes should be resting on the upper one-third of the screen. My ergonomic assessment starts from the eyes, and then I look at the back, hips, knees, and ankles.
If there is a window, ensure the client's back is towards the window, and there is no glare on the screen. My personal favorite is a corner desk without a window. If you can have a window to the side, that is awesome because they can look out at the side. I have a window by my computer, and whenever my eyes get tired, I look out. That is my 20/20/20 rule. You can adjust the blinds throughout the day to ensure good lighting around the task area.
Choosing wider monitors for an increased field of view is also crucial. However, do not go too wide because if you do, you have to have exaggerated head turns that may cause a neck ache. Flat screens are preferable, as they reduce distortion at the edges and increase the usable field.
Use LCD crystal display monitors because they reduce glare. You can also decrease pattern density by spacing text and increasing size.
Modify the Environment
- Know the client's organization system and work accordingly
- Organize with the client, not "for" the client
- Establish a labeling system
- Increase contrast
- Decrease pattern
- Decrease clutter
- Increase font size / large print
We often modify the environment in our treatment and can use the same principles here. Know the client's organization system and work accordingly. Teaching a client a new organizational system is not advisable when they already have a visual deficit.
You can always teach anybody new tricks, but I have learned from experience that it is better to work with their organizational system rather than teach them something new. Organize with the client, not for the client, because you will leave, and they will not know what happened.
Establish a labeling system. A labeling system could be as simple as using real paint on appliances, index cards, or adhesive stickers. When you are labeling items, be sure to be cognizant of the font size on the labeled item because the client has to be able to read it. Sometimes when I am doing a labeling system, I may have the help of a family member or client as they know what their system is.
You can also increase contrast, decrease pattern, decrease clutter, and increase font size. Here is an example of contrast in Figure 30.
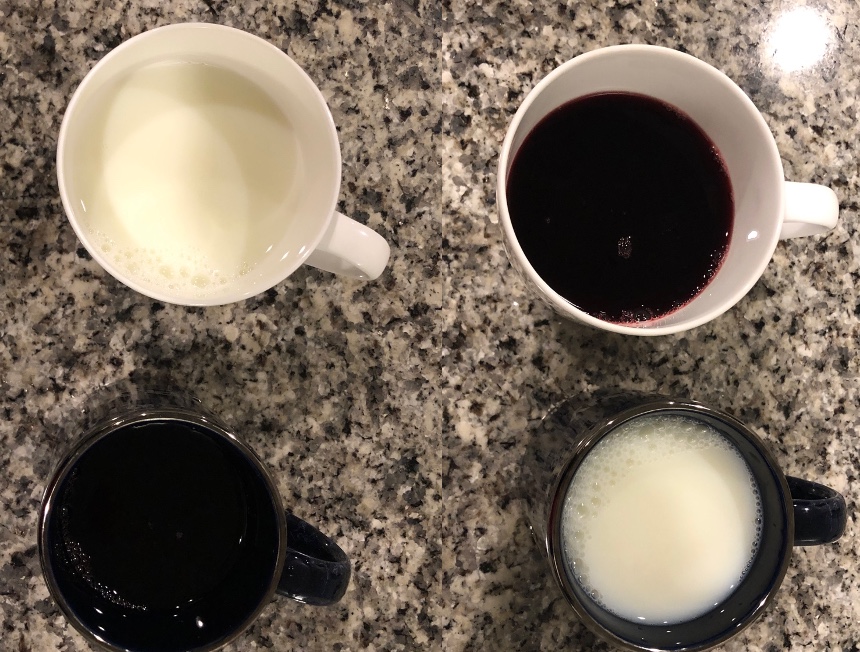
Figure 30. Increasing the contrast of the liquid in the glasses helps with vision.
Appliances these days are sleek and shiny, and everything blends. They are not very friendly to our low-vision patients. They do not even have the dials and the raised dots they can feel. Clients often fear upgrading their appliances because they are used to the dials. Here we have used principles of magnification for the three and zero in Figure 31.
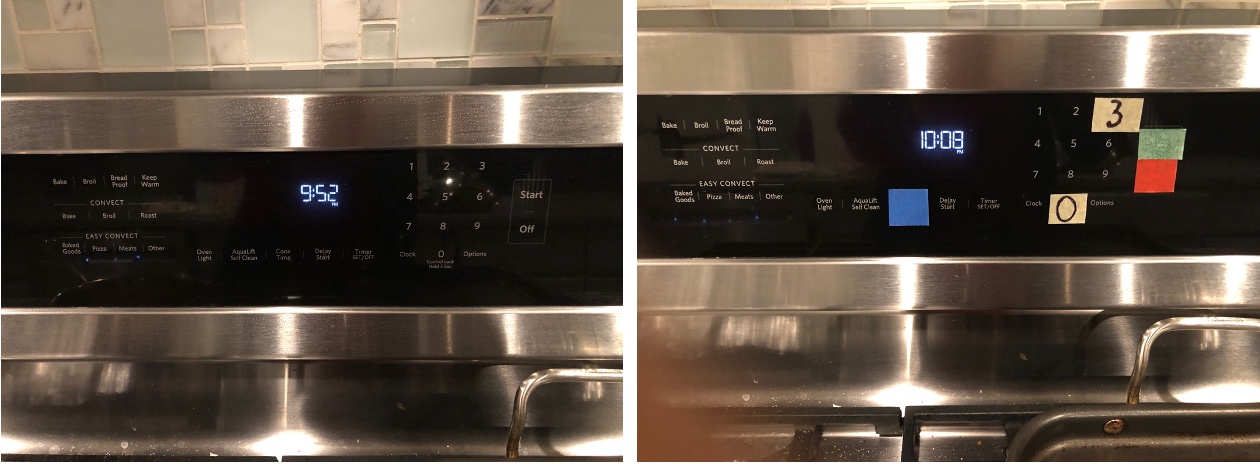
Figure 31. Modifications to the front of the stove.
You also see the tape that has been used to add contrast. Do not modify every setting on the appliance because that will defeat the purpose. I will ask, "What do you eat?" If they say bean casserole, I ask, "What setting?" They may say 300 degrees Fahrenheit for 30 minutes. I will then label the 300-degree Fahrenheit setting and the 30 minutes because that is what they will use most often.
Here we have eliminated patterns, added a solid color, and reduced the visual clutter in Figure 32.
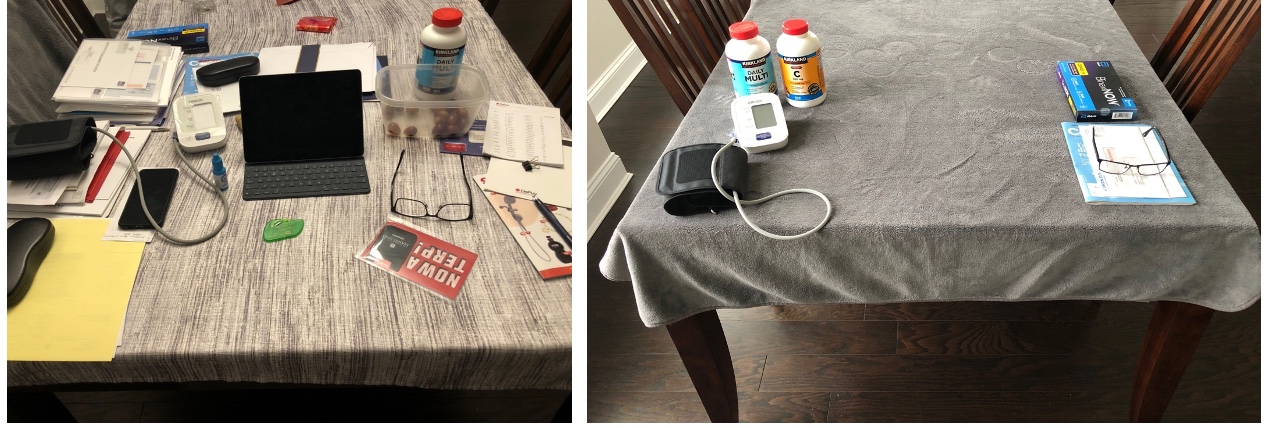
Figure 32. Example of reducing pattern and visual clutter for a work setting.
Again, you are not organizing for the client. You are organizing with the client. Here is an example of decreasing pattern by adding a solid color and contrast to a puzzle activity (Figure 33).

Figure 33. Contrast for a puzzle activity.
Kitchen and bathroom areas, especially water, can be hazard zones within the house. Bath toys can be added so clients can see the rising water (Figure 34).

Figure 34. Toys in the bathtub shows rising water.
Functional Mobility
- Adequate lighting is essential
- Remove obstacles and potential hazards
- Add contrast
- Decrease glare
Indoor mobility is another area for OTs. Outdoor mobility sometimes falls in the realm of the COMS, a certified orientation, and mobility specialist. They work on cane training or sighted guide techniques. For indoor functional mobility, we need adequate lighting, removing obstacles and hazards, adding contrast, and decreasing glare.
Examples of these principles are shown on a staircase in Figure 35.

Figure 35. Adding contrast and decreasing glare on a staircase.
There is good contrast at the edge of the stairs using tape, and the mat contrasts with the steps and floor. Make sure that it is a nonskid mat, or put Dysem underneath.
Telescopes
- Can use telescopes to increase the ability to see detail
- Easier for an older adult to use telescopes with low power
- Keep in mind that slight motion may occur, which may affect balance and safety
An example is in Figure 36.

Figure 36. An example of a telescope.
Photophobia
- Use light-colored filters indoors and dark-colored filters outdoors
- Use hats or visors outdoors and indoors
- Overlays
- Cover surfaces
- Avoid positioning next to the window
Photophobia, or glare sensitivity, can be reduced by filters, as shown in Figure 37.
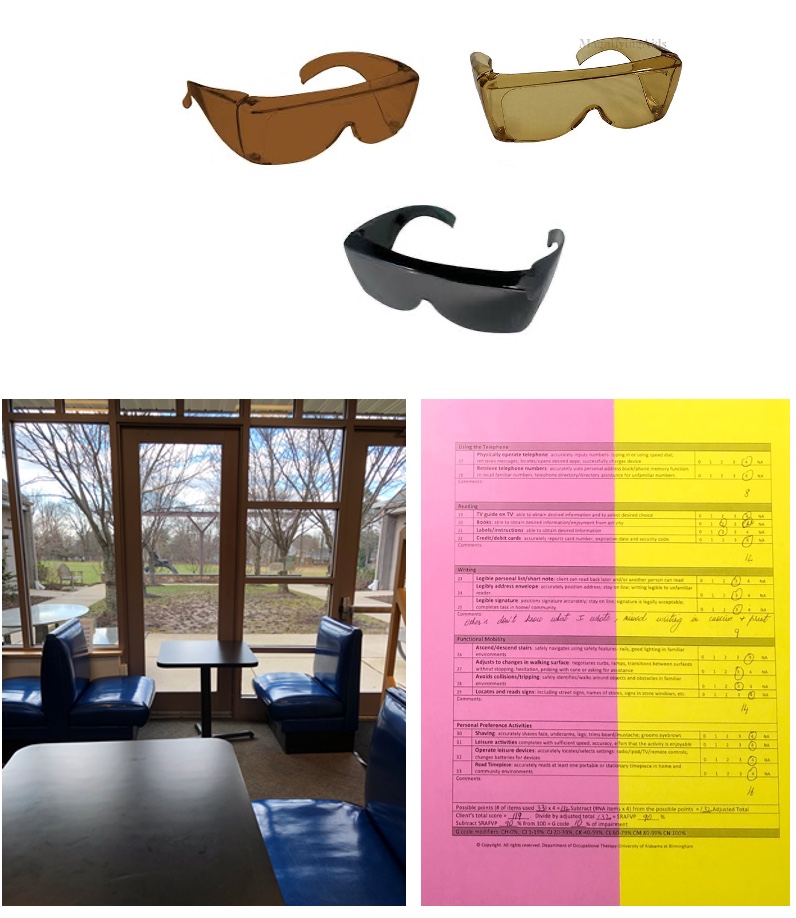
Figure 37. Glare sensitivity shown in a room with different filter options.
Use light-colored filters indoors and dark-colored filters outdoors. The nice thing about these glasses is they have side shields and lips to prevent light from entering the eye. They can also use hats or visors indoors if need be. In my mobile kit, I have overlays of all different colors, and I place them side to side so that the client can figure out which one works for them. The only disadvantage of overlay is that it does not work well with spiral-bound notebooks.
I also cover surfaces all the time. I like to find neutral-colored bed sheets to put on shiny desks. You can put this on a vinyl seat as it reflects light like crazy. We also want to avoid positioning the client next to the window.
Sensory Augmentation-Tactile
When creating this slide, I thought about labeling it a "Sensory Substitution." I stopped myself and changed the title to "Sensory Augmentation" because we, as OTs, are trying to facilitate the usable vision that the client has. We augment the client's vision when we add tactile, auditory, and cognitive strategies. Figure 38 shows some examples.

Figure 38. Sensory augmentation ideas.
Bumper dots are raised and can be put on appliances. Some dots and dashes can go on the keyboards, or keyboard stickers can be used. The keyboard sticker is black on yellow to give high contrast. Raised writing pen creates tactile input. We can use different rubber bands on similar cans. For example, there is a thick rubber band on the left and a thin rubber band on the right. We can also use a rubber band on one and not the other. Work with a client to come up with a system.
Sensory Augmentation-Auditory
- Techniques like recognizing the beep when the dryer is done or bacon pops when it is done
- Talking devices like BP monitors, liquid level indicators, electronic watches, calculators, and smartphones
There are also auditory approaches. Talking devices like BP monitors, glucometers, and liquid level indicators.

Figure 39. A talking glucometer and a liquid level indicator.
In the image on the right, when the water rises and hits the sensor, there will be a shrill beeping voice. Electronic watches, calculators, and smartphones all help. Monitoring blood pressure, as well as sugar and medication management, are two essential areas that we address as OTs. Medicare covers the talking blood pressure cuff and the glucometer. Please educate the client as they are reimbursable.
Cognitive Strategies
- Put toothpaste directly into the mouth
- Dip the measuring spoon into the oil instead of pouring oil into the spoon
- Pre-chopped vegetables
- Wrinkle-free clothing
- Visual memory
Here are some cognitive strategies. Putting the toothpaste directly into the mouth is one tip, instead of adding another visual step of lining the toothpaste on the toothbrush. Another one is to dip the measuring spoon into the oil instead of pouring the oil on the measuring spoon. Other simple ideas are pre-chopped vegetables and wrinkle-free clothing.
Visual memory is also something that can be tapped. If the water is boiling, the individual may hear the sound of the bubbles or feel the heat rising, triggering visual memory. Figure 40 shows this technique.
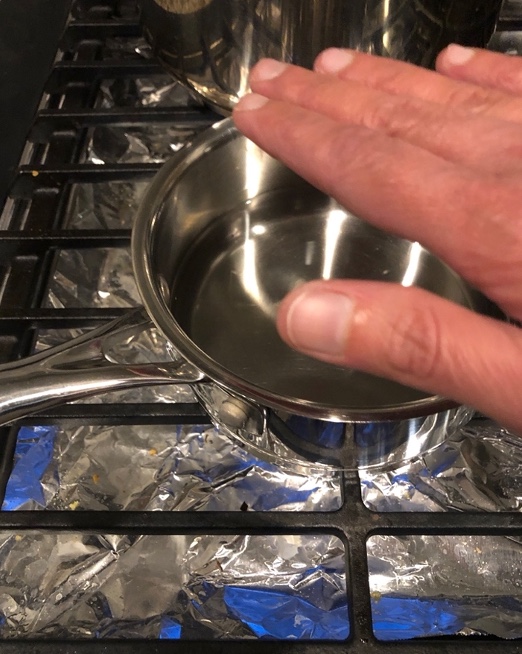
Figure 40. The visual memory of water boiling.
Assistive Technology – Low Tech

Figure 41. Low-tech assistive technology.
Here are examples of low tech assistive technology like a hands-free magnification (between 2X to 5X). It is also illuminated. This enlarges what the person sees and helps them stay on the line. Jewelers and dentists sometimes use these. The cards, calculator, and phone show increased font and contrast, and there is also a high-contrast keyboard. Clients can also get a large print checkbook. Banks have these available, but the client has to know to ask for them. There are also talking prescription recorders. I the patient goes to the pharmacy and buys this kit, the pharmacist will record the name of the medication. For example, Synthroid would be entered into the prescription recorder, and they press the button to hear what that med is.
Computer and Accessibility Features
Computer and accessibility features are important in the COVID world. Figures 42 and 43 show some of how to navigate accessibility on a PC.
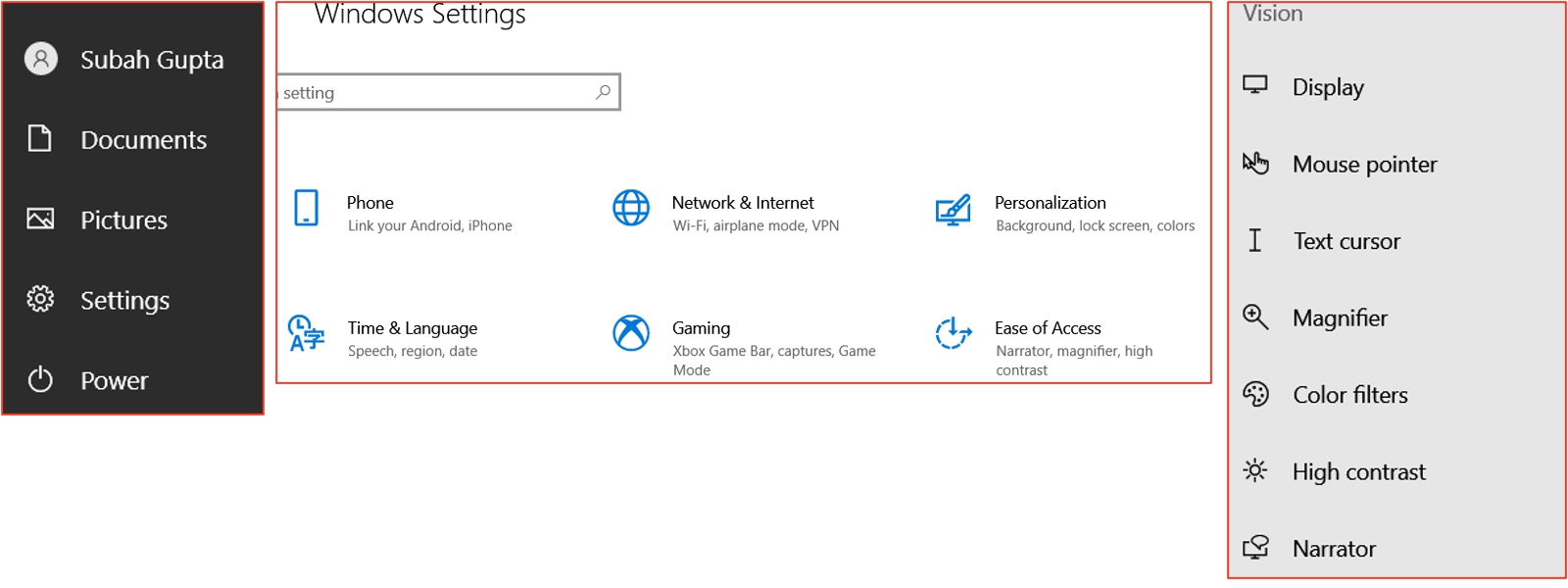
Figure 42. Windows settings for accessibility.
Once you find the ease of access, you have a host of options under vision.
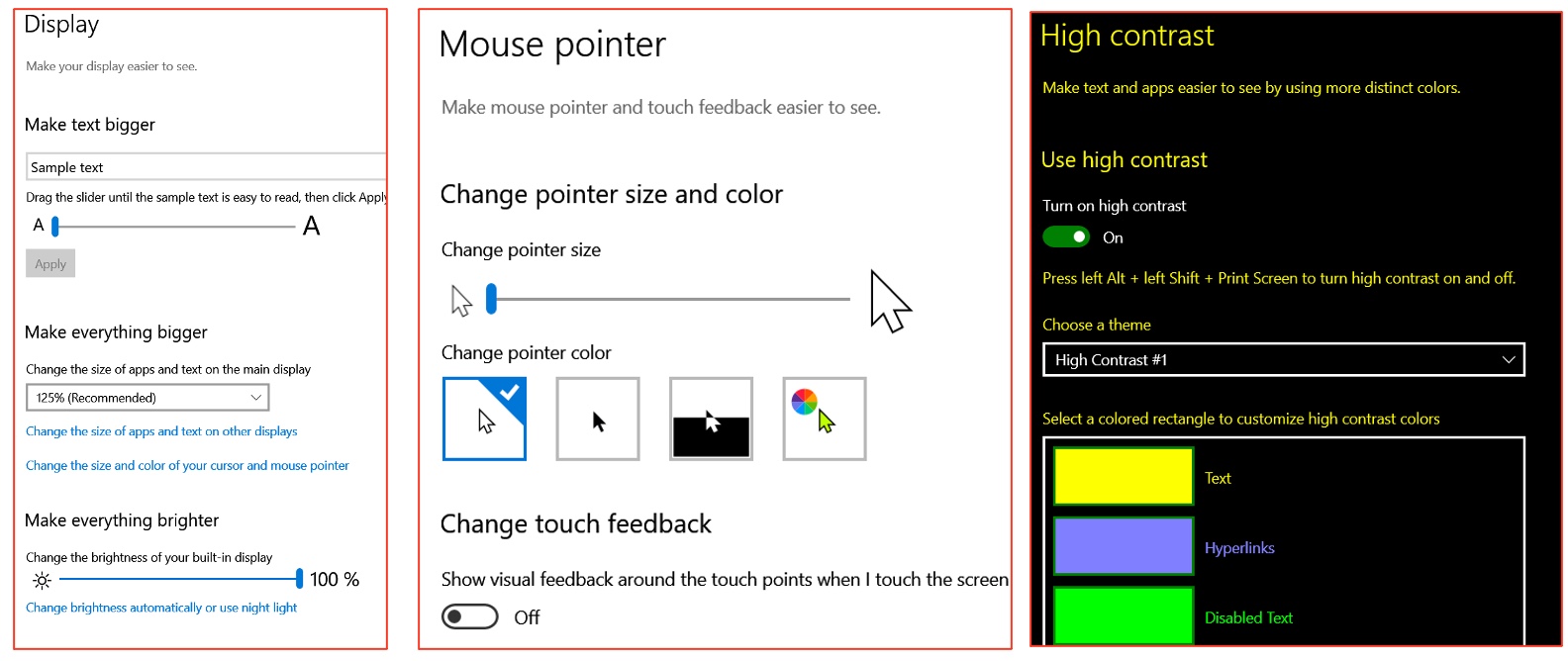
Figure 43. Options for vision.
I would encourage you to play with these options. Magnifying what you see on the screen can be easily done by hitting the control key and the plus together, but it can also be done under the display button, where you have to make the text bigger. If you are making text bigger, it makes sense to make the mouse pointer bigger too. Otherwise, you will lose the mouse pointer in the text, and it will be hard to figure out or track where you were.
Another neat feature is this inverted feature, where the mouse pointer may automatically change colors. It is going to be white on black or black on white.
The high contrast feature automatically inverts the screen for the option of yellow print on black and a few other choices. You can get a green print on black or a white print on black. A word of caution, when you turn the high contrast feature on, it does compromise picture quality. So if the client is using the computer for online shopping, for example, Amazon Prime, they will not like it. The picture quality is significantly compromised, but this is a great feature if the client uses the computer only for work purposes, like Word and Excel.
Assistive Technology- High Tech
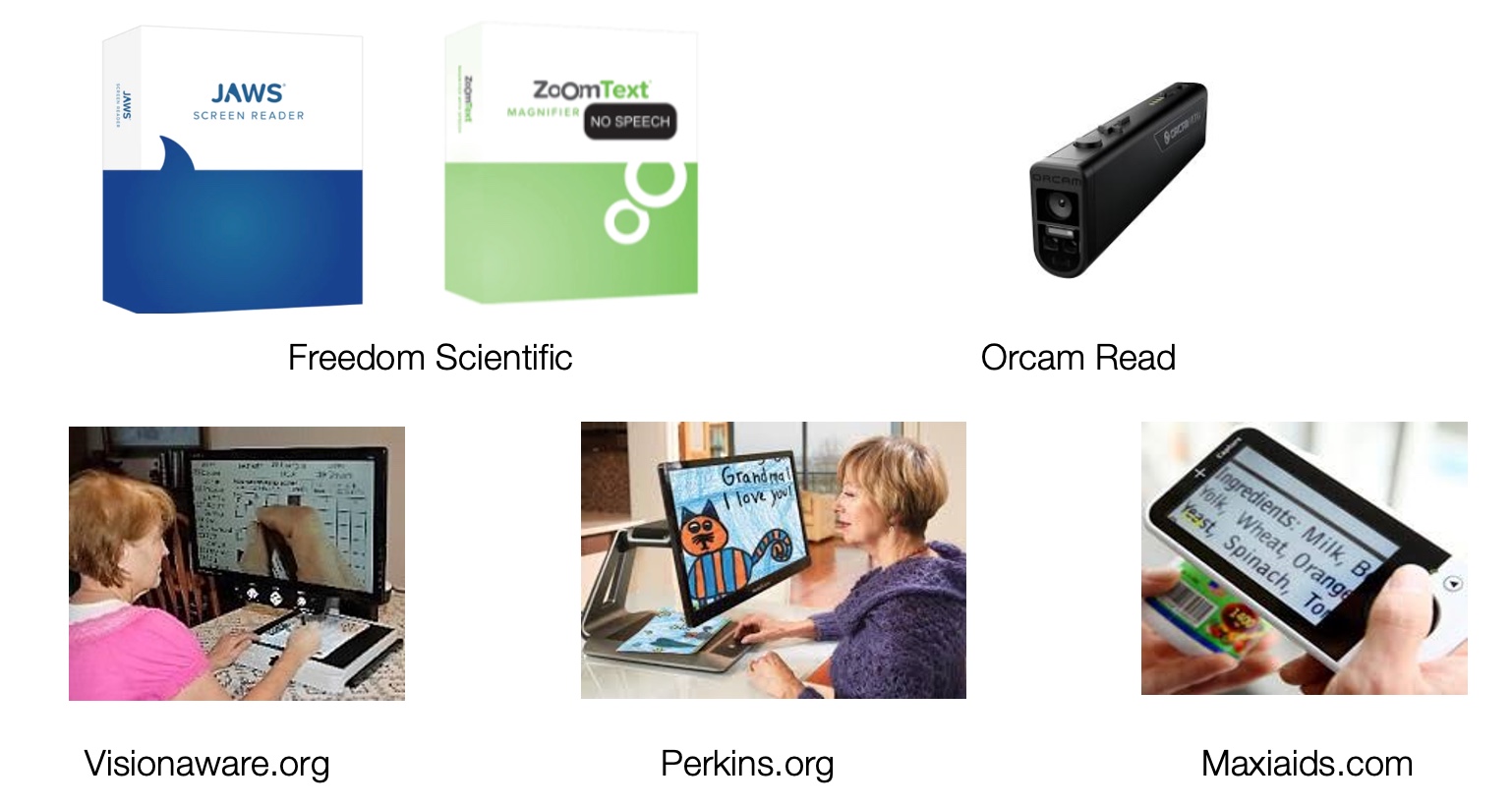
Figure 44. High-tech assistive technology.
This is a picture of JAWS and ZoomTech by Freedom Scientific. It is also available as a free download. The client can experiment with it, use it, and decide if this is a subscription they would like. JAWS is text-to-speech technology and a screen reader, whereas, Zoom is just magnification. Orcam is a neat piece of equipment as it takes a picture of the document and reads it aloud. It will also look at the barcodes and tell you what the item is. It even recognizes faces.
Other CCTV options are at the bottom. If a client has difficulty reading 8M print and wants to read continuous text, we can use electronic magnification. You would put the text underneath, and it magnifies it. You can also do it for writing. In the bottom left image, the client is doing a crossword puzzle or writing. The only thing that you have to think of is when you are writing. We are visually monitoring our hands. With the CCTV, you have to look at the screen, not your hand, so this is a bit of an adjustment. There are also portable electronic magnifiers. My clients love it because it allows them to read menus.
Reading
- Make sure that the client has the most current prescription glasses
- Complete PRL training
- Locate the target
- Track a target
- Gaze shift
- Pre-reading exercises
- Comprehension exercises
- LUV series
- Pre-reading and writing exercises
- Training is completed without the use of an optical device
I will not go into detail because this is an advanced level. We, as OTs, can do visual skills training to help a client read. Please keep in mind that reading is a three-step process. At the sensory level, we have to decode the print, and the print has to be clear. At the decoding level, you have to recognize the letters and the words. Lastly, we must recognize or understand the sentence's meaning at the comprehension level. These are the steps we go through regarding pre-reading and comprehension exercises. Figure 45 shows an example of one of those pages.
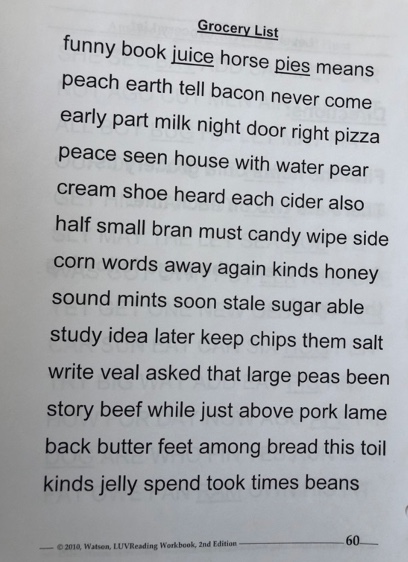
Figure 45. An example of a comprehension exercise.
Magnification
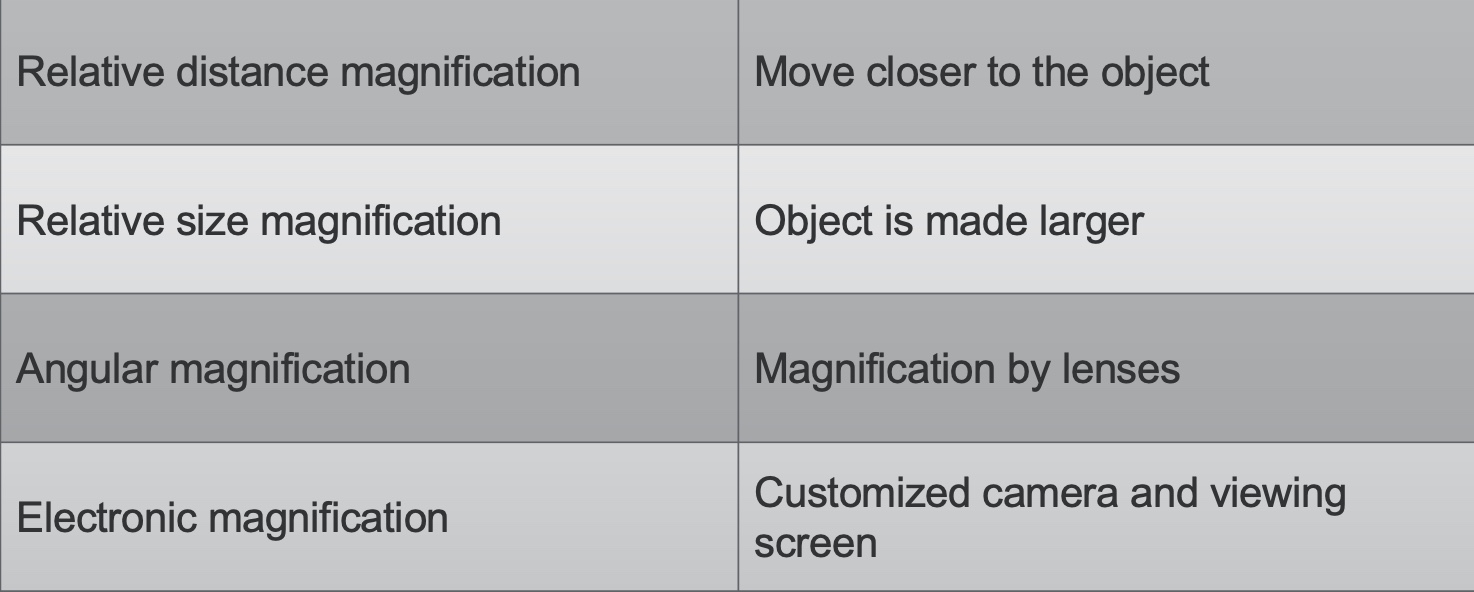
Figure 46. Magnification principles.
Magnification is either changing the distance by moving closer to the object or by making the object larger by using lenses or electronic magnifiers.
Angular Magnifiers
- Always train the client to look through the center of the lens as there is light scatter at the edges of all lenses
- The handheld magnifiers should be kept parallel to the print that needs to be read
- The refractive strength of the lens is measured in diopters, most magnifiers range between 2- 60 diopters
- It is important to know the focal distance of the magnifier
- If the strength of the magnifier is known, the focal distance can be calculated by using this formula:
- 100 divided by diopters. For example - If the diopter strength is 20, the focal distance is 100 divided by 20, which is 5 cm.
- Strength is also sometimes given in X units
- 1x = approximately 4 diopters
- Focal distance determines the distance the client should hold the magnifier from the page to get the clearest image; if the object is too close, the image is magnified but not clear; if it is too far, then the image is upside down
- Keeping the eye closer to the magnifier increases the field of view
- The weakest magnifiers have the biggest lens, strongest magnifiers have the smallest lens
When looking through a magnifier, you train the client to look through the center and keep it parallel to the print being read. You also have to figure out what the magnifier's focal distance will be. This means that the object that needs to be read must be within the magnifier's focal distance. The formula you use is taking 100 and dividing it by the diopter strength. This particular magnifier is 16 diopters. So I would divide 100 by 16, and the number I get will be the distance the paper needs to be held (100 by 20 is five centimeters). If the paper is over five centimeters, it will be upside down. I wish I knew this as a generalist OT because I cannot tell you how often I had patients walk in and tell me that the magnifier did not work. They were holding the print too far away from the focal distance. What I do now is to tie a string to the magnifier's stem; in this case, it would be five centimeters in length. I tell the client to make sure their paper is in between the size of the string.
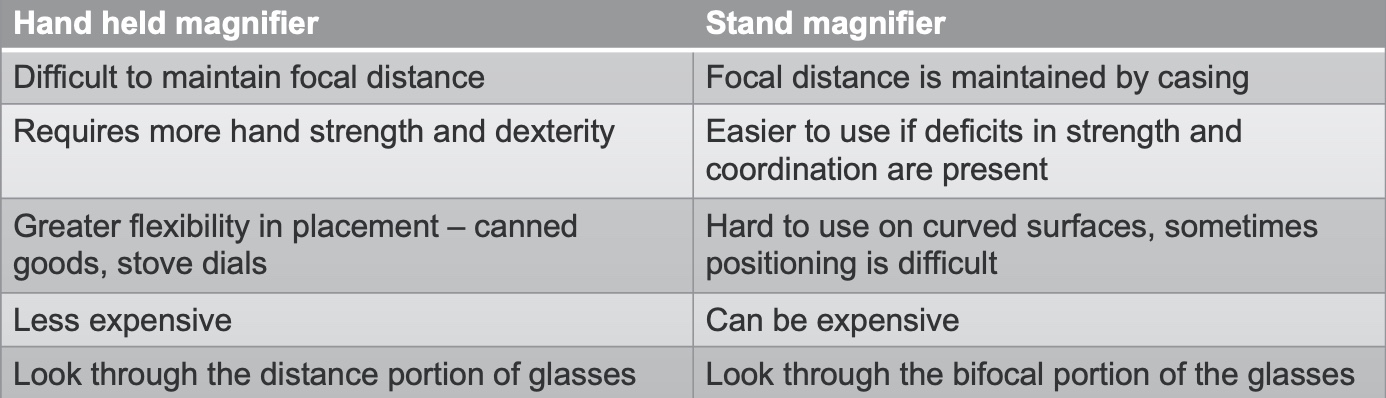
Figure 47. Differences between a handheld and stand magnifier.
Examples of handheld magnifiers are seen in Figure 48.
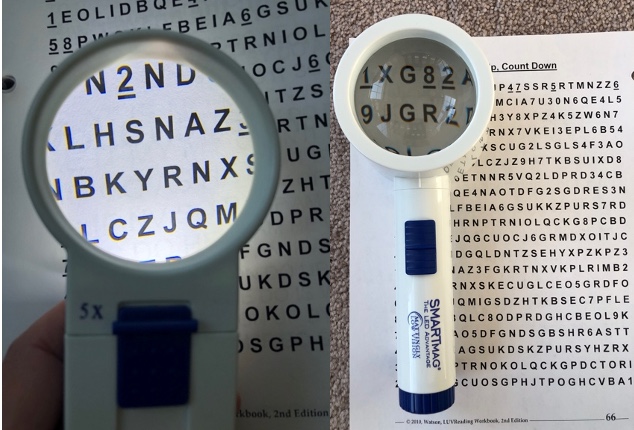
Figure 48. Handheld magnifiers.
Handheld magnifiers can be helpful because you can look at canned goods and stove dials. On the other hand, stand magnifiers may be beneficial if the patient does not understand the focal distance because, with the stand magnifier, the casing of the magnifier is the focal distance in itself.
Telescopes are one of the most underutilized optical devices. I want to mention it here because it is easy for an older adult to use a telescope with low power to see objects at a distance.
Writing
- Difficulty staying on the line
- Difficulty with spacing
- Difficulty with reading what is written
- PBS Technique taught
Example of a patient with visual deficits for writing (Figure 49).
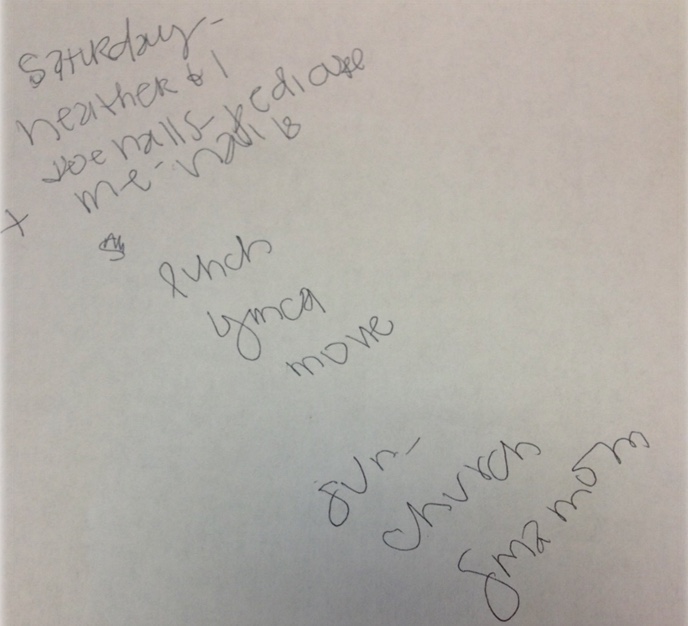
Figure 49. Sample of writing from someone with visual deficits.
They have difficulty staying on the line and difficulty with spacing in this sample.
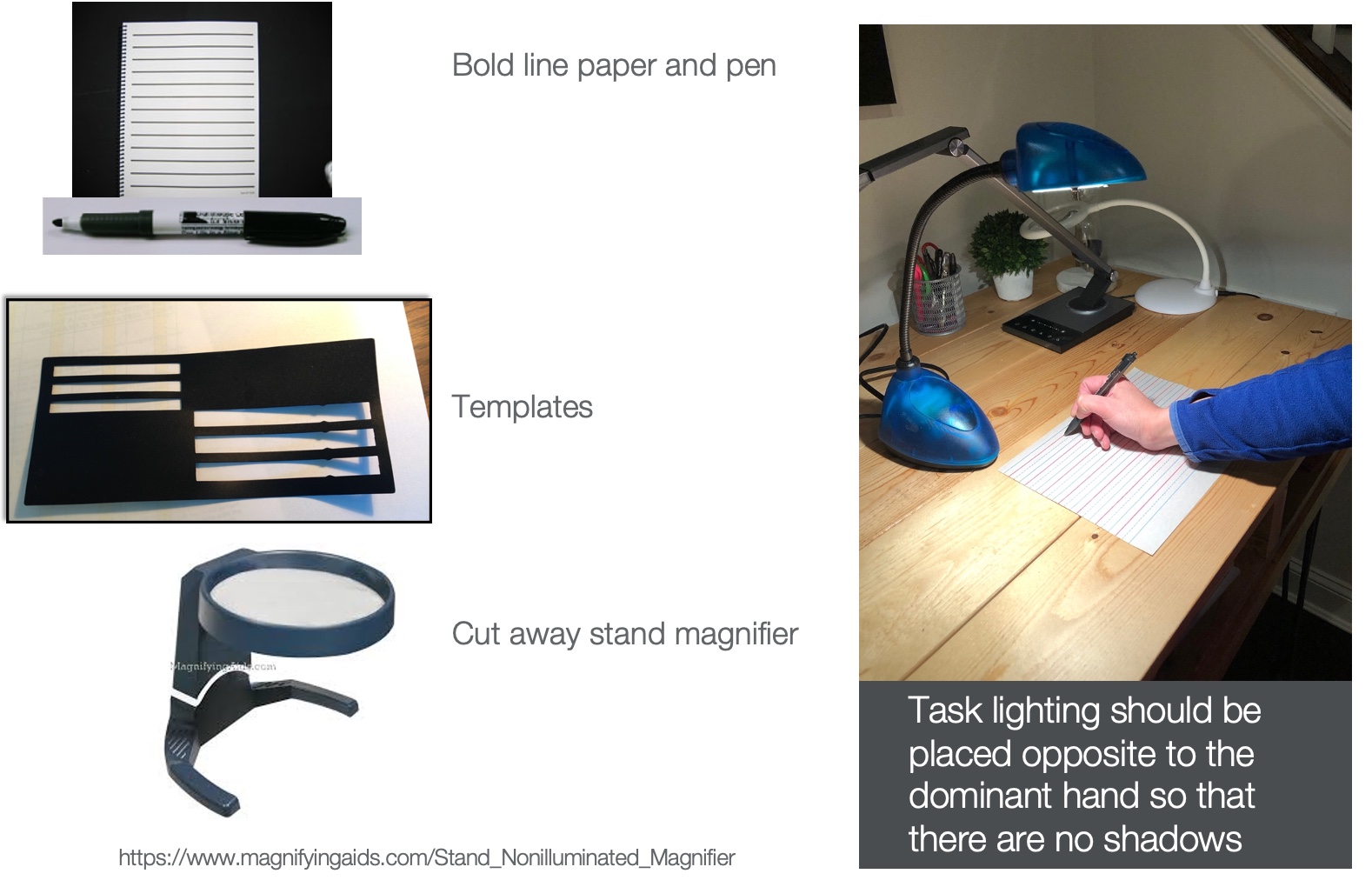
Figure 50. Here are some other reading and writing options.
You can teach them to print big block letters and spacing techniques. I often give them bold line paper and pen to teach this technique. Above is a template for an envelope. There are templates like this available for writing a check as well. These help the client read and keep the alignment, so they are not skipping lines or jumping lines. Another picture shows a stand magnifier. Something important with task lighting is that it should be placed opposite the dominant hand, so there are no shadows.
Low Vision Apps
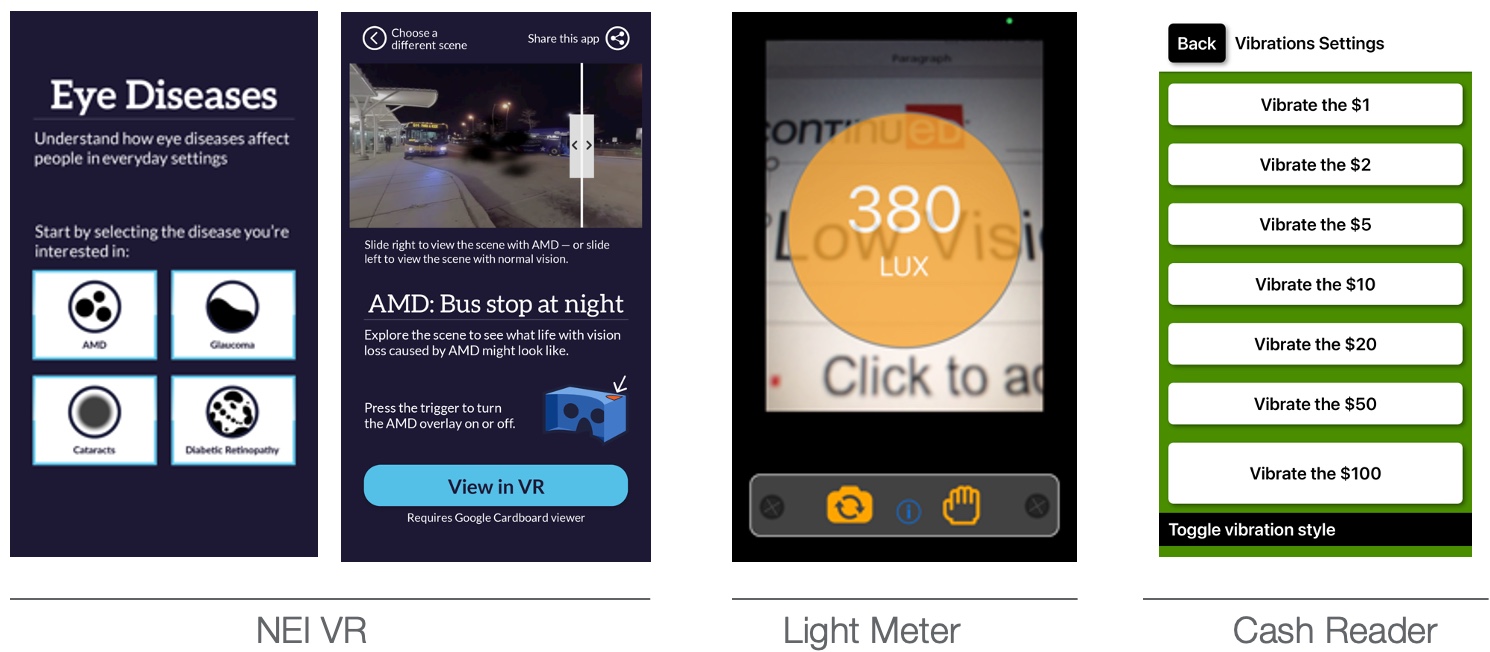
Figure 51. Examples of low vision apps.
This is a National Eye Institute virtual reality app. It does a great job of depicting what vision is with macular degeneration, glaucoma, cataracts, and diabetic retinopathy. I often use it as an educational tool for family members.
There is also a light meter app. In my experience, I have tried to do a reading with the light meter app and the light meter, and I have never come across equal values. However, I encourage the client to have a light meter app because they can appreciate the jump in lighting when they take away that opaque shade of their lamp or bring the light closer to what they need to see. They may see this number jump from 380 to 600, so you can get the patient's buy-in.
There is a cash reader app. If you have a client who lacks hearing and vision, it uses vibrate mode to determine what the currency is.
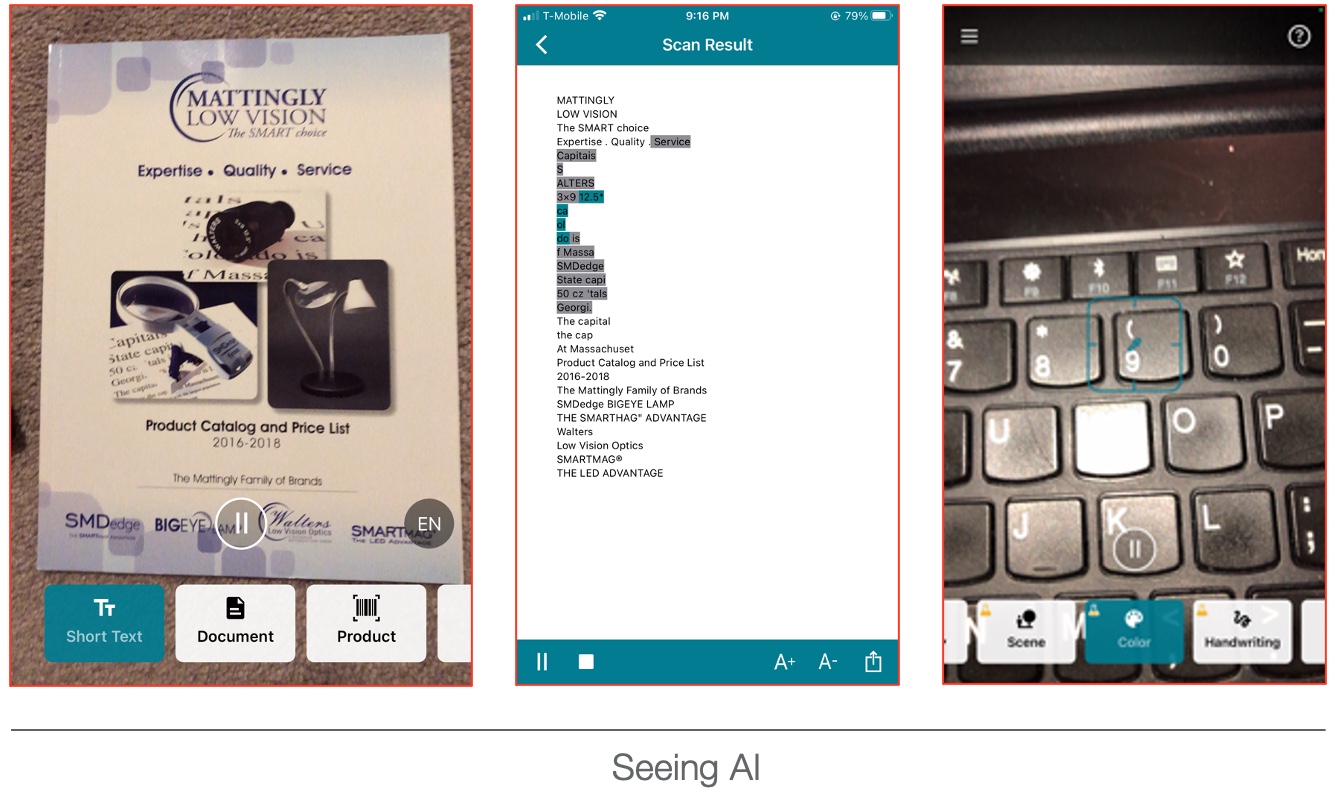
Figure 52. Seeing AI on smartphones.
This technology is on phones. It can read a document, identify colors, and recognize products by scanning the barcodes.
Driving and Driving Cessation
- Know the requirements to be eligible for driving privileges in your state
- For example, in PA, visual acuity/best-corrected vision has to be at least 20/100 or better, and the horizontal visual field has to be at least 120 degrees; in NJ, only visual acuity standards need to be met, which is a best-corrected vision of 20/50
- Inform the family and physician about your findings
- Educate the patient regarding driving cessation and alternative transportation sources
Last but not least, let's talk about driving and driving cessation. This is often the elephant in the room. My role as an OT is to inform the family and the physician about my findings. I do not call the BMV or the DMV myself. I let the physician know my findings and then let the physician decide the best plan. However, it is essential to understand the requirements to be eligible for driving in your state. I live in Pennsylvania, where visual acuity or best-corrected vision has to be at least 20 by 100 in the better eye, and you have a visual field of 120 degrees to drive. New Jersey is 30 minutes away from me, and their visual equity standards are a best-corrected vision of 20/50 and no visual field requirements.
Specific Areas Addressed
- Eccentric Viewing
- Bioptic Driving
- Diabetic Management
Here are some other areas that OTs can address but are outside of today's scope.
Summary
Thanks for your time and attention. Feel free to reach out with any questions.
Questions and Answers
If I heard correctly, you said task lighting should be behind the dominant eye, but should be opposite the dominant hand. Where do you place the task light if the dominant eye and dominant hand are the same?
I do not know if you saw it in the picture. You can put the task lighting right next to the paper. Please do not put it behind the shoulder; have the task lighting opposite the dominant hand. Bring it down so that there is enough light on the paper.
Do you perform home evaluations? And if so, how do you bill for that visit and any interventions recommended?
It is billed as an outpatient service like any other regular assessment. I do not come up with the ICD-10 diagnosis myself. The physician comes up with that code, and I get that information from the physician.
Which assessments would be used in skilled nursing facilities?
You can easily do the National Eye Institute Visual Functioning Questionnaire (NEI) in a skilled nursing facility. Make sure that you have a light meter so that you can measure the lighting within the room. It is okay also to use MNRead, the Pepper Test, and the near and distant acuity vision charts.
Do you work with driving assessments?
I am not a CDRS-certified driving rehab instructor, so I never go behind the wheel with the patient. However, I do everything else to prepare them to go behind the wheel.
References
Blaylock, S. E., Barstow, B. A., Vogtle, L. K., & Bennett, D. K. (2015). Understanding the occupational performance experiences of individuals with low vision. British Journal of Occupational Therapy, 78(7), 412-421.
Enoch, J., Jones, L., Taylor, D. J., Bronze, C., Kirwan, J. F., Jones, P. R., & Crabb, D. P. (2020). How do different lighting conditions affect the vision and quality of life of people with glaucoma? A systematic review. Eye, 34(1), 138-154.
Frolov, A., Feuerstein, J., & Subramanian, P. S. (2017). Homonymous hemianopia and vision restoration therapy. Neurologic clinics, 35(1), 29-43.
Lauren O' Farrell, Sandra Lewis, Amy McKenzie, Lynda Jones(2010). Charles Bonnet Syndrome: A Review of the Literature. Journal of Visual Impairment and Blindness, 261-274
Le Jeune, J. (2001). Things I never knew until I married someone with low vision. RE: view, 33(2), 5
McDowell, N., & Dutton, G. N. (2019). Hemianopia and features of Balint syndrome following occipital lobe hemorrhage: identification and patient understanding have aided functional improvement years after onset. Case Reports in Ophthalmological Medicine.
O'connell, C., Mahboobin, A., Drexler, S., Redfern, M. S., Perera, S., Nau, A. C., & Cham, R. (2017). Effects of acute peripheral/central visual field loss on standing balance. Experimental Brain Research, 235(11), 3261-3270.
Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. Am J Occup Ther 2020;74(Supplement_2):7412410010. https://doi.org/10.5014/ajot.2020.74S2001
Şahlı, E., & İdil, A. (2019). A common approach to low vision: examination and rehabilitation of the patient with low vision. Turkish journal of ophthalmology, 49(2), 89.
Smallfield, S., & Kaldenberg, J. (2020). Occupational therapy interventions to improve reading performance of older adults with low vision: A systematic review. The American Journal of Occupational Therapy, 74(1), 7401185030p - 7401185030p18.
Soucy-Moloney, L. A. (1998). Labeling and marking: A rehabilitation teacher's perspective. RE: view, 30(1), 33.
Sunness, J. S. (2008). Face fields and microperimetry for estimating the location of fixation in eyes with macular disease. Journal of Visual Impairment & Blindness, 102(11), 679-689.
Watson, G. R., Wright, V., Wyse, E., & De l'Aune, W. (2004). A writing assessment for persons with age-related vision loss. Journal of Visual Impairment & Blindness, 98(3), 160-167.
Wittich, W., Jarry, J., Barstow, E., & Thomas, A. (2017). Vision and hearing impairment and occupational therapy education: Needs and current practice. British Journal of Occupational Therapy, 80(6), 384-391.
Resources
National Eye Institute: https://www.nei.nih.gov/
R-SRAFVP: https://www.uab.edu/shp/ot/post-professional/low-vision-gc/student-resources
Macular Degeneration Group: www.mdsupport.org/
American Council of the Blind: https://www.acb.org/
American Foundation for the Blind: https://www.afb.org/
National Federation for the Blind: https://www.nfb.org
Library for the blind: https://loc.gov
Physician's Guide to Assessing and Counselling Older Drivers
Low Vision Products: https://www.freedomscientific.com/products/lowvision/
State Commission for the Blind: Various links depending on the state
State Library Talking Book and Braille: https://www.loc.gov/nls/braille-audio-reading-materials/find-a-local-library/
Low Vision Simulators: www.lowvisionsimulators.com
visABILITIES Rehab Services Inc.: www.visabilities.com
Citation
Gupta, S.(2022). Aging and vision: The occupational therapy role. OccupationalTherapy.com, Article 5521. Available at www.occupationaltherapy.com
