Editor's note: This text-based course is a transcript of the webinar, Assessing And Preventing Falls At Home: A Practical Approach For The OT, presented by Krista Covell-Pierson, OTR/L, BCB-PMD.
Learning Outcomes
- After this course, participants will be able to:
- List 3 assessments that can help determine a patient’s fall risk.
- Recognize safety hazards in a patient’s home that may increase fall risk.
- Identify 2 strategies to implement in a patient’s home that will keep them safer from falls.
Introduction
I am excited to be here to talk about preventing falls at home. We all know that falls are a hot-button topic, and we hear it often discussed regarding older adults. However, we can address falls with all ages so keep this in mind. I want to give you practical tips and strategies that you can use right away.
I will start globally and then focus on occupational therapy interventions for this presentation. We will talk about treatment ideas to get your creative minds flowing. We are all trying to do our best quality of care, but it is hard in some settings due to productivity pressures. Thus, some of these treatments may have to be adapted, but I want to give you some things that can be done in quick visits.
I have worked in home care, outpatient, skilled nursing, and hospitals, and currently have a private practice, Covell Care and Rehabilitation, which is mobile outpatient. We have OT, PT, speech, and licensed clinical social workers in people's homes, mainly through Medicare Part B. We serve Colorado all across the front range. I have spent countless hours in people's homes, and fall prevention has been a big part of those treatments.
Figure 1 shows me with my client Delores.

Figure 1. Author with a client in her home.
As occupational therapists, we do some of our best work in a natural context or environment. Even if you do not work in a client's home, you can still take some of these strategies and apply them in your treatment setting. I also want you to walk away with a good understanding of our role in fall prevention care so that this area does not always fall to our physical therapy counterparts. We want to be one of the disciplines that can be referred to right out of the gate when someone falls. We have many skills in the area and need to educate people on these.
Perhaps, you would like to start a private practice. It may seem daunting, but initially, I started doing home safety assessments on the side while I was working full-time in a skilled nursing facility as the rehab manager. So if you are interested in working on fall prevention and home safety, you can certainly do that in private practice.
No matter where you work, I encourage you to reach out to physicians, including neurologists and other specialists, to inform them about our role in fall prevention. You can do that from a management point of view or as an individual practitioner. For example, you can talk to your manager about writing a letter to some of the physicians or present it to your local ED. We spoke with local ER physicians about our occupational therapy services for falls for my private practice. It took us a while to get to that audience, but it was very eye-opening to the physicians there.
You can also present to the interdisciplinary team in your facility. You could start a falls committee, or you can engage on social media about falls. Some of my favorite ideas have been sourced from other therapists on social media. You can share research articles with your team, clients, and referral sources. There are many continuing education courses and certifications in fall prevention.
Keep in mind that September is Fall Awareness Month. This would be a great time to focus on educating others on our vital role. You may be able to team up with other proactive physicians and clinicians to advocate for occupational therapy to be more present in primary care.
I hope that after this talk, you will take the initiative to educate people about fall prevention and occupational therapy.
Fall Statistics
- Millions of people 65 and older fall every year
- 1 out of 4 people fall each year
- Falling once doubles your chances of falling again
- One out of five falls cause serious injury
- 3 million people are treated in emergency rooms for falls every year
- In 2015, the total medical costs for falls totaled more than $50 billion
Let's look at some facts and statistics related to falls as they are staggering and are helpful to share with administrators, colleagues, and clients. Millions of people 65 and older fall every year, and one out of four people fall every year. And once you have fallen, this doubles your chance of falling again. When somebody falls, even if it is a fluke, this should be a warning flag for us. One out of five falls causes a severe injury, like a broken bone, a head injury, or a laceration which usually means people are most likely going to the ER. Three million people are treated in emergency rooms for falls every year. If you can get in front of ER docs, you can see how this can be helpful. There might be some red tape to access the ER and physicians but keep at it.
In 2015, the total medical costs for falls totaled more than $50 billion, of which Medicare and Medicaid shoulder most of those costs. Thus, falls are an expensive piece of healthcare.
- Falling can cause fear of future falling
- Falls are the most common cause of TBI
- 32,000 deaths occur each year due to falls
- 300,000 people sustain a hip fracture due to falls
- Women fall more than men
- Every second of every day, an older adult suffers a fall in the US
We know that falling can cause a fear of future falling, increasing people's fall risk. I will talk more about fear concerning falls and what we can do about that later in the talk.
Falls are the most common cause of traumatic brain injury, and 32,000 deaths occur every year from falling. We want to help bring that number down, even by one. If we can prevent one fatal or terrible fall, let's do that. Additionally, 300,000 people sustain a hip fracture due to falls annually. Many of these make up our OT caseloads.
Every second, an older adult suffers a fall in the United States, and these are women more than men. By the end of this presentation, 120 older adults will have fallen just to bring that statistic alive for you. You can even use this as a reference for your clients. We want to educate people about the fall statistics and the resultant problems even if they are doing well.
Why Should OT Be Involved In Falls?
- Less than half the people tell their doctor when they fall. Conditions that contribute to falling include:
- Lower body weakness
- Vitamin D deficiency
- Medications
- Vision problems
- Foot pain
- Poor footwear
- Home hazards
The big question is, why should an occupational therapy professional be involved in fall prevention? I did not share the fall statistics to scare you or sensationalize the issue, but these numbers should be part of your client and clinician education so that they can see the impact. Again, if this presentation helps one person, it is worth it. Less than half the people tell their doctor that they have had a fall. We are fortunate as therapists that we get to spend so much time with our clients and can establish rapport and trust. So if a patient does not tell you right away that they have had falls, this information may be shared over time. We need to massage those conversations so that revealing fall information does not appear to be a checkmark on their record. Many people fear what it means if they tell their healthcare professional that they have had a fall.
Some of the conditions that contribute to falls are lower body weakness, a vitamin D deficiency, certain medications, including those over-the-counter, problems with vision, foot pain, poor footwear, and home hazards. We are skilled at activity analysis and equipment recommendations. Thus, the home hazard piece certainly falls in OT's wheelhouse.
- According to the AOTA, “Occupational therapy practitioners possess the critical skills needed to address fall prevention with older adults.”
- Skillset includes:
- Reviewing the context
- Evaluating client limitations and strengths
- Interventions targeting improved abilities
- Modifying homes
- Changing patterns and behaviors
Beyond the fact that we are already in the picture and assessing these things, the American Occupational Therapy Association (AOTA) and other credible sources say that occupational therapy practitioners possess the critical skills needed to address fall prevention with older adults. Print that out and hang it up in your rehab gym or home care office or use it in your marketing to physicians.
Based on research, the AOTA says that falls are multifactorial. Falls are influenced by conditions within the individual, the environment, and the interaction between the two.
The most successful fall prevention initiatives use multifaceted approaches. OT practitioners are skilled at evaluating and addressing influences from the person, their activity, roles and routines, and the environment to maximize independence. We link the client's goals and priorities with modifications and adaptations that support their ability to participate in meaningful activities. This is the hallmark of occupational therapy.
Many times facilities have a falls team, but often occupational therapy is not represented. It would be beneficial if OT and PT were both automatically referred in fall cases, and sometimes we have to educate our interdisciplinary teams on that. Often, people fall because they are doing things that are meaningful or everyday tasks, and we can work on that. I have a personal example of that. My mom was at my house when I was out of town. My dog had an accident on our rug in the front room. She went outside to clean it and fell. On the same weekend, she fell over a baby swing on the way to the bathroom because it is not usually there. She had two falls on the weekend doing things that were regular tasks. We had to go back to clear pathways. We can review the context of the fall.
We already look at limitations and strengths, but now we need to look keenly at what caused the fall. My mom can continue to take things outside to clean or carry heavy items, but we need to ensure that she is doing that safely. We already modify homes and are good at changing patterns and behaviors.
OT's Unique Skill Set
- Holistic
- Focus on meaningful occupations
- Adaptable
- Client-centered
- Educators
- Trusting relationships with clients
- Access to equipment
- Creative
- Medical knowledge
- Client advocates
OTs tend to use a holistic approach and focus on meaningful occupations. We are adaptable, and we do not want to give cookie-cutter recommendations regarding fall prevention. As a discipline, we are client-centered and educators by nature. I have met many occupational therapy professionals who wanted to be a teacher before finding occupational therapy. We can educate our teams, patients, and families and develop trusting relationships with clients. We can be creative with our treatment and use equipment if needed. Everybody that works in the skilled nursing or hospital setting knows what is in an OT closet. And if we do not have something to use, we can typically figure something out or tap into loaner closets or DME providers. We also have a lot of knowledge about how to adapt the environment. A client with multiple sclerosis versus someone with Huntington's disease will have different needs, and we need to bring in our medical knowledge to intervene. Lastly, we are client advocates. We could give the same checklist to every patient we see, but that is not good enough. We advocate for what each client needs.
- Assessment of intrinsic factors
- Assessment of extrinsic factors
We look at both intrinsic and extrinsic factors. Intrinsic factors include weakness, impaired balance, impaired cognition, urinary incontinence, sensory impairments, a fear of falling, and the effects of the medications. We also assess extrinsic factors in the environment like throw rugs, loose carpets, lighting issues, pets in the home, uneven walkways, broken stairs, and the need for equipment like sliding boards, grab bars, and handrails.
Home Assessments and Fall Prevention
- Person-Environment-Occupation-Performance Model (PEOP)
We also want to assess using the PEOP model, or the Person-Environment-Occupation-Performance Model. It is a systems model and views the function of a person in the system as a whole. It considers the interaction between the three components that make up occupational performance. I will come back to this model in a minute, but I want to give you some examples first, as shown in Figure 2.

Figure 2. Examples of home assessment.
Again, we are looking at the person, environment, and occupation, and I want you to envision yourself in the overlapping place in the middle (Figure 3).
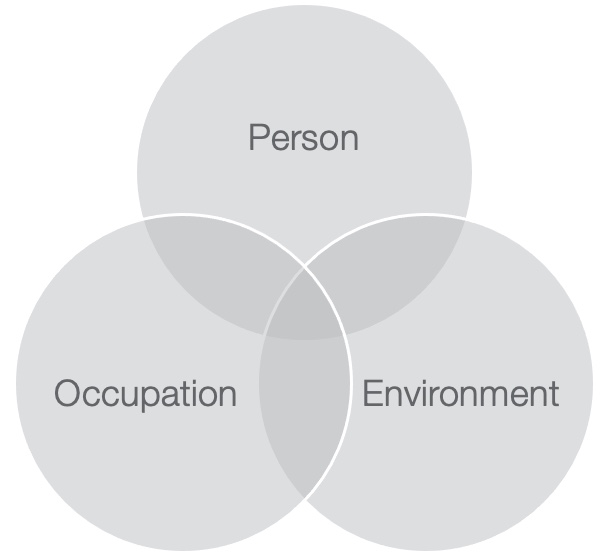
Figure 3. PEO model.
I am going to use the example of Delores again. I looked at physiological, psychological, motor, sensory perception, cognitive, and spiritual issues. You can see in Figure 2 that I am sitting in Delores' power wheelchair. You can also see a reacher attached to the handrail, oxygen, and her electric recliner. Delores had advanced ALS that was impacting her across the board. She had a solid faith, but she was also struggling with some deep grief due to the loss of a family member in a tragic accident. Her motor components were impacted by ALS and were changing very fast, one of the most rapid cases I have ever seen. Every day, I felt like she was dealing with different challenges. Cognitively, she was sharp as a tack and lived alone.
We looked at her environment. She lived in public housing with a strong neighborhood community, but she did not like asking for help from her neighbors as many had health issues. We had to look at other social supports like her church, her family, and a non-medical home care agency. We also had to look at the low-income housing policies to ensure they supported changes. Another thing to look at is assistive technology. When I first started as an occupational therapist 20 years ago, this was not something that we looked at regularly, but now many use tablets, computers, and smartphones. Delores also had advanced rheumatoid arthritis, but she could use a cell phone and tablet reasonably well, so we could incorporate that into her care plan.
These two pieces support her occupations that we can further assess related to fall prevention. We had to look at what was important to her. One thing she wanted to do was get to the bathroom on her own to manage her bowels. This was a big challenge and a red flag for fall prevention. She also wanted to complete shower transfers with her CNA. She identified coloring activities to keep her hands busy and help her mental health and depression. We had to make goals that impacted her, the environment, and her occupations and make sure they all fit together.
We had to start picking some things apart regarding fall prevention, like her risks from sitting in the recliner, reaching, bending, and transferring in and out of the shower. Getting into the shower was not a big deal for Delores, but getting out was more problematic. I also had to consider things when it came to her bowel routine. The PEOP model is very client-centered and can help us analyze a complex situation. You can even write that diagram with your client and start filling things in the circles. Their goals are going to go right in the middle.
Even if you are not seeing a patient specifically for falls, fall prevention needs to be on your radar. This does not mean that you have to be rigid and exact with your questions or use the same assessments. Clients do not want to talk about falls because they are never sure what that will mean for them. So you can ask them some sly questions and get some good answers about their fall risk. "Do you ever lose your balance when walking with your walker?" Or, "Do you ever trip over these items in the hallway?" "Have you ever slid or almost slid off the side of your bed?" They often say they slid off something but "did not fall." It is essential to focus on rapport and build trust with your patients.
Person
- Person (aka Patient):
- Ask questions with all assessments
- Focus on rapport building
- Be a detective
- Use activity analysis
- Regularly ask yourself, “Could this contribute to falls?”
Looking at the model, we are going to start with a person. It is great to have a mental checklist or a cheat sheet. I will give you an example of a male patient standing in his kitchen in Figure 4.

Figure 4. A client standing in a kitchen.
It may not be glowingly evident that he is at risk for falls. He has a cup in his hand, has an upright posture, and not using any assistive device. In this quick snapshot, he looks pretty good. You need to be a detective and look through the patient's medical record to find all the warning signs.
He is a 78-year-old male, so automatically, he is in a high-risk age category. He has had a history of two cardiac ablations and AFib, which means he has heart palpitations and fatigue. I could ask him questions like, "Do you feel different when you're having that dizziness or wooziness, and do you feel like it could contribute to a fall?" "Do you ever think your knees will buckle, or you need to lay or sit down?" Additionally, he has neuropathy in bilateral lower extremities, a potential fall risk indicator. And impacting his center of gravity is kyphosis, but the spinal deformity may not be a big deal except when added to other factors. He also has cataracts in both eyes and has not had surgery yet. This could contribute to falls. With osteoarthritis, he is more at risk for an injury if he has a fall. Medical history also tells us he has chronic pain in the left hip due to bursitis that he is managing with over-the-counter medications and a stretching program from physical therapy. We can ask more questions about how therapy is affecting him. Can he get up and down the stairs when his left hip is bothering him.
He lives with his wife, who is pretty active. What do they like to do together? He is also alert and oriented times three. We will talk about cognition in a little while. He uses a walker only when his hip is hurting, but we also want to see if the walker contributes to falls.
He is also a semi-retired realtor. Is he driving around in the community? Is he going in and out of other people's homes? How does that contribute to his potential fall risk? We always want to ask a person if they have a history of falls. If so, we want to know if it was night, whether they were carrying packages, etc. We want to analyze the information to see if there is genuinely a fall risk.
Medicare has a red flag system to indicate if someone is a fall risk. If they have one fall with an injury or two or more falls without an injury in the last year, they are a fall risk. Falls may also be listed in the medical record.
Environment
- 1 in 4 people will fall on the stairs
- 13% injured in bathrooms
- 31% fall in the living room
- 23% fall in the yard
The next thing we want to do is tackle that environment. Where do you think that most people fall? Here are the statistics. Every year about one in four people over the age of 64 will fall on the stairs, 13% of older adults are injured in the bathroom, 31% take a tumble in the living room, and around 23% fall outside. So these are all places where we should be assessing our patients.
If you see somebody in a skilled nursing facility or a hospital, you may have to simulate the situation at home. When I worked in the hospital, we would often go down to the day room where patients' families would hang out because there was more typical furniture there versus the real rigid furniture in a hospital room. In a home environment, we need to think about the type and arrangement of furniture, any clutter, and the time of year. Patients' houses get dark earlier in the winter. They may also have holiday decorations that we need to consider. They may have Amazon boxes being delivered. There are a lot of moving parts in the environment.
Other considerations are rugs and nightlights. It is hard to have time to assess everything. Perhaps a checklist can be given to patients and families to do independently. Or, if you are going to do a home assessment, maybe you have them do a checklist before that to be as efficient as possible when you are there. Some other things to consider are looking at the outside on the left in Figure 5.

Figure 5. Home assessment examples.
This client likes to spend time outside, and he also needs to access his upstairs bedroom. At the same time, it is essential to look at the common areas like the family room and the kitchen. One of your goals could be that the patient will participate in an additional fall prevention assessment in the XYZ area of the home. For this gentleman, he had a long driveway to get up into the house with a mailbox at the bottom. In the left photo, he is going to get his mail. He is also still taking his garbage cans up and down the driveway. The critical thing for an occupational therapist is to make sure that these tasks are safe, so you would want him to show you how he does all these daily tasks. You do not have to mention that you are assessing him for falls, but you are looking at these tasks through a fall prevention lens.
Take a look at different stairs in the house or outside and whether they have handrails. Make a note of safety concerns as you go. At the end, you can say, "I noticed some things that might be contributing to your fall risk. I'd like to go over them with you." Examples are throw rugs. Some of our patients do not want to move their rugs or put double-sided tape underneath them. It is important to explain why this is important. You may even show them the difference between walking with a walker without a rug. If somebody has had a rug in the same place for a long time and does not want to move it, make sure they keep the same rug. Changing to a rug of different width or height can be a fall risk. Look at the rooms that they use the most often. If the master bedroom is on the main floor, that is great. If there is a transition from carpet to hardwood, have them show you how they manage this.
Remember, our gentleman has cataracts. Is there any glare from the lights? How is that light being filtered at different times of the day? Does this change in lighting contribute to a fall risk? As he is a semi-retired realtor, let's go to his office to see how it is arranged or if it is cluttered with paperwork. Let's see how he maneuvers in and out of different areas. We need to hunker down in these environments and ensure that this patient is safe.
I talked to an occupational therapist who works for me this morning, and we spoke of home evaluations. He gives his patients many handouts about fall prevention and disease management, which is excellent, but he also needs real-time, hands-on, environment-based treatments. We cannot just stop at education.
Going back to my client, he has a walk-in shower. I had him step in and out and observed what he needed to grab. Is he safe? He also goes into the pantry a lot even though his wife cooks. Can he turn around in the pantry safely? Is he holding on to shelves? Does the client furniture surf to move around? There are many things we can investigate when it comes to the environment. And this brings us to the last circle, which will be occupation.
Occupation
Going into my patients' homes is one of my favorite parts of being an OT. I love to see how people live and have learned about different cultures and ways of doing things. When I first became an OT, I could not believe how many different ways to brush your teeth. People do things differently, and we have to be respectful of that. And it enhances our practice of working with a variety of people to add things to our toolbox.
If a client lives in an apartment complex that is ADA compatible, do not automatically assume that it is safe. The Americans Disabilities Act became federal law in 1992 and has codes so that people with a disability related to sight, hearing, or movement have the same advantages as an able-bodied person. I have a patient with spina bifida, and she lives in an ADA-compliant apartment. However, this does not mean that it is safe for her. We had to make many changes so that she could be independent.
- Go into the home
- Review photos
- Work together on drawings
- Consider your patient and the environment
- Use videos
- Consider video calls/visits
- Simulate real life
If you cannot go into the home, ask the client or family members to send you photos, draw things, or take measurements. Try to simulate the setting as best as you can. I have even taken two by fours before to simulate shower ledges to step over. You can also have your client or their family provide videos. We did a lot of home safety and fall prevention assessments via video calls during COVID. There are photographs sent to me from patients in Figure 6.

Figure 6. Examples of different bathroom set-ups.
A clawfoot tub is an OT's worst nightmare. This was a bathroom set-up for me to navigate because the family did not want to get rid of it. How can we make this as safe as possible? The bottom left-hand picture is a drawing that I sketched based on my client's description. She wanted to be able to sit and stand in the tub. We brainstormed together. Then, her son sent some videos and measurements of the actual bathroom so we could sit down and do some more exact drawings.
- Let the patient guide the visit
- Stay away from canned recommendations
- Go beyond the basics
We want the client to drive the visit. We have to figure out what will be the safest version with the situation that we have. If you have a patient with tripping hazards but they refuse to make any changes, you have to figure out ways to manage them while also educating the client about safety concerns. Stay away from those canned recommendations. I see this a lot with occupational therapy practitioners. We tell them everything they need to do. Instead, we need to be a little bit more creative and go beyond the basics to make an impact when it comes to fall prevention for our patients.
Assessments
Use good clinical reasoning when selecting your assessments because you want to accurately find the deficits to guide your treatment plan and provide evidence to third-party payers. Assessments can also be a great teaching tool for patients. Take the time to go through an assessment so that they understand the score. There is nothing worse than getting an assessment from a healthcare professional and then they do not talk to you about it. Talk about the results with them. "You did great on this assessment, but there are a couple of areas of concern."
The American Occupational Therapy Association says the following about choosing an assessment. An assessment provides the most valuable information for addressing your client's home modification or home safety needs. The evaluation also needs to apply to your particular patient or situation. My client is semi-retired. We would use a different evaluation for him versus someone in the end stage of Parkinson's disease. Assessments should look at both intrinsic and extrinsic factors. Lastly, we want an assessment that is standardized and valid.
- In-Home Occupational Performance Kit
- Safety Assessment of Function and the Environment for Rehabilitation—Health Outcome Measurement and Evaluation (SAFER HOME)
- Home Falls and Accidents Screening Tool
- Westmead Home Safety Assessment (WeHSA)
- Rebuilding Together’s Safe At Home Checklist
- https://www.aota.org/-/media/Corporate/Files/Practice/Aging/rebuilding-together/RT-Aging-in-Place-Safe-at-Home-Checklist.pdf
In-Home Occupational Performance Kit (I-HOPE)
The In-Home Occupational Performance Kit is also called the I-HOPE. It targets activities performed in the home, specifically those aging in place. The purpose of the I-HOPE is to measure the effects of the incompatibilities between the person's abilities and the environment. The I-HOPE measures clients doing their in-home activities and observes changes in the person-environment fit. Hopefully, after doing our treatments, we will see a better fit. It also offers a psychometrically sound assessment of daily activities that considers the client's perspective and satisfaction, which is also key. It considers activities that are meaningful to the client and acknowledges the role of the environment on performance. This assessment comes from the Participation, Environment, and Performance Lab because there were not a lot of evaluations that looked at the environment. Again, this is why occupational therapy needs to be there because we incorporate the environment into fall prevention practices.
Unfortunately, this assessment does require training and the purchase of supplies, but the training is an opportunity to grow as a clinician.
Safety Assessment of Function and the Environment for Rehabilitation—Health Outcome Measurement and Evaluation (SAFER HOME)
The next one is called the SAFER HOME, Safety Assessment of Function and Environment for Rehabilitation, Health Outcome Measurement and Evaluation. This assesses an individual's abilities to safely manage functional activities within the home, considering the environment and the client's capabilities. It covers 97 items within 14 sections and includes their living situation, mobility components, kitchen set-up, fire hazards, eating, wandering, memory aids, and an overall general assessment. Fall prevention can be figured into a lot of those pieces. It is designed for older adults, and you can use it with people that do or do not have cognitive impairments. This is key as some assessments are not sensitive to people with cognitive impairment. It takes about 45 minutes to 90 minutes to complete, so it is manageable within a treatment. Ninety minutes is most likely getting a little bit outside of what you can do, but it would be great if you could get it to 45 to 60 minutes. You can buy the SAFER tool online from various vendors.
Home Falls and Accidents Screening Tool
The Home Falls and Accidents Screening Tool (Home FAST) is free and designed to identify older people at risk of falling because of hazards in the home. The tool consists of 25 items, and the higher the score, the higher the risk of falling. It is pretty quick to administer.
Westmead Home Safety Assessment (WeHSA)
The Westmead Home Safety Assessment (WeHSA) identifies fall hazards within clients' homes and was originally developed for older adults. It is a 72-item checklist that assesses internal/external traffic ways, the general indoors, the living areas, seating, bedroom, bathroom, kitchen, and laundry room. Many falls can happen in the laundry room because of the dynamic movements in that space. This assessment also looks at footwear and medication management, which are significant contributors to falls. You go through those categories and rate them as relevant or not relevant for the patient. You also deem them as hazards or not. It was developed in Australia, takes about 60 minutes to complete, and there is a cost.
Rebuilding Together’s Safe At Home Checklist
Rebuilding Together's Safer At Home Checklist is from Rebuilding at Home. I suggest that you look them up as they are pretty interesting. They focus on safe homes and communities for everyone, which aligns with us as occupational therapists. They also have contracts with many national partnerships like the area agencies on aging, AARP, American Occupational Therapy Association, the National Association of Home Builders, and the National Council on Aging. This checklist identifies home safety, fall hazards, and accessibility issues for the homeowner and their family members. It is also an excellent talking tool to use with patients that you can fill out with them. These are all function-based assessments. Now, we are going to look at more balance-related assessments. These assessments look into more of the components that contribute to falls.
- Timed Up and Go (TUG)
- The Activities-specific Balance Confidence (ABC) Scale
- The Falls Efficacy Scale International (FES-I)
Timed Up and Go (TUG)
The Timed Up and Go is a straightforward, reliable test widely used. Physicians recognize this tool, so if you send the results to them, they will understand what you are telling them. It looks at the dynamic balance of the participants. It measures the time in seconds that it takes a person to stand up from a chair, walk three meters, and come back and sit back down again. It identifies patients at risk for falls and can be done in most environments. Sometimes, there can be some limitations depending on how large the home environment is or the amount of clutter in the home.
Activities-specific Balance Confidence Scale (ABC)
The next one is the Activities-specific Balance Confidence Scale known as the ABC. This is self-administered as it is designed for the patient to fill out. I go over this with patients in my setting because I do not have a front desk person or a rehab tech. Sometimes my patient cannot do it ahead of time, so I do it with them. It is a structured questionnaire that measures an individual's confidence in performing activities without losing their balance, as we know balance is a significant contributor to falls. There are 16 questions about tasks where they rate their confidence. The questions include walking around the house, going up and down the stairs, sweeping the floor, walking across a parking lot in the mall, stepping on or off an escalator while holding packages, and getting in and out of the car. The ABC is scored from zero to a hundred percent, and then as the patient has confidence, it goes up by 10% increments.
Falls Efficacy Scale (FES)
The last one I have listed here is the Falls Efficacy Scale. It is a short tool that records the fear of falling. This is an area that occupational therapists and other healthcare professionals rarely address. Fear of falling needs to be addressed as it is a vital piece of the puzzle regarding fall prevention. You can either do a seven-item or 16-item questionnaire, depending on if you do the short or long version. They rate items on a scale of one to 10, with one being very confident and ten not being confident. Items ask about taking a bath, reaching into cabinets or closets, walking around the house, preparing meals that do not require carrying heavy objects or hot objects, getting in and out of bed, answering the door, getting in and out of a chair, and getting dressed. It addresses the ADLs that we are already assessing, but it also talks about the fear that goes with them. You can have a patient that has never had a fall, but they might be afraid of falling, so it is essential to know that.
Addressing Fear of Falling
- Take your time
- Identifying successful transfers and movements
- Ask questions about how the patient feels
- Stop during tasks to reduce anxiety
- Deep breathing
- Visualization
- Demonstrations
- Step-by-step
- Trouble-shooting
There can be a lot of different reasons for fear of falling. Fear is an emotion when there is a threat of harm. It can be physical, emotional, or psychological. You may have a patient that has had multiple falls and another with zero falls, but they are imagining falling. Their mom may have had falls and ended up in a terrible facility. Fear can be a helpful emotion because it helps to keep us safe. There is nothing wrong with being afraid, and you can tell your clients that. However, we need to learn how to cope with the fear and understand when there is genuinely a threat.
The Falls Efficacy Scale is a great conversation starter, and then you can move into some of the more sensitive, vulnerable areas for your patients. You also want to talk about the intensity of the fear. When do they feel afraid? Are they afraid every single time they get up? Or are they just scared when they walk on ice or in a particular location where they fell in the past? The goal is to reduce the fear, and when you tell your patient that, they are typically open to that. The patient is going to need professional guidance. "We will practice some situations together to make you feel more confident on your own. Would you like to do that?"
You can also discuss how the fear manifests. This could be tightness in the chest and/or an anxious feeling like they need to sit down. You want them to slow down and take their time. You want to be respectful of how they feel about their fall risk and talk to them about it at the beginning of each treatment. "I want to know how you feel about your shower transfer since our last visit. Be honest with me so we can work on it together. And, at the end of our session, I hope that you will feel less afraid."
I like to also educate clients about deep and diaphragmatic breathing. I use this a lot in my treatments if a client is anxious at the beginning, as it helps them to concentrate. I worked with a patient that had an amputation, and he was terrified of falling, rightfully so. We did a lot of deep breathing at the beginning of his treatments because if I jumped right into treatment, he was very impulsive and much more likely to fall. He would grab at things, move quickly, and forget to set himself up correctly. We started with deep breathing and moved into some visualization. This can be helpful, especially if your client has had an accident at home. Research shows that doing bicep curls along with visualization increases motion and strength. So if somebody can visualize how they are going to go from the bed to the wheelchair safely and step-by-step, this can help them be a lot more successful and manage that fear.
The other thing that can help is demonstrations. If somebody is fearful of getting in and out of the tub, show them the steps and the placement of your hands before they try. "Now, I will put my right hand here and my left hand over here. Then, you can even ask them to talk you through it the next time. They can also give you step-by-step instructions while you do the demonstration. This can help to decrease the fear of falling.
Collaboration
- Collaborate with your team
- Review other disciplines’ assessments
- Discuss findings
- Review fall analysis with one another
- Communicate with the physician
Collaboration is a big part of what we do as occupational therapists. It is good to find out what is going on within the team, like the client's gait speed and lower extremity strength. Occupational therapists can assess lower extremity strength, but we tend to look to PT. Talk to your team about what you are working on with falls. Remember, AOTA says that fall prevention has to be multifactorial in what we assess and what we provide. Thus, you cannot use just an OT lens. Perhaps the PT focuses only on PT stuff. Let's get in there and make them work with you. Education and advocacy can be used in the interdisciplinary team as well.
If PT is not working with your client, I encourage you to consider integrating the 10 Meter Walk Test and the 30 Second Sit to Stand Test into your assessment. If it is indicated, you can also get a PT referral. Sometimes PT may have already been discontinued, but we might need to get PT back in the picture if needed. Advocate for that because collaboration is going to help our patients. OT can be the one that identifies the different types of fall risk issues like increased medications or decreased cognition. You can talk about that with your IDT and get the right people involved. And if you are addressing falls and other people are addressing falls as well, listen to them as that is the way to be a successful OT. We know that two brains are better than one, and it is also a great way to track outcomes. Make sure that you are talking about that with your team. If you start seeing many people who have had falls, start tracking that and see how you can be successful as a team.
The last thing is to communicate with the doctors. Often, we do not communicate with doctors because we think they are too busy. We have to change our mindset and think the doctor wants to hear from us. You can do this by faxing, calling, or stopping by in the hallway to talk to them. Most doctors want to know because they are trying to mitigate people's fall risks at home, and we can help them do that. If they see that you are doing that too, you are more likely to get more referrals from that doctor.
Cognition and Falls
- Screen cognitively impaired patients for fall risk
- Gait speed
- Balance impairments
- Depression
- Research suggests physical exercise and cognitive training reduce fall risk.
There is a correlation between cognitive impairments and fall risk. When a patient has dementia or cognitive impairment, we do not always automatically think to address that person's fall risk because they are moving around quite well. When I worked in a skilled nursing facility, I watched a patient climb over a six-foot fence. He was angry at his wife and had delusions about where she was spending her time, so he climbed the fence to get out of the courtyard and landed his feet on the other side. Physically, he was doing quite well, but I want to be sure that as OT professionals, we are advocating for our patients that have cognitive impairments to be screened by OT for fall prevention even if they are moving well.
Research supports this as older adults with dementia fall more than healthy older adults. I do not think this is a surprise. However, it might surprise you that people with dementia who do not have Alzheimer's are more likely to fall than patients with Alzheimer's. People with a non-Alzheimer's type dementia were 64% more likely to fall, while people with Alzheimer's disease had a 50% increase in their likelihood of falling. Older adults, in general, have a 25% increased fall risk versus their cognitively impaired counterparts. For those non-Alzheimer's dementia patients, make sure you get involved with them. Sometimes I think we group people into the Alzheimer's type too often, and we have to remember that these dementias are different.
Research also shows that it is not the memory impairment that causes an increased risk for falls, but rather it is the decline in executive functioning. OTs certainly have the skills to address executive functioning. We also know that there is a close connection between gait disturbances and cognitive decline. A decline in somebody's gait pattern is typical for neurodegenerative diseases like Alzheimer's and can be a biomarker for dementia. If we think about this in layers, cognitive impairment leads to higher fall risk, and then on top of that, the gait changes come, which also increases fall risk. The impairments in executive functioning and gait pattern are double whammies for this population. Again, this is an excellent opportunity to work with the team, especially PT. We can address executive functioning through compensatory strategies, and PT can address gait training. The rest of the team can support this treatment.
On top of working on executive functioning via compensatory or restorative techniques, and gait training, we also know that overall strengthening helps reduce people's fall risk. We want to use evidence-based strength training through exercise groups, restorative nursing, and community programs. You should include gait, strength, and executive functioning on your checklist. Again, we may not be assessing and changing things related to gait, but you should be interacting with your PTs and getting that information to include in your treatments.
We want our treatment to be a multifactorial approach. Falls can be overwhelming because we have to look at all these different areas. Balance impairments are key for fall prevention for people with cognitive issues. Depression also adds to cognitive impairment. When a client does not initiate ADLs and is not getting up, this leads to weakness and decreased confidence to do things. They may not do things as well as they usually would.
Cognitive Assessments Related to Fall Prevention
- Dementia
- MCI
- MoCA
- Memory
- Executive function
- Attention
- Language
- Abstraction
- Naming
- Delayed recalls
- Orientation
- MoCA
There are many areas that we need to address regarding cognition and fall prevention. Many of us see patients with dementia regularly, but we cannot forget about people with mild cognitive impairment. For the OT professionals that may need a quick snapshot of mild cognitive impairment versus dementia, MCI is relatively common in older adults. You have probably seen folks with mild cognitive impairment, but maybe you do not see that diagnosis in their chart. It can lead to dementia, but it does not always, and we also do not see significant errors in their thinking the way we do with somebody with more advanced dementia. Mild cognitive impairment can go undetected for a long time. We are in a pivotal position to communicate our concerns to physicians as patients can sometimes rally a little bit when they are with their physicians. And typically, physicians are focused on physical issues like back pain, incontinence, pending shoulder surgery, and all those things.
If you are seeing mild cognitive issues in your clients and they are at a higher risk for a fall, I encourage you to try the Montreal Cognitive Assessment, MoCA, a brief 10-minute assessment. It is one page with 30 items, but it looks at things that can indicate mild cognitive impairment like impaired memory, executive functioning, attention, language, abstraction, naming, delayed recalls, and orientation. The MoCA is widely used and used internationally. You can then send the results over to the physicians. OTs can take the lead in falls assessment for clients with mild cognitive impairments because I guarantee that this area is not being addressed.
How to Write Fall Prevention Goals
Fall prevention goals are an essential part of our treatment plan. The goals we pick will guide our treatment. For example, we do not want to tell a client that has AFib and uses a walker 30% of the time that he needs to run a marathon. Goals need to be obtainable and appropriate. Fall prevention is no exception.
- At least one of the goals needs to be functional
- Using a score in a goal helps to show progress
- Goals can be caregiver based as long as other goals are patient-based
- Include an anticipated goal completion date
- Include at least one long-term goal
- Consider using several trials to demonstrate mastery
- Include baseline performance
Here are some general guidelines for strong goal writing. At least one of your goals needs to be functional. They cannot all be impairment-based and refer to strength, range of motion, or how they scored on a test. I will show you how to make your goals a little bit more functional in the next slide or two.
Using a score in a goal helps to show progress. If somebody has 50% of confidence and we want to increase that, then maybe our goal is 60%, 80%, or whatever is going to be most obtainable and appropriate for your patient.
You can write a caregiver-based goal, but you also have to have patient-based goals. I was always taught that I could not make goals about caregivers, but you can have one and might have to be creative with how you write it.
You should include an anticipated goal completion date. Is it going to be two weeks or two months? You also should include one long-term goal. If you know that you will be seeing a client and their certification period goes to 12 weeks, but you are planning on seeing them longer than that, your long-term goal can go past your certification date. This is also true when you are doing a maintenance program for fall prevention. You can make a long-term goal six months down the line that your patient will not have any decline related to their shower transfer or walking to the mailbox. We are taught that short-term goals lead to a long-term goal, but many third-party payers do not care about the client's short-term goals. They want to know the long-term goal, so make sure you have those in your documentation. You always want to follow what your employer is recommending for your documentation, but if you are not sure, take this information back to your employer and ask them to show you what you need to include in your documentation.
An excellent way to show mastery of a task is to do several trials. If they can do a transfer one time in the morning, that is great, but maybe you need to make the goal that they can do it three out of three times consecutively in the afternoon. Make those goals good and measurable. Always include your baseline performance, so we know where your patient is coming from and where they are headed.
- Patient will complete a fall assessment in his yard within the next two weeks in order to identify safety concerns.
- Caregiver will demonstrate independence with setting up the wheelchair, front-wheeled walker, and gait belt at the bedside with the patient in order to transfer the patient safely to and from the bed.
- Patient will demonstrate good safety entering and exiting the home from the front door 5/5 trials without verbal cues independently.
- Patient will safely step into her new walk-in shower with appropriate hand placement on grab bars with 0 verbal cues with CGA 3/3 trials.
- Patient will report improved confidence in IADL as evidenced by improved score from 50% confidence on the ABC to 70% confidence within 4 weeks.
I am going to give you some examples of goals. Remember, if your assessment suggests that your patient is at risk for falls, even if you are in there for other reasons, make this part of your treatment plan. For example, we do a lot of wheelchair assessments at Covell Care. If the client is at risk for falls when they are toileting or getting out of bed in the morning, I need to address that even if I am only there for the wheelchair. I need to get that into my care plan and make the goals excellent and solid.
An example is that patient will complete a fall assessment in his yard within the next two weeks in order to identify safety concerns. You can write in your documentation that due to time constraints at the evaluation, you could not go out in the yard or that you needed to address showering first. However, the yard is a concern because that will be part of the long-term goal as the patient is going to be out in the yard doing gardening. We can also say that a kitchen assessment was the only thing completed due to a patient's tolerance. The goal would be to go out in the yard, the bedroom, or wherever the next time. This all needs to be part of the assessment and documentation as these goals are client-based. If there are risks involved and you have not been able to get out in the yard or to another area, make sure you are at least providing education. Let's say somebody just got home from a skilled nursing facility (SNF), and they want to make their breakfast this week, but you have not been able to address it. Ask them to get assistance until you can come back. Educate them on your concerns, and then you can plan to do this in a few days. Time constraints can be a big thing for your treatments, but you have to address them the best you can and keep your patients safe. Safety is the number one goal, no matter what treatment you provide.
An example of a caregiver goal is, "Caregiver will demonstrate independence with setting up the wheelchair, front wheeled walker, and gait belt at the bedside with the patient in order to transfer the patient safely to and from a bed." It is a caregiver-based goal, but it is related to the patient. You can even take that patient out of the picture and say the caregiver will demonstrate this so that when the patient wakes up, he can get in and out of bed easily. Now, remember you cannot extend a patient's care because you need to provide more education to the caregiver. However, as long as you address things with the patient, you can continue to address things with the caregiver. "Patient will demonstrate good safety entering and exiting the home from the front door, five out of five trials without verbal cues independently." There are our trials. We can also make this more functional by adding "in order to" at the end of the statement. Why does this person need to get in out of the front door? This may seem crazy to you to add this because everybody wants to get out of their front door, but a third-party payer may ask this question. Or, "Why can't they just go out of the garage?"
We could add in order to retrieve his mail, get into an Uber, go to the store, or sweep the front porch. Here is another one. "Patient will safely step into her new walk-in shower with appropriate hand placement on grab bars with verbal cues and contact guard, three out of three trials." Or, "Patient will report improved confidence in IADLs, evidenced by an improved score from 50% confidence on the ABC to 70% confidence within four weeks." Make sure that you repeat those assessments you used at the evaluation to show progress. If your assessments are not showing improvement, this does not necessarily mean you have to discharge. Still, you do have to have documentation in there to explain your clinical reasoning to continue with the patient or why the advancement of their progress has been delayed.
Demonstrating Skill When Writing About Falls and OT
- Report what the patient does during treatment
- Focus the note on the skilled interventions provided
- List levels of assistance provided and why it requires an OT
- Write what risks are present without OT
- Help the reader see your interventions
- Explain the rationale
- Tie the interventions to the patient’s medical condition
- Document communication to the doctor
- Include caregiver education and training
- Attach assessments to the patient’s record
- Repeat assessments throughout the treatment plan
Report what the patient does during treatment. OTs are good at reporting the level of assistance someone needs, if they are at risk, what they worked on that day, what adaptive equipment they have, and what they did during the treatment session. Perhaps you practice shower transfers for a full hour. What most OTs need to do better is focus on what they are doing. What did you do as an OT for fall prevention that is important? The patient got in and out of the shower, but what did you do? Did you provide education or verbal or tactile cues? Did you assess for pain? Did you demonstrate a safe way to do it and then provide step-by-step instructions that they were able to return? Did you train the caregiver? Not including the skilled language in your note leaves out the most critical piece of what you are doing as an occupational therapist. A third-party payer reviewer will probably not validate what you did and can take the money back from the company.
Additionally, the referral source that referred that patient to you for fall prevention will not see what skilled service you are providing. If you practice getting in and out of the shower with the client, could the wife have done that with them? You need to tell them what you are doing as the OT. OTs are not the best at tooting their horn, but we need to improve our documentation so that we are not undervalued in our role in fall prevention and risk nonpayment for our services. Again, this also limits possible future referrals because doctors, nurse practitioners, and PAs will not see "skilled" treatment. I do not want you to falsify things, but rather, I want you to be good at documenting your therapy so that a third party person, no matter what their background, can read it and think, "this OT knows what she is. Doing."
Lists levels of assistance provided and why it requires the OT. If you only write down what someone needs and not the skilled OT portion, a reviewer might think the RN could have done that. You want to highlight how you positioned the person's body at the edge of the bed, how many verbal cues you used, and if you were able to downgrade or upgrade the level of intervention that you provided. Another great thing to include in your documentation is the risks involved if you are not there. A simple way to do that is to say a patient is at risk for more falls, a decline in their ADLs, a reduced initiation of ADLs, injury related to falls, et cetera if occupational therapy is not involved. Explain your rationales for your interventions. What are your skillsets and clinical reasoning? For example, why did you upgrade or downgrade the task? Why did you decrease in frequency? Write all of that rationale down. You need to answer "the why," especially in fall prevention because people defer to physical therapists. We want to show that we can do things that help our patients.
Tie the interventions to the medical record as it supports your rationale. Perhaps you are working with somebody that has Parkinson's. You may be helping the client to move their arms back and forth while they are walking to do their ADLs around the house. You want to tie that back to their diminished movements related to Parkinson's disease. While it may seem obvious to you as the OT practitioner, it may not be evident to everybody else.
It is also crucial that we investigate conditions and how they are related to falls. Do not feel bad if you see a diagnosis that you have never seen before and you are not sure how that relates to falls or anything else that you are trying to work on for ADLs. Get on the internet and research things. I also have the "Quick Reference Guide to Occupational Therapy" on my desk. It can give you great ideas of what to address in your care plans that you can then relate back to falls.
Skill Development Opportunities
- Training on the assessments mentioned
- Falls Prevention Digital Badge from AOTA
- Stopping Elderly Accidents, Deaths, and Injuries (STEADI)
- Stepping On (https://www.steppingon.com/training/)
- Train on incontinence prevention and resolution
- Develop understanding about falls and car accidents
- Tai Chi
There are other ways to develop your skills related to fall prevention, and I encourage you to do this. The first suggestion is to do training on the assessments that I referred to earlier, like the I-HOPE, the MoCA, or some of the checklists. You can also work towards a Falls Prevention digital badge from the American Occupational Therapy Association. They have a fall prevention one, which includes two courses related to community-dwelling older adults. The highest level of the badge consists of an additional module about hospital settings and falls, which is another long conversation because falls are a big deal for occupational therapy patients in hospitals.
Stopping Elderly Accidents, Deaths and Injuries called the STEADI is a widely used course that healthcare professionals can take. It gives steps to providers to prevent falls in a variety of different practices. The ultimate goal is to reduce falls among the older adult population, 65 and older. The STEADI promotes health and independence, is provided through the CDC, and is recognized by many physicians and hospitals. This tool is an excellent way for you to help them see the role and benefit of OT. Our hospital system in Northern Colorado and my company both used the STEADI, which has enabled us to communicate.
Another program is called Stepping On. It is an evidence-based and effective program proven to reduce falls in older people living in the community. If you are doing home care, mobile outpatient, or community outpatient, this is an excellent program for you to embrace. It takes about six weeks and incorporates strategies for positive lifestyle changes. The goal is to keep people independent and active, which is in OT's wheelhouse. The evidence has shown that the Stepping On program reduces falls by 31%, which is huge. I encourage you to look it up and complete training if this is of interest to you. The program brings in multiple professionals to talk to the participants, which is excellent. Still, you could also become the professional that the Stepping On leaders and teachers bring in for the exercises. I have done that. For example, you could do the TUG on the first day and teach them exercises, and then the program teachers will modify the exercises for home. Then, you could come back at the end and remeasure everybody via the TUG. You can also go in and talk about home safety and adaptive equipment. I have set up a massive table with adaptive equipment before class so that participants could investigate some of these options. It has been great.
If you want to get involved in fall prevention, you could see if the administrative team and marketing would support this initiative. It would help them to get referrals and recognition, and it enhances you as a practitioner.
Another idea is getting trained in incontinence prevention and resolution. I am board-certified in pelvic muscle dysfunction using biofeedback, and incontinence is huge for fall prevention. Research shows that if somebody gets up at least once a week with urge incontinence, falls go up by 26%, and the risk of fractures increases by 34%. I had a woman I treated in my private practice with lots of issues, including incontinence, I talked to her about that, but she did not want to address it. I pushed her, but she declined, and I eventually discharged her. Fast forward about six months, I was filling in PRN at a skilled nursing facility to do evaluations for the OT, and I saw her name. She had shattered her ankle by falling when going to the bathroom at night. Due to urge incontinence, she had urinated all over the floor and slipped. She said, "I think I'm ready to address incontinence," when she saw me. This was a little late, but better late than never.
There is also a correlation between falls and car accidents. Older adults that have fallen are 40% more likely to experience a car crash than other older adults that have not fallen. You can check people's cars for dents and other signs of impact. Talk about falls and car accidents with patients and families.
Lastly, if you have never experienced Tai Chi, I encourage you to look into it. Tai Chi is very helpful for fall prevention, and there is excellent research behind it. This is a great tool to integrate into your care.
Creative Ideas Related to Fall Prevention
- Lower extremity strengthening
- Aquatic training
- Focus on improved confidence
- Train doing practical activities
- Tai Chi
Let's now talk about creative ideas related to fall prevention. These are going to be a little bit all over the map. First, lower extremity strengthening is essential and research backs that it helps with fall prevention. Many OTs steer clear from that, but if PT is not involved, do it. And even if PTs are involved, find out what they are doing, and then you can help your patient figure out how to incorporate that into their daily routine. You can also take some CEUs on the topic. There is no problem with OTs doing lower extremity strengthening.
Most of us do not have access to a pool, but if you do, please use it. You can also find out how clients can access a pool in the community as aquatic training reduces people's fall risk. I have taken clients to a local pool. One of the main challenges was helping them change into bathing suits in the locker room. Often, there is only a bench that has no arms or handrails. They also have to manage a locker, get to the pool bare feet, and enter without falling. One of our OTs was with the patient, and when she went to sit down on the bench, she missed and fell on the floor. Falls can happen while clients are engaged in OT, and we have to be prepared to keep people as safe as possible. Encourage patients to go to aquatic training or a Stepping On class. You just need to make sure that you are bumping that occupational profile out a little further to address all the pieces that go into those community activities.
Focus on improved confidence with your clients, especially the fear of falling. We will do training on practical activities anyway but also include the fall prevention piece. For example, if you see a patient in a skilled nursing facility for a hip fracture, do you always have to walk to the gym through the hallway? Could you take them on a longer route or outside on the sidewalk? Can you set up obstacles on the way down to the gym? Discuss curb awareness, obstacles, different surfaces like ice, gravel, grass, and other things that people will have to navigate when they leave the skilled nursing facility.
I want to go back to Tai Chi for a moment. I worked with an OT that had training in Tai Chi. He integrated many of the movements into his home exercise program assignments, making a difference.
- Add loops to Velcro shoe straps and use a dressing hook to fasten and unfasten
- Trial the Able Tray
- Improve footwear
- Vision assessments
- Clutter removal
- Make items easy to reach
- Evidence-based exercise programs
Adding loops to Velcro shoe straps and using a dressing hook to fasten and unfasten shoes are one example of an adaptation to prevent excessive leaning. Occupational therapists are pros at low-tech adaptive equipment. We just need to make sure that we train people on using the equipment, so they are using it to the best of their ability. Other types of equipments such as sock aids, reachers of different lengths and styles, long-handled shoehorns, and lazy Susans on counters or in cabinets are great tools for fall prevention. I like to take a big bin of adaptive equipment or even laminated pictures when I visit clients. The pictures or videos are beneficial for the larger equipment that is difficult to carry from home to home. It is helpful for patients to see people similar to them using the equipment. You can also get catalogs to give to clients. They may find equipment that might be appropriate for their situation and open them up to other fall prevention ideas.
Figure 7 is the Able tray.

Figure 7. The Able tray.
This is a piece of equipment that I like. In one of the hospitals, we set up a little sitting room where patients could try different seating heights and equipment. I had an Able tray in there.
Improving footwear seems obvious, but it should be highlighted to your clients. There is a slip-on shoe called Kizik that is a great option. For those with foot deformities, make sure that you get them to a podiatrist. This is another discipline that you can collaborate with on falls.
Vision training is helpful to help clients with fall prevention. I have another bin for magnifiers, different light bulbs, and other options for vision impairments. I even have teaching glasses that mimic macular degeneration or cataracts. Caregivers can put these on and see what their loved one is experiencing with eye disease.
We want to look at the environment and remove clutter. This is an obvious intervention for OTs, but you can even integrate this into your visits. "We will work on a little bit of clutter removal right outside of the bathroom door today." We want to make our interventions meaningful to patients and set up their space to support function. Evidence-based exercise programs are great, especially the Stepping On exercise program, which is easy to integrate into daily tasks.
- Add high-contrast in bathrooms
- Install toilet lights
- Motion-detecting night lights
Another fun thing is adding high contrast to bathrooms. An individual with cognitive impairment, like dementia, can be confused if the floor, shower, toilet, and sink are all white, putting them at high risk of falls. People need to see can see where they are going. If you throw a black mat onto a white floor, the opposite can happen. Those with dementia may think it is a hole in the ground and walk around it. Knowing how the contrast of things will work for your specific patient is essential. A colored toilet seat on a white toilet or putting a contrasting color (tape or paint) along the edge of a floor transition can be helpful. Toilet lights or motion-detecting night lights help make sure somebody is sitting in the right place, but it may still be hard to see with a white toilet on a white floor. Figure 8 shows a toilet light.

Figure 8. Example of different toilet lights.
- Add lamp touchpads
- Garage lighting
- Non-skid flooring
You can also add lamp touchpads. I had a patient that was very fearful due to low vision. We put a lamp touchpad like the one in Figure 9 next to her in the bed because she had fallen multiple times in her bedroom trying to get the lamp turned on.

Figure 9. Lamp touchpad.
It was simple and a very easy fix.
Another place that I encourage you to spend a little time is in your patient's garage and outside areas. People with limited mobility may not make it into the house before the garage light goes out. I had a client who broke his hip and humerus after coming home after dropping off his wife to get her hair done and tried to walk through a dark garage. Spend some time in the garage and outside to make sure individuals have good lighting available all of the time.
Where is their mailbox? They can have a mailbox attached to the side of their house if they have a fall risk. You can simulate that and see if that works for them. I worked with a woman that had a neurodegenerative disease, and the first time she went to get her mail on the side of the house, she fell. This is why I started seeing her. You want to make sure that you are addressing that ADL thoroughly.
What do they do for different seasons? Do they water flowers in the summer? What do they do for ice? Do they have ice melt near their front door if they need to get outside? Non-skid flooring can be helpful as long as their feet are not sticking on the floor when walking.
- Med review
- Practice transport of items
- Add a handheld shower head holder to the shower wall
Make sure you review medication with the client and encourage them to talk to their pharmacist or physician if you suspect their medication is causing a fall risk. You can also reach out to the physician to review the client's medication with their permission.
It is essential to practice the transport of items. This is one of my favorite treatments to do for fall prevention. I have them practice moving objects, like laundry, with a walker or whatever assistive device they use. We talk about walker bags, and sometimes these are donated from churches. I have also used baskets that slide under a shelving system in your closet. These fit perfectly onto a front-wheeled walker. They can put their dish with a lid, a water bottle, or a covered cup. Even a plastic Walmart bag tied on the side of the walker for trash is an easy fix. There are many creative fall prevention ideas on Instagram. Talk about what people need to carry in a daily routine and develop a checklist to go over in treatment.
You can also add a handheld shower holder. One is held by a 3M disc shown in Figure 10.

Figure 10. A detachable handheld shower holder.
We do a great job recommending handheld showers, but we do not always put them where people can reach them. People often have to reach forward, and we see falls in the shower because of that.
- Install grab bars
- Modify thresholds
- Add voice-activated tools
- Address incontinence
We can also prevent falls by installing grab bars. We have to follow ADA requirements, but we also need to make sure that we are letting the installers or family know where the grab bars should be. We also need to look at all thresholds. Some devices can cover a high threshold to make mobility easier. It is vital to get rid of all tripping hazards.
Voice-activated and remote control devices can also be great tools. Figure 11 shows a remote control door that is shown at the top.

Figure 11. A remote control door.
Many clients that I work with have spinal cord injuries or muscular dystrophy. Remote control doors are great because their door is locked, and they feel secure. If they have caregivers coming, they can push a switch and open the door. And doors can put people at risk for falls. We talked about incontinence earlier. Lastly, I have listed some links to all the equipment I referenced.
- Toilet bowl light - https://www.amazon.com/16-Color-Activated-Detection-BirthdayGadgets/dp/B07L2Y62G2/ref=sr_1_3_sspa?keywords=toilet+bowl+light&qid=1638240026&sr=8-3-spons&psc=1&spLa=ZW5jcnlwdGVkUXVhbGlmaWVyPUFBTkc0TVhQWFVRRjgmZW5jcnlwdGVkSWQ9QTAzNDIyMTI5NEc3Tk02UEY4Vk4mZW5jcnlwdGVkQWRJZD1BMDc0OTQxMTNMMVFJRjI2U1BQOFImd2lkZ2V0TmFtZT1zcF9hdGYmYWN0aW9uPWNsaWNrUmVkaXJlY3QmZG9Ob3RMb2dDbGljaz10cnVl
- Lamp dimmer control switch - https://www.amazon.com/Dimmer-control-switch-dimming-chandelier/dp/B07TV9B6XK/ref=sr_1_4?keywords=touchpad+for+lights&qid=1638240297&qsid=140-7965901-2605033&sr=8-4&sres=B08K87X6SG,B087R8TLS7,B07TV9B6XK,B08PP14BVB,B08G1KN12F,B018WOIRWI,B074GR1VM8,B00BX0YKX4,B000FPCEFY,B07SN37DFC,B00I5SW8MC,B07FSKZVRG,B09BRG3MZ2,B077VYRMC1,B08BX7FV5L,B00KLAXFQA,B00B8Q31UQ,B07SD3T8M1,B00JJY0S4G,B07C6LX1NF
- Handheld shower head holder - https://www.amazon.com/BRIGHT-SHOWERS-Handheld-Showerhead-Positions/dp/B07814TBHB
- Residential door opener - https://www.careprodx.com/ada-door-openers/residential-door-opener-deluxe/?sku=DS 4-R
- Able Tray Table - https://www.lowes.com/pd/Able-Life-Able-Tray/1003166866
Summary
You want to teach people how to get up off the floor as part of your visit. What will you do if you cannot get off the floor? Can you crawl to the couch or a chair? The other thing to remember with fall prevention is that it does not always happen when the client is up and walking around. Falls can occur when they are lying in bed, so positioning is huge. Talk about different positions like sitting, standing, leaning, and bending.
It would help if you also talked about their health conditions, which can empower patients. Most of us do not take the time to step back and talk about a client's underlying issue. For example, a patient may have had Parkinson's disease for 12 years, but they must be knowledgeable about brain changes, how that may affect them neurologically, and what that means for fall risk. We provide a lot of education via handouts, presentations, talking to doctors, et cetera. Still, we do not always talk to the client about how that will affect meaningful tasks. Bring that home for them and help them plan for the future. Some examples of decline are furniture surfing, a decline in initiating ADL, a more challenging time getting up, or needing to grab things to pull up. Tell your family members that they should call you or let their doctor know if they see these red flags.
Talk with your clients about foot care for neuropathy and diabetes. If people have sores on their feet, they cannot feel injuries or need to change their shoes all the time. This creates a risk for falls.
You also want to talk about alcohol use. If somebody is drinking every night, what does that mean? I had a patient that was 103 that had a hot toddy every night. There was no way she was going to give that up. I made sure that she did not have her hot toddy until she was done with her evening ADLs, and she was in her chair, and all she had to do was go to bed. There was a risk, but at least she was not having the hot toddy and then getting ready for bed, which put her at a much higher risk.
Check people's vestibular systems, and get extra training if that interests you or refer out. You can also talk to the orthopedic surgeons, neurologists, and podiatrists about what OT can do related to fall prevention and how it relates to their practice. They will embrace that. Many of our doctors do not have the time to address all the things with patients. You can use the MoCA, the TUG, or the ABC to get baseline data to share with the doctors. They will appreciate that, and then hopefully, you will start getting feedback from them too.
Get people involved in a community if you are working in outpatient, whether mobile or in a brick-and-mortar structure, and understand what is going on in your community. Research tells us people have fewer trips to the ER if they are involved in their community, even if they are only going to the senior center to play bridge. Help them figure that out as they will be more active and less depressed. And we see all these risk factors go down. Remember to scope out where they will look for fall risks, like I mentioned earlier about the aquatic training center.
Refer out for ongoing support. Are there support groups for Parkinson's that would help them? Is there a Stepping On program? Remember that you do not always want to be the end of the rehab experience; you want to give them the next link in the chain. What should they do after they see you? Seek out occupational therapists writing blogs or people on Instagram as they may have good ideas for your patients.
I have a wrap-up quote, and then I will answer some questions. "True prevention is not waiting for bad things to happen. It's preventing things from happening in the first place." If you have a patient who has not fallen or has only had one or two falls and is a little resistant to some of the education you are giving them, give them this quote. Tell them that your job is to help them figure out how to prevent falls.
Questions and Answers
What do you do about pets?
Pet care is a fall prevention issue. Many people would risk a fall rather than get rid of their pets. I have seen countless people fall over their pets, but they still love their pets and are going to keep them. They can put their pets in a kennel or a different room when they are doing their ADLS, so they do not have to manage around the pet. There are also creative ways to feed pets so that people do not have to bend over. You can look up adaptive equipment for pet care. If a cat litter box can be placed up high, I would do that. Dogs that jump can be a problem. I would encourage your patient to get the dog enrolled in some sort of obedience training. Education is huge. "Your dog is a trip risk because of XYZ."
What did you do about the clawfoot tub?
We went round and round and did a sliding bath bench in and out of the tub. The patient could stay in the tub, but there was a height difference. We added a lot of grab bars on the back and the front wall, and they could do it. It was not ideal, but they wanted to keep it, and as far as I know, they are still using it.
I like your idea of talking about the future in an evaluation.
Definitely, if somebody has a neurodegenerative disease, we know that there will be a progression, so education is the key. One thing is whether they are having a good or bad day when you are assessing them. I also encourage you to try to visit those with cognitive issues later in the day. If you come at 8:30 in the morning, they may be bright-eyed and bushy-tailed, but they may look different afterward. Caregivers are also great to ask. "Is this a normal day for her or a bad day? How do they normally look?" We always want to learn about those bad days and treat them from there. If we just treat them on good days, we will not make as much of an impact.
Any advice on working with families who are in denial of how the patient's dementia may result from the falls?
I do have a couple of thoughts about that. If you have some research articles to leave behind, ask them to read them and then come back to discuss. I have also been able to make it less personal by discussing the benefit of strengthening for people with dementia or older adults.
There is a magnet system that attaches to shoelaces for inexpensive adaption to easier don off, doff shoes.
That is an excellent recommendation. Again, OT blogs are great resources.
About the patient that did not want to address incontinence due to dignity and pride, what are some of your suggestions to address safety adaptive equipment?
I may come back with more of a global approach. "We do not always want to integrate using adaptive equipment because we have done it the same all these years. However, I want you to try something for two days. Would you do that?" When it comes to dignity about incontinence, I sometimes give them a checklist and ask that they fill it out the best they can. Then, we can review it on our next visit. "I understand that talking about bowel and bladder health is uncomfortable, and I get that. If you are okay, can I ask you some questions?" Sometimes that will help. If you can get comfortable saying things like uterus, bladder, and bowel, and you are comfortable, they will also be more comfortable.
What did you say about the mailbox?
You can contact your local post office and put in a medical request that a little mailbox be posted on the house so they do not have to go down to their mailbox at the driveway or down the street if they have a community-based one.
Could you give us some OT treatment ideas to improve balance?
I have plenty of ideas. Perhaps you can put a gait belt on them and have them balance on one leg while doing ADLs. You could have them stand on a foam block while washing dishes to work on balance. Stepping On focuses on balance exercises, and there are many things you can do with balance. I challenge all of us to work on balance in our treatment.
With stairs being a high-risk area, what do you recommend?
Stairlifts may be a good idea. PT may want to encourage a patient to do the stairs or encourage them to live downstairs. However, many clients do not want their freedom limited. You have to consider this.
References
Citation
Covell-Pierson, K. (2021). Assessing and preventing falls at home: A practical approach for the OT. OccupationalTherapy.com, Article 5500. Available at www.occupationaltherapy.com
