Cara: I am glad that you took time out of your day to come and learn about building healthy brains. It is really important for us, as therapists, to understand posture. This is an intermediate course as I am hoping that everybody has a basic understanding of a child's sensory system. Our distal coordination is contingent on our proximal stability. That is very critical for all function. We have to have this coordination of our entire bodies in order to access higher brain function.
Importance of Movement
There is a push in our country to have children learning at earlier and earlier ages, and many kids are addicted to technology. They are using technology constantly even as little babies. We also have companies that want to help facilitate babies in these positions as shown in Figure 1 on the left.
Figure 1. Sedentary activities.
My kids had vibrating bouncy seats when they were little. These seats put babies in a seated posture before they are ready. They do not have the strength and skills to sit up against gravity, but yet we are forcing them to do so. We also have kids that are sedentary due to using devices (picture on the right). There are wonderful apps that can be great, but they are so visually complex. We are also giving them to our kids way too early. This becomes problematic as kids access higher level education. They need to fidget and move, and we are asking them to sit still and pay attention. When our systems are not integrated, difficulties are going to occur. According to an article from the National Association for Sports and Physical Education, young children should never be sedentary for more than 60 minutes at a time. I think 60 minutes is actually too long. We need implement activities a lot sooner than that.
I call sitting devices containers. We are putting these babies into these containers for convenience or to free up our time to do other activities like cooking dinner. As you can see, this baby is stuck in a flexed pattern, and she is sucking on a pacifier to organize herself. The child on the right is in a W-sitting position in order to stabilize to use his electronic device. Our body is designed to integrate our vestibular, proprioceptive, tactile, and visual systems so that we can stabilize our body and move our eyes independently.
Vestibular System
This is a photo of the ear in Figure 2.
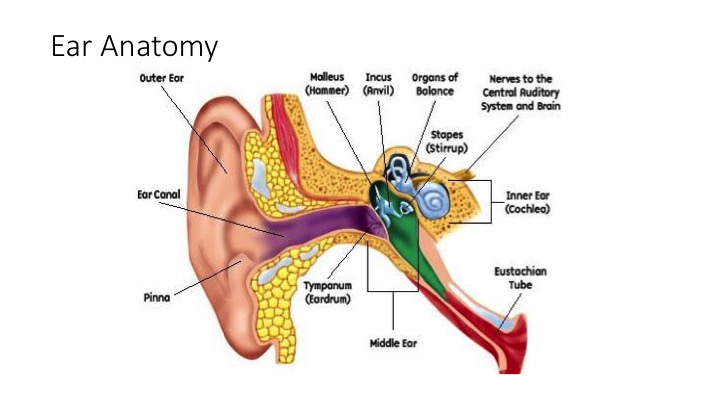
Figure 2. Ear anatomy.
There is the outer ear that we can see and then inside are the different organs. We are going to zoom in a little bit in Figure 3.
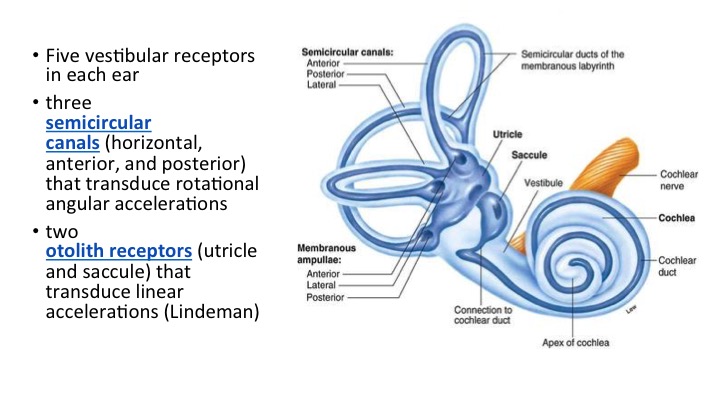
Figure 3. Total of 5 vestibular receptors.
The first three are the semicircular canals that are oriented in different directions: vertical, horizontal, and diagonal. There are also two otolith receptors, the utricle and saccule, for a total of five vestibular receptors in the inner ear. They also transduce movement and linear acceleration.
The vestibular system is more than just the inner ear. Integrated Learning Strategies are amazing and they have some cool graphics like Figure 4.
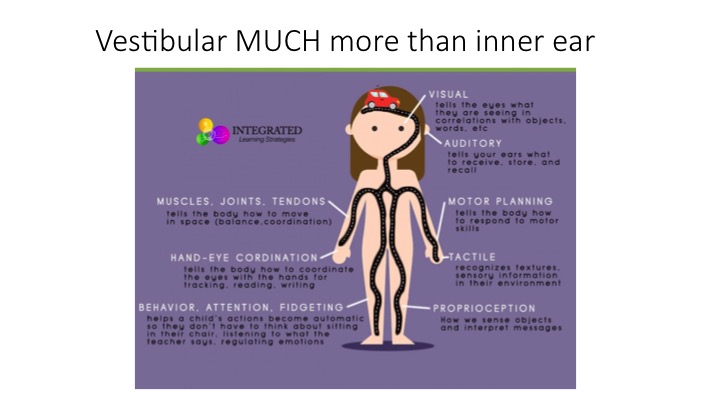
Figure 4. Overview of the vestibular system.
The vestibular system tells the eyes what they are seeing in correlation with objects and words, what we hear, and what we process, store, and recall. It also helps us with motor planning. Our tactile system are receptors that tell us about textures and relays sensory information.
It can be very complicated. We, as OTs, need to understand that what we are doing can have a significant impact on a person. We are not just spinning a child and causing some postrotary nystagmus. There is a ton of complicated neurology involved in these processes and movement. As I mentioned, I just presented this last weekend at a state conference. I had a bilateral ear infection when I did this, and as a result I experienced a dizziness and disorientation. If you have ever had a sinus or an ear infection, you fully understand the implications of a child that has poor vestibular responsiveness, whether it be hyper or hypo.
It is important for us to remember that not only are we moving forward and backward, but also in these planes of motion. We move forward and backward, side to side, twist and turn, and a combination for diagonal movements.
The Pyramid of Learning
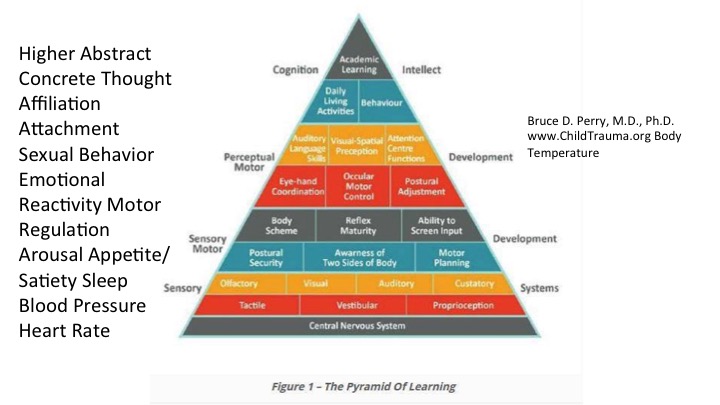
Figure 5. The Pyramid of Learning.
The bottom of the pyramid of learning is very critical (see Figure 5). This is basic sensory information that we all know as OTs. I would further add the term interoception here, which is the knowledge of your body. These are the receptors inside of your body that control heart rate, toileting, hunger, and thirst. You have all of these sensory systems working in combination, which are way at the bottom of the pyramid. Next, in the blue, are postural security, awareness of two sides of body, or bilateral integration, and motor planning. Moving up into the gray areas, there is reflex maturity. This is not just reflex integration, but maturity of the reflexes as a whole. This includes posture and equilibrium. Additionally, at this level, is the ability to screen input, or deciding what is important and not and body scheme. Further up, we have hand-eye coordination, ocular motor control, and postural adjustment. You can read all the way to the top where we have our abstract, higher level academic learning.
There are children that cannot even sit in their chairs because they have decreased reflexes or vestibular hypo- or hyper-responsivity. You can see how not having the foundational skills can affect their ability to access these higher level skills. This was really eye-opening to me as a clinician. During my 20 years of practice, I feel as though I have done a little bit of a disservice to my clients by not addressing some of the base elements first. For example, if I got a referral for handwriting or poor hand-eye coordination, I do not know that I always addressed some of the foundational elements first. A child has to have a strong base of support if they are going to move to a higher level.
Modulation
How do we achieve modulation? Modulation and regulation are controlled in the brain stem and mid-brain. When we treat kids that have behavior issues, we first need to look at where they are functioning. When a task is required, your body has to regulate so that it can meet the demands and is ready for learning. Often when a task is requested, these kids melt down and fall apart. Regulation is when we assist with the change required, and self-regulation is when the child makes the change on his own.
Brain Review
Let's go over a quick brain review in Figures 6 and 7.
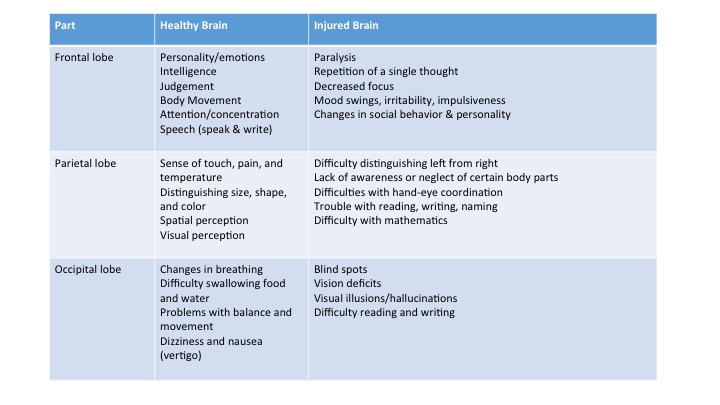
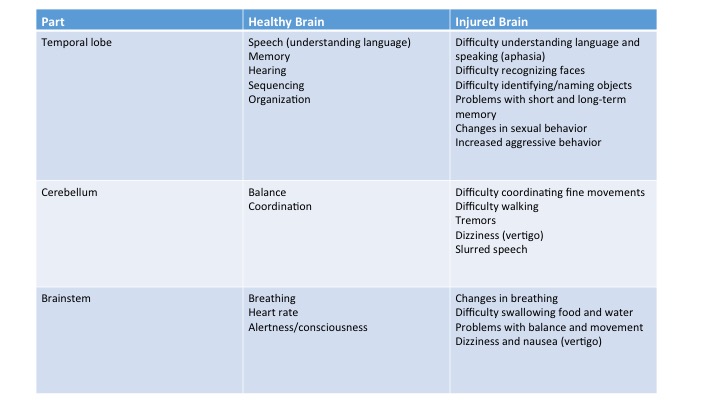
Figures 6 and 7. Brain overview.
The frontal lobe is where our executive function takes place. This is our ability to organize, plan, and execute. It is also where our personality is. The parietal lobe, in a healthy brain, controls pain, touch, temperature, shape, size, color, and spatial and visual perception. The occipital lobe controls breathing, swallowing, and balance and movement. The temporal lobe has the speech, understanding, memory, hearing, and organization control centers. Balance and coordination are found in the cerebellum. The cerebellum is very specialized, and with damage, a child is going to have difficulty coordinating fine motor movements and walking. They also may have tremors, vertigo, and slurred speech. The brainstem is at the lower level and controls basic functions.
Physical Manifestations of Immature Brain Function
Signs of Complex Sensory Processing Disorders
Sensory Modulation Disorder. This is a problem with regulating input. It can result in withdrawal or a negative response. These are kids that are upset by sounds and noises, like the fire alarm. They have a lot of sympathetic nervous system responses, such as fight or flight, and a lot of cortisol in their systems. They are easily distracted and often need to sit in the front row because the movement of students in front of them might distract them. They may have trouble with sleep. They often have melatonin recommended to help with this. They may also need seamless socks and seamless undies due to hypersensitivity.
Sensory Discrimination Disorder. Sensory discrimination disorder is a problem recognizing and interpreting differences or similarities in the quality of stimuli. These are the kids that use too much force. They are crashers and bumpers. They are the kids that are super responsive. They are afraid of heights if they are vestibularly or gravitationally insecure. They can have poor balance.
Postural-Ocular Disorder. These kids have problems controlling their posture and movement, as seen in their muscle tone, joint instability, and poor functional vision. They may have a lot of problems in school. I always suggest a functional vision evaluation if I suspect this. This is not to test acuity, but rather to assess depth perception, are the eyes moving in tune with each other, and focusing on one thing. They may also have flat feet, slump, are weak, and problems with eye tracking.
Dypraxia. This is problems in planning, sequencing, and executing unfamiliar actions. They want routines. They may have trouble with ADLs and completing complicated tasks. Most do not prefer sports.
Case Study #1
This is Joshua, and he is 11 years old. He has mitochondrial disease and autism. He has reflux and is GJ tube fed. He has a fear of making errors, and he does not want to do things on his own because he is afraid of making a mistake. He also has flat feet, which you will see in the video. He has low energy. He is very smart, but has trouble reading and is below grade level in school.

As a rule of thumb when I am assessing a student, even for a simple handwriting assessment, I like to tape a line on the floor to assess his movement. I did not expect to see this with this little boy when I first got him as my client. When he is duck and pigeon walking, he has trouble differentiating his upper body movement from his lower. For example, when his feet are turned in, his arms are turned in, and his whole body collapses. You can also see his mouth change as well. He is unable to coordinate independent movements. His feet are flat, and he is really uncomfortable even doing these basic movements.

Prone extension and supine flexion are standard things you should assess. Can they access these positions? With Joshua, he was unable to maintain the position of prone extension for more than a second or two with any quality. A child, with no core or postural issues, can typically do this position for 30 seconds.
Even when Joshua would sit, his whole posture was stuck in a flexion with very low tone. He had a weak core with many breathing issues. This is because his rib cage and diaphragm were compressed, and he was not getting proper oxygen flow. He has postural-ocular disorder along with some other things. I will talk about what I did with Joshua in a little bit.
Case Study #2
This is Jacob, and he is 14. He is hypervigilant and very responsive to sounds. In fact, he cannot go to school and is homeschooled as he is so afraid of the fire alarm going off. He has a genius IQ, yet he has very few friends. He is a toe-walker, and was serial casted by physical therapy when he was little. He has a retained moro, or startle reflex. Like Joshua, he is also afraid of making errors. He has difficulty sleeping, poor balance, and is gravitationally insecure.

During the assessment, I am looking specifically at reflexes and the ability for him to integrate them. I purposely have him put his feet together, and this is going to give me a better idea of his reflex integration. In this video, I am testing to see if he can maintain an upright position. He has a lot of trouble even with his eyes open. He loses his balance and complains of dizziness by the end of our assessment.

I also always like to test the crawling position. One of the other critical questions to ask parents is if the child skipped crawling. Crawling helps a child to bear weight through their hands and helps them to separate the different sides (thenar and hypothenar) of their hands, which ultimately helps with handwriting. Crawling also helps with neck extension. Jacob skipped crawling, and he needs a lot of work in that position. He has balance issues as you can see in the video. We practiced this activity before filming so I knew he was not going to fall. He also has sleep issues. He is a kid that slipped through the cracks because no one had assessed any of these things with him before. He has a weak core and spinal reflexes. These kids commonly have trouble riding a bicycle due to coordination and balance issues. Jacob has both a sensory modulation disorder and a sensory discrimination disorder.
Regulation
Emotional regulation issues are very common in the children I see. They are very immature. Depending on what they are doing, there are only certain moods that are available to them because of their current body state. They cannot be happy and calm when their adrenaline and cortisol hormones are at their peak levels. When our sympathetic nervous system is on, there is no "off" button. It is a non-teachable moment when you have a child in this state of arousal, and it takes time for those hormones to resolve. On the contrary, the parasympathetic system focuses on "rest and digest", and has our feel-good hormones. When we are feeling good, it is harder for us to be angry. Make sure that their state matches.
Breathing is important to balance arousal levels. This is why when you are testing kids, breathing and rib cage and diaphragm movement are critical. Go ahead and do a W sit for me if you are able, and then try to take a deep breath. In addition, try to do the Valsalva maneuver, which is when you push to go to the bathroom. You cannot do this if you are hunched over with a posterior pelvic tilt.
With motor and emotional regulation issues, we may have an imbalance. How do we regulate? The sympathetic nervous system, which I did not know until I took a recent neurology course, is located in the thoracic cord. This is how basic these reflexes are. Even if you do not believe in reflex integration as there is not a ton of evidence, it is good to realize that these are basic reflexes. Parasympathetic reflexes are located in the sacral cord. I think that is interesting. When you look at interoception, that eighth sense, and sexual arousal, those are in the parasympathetic nervous system, but climax is located in the sympathetic nervous system. Even that takes quite an orchestration of our bodies.
Three Levels of Brain Function
Arousal. Arousal is a basic state. When a baby is in aroused state, they are alert. They are either in flexion position, or extension, and they are thinking about themselves. They are existing.
