Introduction
Today, I want to go over my role as an occupational therapist in the treatment of eating disorders in private practice. I conduct CBT sessions where clients learn skills and apply and practice them in real life occupation-based situations. Therapy could include CBT in-office sessions, community sessions, or home sessions. An example is a grocery shopping session where we work on healthy food selection and portions. We then complete home-based sessions for food prep. This could be working with a college grad student who is preparing food for himself or herself or supporting someone who is cooking for their family. Other sessions are conducted by visiting restaurants and practicing some of the CBT skills that are learned in earlier sessions. We work on things such as increasing and decreasing the time spent eating, looking at food rituals and practicing coping skills. Another element that we address is clothes shopping. We also do fitting room sessions with the ultimate goal of replacing unhealthy coping skills with healthy coping skills as an individual progresses in treatment. We are going to hone in on the cognitive behavioral therapy aspect of the treatment.
Occupational Therapy
As occupational therapists, we focus on enabling individuals to participate in meaningful and purposeful activities of daily living. That is at the heart of what we do. Occupational balance is an even distribution or condition in which different elements are equal or in the correct proportions. I do not believe this definition works when it comes to our occupational balance because equal essentially means perfect. You cannot ever have your occupations be perfectly balanced. Naturally, we are going to be spending more time in a day on certain tasks rather than others. We need to give up this notion that we have to spend an even amount of time in each task or occupation of daily life. Occupational balance can be defined as an individual's perception of having the right amount of occupation and the right variation between occupation. For one person, this can mean spending more time with family rather than at work. For someone else, it can mean having alone time rather than family time. This is something that is entirely individualistic, and there is no right or wrong way. Regardless, for a person who is struggling with an eating disorder, their prior healthy roles and occupations fade and their primary occupation becomes the eating disorder and the rituals and behaviors that are required to maintain it. They experience an imbalance where the configuration of activities within their lifestyle does not meet their physiological or psychological or social needs in a manner that is helpful and satisfactory to the individual. For example, if we are looking at leisure activity, someone with anorexia nervosa may over-exercise or workout excessively rather than take part in the activity as an enjoyable leisure activity. They may stop socializing or going out to eat with their friends because of their eating disorder. As occupational therapists, we want to integrate each person's interests and daily routines back into their activities of daily living. An eating disorder impacts every occupational and client factor including rest, sleep, basic ADLs, social participation from cognition to body function, and many things in between.
What Can We Do?
- Provide a safe setting where a person with ED can engage in multi-sensory activities via doing
- Practice habits which create or reinforce healthy roles and occupations
- Provide patient with a setting where verbal insights can be converted into new behavior
- Develop functional life skills through meaningful occupations
- Identify the source of a client’s relationship with food and weight
- Implement a variety of activities to help individuals engage in daily routines such as meal planning and grocery shopping.
- Experiential components sit at the heart of authentic OT theory and practice.
We can provide a safe setting where a person with an eating disorder can engage in multi-sensory activities via doing. These are practice habits which create or reinforce healthy roles and occupations and provide the patient with a setting where verbal insights can be converted into new behavior. We can help them to develop functional life skills through meaningful occupations. We can help them to identify the source of a client's relationship with food and weight by implementing a variety of activities to help the individual engage in daily routines such as meal planning and grocery shopping as I mentioned earlier. Experiential components are at the heart of authentic OT theory and practice.
What exactly are we talking about when we say experiential interventions? "Experiential interventions" is another way of saying a hands-on approach. It can include several things like the use of learning new coping skills, mainly through cooking and clothes shopping, the use of alternate mediums for expressing thoughts and feelings, like creative writing and drawing, and talking while engaging in an activity so we have increased access to a client's inner emotions, their feelings, their thoughts. Another example is guided movement and sensory strategies. Yoga is very popular when it comes to reconnecting to one's physical self.
Evidenced-Based Practice
One of the reasons we do not hear too much about occupational therapy and eating disorders is the lack of research that is being done on the subject. However, the occupational therapist is vital to providing a complete assessment and thorough treatment of the population with eating disorders (Breden, 1992). One of the reasons we do not hear too much about occupational therapy and eating disorders is the lack of research that is being done on the subject. However, the occupational therapist is vital to providing a complete assessment and thorough treatment of the population with eating disorders. "Occupational therapists working in eating disorders face challenges related to the lack of evidence base for OT in this area. Future research should focus on developing further evidence for OT and eating disorders and designing outcome measures that capture improvements in daily functioning. These efforts would strengthen the role of OT and reduce risk of burnout" (Devery, 2018).
Cognitive Behavioral Therapy (CBT)
Overview
Cognitive behavioral therapy is a short-term, goal-oriented psychotherapy treatment that takes a hands-on practical approach to problem-solving. CBT works to change people's attitudes and behavior by focusing on thoughts, images, beliefs, attitudes that are held, a person's cognitive processes, and how these processes relate to the way a person behaves as a way of dealing with emotional problems. CBT focuses on changing cognitive distortions that affect our behaviors and emotions. It follows this premise that if you modify the way you think that you change how you behave and feel.
These three things in Figure 1 all affect each other.
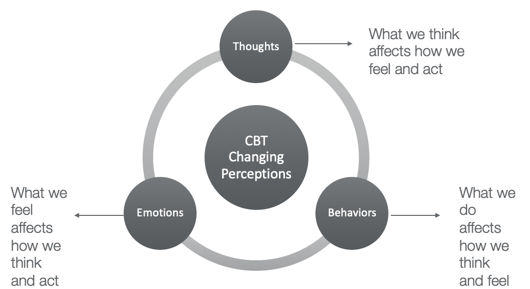
Figure 1. CBT overview.
CBT is unique as it was created to focus on a variety of affective-cognitive and behavioral techniques that make it more problem-focused and action-oriented. It is used for the treatment of anxiety disorders, panic disorders, behavioral difficulties in children, chronic fatigue, and anger management. Figure 2 is a simple representation that shows how our emotions, thoughts, and behaviors all influence each other.
Figure 2. Representation of our thought processes.
Our thoughts create our feelings, our feelings create our behavior, and our behavior reinforces our thoughts.
What Can We Do As Therapists?
We can work with clients to help them to break down their problems into smaller parts. We can help them to analyze what thought processes are dysfunctional and that are creating unhappiness and impeding independence in the person's occupational performance. These can all be related to the thoughts that the client feels about themselves, the thoughts and feelings of others, and/or their thoughts about the future. The role of the therapist is to help the client to focus on creating a positive future. This is sometimes compared to psychoanalysis, but we do not want to confuse CBT and psychoanalysis. Psychoanalysis focuses a lot more on the client's past and how they came to be how they are today. In CBT, we do not focus on the history of the patient, but rather we focus on their thought patterns. Thought patterns are changed. The goal is to help the client learn how their thoughts feed their feelings and behaviors while learning practical techniques that can be used daily in managing their thoughts and emotions.
CBT Sessions
- Number of CBT sessions can range from 5 to 20
- Sessions: 30-60 minutes
This is just a ballpark because every case can be very different. The number of CBT sessions can vary anywhere from five to 20, with each session lasting 30 to 60 minutes.
Evidence
- CBT is effective in treating addictions (Powers et al., 2008), smoking (Song et al., 2010), and gambling (Oakley-Brown, et al., 2000), reducing symptoms of schizophrenia (Gould et al., 2001), depression (Van Straten et al., 2010) bipolar (Gregory, 2010), and eating disorders (Murphy et al., 2010).
- CBT is also highly effective for various anxiety-related disorders (Hofmann & Smits, 2008) & obsessive-compulsive disorder (Kaczkurkin, 2013).
There is a lot of evidence showing CBT can be just as helpful as medicine, and it can be done in a short period of time. For example, it has been shown to be very effective in the treatment of addictions, substance abuse disorders such as alcohol dependence, smoking, gambling, reducing symptoms of schizophrenia, depression, and bipolar disorder. It is also a highly effective treatment for various anxiety-related disorders, obsessive-compulsive disorders, and can treat other general psychological issues such as insomnia, stress, criminal behavior, anger, and aggression. It is a highly effective treatment for many disorders and conditions, both psychological and physiological, and it has become one of the most recognized and sought-after treatments in both general populations and medical establishments.
Psychopathology of Eating Disorders
- Genetics
- 1st and 2nd-degree relatives more prone to developing ED
- Twin siblings 50% chance of developing ED
- 50-80% risk
- Behavioral
- Psychodynamic
The psychopathology of eating disorders centers around body image disturbance, concerns with weight and shape, being too dependent on weight and shape, fear of gaining weight, and even when you are underweight, a denial of how severe the symptoms are and distortion in the way that the body is experienced. It is clear that individuals have a distorted view of body weight and shape. This is not just a concern but more of a fear of gaining weight or changing shape.
Eating disorders happen as a result of a severe disturbance in eating behavior such as an unhealthy reduction of food intake or extreme overeating. It often starts off with someone eating smaller or larger amounts of food as compared to usual, but at some point, the urge to eat less or more spirals out of control. Eating disorders do have genetic causes. Anorexia actually runs in families. There was a study by Strober and Katz (1987) that found the first and second-degree relatives of individuals with anorexia are more prone to developing eating disorders. Another study by Askevold and Heiberg (1979) stated that twin siblings have 50% chance of developing the same eating disorder, but that study, unfortunately, did not explain if the twins developed it because they grew up in the same environment or not. There is a 50 to 80% risk of anorexia and bulimia both being genetic.
Behaviorists explain eating disorders as a condition that is shaped by a stimulus-response. When an individual is interested in improving their body weight, it can develop into an obsession. Receiving admiration and positive remarks from friends, family, strangers really reinforces this behavior. Then, there is pressure from society, cultural norms, and sometimes the person's role in society comes into play. For example, celebrities and models have high pressure to be thin.
There is also the psychodynamic approach by Freud that explains most of our actions happen on a subconscious level. A person that develops an eating disorder may have a subconscious desire to stay in their youngest version of themselves by looking very thin. Some females may be scared of growing up and becoming sexually mature. With low body weight, we know that menses often stops. Anorexic individuals have bodies that resemble teenagers or have boyish looks where breasts and hips are not as rounded as in mature women. Anorexic individuals also cannot become pregnant. These factors can all play a role in an eating disorder.
A lot of this may also have to do with trauma. I believe that the statistic is around 50 to 70% of females, who are diagnosed with anorexia nervosa, have had some experience with trauma in the past, and we will get into that in a little bit. However, some of what we know when it comes to trauma and eating disorders is that the person may use the eating disorder as an unhealthy coping mechanism to handle that trauma that they experienced as a way of gaining some self-control of an aspect in their life.
Eating Disorders
Overview
- Eating disorders (ED) such as anorexia, bulimia, and binge eating disorder include extreme emotions, attitudes, and behaviors surrounding weight & food issues.
- ED are serious emotional and physical problems that can have life-threatening consequences for females and males (National Eating Disorders, 2017).
- Almost half of the sufferers never seek or receive professional treatment.
Eating disorders such as anorexia, bulimia, and binge eating disorder include extreme emotions, attitudes, and behaviors surrounding weight and food issues. Eating disorders are serious emotional and physical problems that can have life-threatening consequences for females and males. Almost half of the sufferers never seek or receive professional treatment.
Statistics
- 4/10 individuals have either personally experienced ED or know someone who has.
- 1.0-4.0% of women have suffered from anorexia in their lifetime, and it has the highest fatality rate of any mental illness.
- 4% of anorexic individuals die from complications of the disease.
- 4% of females in the U.S will have bulimia during their lifetime (3.9% of these individuals will die)
Four out of 10 individuals have either personally experienced an eating disorder, or they know someone who has. One to 4% of women have suffered from anorexia in their lifetime, and it has the highest fatality rate of any mental illness as 4% of anorexic individuals die from complications. Also, 4% of females in the US will have bulimia during their lifetime and 3.9% of these individuals will die.
Types of Eating Disorders
- The main types of ED include:
- Anorexia Nervosa
- Binge Eating Disorder
- Bulimia Nervosa
The main types of eating disorders include anorexia nervosa, binge eating disorder, bulimia.
Anorexia Nervosa
- Low weight d/t inadequate food intake, intense fear of weight gain, obsession with weight and body image, persistent behavior related to preventing weight gain, a distorted image of own body and inability to understand the severity of the problem.
- Binge and purge
- Compulsive lengthy exercise
Anorexia nervosa is categorized by low weight due to inadequate food intake, an intense fear of weight gain, an obsession with weight and body image, persistent behavior related to preventing weight gain, a distorted image of your own body weight, and an inability to understand the severity of the problem. Some people may binge and purge. Purging is done via self-induced vomiting or taking laxatives. bingeing is categorized by consuming large quantities of food for example, maybe several thousand calories in one intake, but without the purging aspect. Some individuals engage in compulsive lengthy exercises to reduce body weight and expand consumed calories.
