Editor's note: This text-based course is a transcript of the webinar, Constipation Relief Through Treating The Whole Person: Postnatal Pelvic Health Virtual Conference, presented by Lindsey Vestal, OTR/L, TIPHP.
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
- After this course, participants will be able to identify the critical anatomy and physiology of bowel movements and clinical reasoning to make more accurate correlations between contributing anatomical factors, defecatory dysfunction, and routines.
- After this course, participants will be able to identify behavioral interventions for the relief of constipation for postnatal people, including specific interventions to treat clients whose systems range from overactive, underactive, and/or uncoordinated.
- After this course, participants will be able to recognize a client’s psychosocial components into interventions for holistic constipation relief, resulting in optimal outcomes.
Introduction
Thank you, everyone, for being here today. This is such an important topic, and when we talk about things like constipation, pregnancy, and elimination, I think it’s important to approach it with a bit of humor to make the conversation more approachable. So, let me kick things off with a couple of classic dad-style jokes.
Here’s the first one: Why did the constipated parent bring a pencil to their postnatal checkup? In case they needed to draw some conclusions!
Okay, if that one didn’t get a chuckle, let’s try this: Constipation after childbirth—because when you’re a new parent, even your bowels take their sweet time adjusting to the schedule.
Thank you for humoring me! I’m so glad we’re having this conversation because constipation is such an important topic to address and one that deserves more open discussion.
GI Know: A Brief Overview of Anatomy and Function
3 Main Sections of the GI System
There are just three main sections of the GI system, as seen in Figure 1.
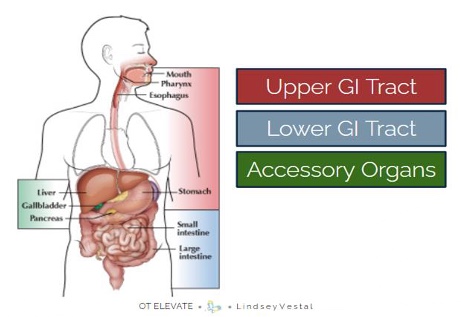
Figure 1. Three main sections of the GI System. (Click here to enlarge this image).
As you can see with my color coding, the upper GI tract, the lower GI tract, and the accessory organs are clearly outlined.
Upper GI Tract
The upper GI tract consists of the mouth, esophagus, stomach, and the first part of the small intestine, known as the duodenum. This section of the gastrointestinal system plays a critical role in digesting food and preparing the body to absorb key nutrients. However, when this part of the body isn’t functioning optimally, it can lead to symptoms such as burping, difficulty swallowing, heartburn, acid reflux, upset stomach, or abdominal pain. These are clear indicators that something might be amiss in the digestive process.
Lower GI Tract
Let’s move on to the lower GI tract. The lower GI tract runs from the small intestine to the large intestine, including the rectum and anus. While technically referred to as the small and large intestines, many of our clients commonly refer to this area as their "guts." As food travels through the colon, water and salts are absorbed, and once all the nutrients have been extracted, the remaining material is formed into stool. This stool then moves into the rectum, where it is eventually expelled as waste.
When issues with the lower GI tract occur, the symptoms can present differently than those in the upper GI tract. These problems may include abdominal pain and discomfort, but we often start to see additional signs such as bloating, distension, diarrhea, constipation, fecal incontinence, or difficulty passing food or stool. Sometimes, these symptoms occur in combination, highlighting the complexity of lower GI tract issues.
Accessory Organs
Figure 2 shows the helper organs.
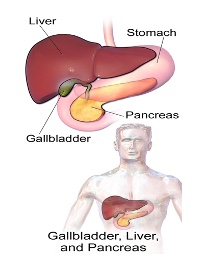
Figure 2. Examples of accessory or helper organs.
The accessory organs, which include the liver, gallbladder, and pancreas, play a crucial role in digestion by aiding the GI tract in breaking down food. However, they are not part of the series of hollow tubes that food physically passes through during digestion. What makes these organs so fascinating is how they secrete substances, like bile and enzymes, directly into the GI tract, which are essential for chemical digestion. They are considered "accessory" because they support the digestive process without being part of the actual path food travels through.
Before we dive into the next slide, I want to talk about mnemonics. I’m a huge fan of them and constantly look for ways to make this information easier to remember. Mnemonics are such a helpful tool for breaking down and retaining complex concepts, and I find they can really make learning this material more approachable and fun.
GI Tract Mnemonic: MOSS is a DJ in LA
Before we move on to the next slide, I want to share one of my favorite tools for remembering complex information—mnemonics. I’m a big fan of using them to make learning easier and more engaging. To help remember the accessory organs of digestion, I came up with this mnemonic: Moss is a DJ in LA (Figure 3). It’s a simple way to connect the key players—the liver, gallbladder, and pancreas—to their role in digestion, making it a little easier to recall when needed.
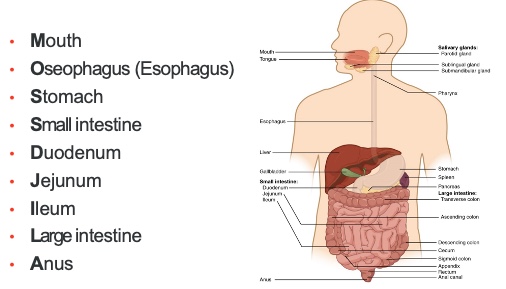
Figure 3. GI Tract Mnemonic. (Click here to enlarge the image.)
This mnemonic helps us remember the path that food takes through the digestive system. In just a moment, we’ll watch a great animation that illustrates this process. It all starts in the mouth, then moves to the esophagus—yes, spelled the British way here, because "Moss" seemed like a much more fun name for a DJ than "Mess." So, "Moss is a DJ in LA" not only gives us a memorable phrase but also helps us connect the acronyms for the key elements involved.
Video: GI Tract in Action
This video, which runs about two and a half minutes, was originally created for kids, making it both fun and engaging—though it does come with a rather annoying song! I’ll talk you through it while it plays, and I should mention it’s a bit repetitive, which I actually find helpful. Going over concepts multiple times can reinforce understanding.
The video starts with someone chewing, and that’s a great thing. Ideally, we should chew about 30 to 40 times to promote saliva production. Once the food is swallowed, it moves down the esophagus, which we’ll see here. This process is driven by peristalsis—those wave-like contractions that push the food along to the stomach. Once in the stomach, acids get to work breaking down the food further.
As the food progresses through the stomach, it becomes something called chyme, which we’ll see next. This is where enzymes enter the picture, breaking down the food even further. These nutrients are absorbed through the walls of the intestines, which have villi to increase surface area and optimize absorption. What we’re seeing here illustrates how those nutrients are taken in to fuel the body.
As we follow the chyme further down the line, it reaches the large intestine. This is where water and electrolytes are removed. What remains after this process is stool, which then moves to the rectum and exits the body through the anus. That’s the full journey!
How Is Food Digested?
All right, so how is food actually digested? It’s a pretty fascinating process because it involves a combination of two methods: mechanical digestion and chemical digestion. Mechanical digestion starts the moment you take that first bite of food. It continues as you chew, breaking the food into smaller and smaller pieces with your teeth, preparing it for the next stage of digestion. This physical breakdown is an essential step to ensure that the food is ready for the chemical processes that follow.
Mechanical Digestion
Mechanical digestion is such a fundamental part of the process that it has to happen first to ensure chemical digestion can be effective. Those 30 to 40 chews really make a difference because they set the stage for the next step, chemical digestion. What’s also fascinating about mechanical digestion is how it significantly increases the surface area of the food. This increased surface area allows digestive enzymes to work more efficiently, breaking down the food at a chemical level and preparing the body to absorb nutrients more effectively.
Chewing
Chewing breaks food down, and while it may sound excessive, chewing each bite of food 30 to 40 times is actually a magic number for a reason. This amount of chewing breaks the food down enough to lose its texture and form what’s called a bolus, jumpstarting the digestive system. By doing so, it takes pressure off the stomach, which no longer has to work as hard to process the food.
Another significant benefit of thorough chewing is that it activates the parasympathetic nervous system, also known as the "rest and digest" state. This is essential not only for handling daily stress but also for maximizing nutrient absorption. To properly digest food and absorb nutrients, we need to be in this parasympathetic state.
In my private practice in New York City, I often observed clients eating on the go—on the subway, between meetings, rushing from one place to the next. They were distracted, anxious, and far from being in a parasympathetic state. While that was their reality, our clients may have their own version of this—whether it’s eating at their desk, in the car, or while managing family chaos.
That’s why, in addition to emphasizing thorough chewing, I always recommend blocking out time for meals. Even just 15 minutes dedicated to eating lunch or dinner in a focused, calm way can make an enormous difference in digestion and overall well-being. It’s not just about what we eat, but also how we eat.
Chemical Digestion
Digestive enzymes play a critical role in digestion by breaking down large, complex molecules—like proteins, carbohydrates, and fats—into smaller ones that can be easily absorbed into the bloodstream and transported throughout the body. These enzymes are released not only when we start eating but also in anticipation of eating, triggered by our sensory system. When we smell, taste, or even see food, it sets the stage for chemical digestion and primes the body for the digestive process.
Now, let’s segue into another essential aspect of digestion: reflexes. Reflexes are those involuntary or automatic actions the body performs in response to a stimulus—completely without conscious thought. They’re a vital part of how our digestive system functions, ensuring that processes happen smoothly and efficiently without us even having to think about them.
Gastrocolic Reflex
We can educate our clients about key reflexes to empower them to understand and optimize their digestive health. One of the most important reflexes to discuss is the gastrocolic reflex. This reflex is responsible for the urge to defecate and the movement of digestive materials into the small intestine, creating room in the stomach for new food. It also increases movement throughout the GI tract and is triggered by stretching within the walls of the stomach and colon.
What’s fascinating is how this reflex works in response to eating and also within about 20 minutes of waking up in the morning. This knowledge can be transformative for clients. For example, I often suggest they try waking up a few minutes earlier to allow time for the reflex to naturally activate. Another effective strategy to kickstart the gastrocolic reflex is drinking a warm beverage in the morning. The combination of waking up earlier, slowing down to enter a parasympathetic state, and enjoying a warm drink can create the perfect environment for the "call to stool" to be more evident and manageable. This small, intentional shift in their morning routine can have a significant impact on digestive health and overall well-being.
Constipation in Pregnancy and Causes
Constipation during pregnancy is surprisingly common, with research indicating that 11 to 38% of pregnant individuals experience it. In fact, it’s the second most common GI complaint during pregnancy, coming right after nausea.
But why is constipation so prevalent during pregnancy? It’s actually a combination of factors, and understanding these can help us guide our clients toward effective strategies for relief.
One of the primary causes is progesterone, a hormone that significantly increases during pregnancy. Progesterone slows down the digestive system, which can lead to constipation. Another factor is a reduction in physical activity, which many pregnant individuals experience at various points during their pregnancy. For some, this happens during the challenging first trimester, while for others, like myself, it occurs later, often in the third trimester. Movement is essential for promoting healthy elimination, so this reduction in activity can have a noticeable impact.
Increased water absorption from the intestines is another contributing factor. During pregnancy, the body naturally absorbs more water to support the growing baby, which can lead to harder stools. Additionally, the pressure from the expanding uterus on the intestines further slows digestion.
Finally, those essential prenatal vitamins, particularly the iron they contain, play a role. While iron is crucial for preventing anemia and supporting a healthy pregnancy, it is well-known for contributing to constipation.
We’ll explore strategies to address each of these factors, empowering clients to make small, manageable changes that can alleviate discomfort and improve their overall digestive health during pregnancy.
Behavioral Modifications to Reduce Constipation in Pregnancy
Fiber/Hydration
Behavior modifications are such a great starting point for addressing constipation—simple, conservative methods that clients can implement easily into their daily routines. One of the biggest culprits we see is a lack of dietary fiber. Americans, on average, consume only about half the recommended amount of fiber. Ideally, we should aim for 25 to 30 grams a day. A simple way to help clients with this is to ask them to track their food intake. By entering what they eat into a search engine or an app, they can quickly see how much fiber they’re getting. Most often, they’ll realize they’re not meeting the ideal intake. Helping them increase fiber consumption is one of the simplest ways to reduce constipation—just focus on doing the basics better.
Another key component is water. Drinking eight to twelve cups of water daily is essential for softening stools and keeping things moving. Warm liquids are particularly helpful as they can stimulate digestion and support the gastrocolic reflex. Again, these are incredibly simple adjustments that can make a significant difference.
Starting with these basics—fiber and water—sets the foundation for helping clients reduce constipation. These are approachable, everyday changes that can empower clients to take control of their digestive health. Fiber, in particular, is a great topic to expand on further!
Two Types of Fiber
There are two types of fiber, soluble and insoluble, and they play different roles in digestion. Soluble fiber forms a gel when it combines with water, which helps to slow down digestion. Foods high in soluble fiber include beans, lentils, oats, and psyllium husk.
Insoluble fiber, on the other hand, doesn’t break down in the digestive system. Instead, it adds bulk to the stool, helping it move through the intestines more efficiently. Foods rich in insoluble fiber include seeds, whole grains, chickpeas, and kidney beans.
For optimal digestive health, it’s best to incorporate a combination of both types of fiber. This balance helps regulate digestion, supports the body’s ability to process food, and prevents issues like constipation.
Intention + Slowness Is Key
Adding fiber gradually is crucial for supporting digestive health, as the colon prefers slow, steady adjustments. Encouraging your clients to track any changes they experience is an essential strategy. The goal is to help the colon adapt gently to the increased fiber intake while monitoring how it impacts stool consistency and the overall experience of elimination.
It’s important to ask clients about their experience: Was elimination easy? Did it feel comfortable? These conversations provide valuable insights and set the stage for collaborative problem-solving during follow-ups. Together, you can evaluate whether additional adjustments are needed to achieve the desired outcome.
When increasing fiber, start with a slow increase of about 3 to 5 grams per week. This gradual approach helps the body adjust without causing discomfort or bloating. There’s no one-size-fits-all solution—each person’s body responds differently. You can guide clients toward sustainable and effective changes by tailoring the plan and maintaining open communication.
Top Tips for Increasing Fiber
Here are some simple, practical tips for busy clients to increase their fiber intake:
Start with a high-fiber cereal—an easy and quick breakfast option. Adding wheat bran to their cereal is another effortless way to boost fiber content. Encourage clients to take a closer look at the grains they’re consuming, as whole grains generally have much more fiber than refined options.
Suggest simple swaps, like using whole grain flour or bran in baking. These small changes can significantly increase fiber intake without altering their usual routines too much.
Finally, remind them to incorporate more legumes, fruits, and vegetables into their meals. These are excellent natural sources of soluble and insoluble fiber, and they can be added to meals in straightforward ways—think lentils in soups, beans in salads, or extra veggies in stir-fries. These tweaks are manageable for even the busiest schedules and can make a meaningful difference.
Hydration
Let’s break water intake down a bit more. The optimal amount is about half your body weight in ounces per day, but it’s just as important to sip water throughout the day rather than chugging it all at once. I like to compare this to watering a plant that’s been neglected. If you go on vacation and forget to water your plant, then come home and pour a large amount of water into it all at once, you’ll likely see soil runoff. The soil, being so dehydrated, can’t absorb the water properly.
Our bodies react in a similar way. Even if we’re dehydrated, we can’t fully absorb water if we take it in all at once. Sipping consistently throughout the day allows the body to stay hydrated and process the water effectively.
Half your body weight in ounces is a general guideline, but hydration needs can vary. To make this recommendation more personal and relatable, I share a visual with my clients (Figure 4) to help them understand and apply this concept in their daily lives.
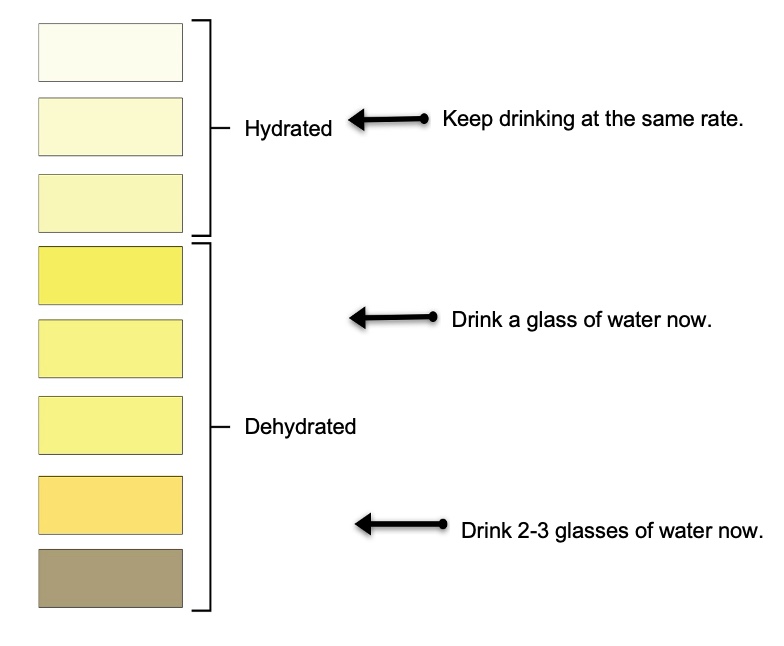
Figure 4. Optimal water intake scale.
It’s such a simple concept, but tracking hydration can make the idea of staying hydrated feel less abstract. One helpful way to assess hydration is by observing the color of urine. Ideally, we want to aim for the hydrated color range. For clients who like to be precise, they can measure their urine output as well. Eliminating about 1,300 milliliters of urine in a day is a good indicator of proper hydration.
To track this, clients can use a collection hat like the ones provided in hospitals. It’s easy to place in the toilet bowl and allows them to measure how much they’re outputting. For those who prefer to keep it simple, the urine color guide can be a great tool. If their urine falls into the middle zone, it’s a sign to grab a glass of water. If they notice a dehydrated color, drinking a couple more glasses of water—while still sipping—can help restore balance.
So far, we’ve talked about fiber and water as key components for improving digestion and maintaining overall health. Let’s continue building on these foundational practices.
Goal: Bristol Stool Chart
What’s the goal? What are we aiming for when it comes to stool? After all, this is a course about constipation, so understanding what healthy output looks like is key. That’s where something like the Bristol Stool Chart, shown in Figure 5, becomes incredibly useful. It’s a straightforward tool that helps both clients and practitioners identify and discuss stool consistency, providing a clear benchmark for what we’re working toward.
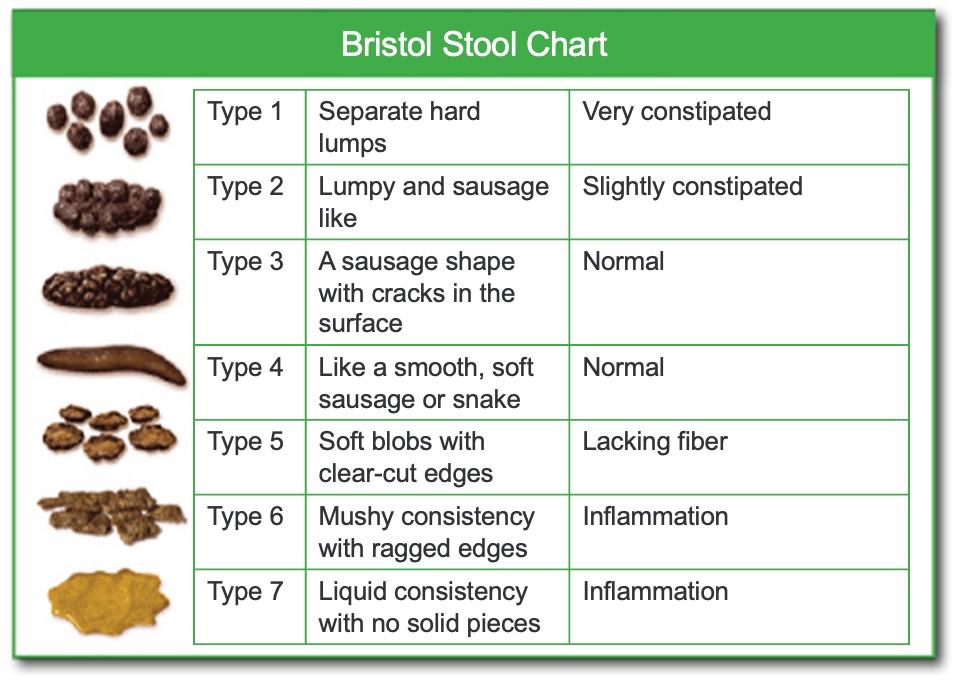
Figure 5. Bristol Stool Chart. (Click here to enlarge the image.)
I love using the Bristol Stool Chart because it allows us to have concrete, clear conversations with clients about something they likely don’t have the vocabulary for. I bring the chart with me to sessions, hand it to them, and ask, "What does your stool look like?" They can then use the images and descriptions to identify what best matches their experience.
When we’re looking at types, anything in the range of type 1, type 2, or type 3 generally indicates constipation, with type 1 and type 2 being more severe. On the other end, types 5, 6, and 7 suggest a lack of fiber and lean more toward diarrhea. This chart not only helps us pinpoint where they are but also gives us a clear starting point for discussing strategies to move toward that optimal zone of healthy digestion.
Behavioral Modifications to Reduce Constipation In Pregnancy, Cont.
Let’s tackle the main reasons why constipation happens and explore actionable solutions and alternatives to help our clients.
One major factor we discussed is the reduction in physical activity, which can occur for many reasons. Encouraging gentle movement is a powerful way to support digestion and bowel regularity. It’s essential to link these recommendations back to your client’s goals to make the changes meaningful for them. For example, something as simple as a short walk around the block, practicing yoga, or swimming (a personal favorite when I was pregnant) can stimulate bowel movements and improve overall digestion. However, it’s crucial not to just throw out generic suggestions—take the time to ask your clients what they think is feasible and accessible for them. For some, a pool or yoga class may be unrealistic, so collaborating with them to identify practical options ensures the advice is tailored and actionable.
Another helpful strategy is eating smaller, more frequent meals. This approach supports digestion and prevents the discomfort that can contribute to constipation. Additionally, discussing safe laxatives or stool softeners with your clients can be beneficial. Many doctors recommend pregnancy-safe options, such as docusate sodium. If these changes aren’t sufficient, these medical interventions can offer some relief.
Another important consideration is to avoid constipation-inducing foods. Processed foods, refined grains, and dairy are common culprits. Encouraging clients to track their food intake and note any patterns over a few weeks can help pinpoint specific triggers affecting their digestion.
Probiotics can also play a key role in gut health. Options like yogurt, kefir, or even a probiotic supplement are great ways to introduce healthy bacteria into the gut, which can aid digestion and alleviate constipation. These small but impactful changes can make a big difference in your clients’ daily lives and overall digestive health.
Ideal Elimination Habits
How you sit on the toilet absolutely matters, and positioning can make a significant difference. Ideally, elevating the feet during a bowel movement mimics a squatting position, with the knees higher than the hips. This adjustment changes the angle of the pelvic floor muscles, allowing stool to pass more easily. It’s a small change that can make a big impact on bowel movements.
That said, this isn’t a one-size-fits-all solution. For shorter clients, especially those under 5 feet tall, or depending on the height of their toilet, a traditional stool might not be ideal. In those cases, something like a yoga block or a lower prop might work better. The goal is simply to find a way to raise the knees above the hips, which adjusts the anatomy to optimize the process.
The posture is also crucial for relaxing the muscles around the rectum. By opening up the angle between the rectum and the anus, the stool can pass with less effort. The key is to sit as comfortably as possible. If a client’s back feels tight or their hips hurt, encourage them to experiment with the angle until they find the position that works best for their body.
Equally important is listening to the body’s natural signals. When the urge to stool arises, it’s important to respond promptly. Delaying this can confuse the body and disrupt natural rhythms. Once seated, encourage relaxation, allowing the body about five minutes to move things along on its own without forcing. By combining proper positioning with an awareness of the body’s cues, clients can create conditions that support healthy and effective elimination.
Managing Constipation in Pregnancy: Tailored Strategies
Iron Supplements
Iron supplements, including those found in prenatal vitamins, can often contribute to constipation, but there are strategies to help manage this issue. Clients can talk to their healthcare provider about switching to slow-release or low-dose iron options. Sometimes, taking smaller doses more frequently throughout the day, rather than one large dose, can be more manageable and less likely to cause digestive discomfort.
Fiber and water remain key cornerstones for addressing constipation. Encouraging clients to maintain adequate hydration and gradually increase their fiber intake can go a long way in counteracting the effects of iron supplements.
Another helpful strategy is pairing iron-rich supplements or foods with vitamin C-rich foods, such as oranges, strawberries, or bell peppers. Vitamin C enhances iron absorption, helping the body make the most of the supplement while potentially reducing its side effects. These simple adjustments can make iron supplementation more tolerable and effective for clients.
Reduced Physical Activity
When addressing reduced physical activity, simple and manageable changes can make a significant difference. Encouraging clients to take 10- or 15-minute walks in the morning is a great starting point, gradually increasing that time as they feel more comfortable. Suggest walking to nearby places instead of driving whenever possible, and remind them that even small steps, like parking further away at the grocery store, add up over time. Clients often need to hear these recommendations framed within the context of their current concern—in this case, constipation—to understand how these small changes directly support their goals.
Setting a timer can also be a helpful tool for those who get absorbed in work or other sedentary activities (something many of us are guilty of). A timer can remind clients to stand up, stretch, or quickly walk around the house every hour. These mini-breaks can improve circulation, encourage digestion, and prevent prolonged periods of inactivity.
For clients who might feel resistant to formal exercise, exploring their favorite occupations can open new possibilities. Activities like light household work, gardening, or other meaningful engagements can count as physical activity while also providing emotional and nervous system regulation. Gardening, for instance, is a fantastic way to combine physical movement with a calming and rewarding hobby. By tying these activities to their personal interests, clients are more likely to stay active without feeling like they’re committing to something burdensome or unrelated to their well-being. The key is finding what resonates with the individual and reframing the activity in a way that feels achievable and relevant.
Stress
Stress plays a significant role in constipation, so incorporating relaxation techniques and creating a calming routine can make a big difference for clients. For some, traditional strategies like deep breathing or mindfulness practices resonate deeply, and they can find great value in integrating these into their daily lives. Others might benefit from more tangible activities, such as scheduling time with a prenatal massage therapist. This dedicated time away from daily responsibilities—perhaps even stepping out of the house or taking a break from caring for older children—can provide both physical relief and mental relaxation.
Creating a calming routine is another powerful tool, and it doesn’t have to be complicated. In my own home, I rely on simple rituals, especially during transitions like evening wind-down time. For instance, as the days get shorter and it gets darker earlier, I light candles to soften the atmosphere. Choosing candles with essential oils adds a sensory component, creating a soothing scent that helps signal relaxation. Turning off harsh overhead lights and opting for softer, ambient lighting can also create a more tranquil space.
Encouraging clients to adopt similar practices, such as taking a shower before bed or establishing a no-screens rule for the evening, can be incredibly effective. Adding small habits like wearing blue-light-blocking glasses while using screens or engaging in relaxing pre-bedtime activities further primes the body for rest. These simple steps can significantly reduce stress, helping both the mind and the body align with the natural rhythms that support digestion and overall well-being.
Let’s Talk Pelvic Floor/Ideal Elimination Habits
Relaxation of the Pelvic Floor
We're going to discuss some ideal elimination habits. Basically, we want the pelvic floor to relax, as shown in Figure 6.
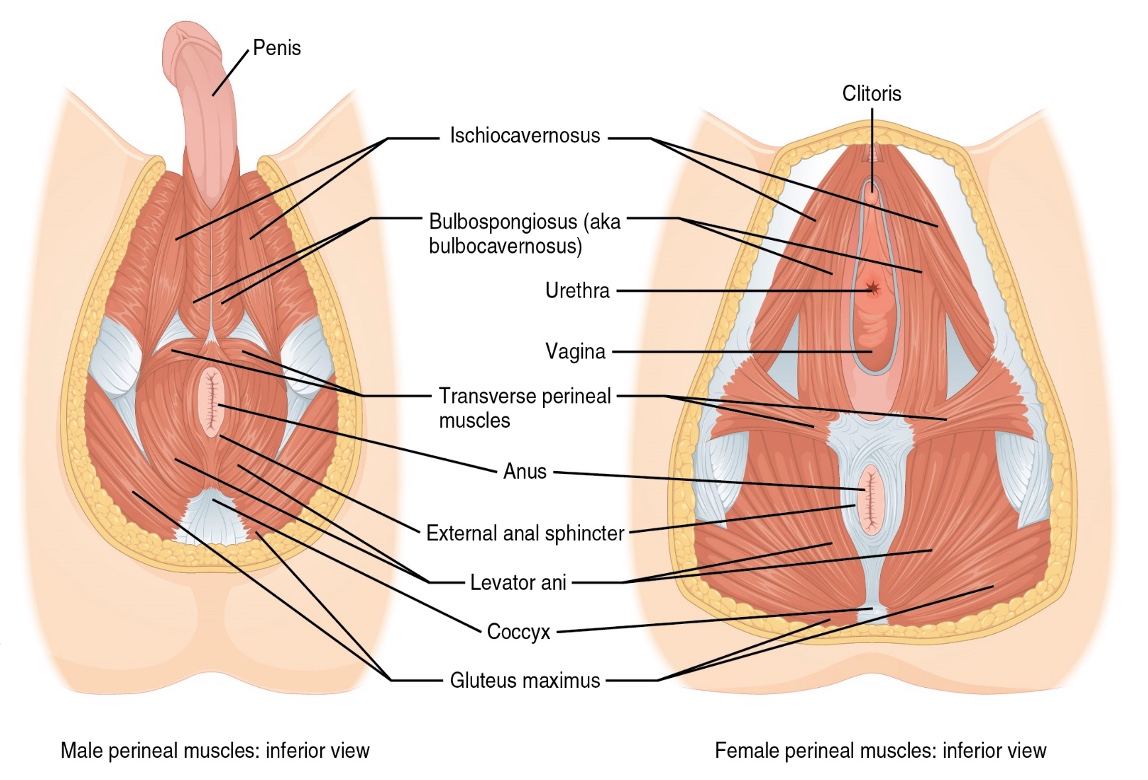
Figure 6. Male and female pelvic floor anatomy. (Click here to enlarge the image.)
Why is relaxation so important? The pelvic floor muscles, often called the "bicycle seat muscles," are capable of contracting or squeezing—something commonly associated with Kegels. But just as important as their ability to contract is their ability to relax and, even further, to yield. This is critical not only for childbirth but also for participation in intimacy and proper elimination. Referring to them as the bicycle seat muscles gives clients an immediate, visceral understanding of the area we’re talking about, as most people can easily connect with the sensation of sitting on a bicycle seat.
These muscles have important jobs. One is to facilitate elimination—helping release urine and stool when it’s time to go. The other is to retain them when it’s not the right time. Each of these actions requires distinct motions of the muscles, which tie back to their range of motion. To keep urine and bowel movements in, the muscles must be able to tighten. To release them, the muscles must relax and let go. Optimal pelvic floor function requires both abilities to work in harmony.
One way we can support the relaxation of the pelvic floor is through proper "potty posture," which we discussed earlier. Ensuring the right positioning during elimination helps the pelvic floor muscles relax, making the process easier and more efficient. This balance between contraction and relaxation is key for maintaining pelvic health and ensuring the body can meet its needs effectively.
Avoid Straining
Avoiding straining during elimination is incredibly important for pelvic floor health. Straining, or extreme pushing, can create unnecessary pressure and tension. While a little effort may sometimes be necessary, many people don’t know how to push effectively. Proper guidance can be a game-changer for clients and yourself.
So, let’s dive into the question: How do you push? Proper pushing involves three key elements: activation of the abdominal muscles, relaxation of the pelvic floor muscles, and effective breathing. Holding your breath while trying to eliminate is not ideal and can make the process harder on your body.
To start, it can be helpful to take a moment to understand your habits. A little task analysis can be revealing. I invite you to try this exercise: place one hand on your belly and one on the side of your waist. You can do this exercise with me or the next time you’re on the toilet. If it feels more comfortable, you can turn off your video or find a private space to reflect.
With your hands in position, ask yourself: When you normally poop, what happens? Take a moment to feel what’s going on. Do you engage your abdominal muscles? Do you relax your pelvic floor? Are you breathing, or do you tend to hold your breath? These are things we’ve done countless times without thinking, but slowing down to observe your habits may reveal that what you think you’re doing isn’t exactly what’s happening. This simple self-check can offer valuable insights and help you better understand how to guide your clients toward healthier elimination habits.
The Importance of Breaks + Breath for Bowel Health
Some key questions I like to ask clients (or even yourself) during this process are: Did you notice if you held your breath? Did you push your belly out into your hands, or did you pull it away from them? What did you feel in your pelvic floor—was there lifting, or did it feel like a pushing out? It might take a couple of tries to notice these things, and that’s completely normal. Most of us have never paid attention to this, so understanding our natural tendencies is an excellent first step to improving how we eliminate without straining.
Now, let’s discuss eliminating properly without straining, a common issue. First, begin in an optimal toileting position. Ideally, your feet are elevated, your hands are supported on your knees, and you’re leaning forward—not slumping, but with a gentle forward tilt. If you want to try it now, even without elevating your legs, simply leaning forward can help you feel the difference. Place a hand on your belly, lean slightly forward, and relax your abdominal wall outward.
Notice how relaxing your abdominal wall allows your pelvic floor muscles to relax. This is due to the neurological relationship between the pelvic floor and the transverse abdominal muscles. For most people, these muscles contract together. Since the transverse abdominal muscles pull the belly in—leading to a pelvic floor contraction or lift—we want to do the opposite. Keeping the belly soft and relaxed helps the pelvic floor relax as well.
Let’s practice this through an exercise. Start with four or five “conscious breaths,” extending the exhale by a few seconds. Over time, you can work up to doubling your exhale length, which is great for nervous system regulation. For now, just extend the exhale slightly. This should help relax the pelvic floor muscles and initiate a sense of bowel movement.
Next, engage the power of your side waist. Instead of pushing directly into the pelvic floor—which can cause it to tighten—place your hands on your side waist with “lobster claw” fingers. Now, say the word “ssssss” a few times while keeping your hands on your waist. You’ll feel some shortening and contraction in your side waist—this is where you have strength at your disposal. Once you’ve practiced this, move your hands to your belly and make the sound “O.” You should feel your belly move forward, which relaxes the pelvic floor muscles. If “O” doesn’t work, try “Ah.”
It’s important to avoid pulling the belly in and pushing down, as this tightens the anal sphincter, which is the opposite of what we want. The goal is to widen the waist, keep the belly soft and out, and allow the pelvic floor to drop.
Who knew pooping could be this complicated, right? But most of us have never been taught this, and practicing these techniques can be transformative for our clients. It may take a little time to master, but it’s a skill that can lead to significant improvement and success.
Autonomic Quieting Techniques
Taking breaks and focusing on breathing for bowel health cannot be overstated. The nervous system's power plays a central role here, and incorporating autonomic quieting techniques is key. One of the most effective methods is diaphragmatic breathing, which involves not just the belly or chest but a 360-degree expansion that engages the sides and back of the body as well. Many clients tend to be chest breathers; some are belly breathers, but true diaphragmatic breathing ensures the entire body participates.
This is essential for parasympathetic activation and relaxation but directly impacts pelvic floor health. The diaphragm and pelvic floor are part of the same system, moving harmoniously. Since we breathe around 20,000 times a day, breathing optimally nourishes our organs, pelvic floor muscles, lymphatic system, and more. Perfecting the art of breath is foundational to pelvic health—it’s like the conductor of the entire core system.
Downtraining activities are another powerful way to help clients move into a parasympathetic state. Spending time in nature is incredibly beneficial. When I lived in New York City and later Paris, I noticed the difference between clients with access to nature and those without access. Planning weekend trips or finding small ways to connect with nature can make a huge difference for clients without regular access.
Rhythmic activities are also a great tool, as the nervous system thrives on rhythm and predictability. Simple practices like humming during elimination, gargling for 30 seconds a few times a day, or engaging in repetitive motions like cycling or walking can activate the vagus nerve and bring a sense of calmness and safety. Chewing gum is another small but effective rhythmic activity.
Social relationships are another vital component of stress management and downtraining. Community gives clients a sense of belonging and support. Asking clients if they feel supported can open doors to helping them build meaningful connections. Finding community at local yoga centers, massage centers, or even neighborhood walking groups can be incredibly beneficial for pregnant or postnatal clients.
Cold water therapy is another fascinating technique that activates the mammalian dive reflex. This can be as simple as splashing cold water on the face or, ideally, taking a cold shower. The sudden exposure to cold helps shift the body into an autonomic quieting state, essentially "hacking" the nervous system to promote relaxation.
As occupational therapy practitioners, we understand the profound power of sensory input. Incorporating these techniques into a client’s routine can create a holistic approach to reducing stress and improving bowel health, reinforcing the critical connection between the mind and body.
Orient (Dropping the Anchor) 5, 4, 3, 2, 1
Helping clients become present and anchored in the moment is a powerful way to support their overall well-being, including their digestive health. A simple and effective technique is "dropping the anchor." If a client feels stressed, overwhelmed, or caught up in anticipating the future or dwelling on the past, this exercise can ground them.
Here’s how it works:
- Name five things you can see in your environment.
- Name four things you can hear.
- Name three things you can touch.
- Name two things you can smell.
- Name one thing you might be able to taste.
I encourage clients to practice this regularly, not just during moments of stress. Incorporating it into their daily routine—maybe as a reminder to walk, stretch, or move—can make it even more effective. It’s a great way to re-center and embody the present moment.
Toilet Meditations
Another interesting concept is "toilet meditations." While it might sound unconventional, these guided practices can be incredibly helpful. A quick online search will reveal several resources, often paired with calming music, that walk clients through relaxation techniques designed for use during elimination. These meditations focus on releasing tension, particularly in the pelvic floor muscles.
Many clients rush through bathroom time, distracted by their phones or focused on what’s next. This disconnect can interfere with the body’s natural processes. By encouraging clients to slow down and become more present during these moments, they can better tune into their body's sensations and allow the pelvic floor to release fully. It’s about creating a space where they feel embodied and present, turning what might seem like a mundane or rushed task into a mindful, restorative practice.
The Client Story
The client’s story is profoundly important, and taking the time to ask about it—and truly listen—can provide critical insights into their recovery journey. This includes exploring their birth story, particularly in a postnatal summit like this. While they may have shared this story many times with family, healthcare providers, or friends, it’s about holding space for a different kind of storytelling, one that goes beyond surface-level recounting.
When a client says something like, “I’m not sure if this is related,” or “I don’t know if this is what you’re asking about,” it often is. These moments are frequently where the most illuminating pieces of their narrative emerge, pieces they may not have shared with anyone else. Some memories might feel small or insignificant to the client, but they can hold surprising weight and influence. Creating space for these stories allows clients to process their experiences and recognize that while these events may have impacted them, they don’t have to define their future.
Let me share two examples of how uncovering client stories made a profound impact on their recovery.
The first was a young client who was around 9 or 10 years old when her grandmother, who had significant medical issues, lived with her family. One day, her grandmother was rushed to the hospital in an ambulance due to fecal impaction. She vividly remembered seeing her grandmother being rushed to the hospital in an ambulance shortly before she passed away. For the client, the two events—her grandmother’s inability to use the bathroom and her passing—became linked. As she grew up, this association caused her intense anxiety, particularly when her stool consistency resembled type 2 or 3 on the Bristol Stool Chart. She hadn’t shared this story with anyone, and it wasn’t until we explored early memories around elimination that we uncovered this deep-seated fear. By working through this story, she was able to start breaking free from the cycle of anxiety that perpetuated her constipation.
The second story is of an 85-year-old client who grew up in a large family with many cousins. On one occasion as a child, he was experiencing a lot of gas, and his cousins were outside the bathroom door laughing and jeering at him. The shame and embarrassment from that moment stayed with him into adulthood, creating a sense of guardedness during elimination. He described the feeling of needing to tighten his sphincters and being hyper-aware of whether anyone could hear him, which contributed to chronic constipation. Unpacking and validating his experience allowed him to release some of the emotional tension he had carried for decades.
These stories highlight how deeply memories—whether from childhood, potty training, or stressful elimination experiences—can influence a person’s present health. Asking about their birth story or early elimination experiences, beyond the standard questions like, “How long did you push?” or “What was the delivery like?” can reveal important details. For example, questions about falls—especially on the tailbone—can illuminate issues affecting their ability to eliminate fully. Taking the time to dig deeper lets clients know you are genuinely interested in their experiences and willing to help them process these memories meaningfully.
The physical aspect of treatment is vital, but understanding a client's story's emotional and psychological layers can lead to deeper healing. By creating a space for these conversations, we help our clients address their physical concerns and reclaim their confidence and comfort in their bodies.
Not Just the Physical Work: Ask Questions
This work goes far beyond the physical aspects of treatment. It's also about exploring how clients feel about their pelvic floor muscles and the basic function of elimination. This is often where those deeper, more personal stories emerge. So, what do we do when we hear these stories? Holding space is vital, but what comes next is just as important.
First, acknowledge their experience. Let them know that what they’ve gone through was challenging and valid. Then, move toward reassurance. Occupational therapy practitioners have a natural gift for therapeutic use of self, and providing that time to process can be incredibly healing. Helping clients "complete the stress cycle" is a powerful step. Emily Nagoski’s book, "Burnout: The Secret to Unlocking the Stress Cycle," offers fantastic insights and strategies, many of which go beyond what’s included here. Examples include journaling, talking with a friend, working with a therapist, moving the body, or simply allowing themselves to have a good cry.
Additional resources can deepen our understanding as practitioners and our ability to support clients. Some resources, like Laura Moseley’s TED Talk "Why Do We Hurt?" focus on the importance of pain science, helping us and our clients better understand the body’s responses to stress and trauma. Sharing real stories of recovery, like those in the last resource link, can also be incredibly motivating and inspiring for clients, showing them what’s possible and offering hope.
Trauma-informed care is a cornerstone of pelvic health work for practitioners interested in furthering their knowledge. I’ve developed a trauma-informed pelvic health certification to help bridge this gap. Understanding and integrating trauma-informed approaches into our practice improves our ability to support clients through these loaded topics and creates a pathway for genuine recovery and empowerment. Providing these resources to clients and internalizing them in our practice equips us to handle the complexity of this work with compassion and skill.
Summary
I'd love to share some resources if you want to learn more about pelvic health. My podcast, which I’m humbled and amazed to say is in the top 5% of all U.S. podcasts, offers a wealth of information on this topic. In addition, there’s a vibrant Facebook group with over 7,000 incredibly supportive and dedicated practitioners who engage in meaningful discussions and share their expertise. On my website, functionalpelvis.com, you’ll also find a resource I created called the OT’s Map to the World of Pelvic Health. It’s a guide designed to help practitioners explore different approaches and integrate key values into their work.
Exam Poll
1)The upper GI tract includes ALL EXCEPT:
The large intestines are the correct answer.
2)Which is NOT a TRUE statement about accessory organs?
Letter C is not a true statement.
3)What is the gastrocolic reflex?
It is the urge to defecate and the movement of digestive material in the small intestines, making room for food and within the stomach.
4)What is a cause of constipation in pregnancy?
The correct answer is D, all of the above.
5)Which is NOT an example of an autonomic quieting technique to help constipation?
Hot water baths are not an example of an autonomic quieting technique so that is the correct answer.
Questions and Answers
I have a 13-year-old male client with hypotonia and severe GI difficulties. He shuts down when addressing these issues. What should I do?
Consider referring the client to a pediatric pelvic floor therapist, in-person or virtual, as they can provide tailored strategies. Address sensory difficulties with simple interventions, such as covering automatic toilet sensors with a post-it note to reduce overwhelm. Explore emotional support strategies to help manage potential shame or discomfort around the topic. Collaborate with the family and specialists to create a supportive and consistent approach.
What are effective supplements for increasing fiber intake?
Psyllium husk is a reliable option, but it’s important to consult a GP to ensure the chosen supplement is safe, non-addictive, and doesn’t interfere with other medications.
What should occupational therapy practitioners educate postpartum clients about in acute care after birth?
Provide printed resources for later review, such as a checklist for postpartum recovery. Include tips on urination (every 2–4 hours without straining), responding to bowel urges promptly, and tools like squatty potties. Emphasize the importance of pelvic floor health and introduce clients to available therapies for long-term well-being.
Why is curiosity important when educating clients about pelvic health?
Encouraging curiosity engages clients and helps them take an active role in understanding their health. Simple tools like a checklist can prompt questions and discussions, leading to a deeper understanding of elimination habits and the importance of avoiding strain.
What should OTPs know about pelvic health across a client’s lifespan?
Addressing pelvic health issues postpartum can provide long-term benefits, as many of these concerns reappear during perimenopause or menopause. Normalizing conversations about pelvic health reduces shame and empowers clients to seek support when needed.
Where can I find additional resources and training on pelvic health?
Explore Emily Nagoski's books and podcasts for insights into health and stress responses. Check platforms like occupationaltherapy.com for relevant webinars, and consider participating in community workshops to share and learn more about pelvic health.
References
Please refer to the additional handout.
Citation
Vestal, L. (2024). Constipation relief through treating the whole person: Postnatal pelvic health virtual conference. OccupationalTherapy.com, Article 5763. Available at www.occupationaltherapy.com
