Editor's note: This text-based course is a transcript of the webinar, Contextual Adaptations For The Neurodivergent Client: Pediatric Acute Care Virtual Conference, presented by Julia Colman, OTD, OTR/L, BCP.
Learning Outcomes
- After this course, participants will be able to analyze the term “neurodiversity” and list non-ableist, strengths-based language, as favored by neurodivergent individuals, to include in acute care documentation and client-centered goals.
- After this course, participants will be able to recognize barriers to care faced by neurodivergent clients in hospital settings and identify appropriate contextual adaptations to improve the overall client experience, enhance performance and participation, and produce more favorable outcomes.
- After this course, participants will be able to distinguish and apply neurodiversity-affirming, sensory-friendly practices for evidence-based provision of occupational therapy services in an acute care setting.
Introduction/Positionality Statement
- Respecting and celebrating differences in how one thinks, feels, and processes as a beautiful part of being human.
- Identity-first language
- “autistic child”
- This presentation will use non-ableist language. This is intentional, as identity-first language is favored by neurodivergent communities and self-advocates (Bottema-Beutel et al., 2021).
Today, we will discuss contextual adaptations for neurodivergent clients, focusing on their application in acute care settings.
This presentation is rooted in the belief that we should respect and celebrate the differences in how people think, feel, and process experiences as a beautiful aspect of being human. Understanding and appreciating these differences is crucial. Throughout this presentation, I will use identity-first language, which may differ from the person-first language many of you have encountered in other areas of occupational therapy practice. This choice is intentional and aligns with the preferences of the neurodivergent community.
Therefore, you will hear terminology such as "autistic child" rather than person-first alternatives. This approach reflects the non-ableist language favored by neurodivergent communities and self-advocates.
Neurodiversity Paradigm
- Social Model of Disability
- Medical Model of Disability
Within the neurodiversity paradigm, we understand that respecting others' traits and behaviors as natural to their neurological makeup is crucial. Neurodivergence is an integral part of an individual's identity. There are two different models of disability: the social and medical models.
Traditionally, the medical model has labeled neurodivergence as an innate problem within a person that needs to be fixed by the medical community. In contrast, the social model of disability views disability as originating from societal attitudes and contexts rather than being an inherent problem within the individual. Figure 1 is an illustration of the neurodiverse paradigm.
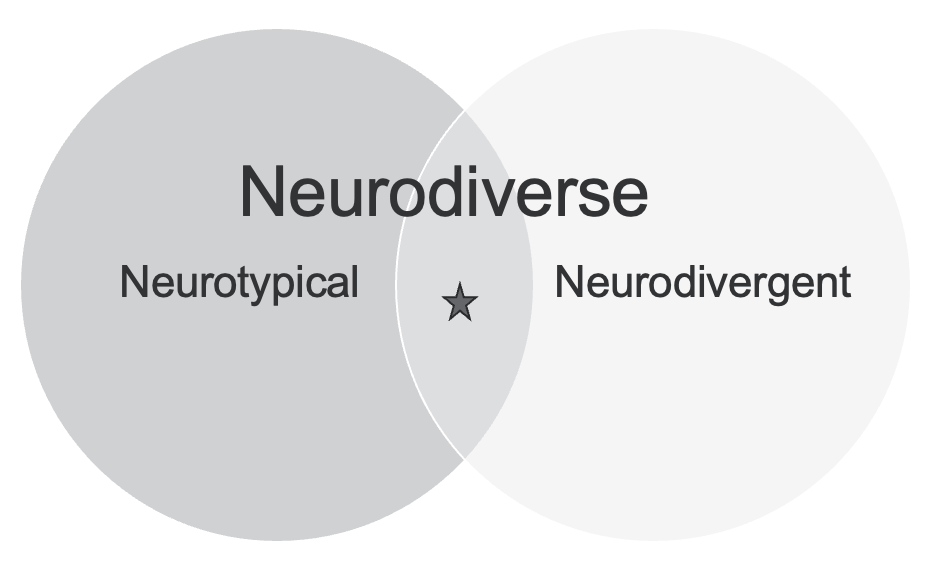
Figure 1. The neurodiverse paradigm.
Society assigns meaning to a disability, and the limitations experienced by individuals with what is labeled as disabilities often arise from societal and environmental barriers rather than innate problems within the individuals themselves. This presents a conflict in acute care practice for occupational therapy practitioners as they strive to balance the social model of disability, which emphasizes making the environment more conducive to individual needs, against the medical model of disability, which traditionally views disability as a problem to be fixed.
Several key terms are essential to understand within the neurodiversity paradigm. "Neurodiverse" refers to a group of individuals with various neurotypes. Within a neurodiverse population, there are "neurotypical" individuals who do not have differences in how their brains process the world compared to the typical population and "neurodivergent" individuals who may have conditions such as autism, ADHD, dyslexia, and other learning disabilities. Essentially, neurodiverse means a population that includes both neurotypical and neurodivergent individuals.
The traditional medical model does not affirm neurodiversity. As acute care therapists, we have an ethical obligation to shift the perspective from placing the burden of disability on the individual and focusing on what is perceived as wrong with them to identifying and addressing issues within the situation, context, or environment. This means critically evaluating how medical care is provided to neurodivergent individuals and creating systems and environments that better support their unique ways of experiencing the world.
Principles of Neurodiversity Affirming OT Practice
- Support wellbeing
- Promote capabilities
- Create meaning
- Facilitate communication
- Recognize microaggressions
- Avoid ABA approaches
(Dallman, Williams, & Villa, 2022)
Recent articles have begun to address the issue of neurodiversity-affirming practices in occupational therapy. I particularly appreciated the work by Dahlmann, Williams, and Villa from 2022, which outlines key principles of neurodiversity-affirming OT practice. These principles include supporting well-being, promoting capabilities, creating meaning, facilitating communication, recognizing microaggressions, and avoiding detrimental ABA approaches.
In the context of acute care, these principles translate to reducing systemic barriers that prevent individuals from accessing healthcare respectfully and affirmatively. This presentation explores these principles and their application in acute care settings.
Healthcare System Interaction
- Higher rates of co-occurring medical conditions compared to neurotypical children
- Limited access to effective primary healthcare
- More frequent medical encounters, hospitalizations, and procedures
- Increased incidence of restraint use and medical sedation
- Longer lengths of stay
- Higher overall healthcare costs
(Davignon et al, 2014; Wood et al., 2019)
Neurodivergent individuals encounter numerous barriers when interacting with the healthcare system. Before delving into these barriers, it's important to understand their typical healthcare experiences. Those with diagnoses falling under the neurodivergent umbrella, such as autism, ADHD, and dyslexia, often have higher rates of co-occurring medical conditions compared to neurotypical individuals.
Limited access to effective primary healthcare due to the traditional medical model's lack of neurodiversity affirmation exacerbates these challenges. This limited access leads to more frequent hospital admissions and encounters in acute care settings. Consequently, neurodivergent individuals experience more frequent medical encounters, hospitalizations, and procedures.
When admitted, they often face an increased use of restraints and medical sedation, a well-documented issue in the literature. Additionally, neurodivergent individuals tend to have longer hospital stays and incur higher healthcare costs. From a systems standpoint, there are significant implications for healthcare service delivery and cost-effectiveness, presenting opportunities for quality improvement.
However, this presentation focuses on how we can better support neurodivergent individuals in the healthcare system.
Barriers to Care in Medical Environments
- Inadequate preparation and competence of healthcare providers in treating neurodivergent populations
- Overstimulating sensory environment
- Reduced tolerance to hospital medical procedures (anxiety, agitation, behavior)
- Hospitals not sufficiently equipped (time, staffing, knowledge) to meet needs; safety risk for patients and staff
- Typical patient flow in medical settings is not considerate of neurodivergent individuals
- Poor interprofessional communication; inconsistencies in approach from provider to provider
- Ineffective provider/client/family education and interaction, Prior adverse experiences (families, patients)
(Davignon et al, 2014; Wood et al., 2019)
Neurodivergent individuals face numerous barriers when interacting with the healthcare system. Before exploring these barriers, it's important to understand their typical experiences. People with neurodivergent diagnoses, such as autism, ADHD, and dyslexia, have higher rates of co-occurring medical conditions compared to neurotypical individuals. Limited access to effective primary healthcare exacerbates these challenges, leading to more frequent hospital admissions and encounters in acute care settings. Consequently, neurodivergent individuals experience more frequent medical procedures, hospitalizations, and increased use of restraints and medical sedation, which is well-documented in the literature. They also tend to have longer hospital stays and incur higher healthcare costs. From a systems perspective, this raises significant issues for healthcare service delivery and cost-effectiveness, highlighting the need for quality improvement. However, this presentation focuses on how we can better support neurodivergent individuals in the healthcare system.
Several recent studies have examined these barriers from different perspectives. The key contributing factors include inadequate preparation and competence of healthcare providers, as many providers lack training and understanding of how to meet the needs of neurodivergent populations. This includes modifying service delivery appropriately, leading to inadequate care. Overstimulating sensory environments in hospitals, which are inherently overwhelming, can be extremely overstimulating for individuals with sensory differences, exacerbating stress and anxiety. Neurodivergent individuals often have increased anxiety and agitation related to medical procedures, with repeated negative experiences compounding this issue, leading to heightened fear and behavioral challenges.
Many hospitals are not equipped to meet the needs of neurodivergent clients due to lack of time, training, and staffing, resulting in increased use of restraints and medical sedation and posing safety risks for patients and staff. The typical patient flow in medical settings does not accommodate the needs of neurodivergent individuals, from the admissions process to transitions between settings, leading to additional stress and anxiety. Inconsistencies in approach from different providers, often due to high turnover and shift changes, can exacerbate challenges for neurodivergent patients. Consistency in care is crucial, and occupational therapy practitioners can ensure continuity by maintaining a consistent team of providers for neurodivergent clients.
Families of neurodivergent individuals often have a history of negative experiences with the healthcare system and frequently assume advocacy roles, expecting barriers and challenges. Healthcare providers need to be cognizant of these prior experiences and approach interactions with understanding and support. Occupational therapy practitioners should consider strategies to address these barriers, such as ensuring consistency in care, improving communication, and creating supportive environments. By acknowledging and addressing these issues, we can enhance the healthcare experiences of neurodivergent individuals.
The Problem
- An estimated 5% to 16% of children have sensory processing differences (and it is much higher in neurodivergent children).
- Unrealistic demands
- More stimuli
- More people/strangers
- More pain
- More unexpected events
- More changes to routine
- Adverse events & poor outcomes
(Ben-Sassoon, Carter, and Briggs, 2009; Davignon et al, 2014)
The problem is significant: an estimated 5% to 16% of all children have sensory processing differences. This statistic, though somewhat outdated, suggests that the actual percentage might be higher, especially among neurodivergent children. The 5% to 16% figure includes neurotypical and neurodivergent children, but the percentage is considerably higher when focusing solely on neurodivergent populations.
Children with sensory processing differences experience the world differently, and the hospital or acute care environment can place unrealistic demands on them. The increased stimuli, such as lights, sounds, unfamiliar people, new routines, and settings, coupled with the presence of strangers and the experience of pain, can be overwhelming. Neurodivergent individuals often have difficulty with interoception, making it harder to perceive and manage discomfort and pain, which adds to the sensory overload.
Additionally, unexpected events in the hospital setting further contribute to their stress. Healthcare providers can help mitigate this by managing expectations and reducing unpredictability. While some aspects of acute care are uncontrollable, many elements can be structured to provide clearer expectations and a more positive experience. Simple interventions, like visual schedules, can make a significant difference.
Ultimately, the current healthcare system's demands on neurodivergent individuals lead to more adverse events and poorer outcomes. Numerous articles cite poor psychosocial outcomes related to inpatient hospitalizations for these populations, including poor coping and adjustment. This often results in escalating behaviors, unsafe clinical interactions between children and staff, and the poor outcomes mentioned earlier.
Common Sensory Differences in Neurodivergent Populations
- Pain perception
- Unexpected vs. expected stimuli
- Tactile sensitivity
- Auditory sensitivity & processing
- Proprioceptive & vestibular differences
- Visual processing
- Changes in routine, structure, predictability
- Interoception (hunger/PO status, noxious stimuli, illness all unfamiliar sensations)
- Sensory overload & emotional dysregulation
Specific sensory differences significantly impact how neurodivergent individuals experience the healthcare environment. One major issue is pain perception, including the potential inaccurate reporting of pain. It is essential to be intentional about the pain scales used with neurodivergent populations and to pay attention to nonverbal signs of pain and physiological symptoms to better manage pain. Discomfort and uncertainty about the source of pain can contribute to sensory overload.
The distinction between unexpected and expected stimuli is also crucial. Simple actions, like informing the child before performing any medical procedure or changing the environment, such as turning on lights or starting a monitor, can make a significant difference. For instance, saying, "I’m going to turn on the lights now" or "You’ll hear a loud beep from this monitor" can help prepare the child and reduce anxiety.
Tactile sensitivity is another critical aspect. In an acute care setting, where a lot of touch is involved, this can be extremely uncomfortable for those sensitive to touch. Limiting the number of people who touch the child at any given time and always informing them before any contact can help. Awareness of the difference between light touch and deep pressure and how these can affect the child is essential.
Auditory sensitivity is another concern. Hospitals are filled with beeping monitors and multiple conversations, which can be overwhelming. Strategies to reduce auditory stimulation might include turning down monitor volumes, closing doors to minimize noise, and providing quieter waiting environments.
Neurodivergent individuals often have proprioceptive and vestibular differences. This requires consideration during patient transport and transfers, ensuring staff are educated about these differences and implementing sensory-based calming strategies when appropriate. Visual processing needs must also be addressed, such as giving a warning before turning on lights or reducing room lighting to prevent overstimulation. The use of visual schedules can provide structure and predictability, reducing anxiety related to changes in routine.
Interoception, which involves internal body signals like hunger and pain, is often challenging for neurodivergent individuals. Situations common in acute care, such as being NPO (nothing by mouth) for procedures, can be confusing and uncomfortable, exacerbating sensory overload. It is crucial to be mindful of these challenges and understand that sensations like hunger might not be easily identifiable for these individuals.
Medical procedures, often seen as routine, can be particularly distressing. For example, having blood pressure taken can be uncomfortable or even painful despite reassurances to the contrary. It's important to validate the child's experiences rather than dismissing their discomfort.
The unfamiliar sensations of illness itself can also be overwhelming. Not understanding what is happening to their body, why they feel nauseous, or experiencing new and uncomfortable feelings can add to the sensory overload. This overload, in turn, can lead to emotional dysregulation, including aggression and heightened fight-or-flight responses, contributing to negative interactions with healthcare providers.
Addressing these sensory differences at all levels is vital in the acute care setting. This involves creating an environment that minimizes sensory overload and supports the unique needs of neurodivergent individuals, ultimately leading to better healthcare experiences and outcomes.
OT Contextual Evaluation
- People
- Physical environment
- Systems
As occupational therapy practitioners in the acute care environment, we need to focus on how we analyze and evaluate the experiences of neurodivergent individuals. While adaptations to the physical environment are often the first considerations when addressing sensory differences, it's crucial to consider the roles of people and systems in this context.
Firstly, we need to focus on the people involved. This includes all healthcare providers and individuals the neurodivergent child interacts with during their hospital stay. Training and educating healthcare providers about neurodiversity and sensory processing differences are essential. Providers should be equipped with strategies to communicate effectively, recognize signs of sensory overload, and approach neurodivergent patients with empathy and understanding. Consistency in care is also vital, so having a dedicated team of providers who work consistently with neurodivergent patients can reduce stress and improve outcomes.
Secondly, while addressing the physical environment, we must consider sensory-friendly adaptations to help reduce overstimulation. This includes controlling lighting, reducing noise levels, and creating spaces that provide sensory breaks. Visual schedules and other tools to manage routines can also be beneficial. Ensuring that the physical space is adaptable to the sensory needs of neurodivergent individuals is a key component of creating a supportive environment.
Lastly, examining the system level involves evaluating hospital policies and procedures. It's important to assess how these policies either support or hinder the experiences of neurodivergent individuals. For example, policies related to patient flow, admission processes, and waiting periods should be reviewed to ensure they accommodate the needs of neurodivergent patients. Hospitals should implement protocols prioritizing sensory considerations and facilitating smoother transitions and procedures for these individuals.
People: Interprofessional Collaboration
- Clear communication
- Between multiple providers on the team
- Neurodiversity-affirming language in documentation
- Document sensory needs, preferences, and communication strategies in the chart
- Prepared, proactive providers
- Medical team member training on how to communicate with and approach neurodivergent patients (Davignon et al., 2014)
- Professional development resources and toolkits that increase competency and confidence in working with neurodivergent individuals are essential (Straus et al., 2018).
- OT led in-services
- Understand individual needs, challenges, and strengths
- Gather baseline information
- Intake sensory assessment (Thom et al., 2020)
First, let’s focus on the people involved. One crucial approach to improving care for neurodivergent individuals is through interprofessional collaboration. Clear communication between all providers on the team is essential. Providers should consistently use neurodiversity-affirming language and documentation. As occupational therapy practitioners, we must lead this effort because the medical field may not yet fully embrace these practices. We can influence others through education and consistent application by setting an example.
Documentation is critical. We should meticulously document sensory needs, preferences, and communication strategies in patient charts. This includes noting if a patient uses an AAC device, prefers nonverbal communication, or has specific interaction preferences, such as not making eye contact. Our OT documentation should have a dedicated section in the evaluation template for these sensory needs and communication strategies. This practice should become standard.
Providers need to be prepared and proactive. Instead of waiting for a child to escalate or exhibit aggressive behaviors, training should focus on best practices for communicating and approaching neurodivergent patients. This involves professional development resources and toolkits to enhance competency and confidence in working with these individuals. As occupational therapy practitioners, we should lead by providing training and education to the rest of the team through OT-led in-services and journal clubs. Teach your team about neurodiversity-affirming care in the acute care setting, and make necessary adjustments to documentation and evaluation processes. Consistency in care is vital, so ensuring neurodivergent patients see the same OT consistently can help.
Understanding individual needs, challenges, and strengths is another key aspect. Gathering adequate and accurate baseline information early in hospital admission is crucial. Often, I’ve encountered patients whose neurodivergent status was not noted in their charts, leading to missed opportunities for tailored care. As suggested by Thom and colleagues in 2020, intake sensory assessments should be integrated into the hospital’s intake process. This assessment can provide valuable information about intellectual abilities, functional abilities, preferred communication styles, sensory needs, sensory triggers, and sensory supports.
From the start, providing preferred sensory comfort items can help create positive sensory experiences and prevent behavioral escalations. By gathering this baseline information early, we can proactively support neurodivergent individuals, addressing their needs and preventing agitation from the beginning of their hospital stay.
People: Family & Client-Centered Care
- Family preparation
- Encourage bringing sensory supports when able
- Anticipate and actively make attempts to reduce barriers
- Education on post-op and post-hospitalization expectations
- Individual education, preparation, management of expectations
- Transparency, trust, play
- Explain each step
- Allow the child to examine the instruments/tools and model on a trusted adult
- Verbal warning before touch, deep pressure/sustained input versus quick, light touch
- Maintain home routines when possible
- Visual schedule
- Use of visual timers
- Adjust communication style
- Understand differences in communication
- Intentional effort to meet individual’s needs
- Access to AAC, sign language interpreter if needed
(Davignon et al., 2014; Sadatsafavi et al., 2023; Straus et al., 2018)
When considering the people involved in providing care, it is crucial to focus on family and client-centered care. This involves adequately preparing families, educating them and the patient, managing expectations, maintaining home routines as much as possible, and adjusting communication styles based on the patient’s needs.
Family preparation is essential. Encourage families to bring sensory supports when possible, especially during planned admissions or procedures, as neurodivergent individuals often undergo more planned procedures and are sedated more frequently than neurotypical patients. By bringing familiar sensory supports, the experience can be made more comfortable. It's also important to anticipate and actively attempt to reduce barriers. If specific triggers are known, the team should be aware and work to avoid them. Education on post-operative and post-hospitalization expectations is vital, including what the procedure entails, the typical length of stay, which providers will be involved in, and any precautions that need to be followed. This preparation helps families and patients anticipate and manage their hospital experience more effectively.
On an individual level, transparency is key. Explaining what to expect, developing trust, and using a play-based approach can help. Always explain each step of a procedure and outline expectations. Allow patients to examine instruments or tools and model procedures on a trusted adult when possible. Provide verbal warnings before any touch and use deep pressure instead of quick, light touch to significantly reduce agitation.
Maintaining home routines as much as possible can be very beneficial. Use visual schedules and timers, especially if the patient is accustomed to these tools at home. These supports can help manage transitions and changes in routine. Adjusting communication style to match the patient’s needs is also critical. Neurodivergent individuals may require verbal, written, or picture-based explanations and instructions. When creating home education programs or instruction materials, include pictures and diagrams and offer verbal or demonstrative instructions if beneficial.
Neurodivergent children often have difficulty expressing their needs, particularly when scared, overwhelmed, or experiencing sensory overload. Ensure they can access their AAC devices, as communication can become even more challenging without these tools. It is unfair and detrimental to their well-being when these devices are unavailable in a hospital setting. Additionally, provide access to ASL interpreters when needed and recognize that non-speaking individuals can still communicate through other methods.
Understanding that some neurodivergent individuals process information better without forced eye contact is also important. Eye contact can be extremely uncomfortable and lead to heightened anxiety and distress. Respect their preferences for familiar caregivers and try to keep these consistent throughout the hospital admission to provide a sense of stability and comfort.
In summary, focusing on family and client-centered care involves adequate preparation, education, and communication tailored to the individual’s needs. By creating a supportive and understanding environment, we can significantly improve the healthcare experience for neurodivergent individuals.
Physical Environment
- Sensory-Friendly Environmental Modifications
- Use of natural lighting, avoid or cover fluorescent lights
- Access to a private room
- Cluster care
- Close the door to room
- Quiet waiting areas
- Respect tactile differences-gloves?
- Smells-essential oils?
- Alternative seating options in hospital room
- Designated “safe” (no procedure) space in room
- Lower volume of machines, respond quickly to monitor beeps
- Sensory Toolkit
- Noise-canceling headphones
- Weighted blanket
- Sunglasses
- Fidget and sensory toys
- Neurodiversity affirming storyboard about hospital stay
- Provide a visual handout of sensory tools available
- Tablet with mindfulness, stress reduction, progressive muscle relaxation, breathing strategies, visual apps
- White noise machine
When considering modifications to the physical environment for neurodivergent patients in acute care, it is important to implement sensory-friendly adaptations supported by the literature. Here are some key modifications to consider:
One recommendation is to use natural lighting instead of fluorescent lights. While specific procedures may require strong lighting, efforts should be made to dim or cover fluorescent lights at other times to create a more calming environment.
When feasible, access to a private room can significantly reduce overstimulation and provide a more controlled and comfortable space for the patient. This is more practical in some settings than others, but it should be prioritized whenever possible.
Clustering care involves scheduling and grouping necessary procedures together to minimize disruptions. For instance, if the nurse needs to administer medication and the nurse assistant needs to take vitals, coordinating these tasks consecutively can provide the patient with longer, uninterrupted rest periods.
Closing the door to the room and providing quiet waiting areas can help reduce auditory overstimulation. This, combined with respecting tactile differences, such as minimizing gloves when possible, can significantly improve comfort.
Consideration of smells and the use of essential oils can also be beneficial. Many children's hospitals have policies for essential oils, which can be used in diffusers to provide a calming atmosphere, though it’s important to be aware of any contraindications and work within the hospital’s guidelines.
Alternative seating options in the hospital room, such as chairs or couches, allow patients to move out of bed and can make their stay more comfortable. A designated safe space, like a no-procedure area, can also help. For example, if a couch is designated as a no-procedure space, the child can retreat without fear of being poked or prodded.
Responding quickly to monitor beeps and keeping the volume of machines low can reduce auditory overload. Sensory toolkits should be readily available and could include noise-canceling headphones, weighted blankets or lap pads, sunglasses, fidgets, sensory toys, and neurodiversity-affirming storyboards that explain what to expect during the hospital stay.
Additionally, providing a visual handout of available sensory tools and ensuring access to tablets equipped with mindfulness apps, stress reduction exercises, progressive muscle relaxation, breathing strategies, and visual apps can be highly beneficial.
Lastly, white noise machines or vibrating devices can offer positive sensory experiences, helping to create a more comfortable and supportive environment for neurodivergent patients. By implementing these modifications, we can create a neurodiversity-affirming environment that supports the unique sensory needs of these individuals, leading to better healthcare experiences and outcomes.
Systems
- Preventative Care
- OT addition to primary care teams
- Effective caregiver and patient training on precautions, discharge recommendations to reduce readmission rates
- Staffing considerations
- Consistent caregivers (including OT)
- Reduced # of providers in the room at one time
- One person talking at a time (co-treatments?)
- Mandatory education on neurodiversity affirming distraction techniques, safe de-escalation strategies
- Allow the child to move at their own pace
- Consider- productivity requirements
- Give the child space or a break when needed
What can we do at the systems level? In terms of preventative care, this is the bigger picture. Figure 2 shows the different levels of healthcare delivery.

Figure 2. Different levels of healthcare delivery.
In addition to the actions you can take as individual occupational therapy practitioners (OTPs), there is a pressing need for broader changes in healthcare policy, hospital system policy, and departmental policies and procedures to make a long-term impact. While individual efforts are crucial, widespread systemic change is also necessary.
Preventative care is one area where change is essential. Advocating for including OTPs in primary care teams can help reduce hospital admissions by providing more effective neurodiversity-affirming primary care. Effective caregiver and patient training on precautions and discharge recommendations can reduce readmission rates. Often, the emphasis during hospital stays shifts to managing immediate safety concerns, particularly when dealing with agitation or aggressive behaviors, which can detract from thorough discharge preparation. Ensuring that families receive adequate training and discharge recommendations is vital for preventing readmissions and improving the overall experience for the child.
Staffing considerations also play a significant role. Consistent caregivers and reducing the number of providers in the room simultaneously can help minimize overstimulation and agitation. For example, I once encountered a situation where an autistic child became extremely agitated when ten people, including residents, doctors, a nurse, and myself, were in the room simultaneously. The immediate reaction was to consider restraints, but once everyone except one person left the room, the child de-escalated, and the situation improved. This experience highlights the importance of reducing the number of providers present and having only one person speak at a time. Occupational therapy practitioners should consider whether co-treatments are appropriate or if individual sessions might be less overwhelming.
All providers in acute care settings should be required to undergo mandatory education on neurodiversity-affirming distraction techniques and safety escalation strategies, similar to the training required for educational staff in some regions. Allowing children to move at their own pace is also crucial. Productivity requirements often assume that sessions will proceed smoothly without interruptions, which is unrealistic when working with children with sensory processing differences. Meeting the child where they are and being flexible with session pacing is essential.
Finally, giving the child space or a break when needed is important for managing sensory overload and preventing escalation. These changes, combined with the individual actions occupational therapy practitioners can take, will create a more supportive and effective healthcare environment for neurodivergent individuals.
- Wait times
- Advocate for admission & registration in hospital room or treatment room, reduced room changes
- Call to schedule an OT session (& show up as scheduled or communicate otherwise)
- Smooth service transitions
- Effective goal writing
- Utilize EMR-outpatient visits, previous evaluations
- Neurodiversity affirming discharge recommendations
In addition to the individual actions you can take as occupational therapy practitioners, it’s crucial to consider systemic and policy-level changes to improve the care of neurodivergent individuals. Here are some key areas to focus on:
Reducing wait times and minimizing the number of transitions can significantly improve the patient experience. Whenever possible, advocate for admissions and registrations in the patient's hospital or treatment room, especially for planned procedures. Streamline the process to reduce room changes throughout their stay, such as minimizing transfers from the procedure room to the PICU and the floor.
Instead of just showing up for OT sessions, call to schedule them and communicate any changes promptly. This approach can help manage expectations and reduce anxiety for both the patient and their family.
Ensure smooth transitions by writing effective goals and utilizing electronic medical records. Review outpatient visits if the child is seen within the same healthcare system. Understand what the outpatient therapist has been working on and which strategies have been effective. This knowledge can inform your initial acute care evaluation and provide continuity of care.
Provide discharge recommendations that affirm neurodiversity and are tailored to the individual's medical status and needs. Avoid automatically recommending outpatient OT just because the patient is autistic. Assess whether such services are necessary based on their medical status and specific needs during their hospital stay.
Continue to prioritize family and client-centered care by adequately preparing families, managing expectations, and maintaining home routines as much as possible. Encourage families to bring sensory supports and prepare them for what to expect during and after hospital procedures. Provide clear, concrete, and literal patient education to ensure understanding.
Advocate for mandatory education on neurodiversity-affirming distraction techniques and safety escalation strategies for all healthcare providers in acute care settings. This training is essential to creating a supportive environment and effectively managing sensory overload and behavioral escalations.
Implement sensory-friendly environmental modifications such as natural lighting, access to private rooms, clustering care tasks, reducing auditory and tactile stimuli, and providing sensory toolkits. Ensure these modifications are integrated into hospital policies and procedures to standardize care.
Aim for consistent caregivers and limit the number of providers in the room at the same time to reduce overstimulation. This approach can help prevent agitation and improve the overall patient experience.
Advocate for including occupational therapy practitioners in primary care teams to provide more effective preventative care and reduce hospital admissions. Effective caregiver and patient training on precautions and discharge recommendations can also help reduce readmission rates and improve long-term outcomes.
By combining these systemic and policy-level changes with individual actions, occupational therapy practitioners can create a more supportive and effective healthcare environment for neurodivergent individuals, leading to better healthcare experiences and outcomes.
Case Example
Sensory Friendly Strategies Case Example | |
AJOT: Many Hands Working Together: Adapting Hospital Care to Support Autistic Children's Mental Health | Individual Goal Example:
Child will take oral medications with visual cues and the use of preferred sensory strategies for improved coping and adjustment throughout hospitalization.
|
Abstract Importance: Hospitals pose a threat to autistic children's mental health. Adapting hospitals to meet children's needs can address this issue. Objective: To determine the impact of an interprofessional program (Adaptive Care) to support autistic children's mental health on nursing staff's knowledge, efficacy, and confidence. Design: Pretest-posttest, quasi-experimental design. Setting: Large pediatric hospital. Participants: Nursing staff were the first participants in the program implementation. Approximately 300 nursing staff received training through the program, and 107 completed program evaluation surveys. Of these, 18 nursing staff completed both the pretest and posttest surveys approximately 1 yr apart. Intervention: Occupational therapy practitioners and other professionals developed and implemented the program, which consists of staff training and resources to adapt hospital physical and social environments and to ultimately improve patients' hospital experiences. Outcomes and measures: Researcher-developed, pilot-tested, online survey to assess knowledge, perceived effectiveness, confidence, and strategies that staff used while caring for autistic children in the hospital. Results: Respondents had increased effectiveness and confidence working with autistic children in the hospital after program implementation. Respondents reported significantly more strategies to care for autistic children. Conclusions and relevance: Interprofessional collaboration and programming can positively affect social environments in the hospital by enhancing nursing staff's self-efficacy, confidence, and strategies to support mental health and to enhance health care for autistic children. | |
Lastly, here is a case example of how a hospital has successfully implemented these changes to support the mental health of autistic children. Recognizing that hospitals can pose a threat to the mental health of these patients, this large pediatric hospital made significant systems-level changes to meet their needs. The nursing staff were trained to provide neurodiversity-affirming care, and occupational therapy practitioners and other professionals developed a comprehensive program. This program included staff training and resources to adapt both the physical and social environments of the hospital to improve the patients' experiences.
The results were positive. Respondents noted increased effectiveness, and nurses reported greater confidence when working with autistic children after the program’s implementation. Additionally, they felt that they had significantly more strategies for caring for autistic children.
One practical takeaway for occupational therapy practitioners is incorporating sensory-friendly goals into acute care evaluations. For example, you might write a goal: "The child will take oral medications with visual cues and use their preferred sensory strategies for improved coping and adjustment throughout their hospitalization." This goal combines the necessary medical outcome—taking medications—with the sensory-based strategies that can help achieve it without causing distress or leading to oral aversions.
Integrating these approaches into your practice can help create a more supportive and effective healthcare environment for neurodivergent individuals, ultimately improving their overall hospital experience and outcomes.
Practical Takeaways
- Consider the ways that you, as an OTP, can promote positive change at various levels
- Use sensory-friendly, neurodiversity-affirming strategies in your individual sessions and documentation,
- hold in-services and educational sessions for other healthcare providers that you work with,
- & ask your administrators how you can help make the hospital more sensory-friendly.
I want you to consider how you, as an OTP, can promote positive change at various levels. You can use these sensory-friendly neurodiversity-affirming strategies in your individual sessions and in your goals. You can hold inservices and educational sessions for other healthcare providers that you work with, and you can ask your administrators how you can help them make the hospital more sensory-friendly.
Summary
Hopefully, you feel that you met many of these learning outcomes and learned something from this presentation. Let's go to our exam poll.
Exam Poll
1)What is a principle of neurodiversity affirming OT practice?
It is all of the above. We want to support well-being, promote capabilities, and create meaning for our patients.
2)Which is a TRUE statement about neurodiversity and healthcare system interaction?
The answer is B. Neurodivergent individuals indeed have limited access to effective primary healthcare.
3)What is a barrier to care for neurodiverse clients in medical environments?
The correct answer is all of the above.
4)What percentage of children have sensory processing differences (higher in neurodivergent populations)?
The correct answer is 5-16%.
5)What is an example of a sensory-friendly environmental modification?
The correct answer to the last question is B, a designated "safe" space.
Questions and Answers
How receptive are the staff to your suggestions?
I see varying levels of receptiveness. We shouldn't expect change to happen overnight. Having more of a collaborative approach leads to a higher likelihood of being implemented.
Thanks for your time and attention today.
References
Ben-Sasson, A., Carter, S., & Briggs-Gowan, M. (2009). Sensory over-responsivity in elementary school: prevalence and social-emotional correlates. J Am Acad Child Adolesc Psychiatry, 37: 705-716.
Bottema-Beutel, K., Kapp, S. K., Lester, J. N., Sasson, N. J., & Hand, B. N. (2021). Avoiding ableist language: Suggestions for autism researchers. Autism in adulthood: Challenges and management, 3(1), 18–29. https://doi.org/10.1089/aut.2020.0014
Dallman, A. R., Williams, K. L., & Villa, L. (2022). Neurodiversity-affirming practices are a moral imperative for occupational therapy. The Open Journal of Occupational Therapy, 10(2), 1–9. https://doi.org/10.15453/2168-6408.1937
Davignon, M. N., Friedlaender, E., Cronholm, P. F., Paciotti, B., & Levy, S. E. (2014). Parent and provider perspectives on procedural care for children with autism spectrum disorders. Journal of developmental and behavioral pediatrics: JDBP, 35(3), 207–215. https://doi.org/10.1097/DBP.0000000000000036
Mahoney, W. J., Abraham, G., & Villacrusis, M. (2023). Many hands working together: Adapting hospital care to support autistic children’s mental health. American Journal of Occupational Therapy, 77, 7702185040. https://doi.org/10.5014/ajot.2023.050032
Thom, R. P., Hazen, M. M., McDougle, C. J., & Hazen, E. P. (2020). Providing inpatient medical care to children with autism spectrum disorder. Hosp Pediatr, 10(10): 918–924. https://doi.org/10.1542/hpeds.2020-0140
Sadatsafavi, H., Vanable, L., DeGuzman, P., & Sochor, M. (2023). Sensory-friendly emergency department visit for patients with autism spectrum disorder—A scoping review. Review Journal of Autism and Developmental Disorders, 10(4), 684–698. https://doi.org/10.1007/s40489-022-00318-6
Salvatore, G. L., Simmons, C. A., & Tremoulet, P. D. (2022). Physician perspectives on severe behavior and restraint use in a hospital setting for patients with autism spectrum disorder. Journal of Autism and Developmental Disorders, 52(10), 4412–4425. https://doi.org/10.1007/s10803-021-05327-8
Straus, J., Coburn, S., Maskell, S., Pappagianopoulos, J., & Cantrell, K. (2019). Medical encounters for youth with autism spectrum disorder: A comprehensive review of environmental considerations and interventions. Clinical Medicine Insights: Pediatrics, 13, 1179556519842816–1179556519842816. https://doi.org/10.1177/1179556519842816
Thom, C. S., Echevarria, E., Osborne, A. D., Carr, L., Rubey, K., Salazar, E., Callaway, D., Pawlowski, T., Devine, M., Kleinman, S., Flibotte, J., & Lambert, M. P. (2020). Etiologies and sequelae of extreme thrombocytosis in a large pediatric hospital. *medRxiv, 2020.06.01.20119438*. https://doi.org/10.1101/2020.06.01.20119438
Wood, E. B., Halverson, A., Harrison, G., & Rosenkranz, A. (2019). Creating a sensory-friendly Pediatric Emergency Department. Journal of Emergency Nursing, 45(4), 415–424. https://doi.org/10.1016/j.jen.2018.12.002
Citation
Colman, J. (2024). Contextual adaptations for the neurodivergent client: Pediatric acute care virtual conference. OccupationalTherapy.com, Article 5711. Available at www.occupationaltherapy.com.
