Editor's note: This text-based course is a transcript of the webinar, Critical Rehab Needs For Acute Postpartum Patients: Postnatal Pelvic Health Virtual Conference, presented by Jenna Segraves, PT, DPT, MS, Rebeca Segraves, PT, DPT, WCS, CLT.
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
- After this course, participants will be able to differentiate signs and symptoms of critical maternal health concerns following traumatic delivery, postpartum hemorrhage, wound complications leading to embolism, preeclampsia, or maternal cardiac events.
- After this course, participants will be able to compare/contrast the rehabilitation interventions that are typically accessible to patients after knee or hip replacement with interventions accessible to patients after cesarean section.
- After this course, participants will be able to distinguish the appropriate outcome measures to screen patients who would benefit from an acute rehab evaluation in the hospital after birth to support daily occupations.
Introduction
Rebeca: We are so excited to discuss critical rehab needs for acute postpartum patients. Our hope by the end of this presentation is that you will be able to differentiate signs and symptoms of critical maternal health concerns, compare and contrast rehab interventions that are typically accessible to patients with interventions that are also accessible to patients after cesarean section, and to identify appropriate outcome measures for the perinatal population in the hospital after birth that may benefit from occupational therapy services.
Critical Maternal Health Concerns: Maternal Mortality Ratio
I want to start this talk with this graph (Figure 1).
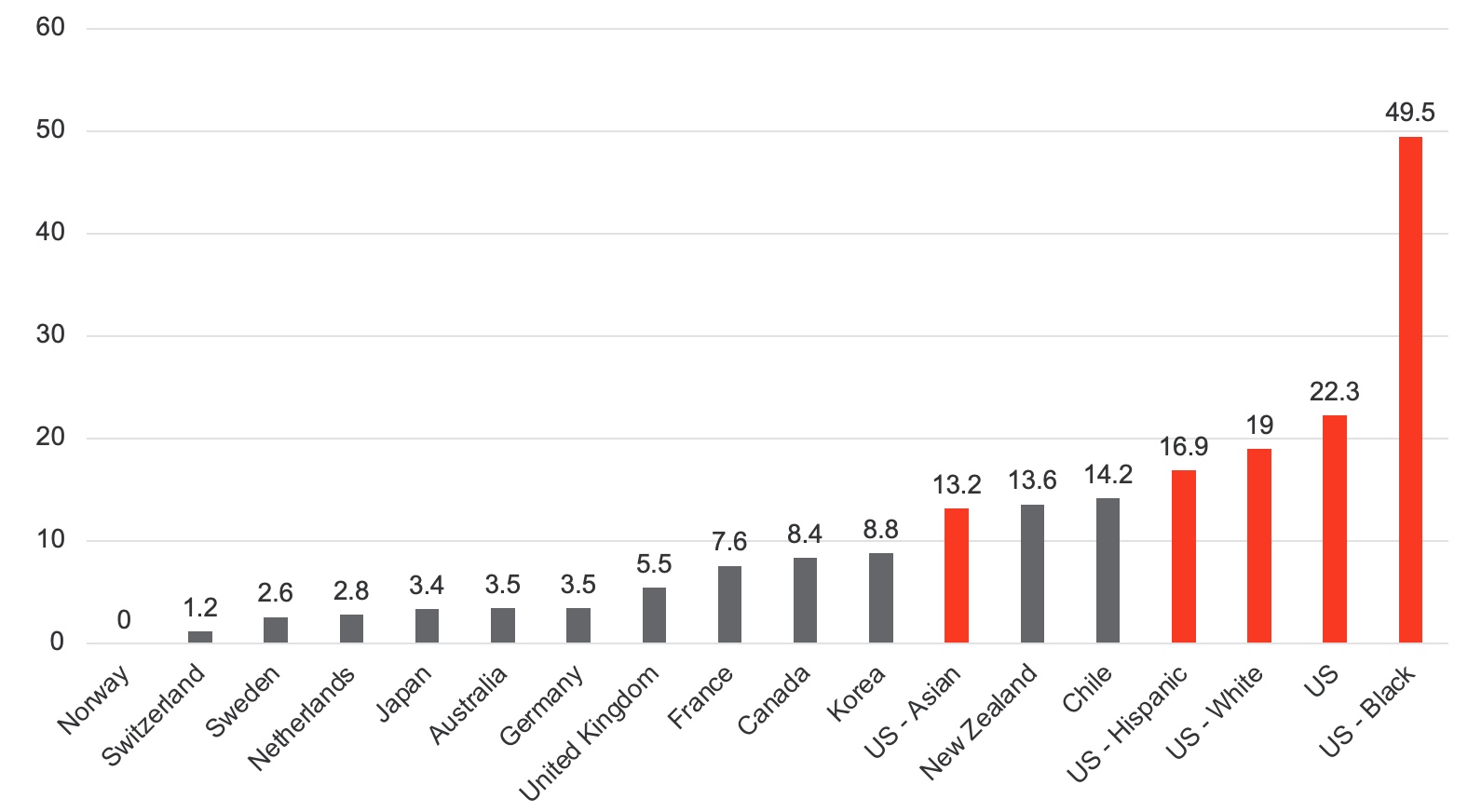
Figure 1. Maternal Mortality Ratio of High-Income Countries per 100,000 Births Deaths During Pregnancy up to 42 days after Pregnancy Termination (Gunja et al., 2024, Commonwealth Fund). (Click here to enlarge the image.)
The data in this graph is collected from high-income countries worldwide, including the United States, highlighted in red. Historically, according to World Health Organization standards, a maternal death rate exceeding 10 deaths per 100,000 live births is considered abnormally high. Unfortunately, the United States has not seen rates below this threshold in years. In comparison, countries like Canada or France maintain significantly lower rates, with European nations showing minimal fluctuation over time. The situation in the United States is particularly troubling as maternal death rates continue to rise, with Black maternal deaths being the most concerning.
I want to reframe and refocus this discussion on what maternal health outcomes mean for care. Consider the hospital environment, where the priority of OB/GYNs and maternity nurses remains early discharge—often one to two days after delivery. Their goal is to mitigate risks, preventing increased maternal deaths and hospital readmissions. As we explore integrating occupational therapy services into maternal care, I urge you to keep these figures and their implications in mind. Reflect on who within the hospital is most at risk for the critical care issues we will examine next.
Critical Maternal Health Concerns: Maternal Health Outcomes: 0-6 Weeks
The three most common causes of maternal deaths in the United States within the first six weeks postpartum are hemorrhage, infection, and cardiovascular conditions.
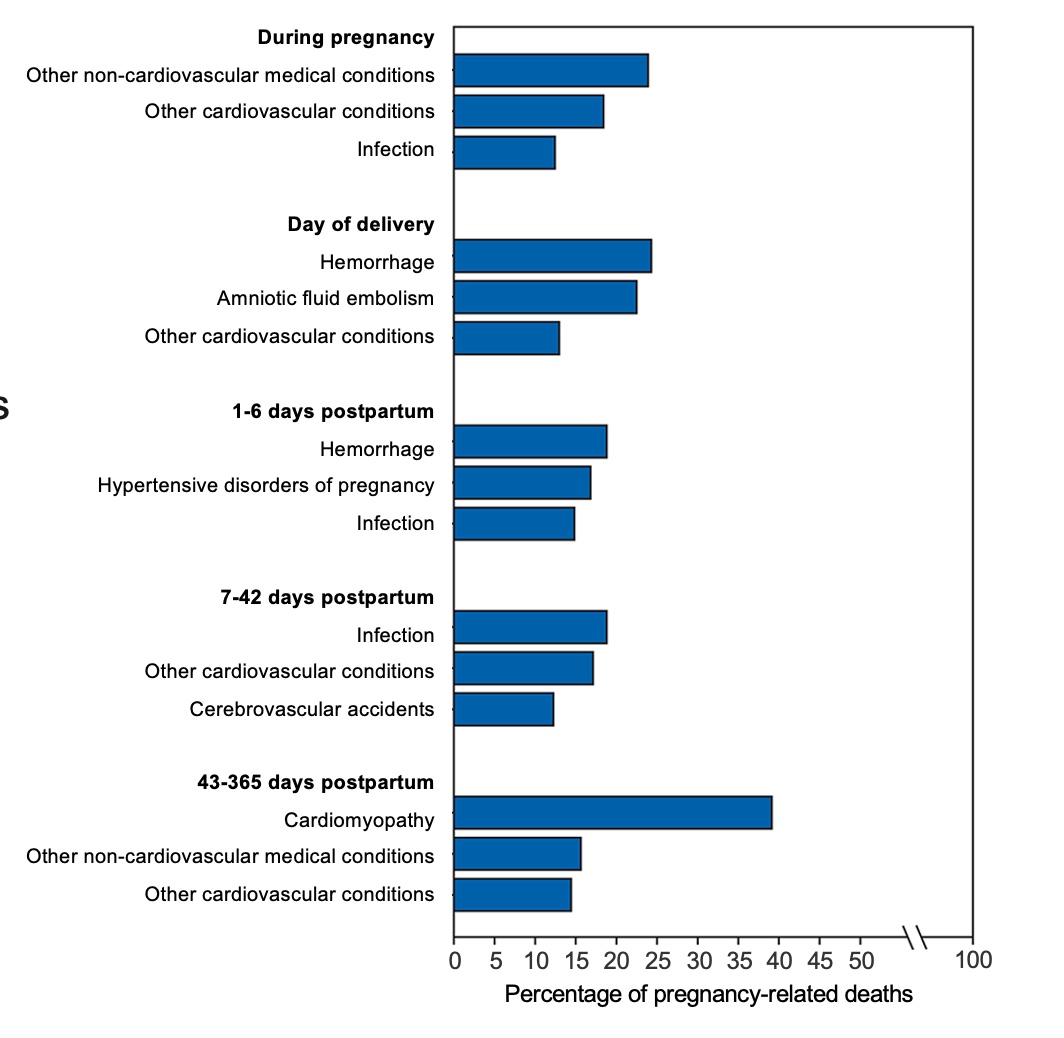
Figure 2. Percentage of pregnancy-related deaths. (Click here to enlarge this image.)
It’s critical to recognize that over 50% of maternal deaths occur within the first six weeks postpartum. For those practicing in outpatient pelvic health, waiting until six weeks to see patients means that many individuals at risk may never make it to your clinic.
Hemorrhage remains the leading cause of maternal mortality during this period, often most severe within the first six days but with the potential to persist for weeks. A significant contributor to hemorrhage is blood transfusion, frequently associated with cesarean sections. Delivery type plays a crucial role, particularly when compounded by factors such as induced labor or uterine atony, where the uterus fails to contract properly and cannot stem the bleeding from blood vessels.
As rehabilitation specialists, especially occupational therapy practitioners (OTPs), our role extends beyond understanding the medical risks. We must address these conditions' profound functional and emotional impacts on the mother. Hemorrhage can severely limit maternal mental health, physical functioning, and the ability to care for a newborn. It is essential to consider how these challenges translate into everyday tasks—getting in and out of bed multiple times a night, performing self-care, managing toileting, and maintaining the stamina required to care for an infant.
In this context, it is crucial to view the individual not just as a patient but as someone deeply embedded in her environment and responsible for others. By understanding these risk factors, we can align our care with the medical team’s objectives—preventing complications and reducing risks—while ensuring that the mother’s recovery supports her ability to thrive in her vital roles.
Critical Maternal Health Concerns: CDC/Severe Maternal Morbidity Indicators
Figure 3 shows the signs and symptoms of severe maternal morbidity indicators.
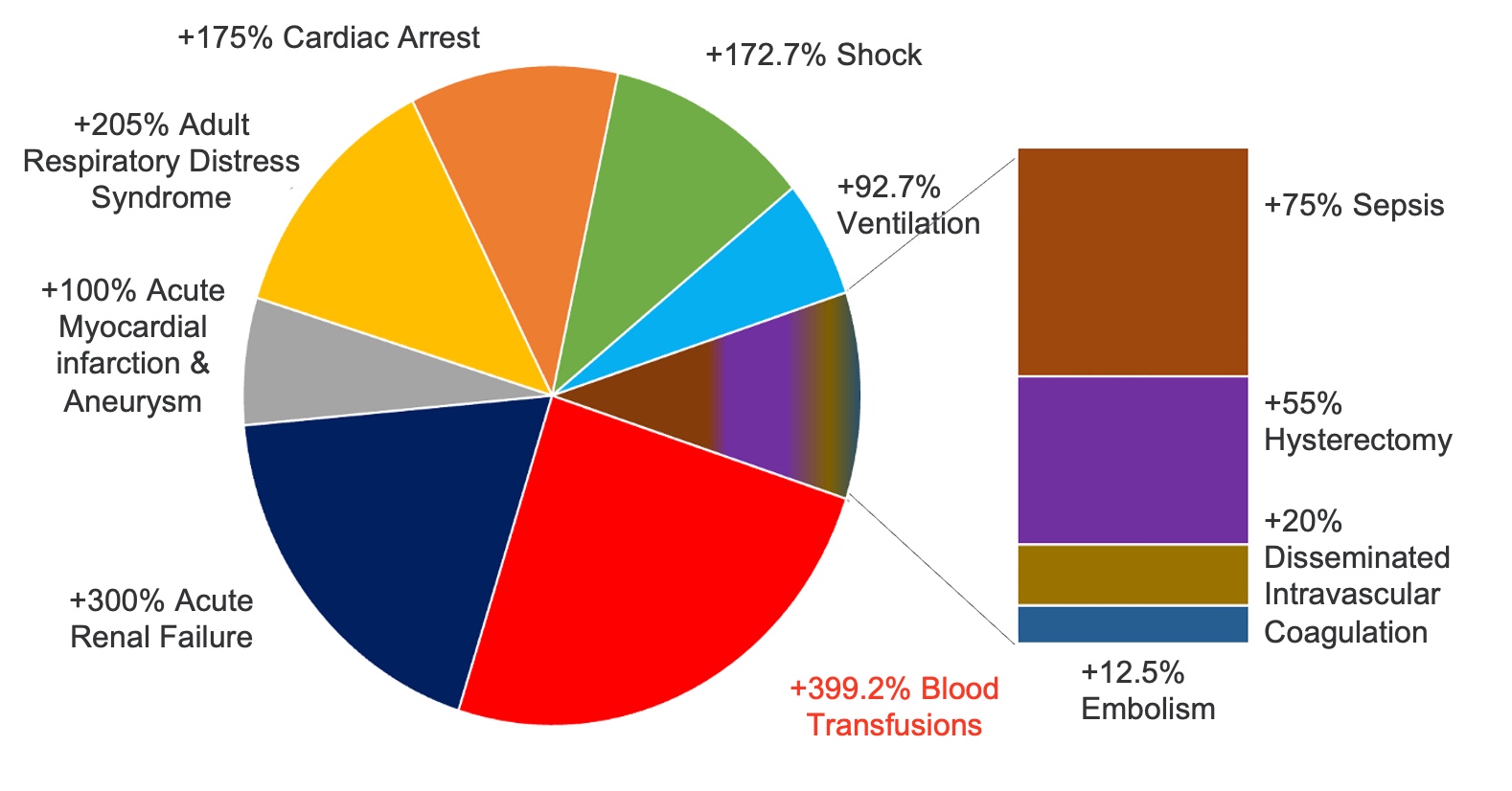
Figure 3. Maternal Morbidity Rate per 10,000 Delivery Hospitalizations Percentage Increase from 1993-2014. (Click here to enlarge the image.)
Hemorrhage
One of the most common complaints related to maternal mortality involves symptoms of hemorrhage, including passing blood clots larger than a quarter, as well as low hemoglobin, low hematocrit, and low platelets. An example that underscores the critical nature of identifying such signs is the tragic death of Olympian Tori Bowie, who was found unresponsive during pregnancy and later confirmed to have suffered from eclampsia and respiratory failure. Her case, along with others in the media, highlights the importance of recognizing symptoms of critical maternal health concerns, particularly during the third trimester and immediate postpartum period.
These stories also remind us of the frequent disconnect between a patient’s concerns and the care team's response. For instance, Serena Williams shared her experiences with warning signs that her medical team initially missed. These examples underline the necessity of a comprehensive, attentive care approach—during pregnancy or postpartum—where every care team member can identify and act on potential symptoms. For occupational therapy practitioners, this means staying vigilant and validating patient-reported symptoms with objective signs when possible. Whether through telehealth, collaboration with the care team, or as an outpatient provider, we are crucial in advocating for lab tests to confirm concerns such as low hemoglobin or platelets.
Infection
Infection, another significant cause of maternal mortality, often arises from cesarean section wounds, perineal lacerations, or retained placenta. While these infections may not present during the initial 24 to 48 hours of hospital care, they can develop later due to complications from delivery. Symptoms such as disproportionate pain, foul odor, purulent drainage, fever, or, in melanated individuals, signs of heat and warmth rather than redness must be carefully assessed. An acute care occupational therapist once helped me realize how simple functional activities, like repetitive movements getting in and out of bed or reaching for a baby, could compromise wound integrity and lead to infection. Beyond teaching proper body mechanics, understanding the patient’s environment and daily demands can prevent such complications.
Hypertensive Disorders: Preeclampsia
Hypertensive disorders, including preeclampsia, require special attention as well. Tori Bowie's story reminds us that baseline metrics are crucial, particularly for athletes. A reading of 140/90 may already indicate a crisis for someone with a naturally lower baseline. As rehabilitation therapists, measuring baseline vitals during pregnancy and monitoring how they change with activity provides vital clues. Disproportionate effort for tasks such as hygiene, self-care, or even putting on socks—particularly for individuals recovering from a cesarean section—could indicate a developing hypertensive emergency. Many patients readmitted within the first three to six days postpartum for preeclampsia lacked adequate social support, further compounding their risk. Evaluating these individuals in the context of their environment is essential.
We must also consider cardiovascular disorders, which receive far less attention than hemorrhage or infection despite being a leading cause of maternal death. While the first six weeks postpartum represent the critical period for hemorrhage and infection, cardiovascular risks persist throughout the first 12 months. By identifying and addressing the functional and systemic challenges these patients face, we can better advocate for their health and recovery.
Suicide and Maternal Mortality
Suicide is the leading cause of death during the perinatal period, which includes pregnancy and up to a year postpartum. This fact highlights the critical need to remain vigilant about the mental health of individuals during this time, particularly when they feel unsupported or unaware of what should be the standard of care.
In many hospital settings, patients recovering from major open abdominal surgeries are routinely provided with rehabilitation services as a standard of care. However, this same level of support is often absent for those recovering from a cesarean section despite it being a similarly invasive procedure. This disparity in care can have a profound and lasting impact on mental health, fostering feelings of neglect and inadequacy. Addressing this gap is essential to improving physical recovery and long-term mental well-being, ensuring that postpartum individuals receive the comprehensive care they need and deserve.
Postpartum Acute Care Occupational and Physical Therapy Algorithm
This algorithm, taken from our 2023 paper, has been enlarged for convenience and is available as a downloadable PDF.
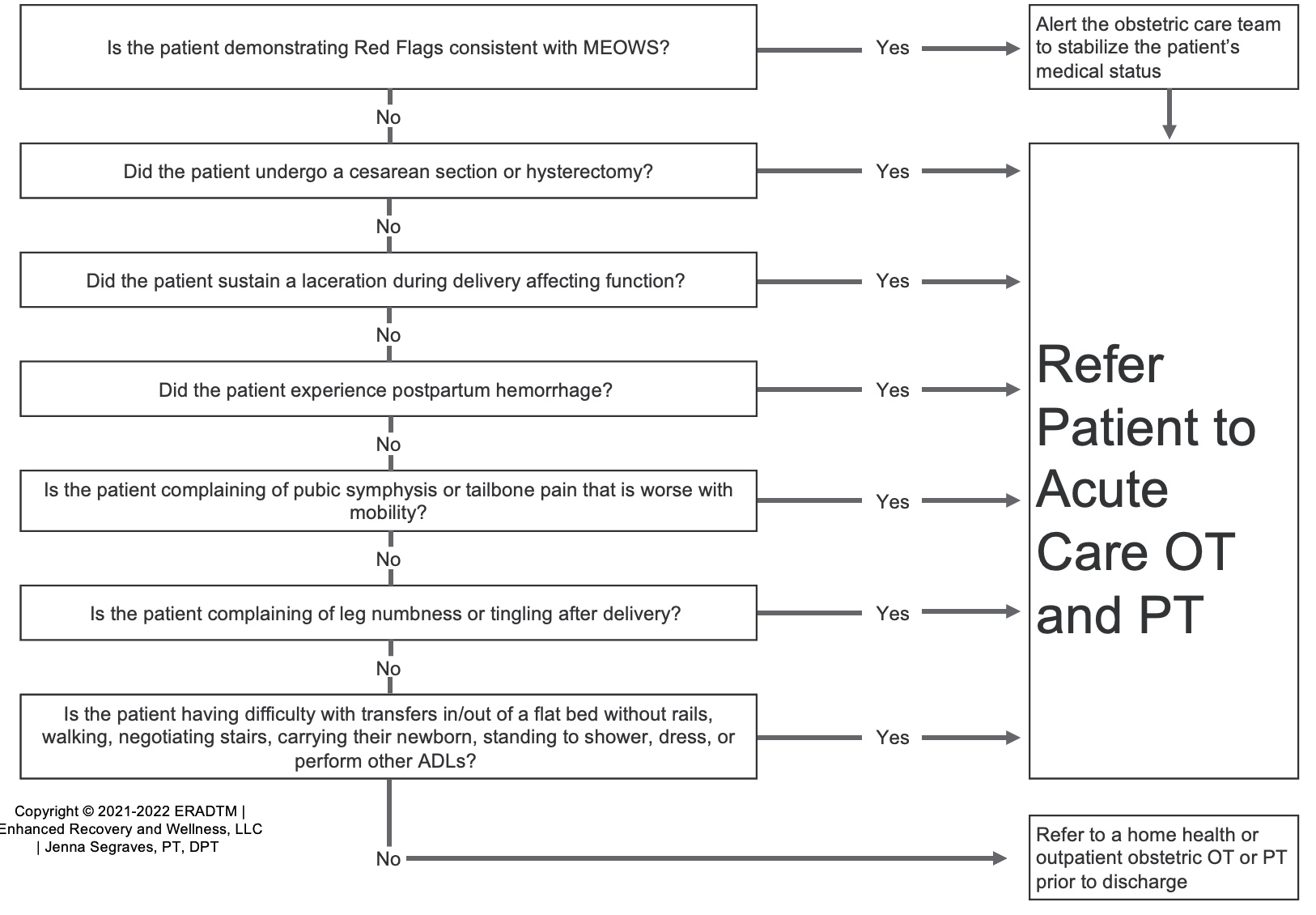
Figure 4. Postpartum Acute Care Occupational and Physical Therapy Algorithm. (Click here to enlarge the image.)
The paper, titled "Initiating Occupational and Physical Therapy in the Hospital After Birth," is open access and can be accessed directly. It outlines guidelines for medical teams and rehabilitation therapists, helping determine the appropriate timing to initiate occupational therapy services during the hospital stay. The goal is to provide these services while the patient is still within the healthcare system, ensuring access to essential resources before transitioning to outpatient care.
Now, I'll hand it over to Jenna.
Cesarean Section: Rehab Evaluation
Jenna: Thank you, Rebeca. As we continue, we will focus on the rehabilitation evaluation for individuals recovering from a cesarean section. As Rebeca highlighted, a cesarean section is a major abdominal surgery, and the involvement of rehabilitation therapists during the first 24 to 48 hours—and especially within the first six weeks postpartum—is essential. This timeframe is crucial for addressing recovery needs and providing comprehensive support to promote optimal outcomes following delivery.
Cesarean Section Complications
Cesarean sections are associated with numerous short- and long-term impairments that significantly impact recovery and overall health. For someone undergoing their first cesarean section, the risk of an unexpected hysterectomy increases by 6 to 14 times. Additionally, there is nearly a fourfold increased risk of developing a pulmonary embolism, a nearly sixfold increased risk of stroke, a fivefold higher rate of postpartum infection, and about 12% of individuals report experiencing chronic pain 10 months after their cesarean delivery.
These statistics highlight the critical need for occupational therapy to be involved in the care of this population. By identifying early signs and symptoms of these complications, OTPs can play a vital role in mitigating risks and, in some cases, preventing these outcomes altogether. This proactive approach can significantly enhance recovery and improve long-term health outcomes for individuals after cesarean delivery.
Unexpected Cesarean Section
When evaluating someone who has undergone an unexpected or expected cesarean section, the evaluation process remains consistent with the principles you would apply to any other condition or individual. Utilizing the International Classification of Functioning, Disability, and Health (ICF) model provides a comprehensive framework for this evaluation.
The ICF model allows us to explore various components that a cesarean section may impact. This includes examining the individual's body functions and structures, identifying activity limitations, and considering participation restrictions. Additionally, it is important to assess environmental and personal factors that may influence their recovery and overall function. This holistic approach ensures that all relevant aspects of the individual's health and circumstances are considered, enabling a tailored and effective intervention plan.
Body Structure and Function. First, we consider body structure and function. For someone recovering from a cesarean section, this involves assessing key physiological and physical components. Examples include evaluating their vital signs to ensure stability, assessing their pain levels and obtaining a rating, and examining bowel and bladder function to determine any difficulties or concerns. Global strength and sensation should also be evaluated to identify deficits or abnormalities. Swelling is another important factor to assess, as it may indicate complications such as infection or poor circulation. These assessments provide a foundational understanding of the individual's physical status and inform the direction of their care plan.
Activity. This includes assessing their mobility, such as their ability to perform transfers and walk safely, as well as evaluating their capacity to carry out activities of daily living (ADLs) like toileting and bathing. Additionally, assessing their ability to lift, carry, and care for their newborn is essential, as these tasks are integral to their role as a parent and critical to their overall recovery and function. These evaluations help identify specific areas where support or interventions may be needed to enhance independence and promote safe, effective participation in daily activities.
Participation. Participation involves evaluating the individual's ability to engage in social and recreational activities and fulfill roles and responsibilities within their daily life. For example, they might express challenges in returning to activities that bring them joy, such as attending church or participating in a weekly dance class. These activities are often key to their emotional well-being and sense of normalcy.
Participation includes home care occupations like cleaning, laundry, and grocery shopping. Additionally, caregiver responsibilities are important, especially if the individual has multiple children. For instance, they may be navigating the demands of caring for three older children and their newborn, which can feel overwhelming during recovery. This might be their first cesarean section, and they may express significant concerns or anxiety about managing this recovery period while balancing these responsibilities. Understanding these challenges allows us to provide tailored support that addresses their specific participation goals and concerns, fostering recovery and confidence in their ability to meet their daily demands.
Environmental Factors. Environmental factors are critical to consider when evaluating someone recovering from a cesarean section. Access to their home is a key area of focus. For instance, do they have stairs they need to navigate, or do they live in a third-floor apartment with no elevator access? The distance from their car to their home entrance is another important consideration, as it could be a significant challenge if they cannot ambulate that far.
Additionally, evaluating the height of their bed is essential, as it impacts their ability to get in and out of bed safely. Assessing whether they have adaptive equipment at home, such as a raised toilet seat or grab bars, and determining whether their insurance will cover any durable medical equipment (DME), recommendations are also important aspects of the evaluation. These external environmental factors can greatly influence their recovery and overall independence, making addressing these considerations in the care plan essential.
Personal Factors. Lastly, we must consider personal factors that uniquely impact the individual’s recovery and overall experience. For example, their maternity leave plays a significant role. Rebeca and I have worked with many patients who reported needing to return to work just two weeks after their cesarean section. Such a limited recovery period significantly alters the approach to education and intervention, emphasizing the need to prepare them for the physical and emotional demands of an early return to work.
Another critical factor is their knowledge of their condition and post-surgical precautions. For instance, many individuals are advised to lift no more than the weight of their baby—approximately 10 pounds or less—after abdominal surgery. Ensuring they understand these restrictions and their importance is essential to minimizing risks. Social support is equally important. Single parents or those without friends or family nearby often face an immense burden, requiring strategies to help them navigate recovery and caregiving responsibilities independently.
Additionally, relevant comorbidities or previous surgeries can influence their recovery. A history of postpartum depression, for instance, may signal the need for more intensive screening and potential referral to a mental health provider. Multiple cesarean sections may necessitate a more thorough assessment of the incision and increased education about wound healing and infection risks due to diminished soft tissue elasticity and strength.
Considering these factors holistically allows us to tailor interventions to the individual's needs, ensuring a comprehensive and supportive approach following a cesarean section during the acute recovery.
Acute Postpartum Rehab Considerations
Body habitus is an important consideration, particularly in relation to wound healing after a cesarean section. For example, a typical low transverse cesarean incision is usually located at or near the hip region. In individuals with an abdominal pannus, this area can become prone to increased moisture accumulation, which may lead to infection. This highlights the need for additional education on strategies to manage this risk, such as teaching techniques to lift the pannus gently to help keep the area clean and dry, reducing the likelihood of moisture buildup and subsequent complications.
Another critical factor is the duration spent in various positions during recovery. Prolonged positioning can impact circulation, pressure distribution, and overall comfort, all of which play a role in healing and function. Figure 5 illustrates a very common position (bed elevated to at least 45 degrees, with her knees bent) I often observe when visiting patients in their rooms, and this posture may provide insights into adjustments or interventions needed to optimize recovery and prevent secondary complications. These considerations further emphasize the importance of tailoring education and care plans to meet each individual's unique needs and circumstances.

Figure 5. A common image seen in acute postpartum.
This position places direct pressure near the incision site, typically in the lower abdominal region. Prolonged time spent in this position can contribute to increased edema in the area that needs optimal healing. Educating patients about position changes is critical. Incorporating periods of lying fully supine can help promote better lymphatic drainage and circulatory flow, which is essential for reducing edema and supporting recovery. While it is perfectly fine for patients to use this semi-reclined position, the emphasis should be on frequent positional changes to avoid complications from prolonged pressure or swelling.
Another important consideration is how transfers affect wound healing. It’s all too common to see postpartum individuals being pulled up by their arms to get out of bed. This pulling motion engages the abdominal muscles and strains the incision site, which should be avoided during the early recovery. To illustrate this, imagine pulling on an imaginary rope before you—most will feel their abdominal muscles engage automatically. This activation is precisely what we aim to prevent in the initial stages of healing following abdominal surgery.
Repetitive infant lifting is another task that poses risks to the healing incision. New mothers must lift their newborns frequently throughout the day and night, and observing how they perform this task is crucial. Providing education on safer, more ergonomic lifting methods can help reduce strain on the incision and prevent wound reopening.
Compression therapy is another valuable tool for this population. Compression aids lymphatic circulation and venous return, which support wound healing and reduce the risk of infection. It also helps minimize the likelihood of edema recurrence. Implementing compression solutions, such as abdominal binders, can be a practical and effective strategy for supporting recovery in postpartum individuals as long as they are applied and used correctly. Tailoring these interventions to each patient’s needs ensures a safer and more efficient recovery process.
Figure 6 shows how using an abdominal binder can provide support during movement.

Figure 6. Example of using an abdominal binder.
Multiple studies have demonstrated that using an abdominal binder after surgery offers numerous benefits. These include reducing postoperative pain and psychological stress, improving mobility, and preventing abdominal wound dehiscence. These findings are consistent across obstetric and general abdominal surgery patients, including post-cesarean individuals.
Additional rehabilitation considerations extend to pulmonary and gastrointestinal (GI) function, often compromised following abdominal surgery. Patients face an increased risk for complications such as pneumonia, atelectasis, constipation, or even postoperative ileus. Positioning is critical to address these risks, emphasizing the importance of frequent position changes to promote circulation, reduce edema, and prevent respiratory and GI complications. As discussed, staying in a semi-reclined position with knees bent for prolonged periods can contribute to fluid accumulation around the incision, hampering healing.
Transfers are another essential focus area, particularly getting in and out of bed or the car, which tend to provoke significant pain in the cesarean population. Educating patients on techniques to perform these transfers safely and independently without straining the incision is crucial for their recovery.
Newborn care has now become an integral activity of daily living (ADL) for these patients, alongside caring for themselves. It is essential to ask about their concerns regarding managing newborn care while recovering from major abdominal surgery. This includes teaching proper lifting mechanics to minimize strain on the incision. For instance, ensuring the baby is held close to the body while lifting or placing the baby in a bassinet can reduce stress on the abdominal muscles and promote safer movement.
In addition to newborn care, patients must manage other ADLs and instrumental activities of daily living (IADLs) upon returning home. These may include showering, cooking, cleaning, laundry, or caring for other children. Helping patients plan and adapt these tasks to accommodate their recovery is a key role for OTPs.
Scar massage is another important consideration, though it is not typically initiated during the immediate postpartum phase. Patients should be educated about the importance of scar massage once the incision has healed, as this can help improve mobility and reduce discomfort in the long term.
Postpartum mental health is a critical area of focus. Patients may show signs of depression or anxiety, particularly if they had a traumatic birth experience. For many, cesarean sections are unplanned, resulting in emotional challenges as they adjust to a delivery outcome they may not have anticipated. Additionally, some individuals may experience perinatal loss, navigating the physical recovery of a cesarean delivery without the joy of bringing a newborn home. These emotional challenges underscore the importance of mental health screening and referral when needed.
Rehabilitation therapists are uniquely equipped to identify these additional needs, provide targeted interventions, and make appropriate referrals. Occupational therapy practitioners, in particular, play a vital role in addressing mental health concerns and supporting patients as they navigate the physical and emotional complexities of their recovery journey.
Acute Postpartum Evaluation
The acute postpartum evaluation for someone recovering from a cesarean section incorporates a blend of assessments and early interventions, as these are often interconnected in practice. Bed mobility is a critical component, with the log roll technique being particularly important. This method minimizes strain on the incision by having the patient roll to their side and then sit up. Simulating their home environment during practice is essential since most patients return to flatbeds without side rails. Hospital beds, with elevated headrests and rails, often make it easier for patients to get out of bed, so asking about their home setup and practicing accordingly ensures they are prepared for their environment.
Lifting precautions are another important topic, as patients are generally advised not to lift more than 10 pounds, the approximate weight of their baby. While lifting their infant is acceptable, carrying them in a car seat or similar carrier often exceeds this restriction. Discussing support systems is vital, especially to ensure they have help with tasks like attending pediatrician appointments early in the postpartum period. Additionally, avoiding the Valsalva maneuver during transitions or bowel movements is crucial, as it increases intra-abdominal pressure, which can strain the incision. Teaching techniques like exhaling on exertion can help patients perform these tasks safely.
Breathing and splinting techniques are particularly empowering for patients. Encouraging movement with their breath not only alleviates pain but also enhances functionality. For splinting, using a firm blanket wrapped in a pillowcase rather than a softer pillow provides better support to the incision during coughing, sneezing, or laughing. This reduces pain and protects the healing site.
Edema management is a key consideration for both abdominal and lower extremity edema. Abdominal binders, commonly available in hospitals, can help reduce swelling and promote venous return. For outpatients, it’s important to ask if they were sent home with a binder and to provide guidance on its proper use during follow-up sessions.
Positioning and posture for feeding are also essential aspects of the evaluation. Whether the patient plans to breastfeed or bottle-feed, simulating their home setup (rocking chair, couch, or bed) allows for identifying supportive measures to prevent musculoskeletal strain, such as neck or back pain. Proper positioning with adequate pillow support can reduce forward-leaning and awkward head positioning during feeding.
A comprehensive transfer and gait assessment is crucial, including their ability to get on and off the toilet, navigate stairs, and walk while carrying objects, particularly their infant. For patients with stairs at home, assessing their ability to navigate them safely multiple times a day is essential, especially if their bedroom is on an upper floor. Assessing endurance through functional tasks while monitoring vital signs and perceived exertion provides insight into how the body responds to necessary activities, helping identify early warning signs of complications.
Pre- and post-activity vital signs are perhaps the most critical part of the early postpartum evaluation. While nursing staff often assess vitals at rest, it is essential for rehabilitation therapists to observe how the patient’s body responds physiologically to basic mobility tasks. These measurements can reveal early red flags that might go unnoticed, allowing the medical team to intervene before the patient is discharged.
As Rebeca mentioned, these evaluations often blend seamlessly into interventions. For example, teaching abdominal splinting techniques or guiding a patient through incentive spirometer use can alleviate pain and improve respiratory function. These techniques were introduced to many of us by acute care occupational therapy practitioners, whose insights have expanded the traditional biomechanical perspective, emphasizing the real-world activities and challenges that postpartum individuals face.
Our patient population is incredibly diverse, ranging from young individuals as young as 13 years old to those in their 50s. Their circumstances vary widely, from new mothers navigating care for their newborns to those experiencing perinatal loss, managing NICU challenges, or recovering from additional procedures like cesarean hysterectomies.
Cesarean Section: Rehab Interventions
Rebeca: As Jenna noted, this list of considerations is not exhaustive, but it highlights the broad scope of care and sensitivity required to support these individuals effectively.
Acute Postpartum Interventions
Let me share a few examples to give you a clearer picture of the critical care needs of the maternal health population, particularly when it comes to practical solutions for challenges like infant lifting. Many of these strategies were introduced to me by OTPs, who opened my eyes to the variety of tools and resources available to support these patients.
One common scenario involves exploring infant lifting alternatives. For instance, during an evaluation or treatment session, we might sit with the patient and browse options online—sometimes even on platforms like Amazon—to find items that can make their daily tasks more manageable. These solutions often ensure that they have tools to support their recovery by the time they get home.
Consider a mom, like the ones Jenna described, who is experiencing severe fatigue, significant blood loss, or complications from hemorrhage. This individual might be unsteady on her feet and unable to sustain standing long enough to take a shower or care for her baby effectively. Identifying adaptive equipment, such as a lightweight infant carrier, a bassinet that adjusts to bed height, or even a shower chair, can make a huge difference. These practical interventions address immediate safety concerns while promoting independence and reducing strain on the body during recovery.
These examples highlight the importance of being resourceful and proactive in identifying tools and techniques that align with the patient’s unique needs and environment. This collaborative and creative approach allows us to address the critical care needs of postpartum individuals effectively.
Infant Lifting Alternatives
Infant lifting alternatives, like a three-in-one baby bassinet that can be placed right by the bed, are incredibly helpful in reducing the physical stress on someone recovering from a cesarean section. These bassinets allow the baby to be brought closer to the parent, minimizing the need for excessive reaching or bending—movements that can strain the incision site and cause discomfort. For someone without a caregiver or support person to assist with lifting and transferring the baby, this can be a game-changer.
It’s important to acknowledge that while these solutions may not address every challenge a new parent faces, they offer practical alternatives that significantly ease some of the physical demands postpartum individuals encounter. In many cases, patients are discharged with little to no equipment or guidance, leaving them to manage recovery and infant care with minimal resources. These tools are not a complete solution, but they represent thoughtful and impactful ways to bridge that gap, making a challenging transition a bit easier.
Infant Carrying Alternatives
Regarding infant carrying alternatives, the insights and creativity of occupational therapy practitioners—and even the lived experiences of moms themselves—are invaluable. Many of these tools and strategies are already familiar to experienced parents, but in the context of someone with limited support, unexpected circumstances, or financial constraints, the need for accessible, practical solutions becomes even more urgent.
Consider the individuals who might not have had a baby shower to receive essential items, or those who faced an unexpected delivery, such as the 13-year-old patient I treated, or someone navigating recovery with no knowledge of or access to the wide range of baby products available. These cases highlight the diversity of needs and the importance of tailoring solutions to meet the realities of each parent’s situation.
I recall many mothers in acute care who were single parents heading home to second—or third-story apartments. Some planned to carry their baby upstairs and return for the carrier, or vice versa. These scenarios, while creative, often reveal the logistical and physical challenges parents face. During a subjective exam, I frequently hear patients grappling with "the next steps," trying to devise a plan without the resources or support that might otherwise ease their burden.
Infant carrying alternatives can be a lifeline in these situations. Occupational therapy practitioners are uniquely positioned to offer practical suggestions and guidance. Whether introducing a lightweight carrier, recommending wearable slings for safer mobility, or brainstorming ways to simplify home logistics, these tools can make a tremendous difference for someone who may feel like they’re figuring everything out independently. The goal is to give these parents a sense of empowerment and relief during an overwhelming time.
Edema Management
Edema management is critical in postpartum recovery, particularly for individuals recovering from a cesarean section. This is especially relevant given the heightened risk of cardiovascular complications like pulmonary embolism (PE) and deep vein thrombosis (DVT). Serena Williams' widely shared experience underscores how easily these conditions can develop, often exacerbated by lapses in medication management. For example, patients who were on blood thinners before delivery may have been taken off them for childbirth and not adequately guided on when or how to restart their regimen.
As rehab professionals, we may be the first to assess these patients post-delivery, providing a unique opportunity to identify early signs of complications. Thorough evaluation involves visually inspecting and palpating the legs for swelling, warmth, or tenderness and educating patients on the importance of movement. Prolonged reclined positions, particularly after a cesarean section, can contribute to the pooling of fluid around the pelvis, increasing the risk of DVT and other complications. Encouraging appropriate mobility, regular positional changes, and gentle exercises can significantly improve venous return and reduce these risks.
This role is crucial to the rehabilitation and recovery process as we bridge the gap between acute care and patient education. By taking this responsibility seriously and working collaboratively with the medical team, we can help prevent serious complications and support optimal outcomes for postpartum individuals.
Energy Conservation
Occupational therapy practitioners have truly opened my eyes to the range of assistive devices that can benefit the maternal population, many of which are not traditionally considered by insurance providers for this group. Navigating insurance hurdles is challenging in any acute care setting, but it is particularly acute for postpartum individuals, as coverage often doesn’t account for durable medical equipment (DME) or assistive devices tailored to their needs. This is where advocacy plays a crucial role, and trusting that if we equip patients with the right information, many will rally their communities to help secure these resources.
One great example is the use of a laundry basket on wheels. I hadn’t considered this until an occupational therapist suggested it as a practical tool for postpartum patients who might otherwise carry heavy loads during their recovery. For a patient recovering from a cesarean section, lifting and carrying items like laundry can quickly deplete their energy and strain their healing incision. A wheeled basket allows them to complete these tasks safely and with less effort.
Breaking larger daily tasks into smaller, manageable increments is another invaluable strategy to conserve energy and prevent overexertion. These environmental and practical adaptations can significantly impact a patient’s ability to meet the demands of early postpartum recovery while protecting their physical and mental well-being.
It’s also worth noting the disparity in support compared to other patient populations. For instance, those recovering from knee or hip replacements often have more structured assistance and resources upon discharge. In contrast, postpartum individuals, despite undergoing major abdominal surgery, are frequently sent home with fewer supports in place. Addressing these gaps with creative solutions and patient-centered planning is critical to ensuring their safety and success in recovery.
Bowel Function
Bowel function is a critical aspect of postpartum recovery, but it can be a sensitive topic, especially when discussing tools like a squatty potty, which may not be suitable for all patients. For the two-thirds of mothers who deliver vaginally, there is a concern about the pelvic floor being overextended, so any intervention must be carefully tailored to their specific recovery needs. However, for some of the postpartum period, we must address strategies that improve bowel function safely and effectively.
Hydration is a key component, particularly for breastfeeding or pumping individuals, as these activities increase fluid needs. Encouraging a diet higher in fiber can also be helpful, though care must be taken to avoid foods that might cause excessive bloating, gas, or discomfort. This balance is best achieved with guidance from a registered dietitian, ensuring that dietary changes are supportive without inadvertently causing other complications. Stool softeners are often prescribed, and patients may need encouragement to use them consistently to maintain soft stool and reduce straining.
Practical techniques, such as "blow as you go," can significantly ease discomfort during bowel movements. In some cases, I’ve assisted patients by helping them elevate their feet slightly—using a garbage can or similar object rather than something as high as a squatty potty—to provide just enough pelvic floor relief without overextending the area. These small adjustments can empower patients, helping them build confidence and ease their discomfort during those challenging first days after birth. This hands-on support can profoundly impact, providing comfort and reassurance during a particularly vulnerable time.
Breastfeeding Positions
Figure 7 shows many options regarding breastfeeding or chestfeeding positions that can be adapted to the postpartum individual's specific needs and physical conditions.
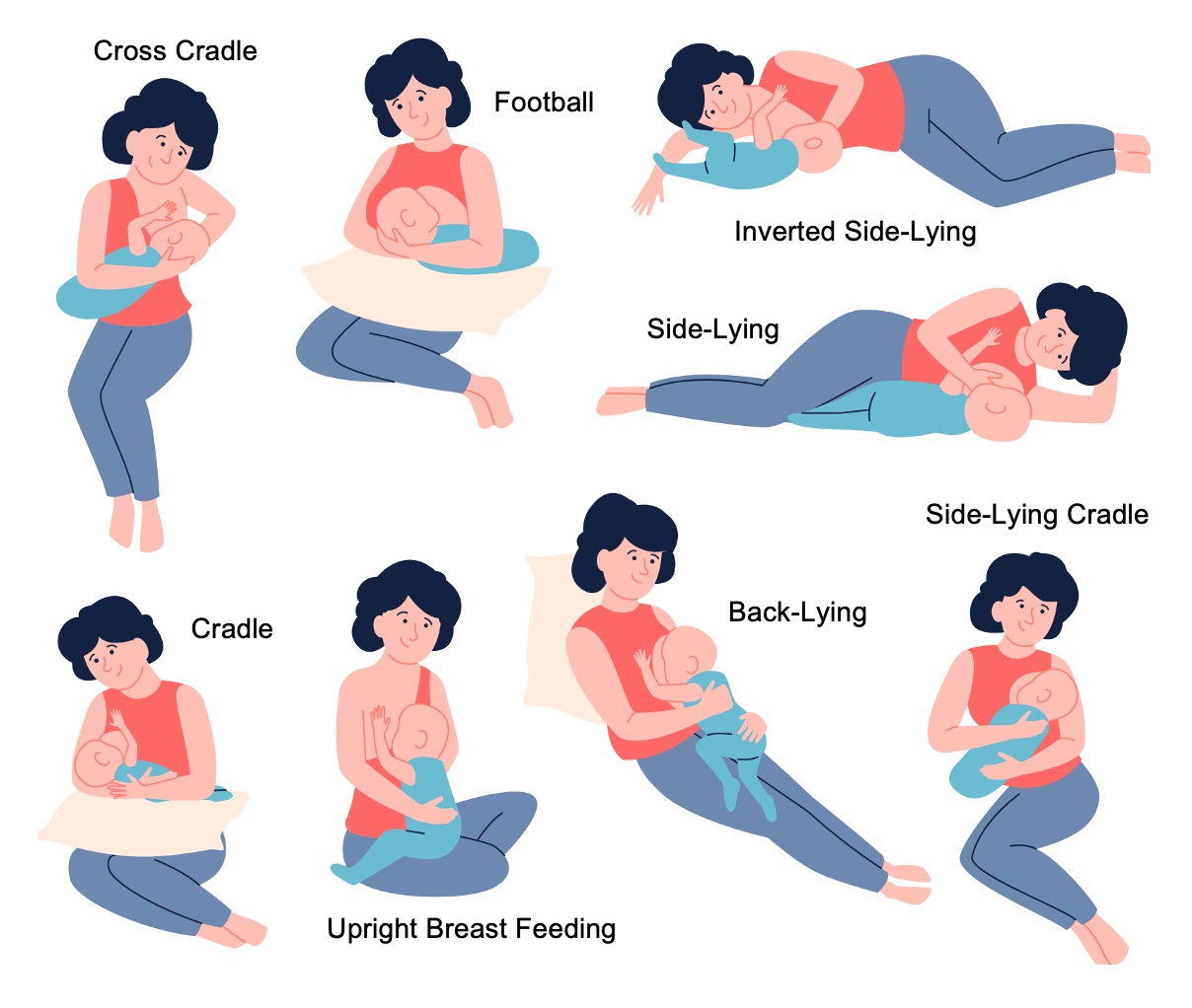
Figure 7. Breastfeeding positions.
In the acute care setting, we often use multiple pillows to support the patient, helping them avoid excessive neck and wrist flexion from looking down at their baby or hunching their shoulders forward. Maintaining a neutral spinal alignment is key, particularly for those recovering from a cesarean section, as prolonged upright flexed positions can strain the incision site and hinder healing.
The choice of feeding position can vary based on the type of birth or delivery and any resulting injuries. For instance, a patient with a tailbone injury may benefit from side-lying or inverted side-lying positions, which reduce pressure on the sacral area while allowing for effective feeding. Exploring different options and being willing to try various setups is essential, even if working with this population is new to you. Understanding common postpartum conditions and applying your knowledge creatively are critical first steps in addressing postpartum individuals' physical and mental health needs.
It’s important to emphasize that the role of a rehabilitation therapist is not to replace or act as a lactation consultant. Instead, the focus is on preventing impairments associated with the activity setup for feeding. This includes avoiding excessive or prolonged flexed positions, teaching extension stretches or post-feeding activities to restore alignment, and reducing strain by adjusting the feeding mechanics. For example, rather than the patient bringing their body down to meet the baby, teaching strategies to bring the baby up to meet their chest or breasts can make a significant difference in reducing pain and promoting recovery.
The goal is to support the patient’s functional independence and comfort, ensuring they can meet their responsibilities and desires in caring for their baby while protecting their physical health and well-being.
Outcome Measures for the Acute Postpartum Patient
Jenna: Thank you, Rebeca. Let’s discuss some outcome measures for the acute postpartum patient population.
There are several effective outcome measures for this group, with one of the most essential being something we’ve already highlighted: taking vital signs. Assessing vitals during functional activities provides immediate, actionable data on how the patient’s body responds to tasks they must perform at home. This process helps evaluate whether their physiological response is within an expected range or if there are concerning signs that need further attention. Simulating daily activities and occupations that are part of their home routine ensures patients are well-prepared, and it identifies potential barriers to a safe and successful transition from hospital to home.
In addition, two other key outcome measures are the Boston University Activity Measure for Post-Acute Care (AM-PAC) and the Readiness for Hospital Discharge Scale Postpartum Form. These measures are instrumental in assessing a patient’s functional capabilities and preparedness for discharge. Next, we’ll examine how these tools can be applied effectively to support the postpartum population.
AM-PAC
The AM-PAC Basic Mobility "6-Clicks" is a quick and efficient tool that evaluates a patient's functional mobility through six straightforward questions. The first three questions assess the patient's current difficulty with turning over in bed, sitting down on and standing up from a chair with arms, and moving from a supine position to sitting on the side of the bed. The last three questions focus on the patient's level of assistance in moving between a bed and a chair, walking within their room, and climbing three to five steps with a railing.
Similarly, the AM-PAC Daily Activity "6-Clicks" evaluates a patient's need for help with six daily activities. These include putting on and taking off lower body clothing such as socks, shoes, pants, and underwear; bathing; toileting; putting on and taking off upper body clothing; performing personal grooming tasks like brushing teeth; and eating meals.
Scores for both assessments range from Unable (1, the lowest score) to None (4, indicating full independence), with total scores ranging between 6 and 24. A score below 20 may suggest a higher likelihood of hospital readmission. This makes these tools particularly valuable from an occupational therapy perspective, as they help identify patients who could benefit significantly from rehab services. By addressing these needs early, therapists can reduce readmission risks and promote a safer discharge.
Readiness for Hospital Discharge Scale – Postpartum Form
The Readiness for Hospital Discharge Scale Postpartum Form is a subjective questionnaire designed to assess how prepared a patient feels to manage their care after leaving the hospital. It includes 22 questions, where the patient selects a number between 0 and 10 to describe how they feel about specific aspects of their readiness. For situations where the full form might be overwhelming, there is also an eight-question short form that can be more manageable for patients who may not tolerate the longer version.
Some examples of questions provide a sense of the tool's focus. For instance, patients are asked, "How would you describe your physical ability to care for yourself in the first few days after you go home?" and "How would you describe your physical ability to care for your baby in the first few days after you go home?" One of the strengths of this outcome measure is how it separates individual care tasks from baby care tasks, reflecting the dual demands that postpartum patients face.
Other questions delve deeper, asking, "How well will you be able to perform your personal care?" followed by, "How well will you be able to perform baby care?" This distinction is particularly useful because readiness encompasses physical ability and other factors, such as emotional or cognitive readiness, that influence a patient’s capacity to perform these tasks.
The scoring ranges from Not at All (0, the lowest score) to Extremely Well (10, the highest score), allowing patients to place themselves along a continuum. This scale provides valuable insight into their perceived readiness and helps identify areas where additional support or intervention may be needed. The care team can proactively help patients feel more confident and prepared for discharge by addressing these concerns.
Higher Hospital Spending on Occupational Therapy is Associated with Lower Readmission Rates
In the insightful article by Rogers and colleagues (2017), "Higher Hospital Spending on Occupational Therapy is Associated with Lower Readmission Rates," a key takeaway is occupational therapy's crucial role in reducing hospital readmissions. The article emphasizes how occupational therapy addresses essential self-care and functional needs, including meal preparation, medication management, bathroom access, and family or nursing support. These interventions can prevent complications and challenges that might otherwise lead to readmission.
This article beautifully underscores the significant impact of occupational therapy across all patient diagnoses and conditions. By focusing on practical and individualized care, occupational therapy supports patient independence, improves health outcomes, and reduces healthcare costs. It’s a powerful reminder of the indispensable value of occupational therapy in acute care and beyond.
Understanding the Meaning of Recovery to Patients Undergoing Abdominal Surgery
Lastly, we’d like to close with an inspiring study by Rajabi Yazdi and colleagues, "Understanding the Meaning of Recovery to Patients Undergoing Abdominal Surgery." In this study, participants were asked to define recovery in their own terms rather than relying on the traditional physician-centered perspective of recovery as merely tissue healing. The findings revealed five major themes that patients associated with their recovery:
- Returning to their habits and routines.
- Resolution of their unique symptoms, such as pain or discomfort.
- Overcoming their mental strains.
- Regaining their independence.
- Enjoying life.
These themes reflect a deeply personal and holistic view of recovery. Isn’t this precisely what occupational therapy practitioners help their patients achieve daily? Supporting patients in returning to meaningful activities, addressing both physical and emotional challenges, and empowering them to reclaim their independence and joy in life are at the heart of occupational therapy.
You are integral to the recovery process. You belong in this space, working with the immediate postpartum population. They need you, and the impact you make is profound. Thank you.
Summary
Hopefully, you now feel more confident in this area of practice. We'd like to open up the exam poll now.
Exam Poll
1)What is a common cause of US maternal death in the first six weeks postpartum?
The answer is D, which is all of the above. Each of these are the top three contributors to maternal death in the first six weeks postpartum.
2)What is one benefit of using an abdominal binder after a cesarean section?
The answer is C, prevention of abdominal wound dehiscence. So an abdominal binder plays a large role not only at reducing swelling, but it also helps approximate that tissue from that incision site to help with the healing process and prevent it from reopening.
3)Which environmental intervention supports perineal or abdominal wound healing in postpartum patients?
The answer is B, which divides daily tasks into smaller increments or energy conservation techniques. I did want to just clarify in A where it says to use high-pressure compression garments, and that was something that we did not specify. So high pressure, we wouldn't want to have too much because we could also cut off circulation. So that's why A is not correct here. Then, abdominal strengthening exercises will be performed in the early postpartum phase. That's something we want to avoid. It utilizes those core and abdominal muscles because it strains the incision. So, B dividing daily tasks into smaller increments is correct.
4)The "AM-PAC Basic Mobility ‘6-Clicks’" assessment includes an evaluation of which functional activity?
The answer is C, moving from lying to sitting on the side of the bed. So. So that is one of the six clicks that you would answer. Some chose to carry items up and down stairs. And I just want to clarify that the measure of that particular outcome measure is just negotiating stairs. It does not include carrying an object.
5)Which of the following is a primary role of occupational therapy in reducing hospital readmission rates?
The answer is identifying deficits in self-care and function that could lead to readmission.
References
Please refer to the separate handout.
Citation
Segraves, J., & Segraves, R. (2024). Critical rehab needs for acute postpartum patients: Postnatal pelvic health virtual conference. OccupationalTherapy.com, Article 5760. Available at www.occupationaltherapy.com

