Introduction
Today, we are going to be looking at dementia symptoms that affect a population that we are dedicated to serving. I hope this course helps you as a practitioner to identify dementia symptoms as well as risk factors. I do not claim to know everything, nor do I believe any of us ever will. However, we all should be lifelong learners.
The Aging Population
- The US Administration on Aging reports that:
- There are over 51 million people over age 65 living in the United States
- In the past decade, the population over age 65 has increased by 34%
- Elders (ages 65+) represented 1 in every 7 Americans
- Older adults report having increased chronic health conditions (almost 100% report at least 1 chronic condition)
(2018 Profile of Older Americans. Retrieved from www.aca.gov)
This matters because the population is aging. According to data from 2018, there are over 51 million people at social security age or older living in this country. This population is a third bigger than it was a decade ago. In this country, approximately one in every seven people are considered elders. However, with that increase in age also comes an increase in the potential for chronic health conditions. Medical science is helping us live longer, and as we live and age, we may have some type of chronic health condition.
Aging and Dementia
- The Alzheimer’s Association’s 2019 report states that in the United States:
- 5.8 million people are currently living with Alzheimer’s Dementia (AD)
- One in ten people over age 65 has Alzheimer’s
- This number increases to one in three over the age of 85
- Almost 2/3 of those with AD are women
- The lifetime risk of a person for developing AD by age 65 is as high as 12% of men, but 21% of women!
(2019 Alzheimer’s Disease Facts and Figures. Retrieved from www.alz.org)
The Alzheimer's Association published information in 2019 specifically on Alzheimer's disease. There are approximately six million people currently living in the United States with Alzheimer's disease and dementia. This means that one in 10 people fall in that elderly population. As we grow older than 85, that increases to about one in three people. My mom will turn 65 this year and my grandmother is in the 85 and older category. Many of you most likely have friends and family members who fall into this category as well.
If you are like me, you are constantly looking for signs and symptoms. We know that there is a decent risk of a person developing Alzheimer's dementia, especially as a woman. There appears to be some hereditary link as well. In my family, almost all of my grandparents and great-grandparents had Alzheimer's disease at some point in their life.
Aging and Dementia - Demographics
- Disparities among minority groups
- African American elders are twice as likely to have AD than non-Hispanic whites
- Hispanic ethnic groups are 1.25-1.5 times more likely to have AD than older whites
- Projections for 2025 indicate the highest percentage increases in these states:
- Arizona: 43%
- Nevada: 36%
- South Carolina: 30%
- Vermont: 31%
- Wyoming: 30%
(2019 Alzheimer’s Disease Facts and Figures. Retrieved from www.alz.org)
When we look at the demographics of dementia, there is a major disparity. When we look at minority groups, African Americans and Hispanic Americans, we find that minority groups are much more likely to have Alzheimer's dementia than your typical European American groups. If you are African American, your risk is twice as high. If you are Latino or Hispanic, your risk is anywhere from about 1.25 to 1.5 more times likely.
The highest percentage of increases in dementia are projected to occur over the next five years in 5 states (as listed above). Arizona is projected to have a 43% increase. I live in South Carolina so a 30% increase is rather alarming to me. We have this large number now but it is going to be even higher in the next five years. I truly believe this is where we are going to be essential as health care providers. We are going to be fighting the characteristics and the symptoms that are coming along with some of these increased diagnoses of dementia.
Dementia - “The Ticking Time Bomb”
- The World Health Organization reports that every 4 seconds a new case of dementia occurs
- Dementia is the #1 cause of disability and dependency among older adults
- Around 95% of the general public believes that they could develop dementia in their lives
- But 35% of carers have reported concealing their loved one’s diagnosis of dementia
- The total estimated annual cost of dementia worldwide is $1 trillion
- 62% of healthcare practitioners believe that dementia is “normal aging”
World Alzheimer Report 2019, World Health Organization (WHO)
If you have ever read anything by Dr. Peter Piot, he calls dementia the "ticking time bomb." I know right now with what is going on in this country, it already feels like a ticking time bomb. However, when we look at dementia, the World Health Organization reports that every four seconds a new case of dementia occurs. I have been talking for almost eight minutes already. Think about how many new cases of dementia have occurred during those eight minutes. It is the number one cause of disability requiring long-term care due to the dependency among older adults. And because we have had an increase in our knowledge of dementia, about 95% of the general public believes that dementia could affect them at some point in their life. Another alarming statistic is that 35% of caregivers have concealed their loved ones' diagnosis. Now whether that is because they are in denial themselves or whether that is because they are trying to protect their loved one, this could be up for interpretation. The annual cost worldwide is about one trillion dollars, and it is not a part of normal aging despite what the majority of healthcare practitioners may believe.
Major Neurocognitive Disorder
- Not a specific disease (though sometimes caused by one)
- Memory is typically considered the primary loss of function
- A disorder/group of symptoms characterized by a loss of function:
- Complex attention
- Executive function
- Learning and memory
- Language
- Perceptual-motor function
- Social cognition
(DSM-5 Criteria)
The Diagnostic and Statistical Manual of Mental Disorders, DSM-5, is now in its fifth edition. It now calls dementia a major neurocognitive disorder. They use that terminology, but the word dementia continues to be an acceptable term as well. It is important to note that dementia in itself is not a disease.
Dementia (Major Neurocognitive Disorder)
- Not a specific disease (though sometimes caused by one)
- Memory is typically considered the primary loss of function
- A disorder/group of symptoms characterized by a loss of function:
- Complex attention
- Executive function
- Learning and memory
- Language
- Perceptual-motor function
- Social cognition
(DSM-5 Criteria)
Oftentimes, it is caused by a specific disease perhaps one of which we will discuss today. When you have dementia, most people have memory loss as their primary symptom that indicates something is wrong. The DSM-5 considers dementia to be a group of symptoms that are characterized by a loss of function like attention, executive function, memory, learning, language, perceptual-motor function as well as social cognition.
Now, we are going to discuss some of the types of dementia. There are a couple of primary categories that we are going to discuss today. The major two are reversible and non-reversible, and then under that non-reversible umbrella, we have progressive and non-progressive. We are going to break all of those down today and talk about some of the different causes of each of these types of dementia.
Dementia-Primary Categories
- Primary categories
- Reversible
- Non-Reversible
- Non-Progressive
- Progressive
Reversible Dementia
- D - drug reaction, overdose, toxicity, anesthesia
- E - emotional disorders (depression)
- M - metabolic or endocrine (thyroid) issues
- E - eyes and ears (sensory loss)
- N - nutritional deficits
- T - tumors
- I - infection (sepsis, UTI, pneumonia)
- A - arteriosclerosis
First, we are going to talk about reversible dementias. Some medical doctors will claim that reversible dementias are not dementias, or that they are delirium. The National Council of Certified Dementia Practitioners classifies them as dementias, and because I am a CDP, I also classify them as reversible dementia, but we are going to discuss a little bit of that as we go.
In reversible dementias, the onset is abrupt. The decline is acute right after some type of incident. We are seeing quite a bit of this right now. In fact, we are seeing some signs of delirium or reversible dementia due to the social isolation that is occurring because of COVID-19, whether that is social isolation in a long-term care facility, an assisted living facility, or out in the community and in homes. People who normally would have a lot of social interaction are now having to practice social distancing. People are not able to just go out and go to the grocery store as they were before. My mom lives across the street, and we check on her all the time, but I refuse to allow her to go to the grocery store. I am very adamant that she still does cognitively stimulating tasks during this time because I do not want to see a decline in cognition.
When we look at reversible dementias, it is important to note that we do what we can to take away the cause of reversible dementias and then we assess to see if spontaneous recovery has occurred. If spontaneous recovery does not occur, then that is when we intervene with treatment. We need to take away the cause before we try to treat it because if the cause is still present, then our etiology is there and we are not going to be able to do as much to change those symptoms.
The research shows though that after that period of spontaneous recovery, adults may be left with long-term deficits without our intervention. I believe that this is where health professionals, in the next year or two or maybe even over the next six months, are going to see a boom in patients. The social isolation will be taken away, but clients may not spontaneously recover as they should. They will need our intervention in order to try to get back to that prior level of function.
I have seen some different research about what typical spontaneous recovery periods are after anesthesia, especially on knees and hips that have been replaced. Research says three hours post-op is a typical recovery. I have seen other reports that it is more like a couple of days. Regardless, if you are working in post-acute rehab or in skilled nursing, by the time those patients get to you, they should be past that spontaneous recovery time frame. Thus, if you are doing the Brief Interview of Mental Status (BIMS) to assess for their cognition, under the new PDPM payment model, and you see their BIMS score shows that they have a cognitive deficit, then we cannot expect them to jump right back in and be normal again without our intervention. Again, this is because the typical spontaneous recovery time has passed.
Emotional disorders and depression are a huge cause of reversible dementias. Hence, the social isolation components that have been occurring since 2020 are going to affect many clients down the road. Thyroid issues, sensory loss, nutritional deficits, tumors, and coronary artery disease are other areas that contribute.
When you see a patient who has had any type of cardiopulmonary condition with reduced blood flow or oxygen, these patients are typically showing symptoms of dementia. If you have worked in healthcare for any length of time, you have definitely seen this with UTI, pneumonia, sepsis, gangrene, or any type of infection in the elderly population. You will see their cognition tank. What we know is that once those antibiotics are given and that infection is gone, we should see spontaneous recovery, and if we do not, then this is when we intervene.
Now, in the next couple of slides, I am going to give you some of the information that I just discussed. These studies are listed in your references as well.
- Infection (UTI, Sepsis, Pneumonia, Gangrene…)
- The American Academy of Neurology recognizes that new or past infections can contribute to cognitive impairment
- NIH study documented sepsis was associated with later cognitive and physical decline
- Journal of AMA says that adults with infection “may be left with moderate/severe cognitive deficits and functional disabilities”
- Anesthesia
- British Journal of Anesthesia:
- Increased evidence that major neurological changes can occur post-anesthesia
- Brain particularly vulnerable at the beginning or end of life
- The earliest manifestation of neuronal damage is a decrease in higher cortical functions of storage and recall of memory and cognitive processing
- British Journal of Anesthesia:
- International Anesthesia Research Society
- Recognizes POCD- Post Operative Cognitive Dysfunction
- A study found that 10-15% of the elderly have postoperative cognitive decline at 3 months post-op
- Surgery may “unmask” intellectual declines already present
- Cognitive decline may result from inflammatory processes after anesthesia
- Recognizes POCD- Post Operative Cognitive Dysfunction
- Research on Anesthesia vs. Analgesic effects:
- A study on knee and hip replacements with different types of anesthesia and cognitive function suggested that normal cognitive recovery from both types happens within 6 hours post-op
I have encountered a lot of people in healthcare, over the past 16 years, who are very adverse to cognitive-linguistic, cognitive-communication therapy. What I say to them is that when you look at the research, the evidence shows that these etiologies, infections, anesthesia, etc. absolutely cause dementia. Another thing about post-operative cognitive dysfunction is that many times patients who may have been able to mask their deficits before their operation, now all of a sudden are unable to do so. You may have to ask a lot more probing questions of the patient and/or their family members in order to really determine if there were deficits before the procedure.
What Else Can Contribute to Decline?
- Prolonged Hospitalization
- Agency for Healthcare Research and Quality
- In pts over 70 years old, 39% reported a loss in cognitive status and subsequent ADL/IADL functions immediately after discharge
- 40% reported a NEW loss of ADL/IADL 3 months post-hospital discharge, reflecting the potential for functional decline
- Agency for Healthcare Research and Quality
Prolonged hospitalization is another cause of decline, and this is where that dementia delirium overlap or coexistence often happens. When you look at patients who have extended hospital stays or extended ICU stays, then you often will see what physicians refer to as delirium. However, once they are out of that environment and it does not spontaneously resolve, we have to see if it is dementia versus delirium.
- Mayo Clinic Study states that the strongest risk factors for Mild Cognitive Impairment are:
- Increased Age
- APOE- e4 gene
- Diabetes
- Smoking
- Depression
- Hypertension
- Hypercholesterolemia
- Lack of physical exercise
- Infrequent participation in mentally or socially stimulating activities
The Mayo Clinic, a very reputable institution, produced a publication that referenced the strongest risk factors for mild cognitive impairment or mild neurocognitive disorder. When you look at this list and you think of your parents, grandparents, patients, and maybe even yourself, many fall into quite a few of these categories. As we will discuss in a later session, we need to do our best to mitigate the likelihood that that may occur.
Non-Reversible, Non-Progressive Dementias
- Traumatic Brain Injury
- Anoxia
- Vascular (single CVA)
Now, we are going to discuss non-reversible or non-progressive dementias. These are typically from an abrupt onset like a traumatic brain injury, an anoxic incidence, or respiratory failure. A single CVA can also contribute to that. We are going to talk about more of a progressive type of dementia-related to CVA a little later, but when you look at a single CVA, this would typically be considered a non-reversible, non-progressive type of dementia.
Non-Reversible, Progressive Dementias
- Chronic Traumatic Encephalopathy
- Parkinsons
- Multi-Infarct
- Fronto-temporal
- Lewy Body
- Huntington’s Disease
- Creuxfeldt-Jakob
- Korsakoff Syndrome
- Normal Pressure Hydrocephalus
- HIV Infection
- Alzheimer’s Disease
Today, we are going to talk about many of these non-reversible progressive dementias listed, but there are others that I have not put on this list such as progressive supranuclear palsy, corticobasal syndrome, and dementia due to muscular sclerosis. There are some common types and some less common types, and then there are some rare types of progressive dementias.
Progressive dementias have a gradual onset. They are progressive as the name implies, but they could be slow, or if other factors are present or some of those acute incidents occur while this progressive dementia exists, you could see a very quick progression. For example, you may have a patient with Alzheimer's disease. If this patient falls and breaks a hip and goes into the hospital, the patient's cognitive score may go from a GDS3 to a GDS5, which we will discuss those GDS levels next time. This is a major decline. This is the difference between being able to live on your own to requiring long-term care. This happened to my own grandmother. Anesthesia and hospitalization really took a toll on her Alzheimer's disease, and she had a very rapid decline. I have seen this happen a lot. A client with some baseline deficits but is otherwise pretty stable can rapidly decline with something as simple as a hip replacement.
Chronic Traumatic Encephalopathy (CTE)
- Originally termed “dementia pugilistic” or “punch drunk” in boxers
- Common in people with repeated concussions/head injuries
- Increased tau protein
- Neurofibrillary tangles
- Gaining national media attention
- Symptoms begin 8-10 years after traumas
The first type of dementia I want to discuss is CTE. If you have seen the movie "Concussion" with Will Smith, you will know exactly what I am talking about. It's chronic traumatic encephalopathy. It is also called dementia pugilistica or in boxers, "punch drunk." This is dementia that is common in people who have had repeated concussions or repeated head injuries. With those repeated head injuries, there is increased tau protein in the brain and neurofibrillary tangles occur. This contributes to a rapid decline that you may see.
There is a lot of national media attention on CTE, and I recently had a very close friend whose father passed away who played football in high school, college, and semi-pro. He was also a football coach for 30 years. She was talking about all of his symptoms and alarm bells started going off in my head. I told her to talk to his doctor to see if it could be CTE. She looked up the characteristics on Google, and she said that he had every single symptom that was listed. He ended up passing away before they got a definitive diagnosis, but we are seeing a very delayed diagnosis of about eight to ten years after a football career or after serving in the military in combat.
Symptoms.
- Headache
- Loss of attention/concentration
- Depression
- Explosivity
- Gait and speech abnormalities
- Suicidal thoughts
- Tremors
After those traumas, we are seeing patients coming in with headaches and loss of attention/concentration. We are seeing patients with very short tempers who blow up. There are also gait and speech abnormalities, behavioral issues including depression and suicidal thoughts, and even some tremors that almost look Parkinsonian. When doing a case history, it may be a good thing to ask if they have had repeated head injuries or repeated concussions in their life. Did they play sports like hockey, football, boxing, etc.?
Parkinson’s Disease-Related Dementia
- 50-80% of people with PD will experience related dementia
- Stress is the #1 trigger for Parkinson’s Dementia
- The average time from onset of PD to the development of dementia is 10 years
- Neuro-hallmark is beta-amyloid plaques and tangles
- Cognitive symptoms usually develop a few years after motor symptoms
- Treatment may consist of medications
(Alzheimer’s Association, 2016)
Anywhere between 50 and 80% of people with Parkinson's disease will actually experience dementia. Typically, it takes about 10 years from that diagnosis at onset until that dementia really starts to rear its ugly head. One of the major triggers is stress. When we look neurologically at Parkinson's dementia, we see beta-amyloid plaques and tangles, but typically with Parkinson's dementia, you will see motor symptoms first. We are going to talk about Lewy body dementia in a few minutes, and motor symptoms for that diagnosis show up later, but for Parkinson's disease, motor symptoms occur first and then you will see the cognitive symptoms down the line. Treatment may include medications as well.
Symptoms.
- Slowness
- Rigidity
- Stooped posture
- Shuffling gait
- Depression
- Head bent forward
- Symptoms may be unilateral
- Drooling
- Akinesia (absence of normal movement)
- Tremors
- Mask-like facial expression
When you see a patient that has Parkinson's disease-related dementia, you may see a shuffling gait, a stooped posture, and a forward head. Many times you will see symptoms more unilateral than bilateral. They will also have tremors, akinesia, abnormal movement patterns, and sometimes a very emotionally labile facial expression that is mask-like.
Multi-Infarct (Vascular) Dementia
- 2nd most common type of dementia
- Can co-exist with Alzheimer’s
- Most common in men, aged 55-75
- Remains under-diagnosed
- Caused by reduced or blocked blood flow to the brain (CVA or TIA), usually a series of neurological events (more than one)
- Symptoms similar to Alzheimer’s Dementia, difficult to distinguish
- Risk factors
- Diabetes
- Atherosclerosis (hardening of the arteries)
- Hypertension
- Smoking
- Alcohol abuse
- Stroke
- Poor diet/exercise
- Poverty may be a risk factor
The next type of dementia that we are going to discuss is vascular dementia. This is the second most common type of dementia behind Alzheimer's disease, but it is important to note that multi-infarct or vascular dementia (those terms are interchangeable) and Alzheimer's can coexist. When they co-exist, you are typically going to see a more severe case. Vascular dementia is more common in men aged 55 to 75. This is because CVAs are more common in men than they are in women.
I live in a county in rural South Carolina that has the highest per capita endstage renal disease, diabetes, and stroke rates in the entire state. It is a very high-poverty, Title 1 county. I chose to move back here because this is where I grew up, and I wanted to come back into this rural community and give back. The stroke rates in this community are very high, thus the incidence of multi-infarct dementia is also a lot higher in my county. Multi-infarct dementia can occur from TIAs or multiple TIAs, as well as CVAs. I have had people tell me that they have never had a stroke, but they have had many TIAs.
It is very difficult to distinguish Alzheimer's dementia from multi-infarct dementia without a thorough case history as well as imagery because the symptoms are very similar.
Symptoms.
- Difficulty with tasks that used to come naturally or easily
- Becoming lost on familiar routes
- Word finding difficulties
- Losing interest in prior hobbies
- Flat affect/mood
- Misplacing items more often
- Personality changes
- Loss of social skills
- Change in sleep patterns
- Difficulty with basic tasks
- Safety awareness deficits
- Agitation
- Depression
- Short-term memory loss
- Fronto-Temporal Dementia (Pick’s disease)
- Progressive nerve loss/shrinking of the frontal and temporal anterior lobes of the brain
- Onset to death is 2-12 years
- Caused primarily by a tau or TDP43 protein
- Strong genetic link
- Younger onset, with a quick disease process
- Very poor prognosis
- No treatment has proven to slow the progression of the disease
- Behavioral issues often treated
(Alzheimer’s Association, 2016)
Pick's Disease
The next type is Pick's disease also known as frontotemporal dementia. In Pick's disease, the hallmark sign is a major change in personality. The frontal and temporal lobes of the brain are typically affected. There is nerve loss and there is a shrinking of the brain. We will look at some Alzheimer's images in just a little while, but Pick's disease looks similar in the way the brain appears to have shrunk.
When you look at all the different types of dementia, you will see an onset to death progression from anywhere from six months to 20 years depending on the type of disease that causes dementia and the progression of it. Pick's disease is genetic. Patients with the Pick's are typically younger than your other patients. While patients can learn to compensate for the deficits using some of those remaining skills, pharmacologically there is nothing that has been shown to slow the progression of the disease. We can treat the behavioral issues but the disease itself will progress.
Symptoms.
- Marked changes in personality and mood
- Communication and motor disruption highly prevalent
- Impaired judgment, impulsivity
- Boredom, apathy
- Inappropriate social behaviors
- The patient often unaware of the decline in function or inappropriateness
- Difficulty with language (receptive and expressive)
- Memory remains largely intact
Here are some of the symptoms that we may see in frontotemporal dementia. Your patient may be sexually inappropriate. They may have a great memory but on pragmatic abilities, they are not so great. And, they are often unaware that it is inappropriate. They are not embarrassed by it because they are not even aware it is there. They often have fluent or nonfluent aphasia. You may also see a change in personal hygiene.
Lewy Body Dementia
Lewy body dementia on imaging looks a lot like Parkinson's disease dementia. It is largely under-diagnosed. You will see cognitive deficits first and physical deficits later. The average survival is only about five to seven years with Lewy body, and they will differentiate between Parkinson's and Lewy body by dopamine transporter PET scans.
Symptoms.
- Emotionally/physically labile
- Hallucinations (recurrent, detailed)
- Confusion varies widely from one day to the next
- Shuffling gait and stooped posture
- Depression
- Motor symptoms usually bilateral
- Cognitive impairments begin either before or within 1 year of motor symptom onset
- Repeated falls
- Unexplained loss of consciousness
- Visuospatial abnormalities
Symptoms of Lewy body are very similar to the ones that I just listed with Parkinson's disease. The big difference is in Parkinson's there are unilateral symptoms, whereas, with Lewy body dementia you often see bilateral symptoms.
Huntington’s Disease
- Largely based on heredity (defective gene on chromosome 4)
- If a parent carries a defective gene, the child has a 50% chance of developing
- Affects younger people (30-40)
- Cases affecting people as young as 2 have been documented
- No known cure
- Treatments focus on the management of symptoms
(Alzheimer’s Association, 2016)
Next is Huntington's disease. You will hear it called Huntington's chorea sometimes. It is a genetic condition. It typically affects very young people in the 30 to 40 age range. There have been cases of children as young as two years old with Huntington's disease and related dementia. There really no known cure or way to slow the process.
Symptoms.
- Confusion
- Diminished coordination
- Fidgety, uncontrolled movements (upper body)
- Behavior changes
- Mood changes
- Anger and irritability
- Memory loss
- Hallucinations
- Decreased reasoning skills
- Obsessive-compulsive behaviors
These are some of the things that you will see in Huntington's disease. The fidgety movements are very hallmark, and then the obsessive-compulsive behaviors and hallucinations are also two very common symptoms.
Creuxfeldt-Jakob Disease (CJD)
- Variant CJD is Mad Cow Disease
- Classic CJD is genetic
- The infectious form of Dementia - less common (may occur from exposure to infected bovine products or tissue transplantation)
- Characterized by prion protein that changes cells into abnormal shapes and rapidly destroys
- Rare (1 in 1 million people annually)
- Approximately 200 cases each year in the US (NIH, 2011)
- 90% of patients die within 1 year of onset
(Alzheimer’s Association, 2016)
There are two types. There are classic and variant CJD, and that is more commonly known as mad cow disease. If you guys have been around any length of time, you would definitely remember when the mad cow disease outbreak happened.
As I sit here looking out my window, I am looking at our newborn calves who are less than a week old. In that mad cow disease outbreak, many cows and calves had to be slaughtered because of the outbreak of CJD. It is an infectious form of dementia and 90% of the patients who get CJD die within one year. Luckily, there are not very many cases that occur. It is rare, but when it does occur, prion protein attacks the healthy cells and changes them into abnormal shapes and destroys them rapidly.
Symptoms.
- motor symptoms (ataxia, muscle twitches)
- confusion
- agitation
- memory loss
- severe dysphagia
- personality changes
- seizures
- sleepiness
- dysarthria
- blindness
(Symptoms progress rapidly with no known treatment/ cure)
These are some of the symptoms of CJD, mad cow disease that you will see. These are things you would probably expect when you think of your cells being destroyed including things like blindness, severe dysphagia, and seizures. This has a rapid onset with no known cure.
Korsakoff’s Syndrome
- Most common in patients with a history of EtOH abuse
- Often preceded by Wernicke Encephalopathy- acute reaction to severely low thiamine
- Increased risk if the patient has a history of binge drinking
- 1 in 8 people with alcoholism will develop KS
(Alzheimer’s Association, 2016)
Our next syndrome is Korsakoff's syndrome. If you have a patient who has chronic alcoholism, you may see Korsakoff's syndrome. A therapist called me about two weeks ago talking about a patient, and I asked if the patient had Wernicke's encephalopathy. She said that she was not sure, but she thought he had Wernicke's aphasia and receptively he was very slow. He had a history of alcohol abuse. Again, the light bulb started going off, and I thought of Korsakoff's syndrome. One in eight people who have chronic alcoholism will develop Korsakoff's syndrome.
Symptoms.
- Motor deficits (staggering, stumbling)
- Confabulation (making up information but believing it, often very detailed)
- Disorientation
- Memory loss
- Impaired reasoning skills
- Malnutrition
- Jerky eye movements
- Major changes in personality
- Lack of insight into the current condition
- Socially inappropriate behaviors
It is one of the saddest types of dementia to me personally. I have seen brilliant Ph.D. level professors who suffered from Korsakoff's syndrome. They have staggering, stumbling, confabulation, and tell crazy stories that never happened. They have a lot of jerky movements and stumbling and socially inappropriate behaviors. Wernicke's encephalopathy is a precursor to Korsakoff's syndrome or Korsakoff's dementia.
Normal Pressure Hydrocephalus (NPH)
- Characterized by excessive accumulation of CSF in the ventricles
- Ventricles enlarge and put pressure on the brain
- However, excess fluid does not often present during a lumbar puncture
- Diagnosed by MRI, large volume spinal tap, or intracranial pressure monitoring
- Treatment includes placement of a shunt to drain excess CSF
(Alzheimer’s Association, 2016)
Next is normal pressure hydrocephalus. This occurs when you have a subdural or subarachnoid hemorrhage, head trauma, a neurological infection, surgical complications, or a tumor. My mother-in-law has NPH from an aneurysm, and she has a permanent shunt. Without that shunt, her cerebrospinal fluid would put pressure on her brain. We saw the NPH dementia going on with her until she got that shunt. Typically, with many patients, once you have that excess CSF drained off, some of the symptoms go away but it may not. It may be a long-term process.
Symptoms.
- Difficulty walking (getting stuck or “freezing”)
- Slowing of movements
- Decreased executive functioning
- Loss of continence
- Symptoms will worsen over time if the condition remains untreated
- Apathy and withdrawal/ changes in mood
- Memory loss
- Sudden falls
With NPH, you may see patients who get stuck or freeze in their movements. For example, my mother-in-law would all of a sudden just stop when walking. You may also see a loss of continence. If you do not place a shunt and get some of that pressure off the brain, those symptoms will worsen to the point where it will cause permanent neurological damage. You often see lots of falls, issues with balance, etc. NPH is something that can be treated and managed when it is caught early.
HIV-Associated Dementia
- HIV crosses the blood-brain barrier (BBB) early in the disease process
- Often acts as a “trojan horse” to come into the brain and then creates an inflammatory effect
- Results in encephalopathy
Fortunately, there are many treatments out there now that focus on those T-cells and reducing the viral load of HIV in patients. However, early in the disease process, the HIV virus will cross that blood-brain barrier and acts as a Trojan horse to the brain causing inflammation that can result in encephalopathy.
Symptoms.
- Memory loss
- Mental fog
- Dysarthria
- Apathetic response to activities previously enjoyed
- Reduced coordination
- Decreased motor skills
- Changes in personality and behavior
- Depression
- Social withdrawal
- Sleep disturbance
- Psychosis/mania
- Seizures
You will see patients who become very apathetic, depressed, and socially withdrawn. They either sleep all the time or they never sleep, and they have manic and psychotic type episodes. You might also see dysarthria in speech with HIV related dementia.
Alzheimer’s Disease
- The most common type of dementia (60-80% of cases)
- Progressive, and not a “normal” part of aging
- Usually diagnosed in the mid-60s
- Characterized by memory difficulty, especially newly learned information
- Can be diagnosed pre-mortem now
- One neuro-hallmark is abnormally high numbers of beta-amyloid plaques and tangles
- Primary neuro-hallmark is “wasting away” of the brain
- Major genetic link
- The current research focus is attempting to slow or prevent AD
(Alzheimer’s Association, 2016)
Everyone has heard about Alzheimer's dementia. It is the most commonly diagnosed type, but as many people including healthcare practitioners believe, it is not a normal part of aging. You should not significantly lose your memory and your language function just because you are aging. Typically, Alzheimer's disease is diagnosed in the mid-60s. A hallmark of Alzheimer's is memory loss, especially short-term memory. Patients who can remember what they did 20 years ago but not what they did 20 minutes ago.
It used to be that Alzheimer's disease could only be diagnosed on autopsy for a definitive diagnosis, but now we can have pre-mortem diagnoses occurring. There are beta-amyloid plaques and tangles in that brain structure, and you will almost see a wasting of the brain. I describe it to patients as a shrinkage of the brain. There is a major genetic link. I know my risk is extremely high because of genetics, but I am very hopeful about the current research on slowing or preventing Alzheimer's.
Symptoms.
- Differ by Stage:
- Mild - memory loss, safety issues, difficulty paying bills, executive functioning skill loss
- Moderate - increased confusion, significant language deficits, behavioral issues begin
- Severe - unable to communicate verbally, completely dependent on caregivers, dysphagia prevalent
As we will go into next week, there are different stages: mild, moderate, and severe. The symptoms differ by stages.
Beta-Amyloid Plaques and Neurofibrillary Tangles.
Here is a picture of the beta-amyloid plaques and neurofibrillary tangles in Figure 1.

Figure 1. Beta-amyloid plaques and neurofibrillary tangles (7mike5000, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons).
One thing that you guys will learn about me if you have been around me any length of time is that I like to put things in layman's terms for my patients. Many of them say, "No, the doctor hasn't told me anything about what Alzheimer's disease is." I tell them, "There are little structures in your brain called neurons that almost look like little spiders. The spidery legs communicate with each other but sometimes there is something in between those little spidery legs almost like if you get gum in your hair, and you can't pull it apart. It really gets matted up and there's really nothing you can do to fix it." The gum in hair description is how I describe neurofibrillary tangles.
Neurological Changes.
Here is what a healthy brain looks like compared to severe Alzheimer's in Figure 2.
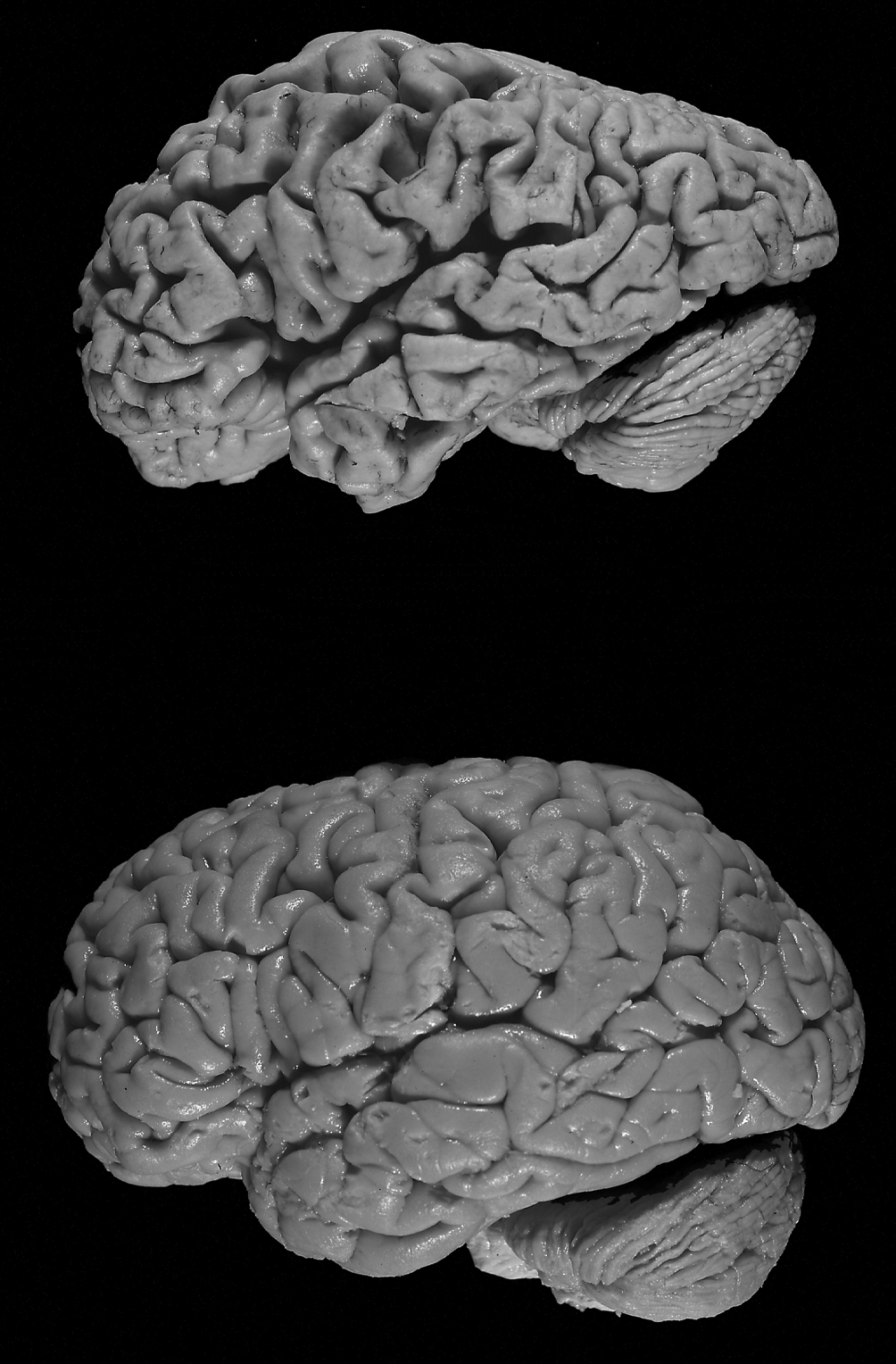
Figure 2. Healthy brain versus a brain with Alzheimer's. (Hersenbank, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons).
You can see the increased size of the ventricles, and it does look like it is shrinking. In our next several sessions, we will go over the neurological changes in each stage of Alzheimer's disease.
Mild Cognitive Impairments (MCI).
- “At-risk” stage of decline
- Cognitive and memory changes are noticeable to others but are not severe enough to seriously interfere with ADLs
- People with CI may get better
- Compensatory activities may slow decline or assist in the progress
- May lead to AD
- Experts recommend re-evaluation every 6 months to diagnose improvement/decline
(Alzheimer’s Association, 2016)
What about mild cognitive impairment? This is the early at-risk stage where people tend to be either in denial that anything is happening or be overly concerned that something may be occurring. This is when you start seeing those memory changes and language/word-finding changes that are noticeable to others, but the person is still fine living at home. They can still cook, clean, and manage their finances, but things are just getting a little harder. You may see people with a mild cognitive impairment that has a reversible type of dementia that will get better. There may be compensatory activities implemented that can slow the decline, but it is about a 50-50 shot. If a person is diagnosed with MCI, about 50% will end up progressing into Alzheimer's Dementia. The other 50% may be okay. My mother-in-law was in the 50% that was okay. After her NPH and her aneurysm, she was diagnosed with MCI, and thank goodness she was the 50% that got better.
Diagnosing Dementia
- Family and medical history
- Brain Imaging (structural, functional, and molecular)
- CT
- MRI
- PET
- Physical exam
- Biomarkers
- Bloodwork
- Spinal tap
- Psychological exam
- Mental status exam
How do we go about diagnosing dementia? It is important to have a family history, brain imaging, blood work, spinal taps, and a mental status exam.
Can Health Professionals Diagnose Dementia?
- A diagnosis must be made by a medical doctor
- Mental status/stage testing may be conducted
- What if we see signs and there is no diagnosis?
- Contact MD with concerns and testing results
- Request consult
- Treat the symptoms under our scope of practice
A therapist cannot diagnose dementia. We can conduct mental status or staging assessments to see the level of cognitive decline, but we cannot give the patient a diagnosis of dementia. If we see a patient with the symptoms and the patient does not have that diagnosis, we need to have a good rapport with that MD so that we can request a neuro consult. We describe the symptoms that we see, and we treat the symptoms. We do not treat the disease process. We cannot stop Alzheimer's disease, but we can treat the symptoms.
What Might the MD Do?
- Medications
- Aricept (1997) - Most common prescribed of AD medications. One dose is taken at night.
- Reminyl (2001) - Used with vascular and mixed dementia. Once (extended-release) or twice per day doses. Linked to renal and liver issues.
- Exelon (2000) - Adds acetylcholine in the brain. Taken once or twice per day. Titration required and potential for GI problems.
- Namenda (2003) - Regulates glutamate activity (related to learning and memory) Often used as a 2nd drug in a “cocktail” approach to pharmacological treatment
There are several medications. I have named four of these here for you. The first three Aricept, Reminyl, and Exelon are cholinesterase inhibitors (CIs), and they decrease the severity of symptoms caused by dementia because the brains keep acetylcholine from breaking down. Acetylcholine is key for memory, mood, and new learning. Those medicines are crucial in keeping the acetylcholine present. Namenda is an NMDA receptor antagonist, an N-methyl D-aspartate receptor antagonist. This blocks the chemical messenger which is glutamate that is released in excess when damaged by Alzheimer's dementia. This gives some protection, they can be hallucinogenic. They are very similar to some of the anesthetic drugs. Sometimes, patients get a cocktail of a couple of different types. You will see the CIs and the NMDAs used together.
Progression of Impairment
- Alzheimer’s Disease is generally characterized into 3 stages
- Early Stage (2-4 years)
- Middle Stage (2-10 years)
- Late Stage (1-3 years)
- From onset to death, the process usually lasts 7-20 years
(Data from NCCDP manual)
Alzheimer's disease is typically characterized into three stages, early, middle and late, and Alzheimer's is typically a seven to 20-year process. There are lots of factors that go into this depending on whether a client has the disease long before they are diagnosed. Thus, they may be in those middle stages often before they are even diagnosed.
Stages of Cognitive Impairment
As we go into our next course, we will be looking at the classifications using the Global Deterioration Scale as well as Allen Cognitive Levels.
Global Deterioration Scale
- 7 Stages
- GDS 1 - Normal adult
- GDS 2 - Forgetfulness
- GDS 3 - Early Confusional State
- GDS 4 - Late Confusional State (Mild Dementia)
- GDS 5 - Moderate Dementia
- GDS 6 - Severe Dementia
- GDS 7 - Late/Severe Dementia
The Global Deterioration Scale has seven stages. Stage one is a normal adult to stage seven which is late or end-stage dementia. That GDS3 is the mild cognitive impairment that we talked about, and GDS5 is the point where the patient can no longer live independently at home.
Allen Cognitive Levels
- Used primarily by OT
- 6 Levels (each with 3 components: attention, motor control, verbal performance)
- ACL 0 - Coma
- ACL 1 - Awareness
- ACL 2 - Gross Body Movements
- ACL 3 - Manual Actions
- ACL 4 - Familiar Activity
- ACL 5 - Learning New Activity
- ACL 6 - Planning New Activity
The scoring for the Allen Levels is reversed from GDS. If you have a GDS1, you are a normal functioning adult, but the Allen Cognitive Level Six corresponds with GDS1. It is inversely scored and can throw people off.
Mental Status Exams
- Brief Cognitive Rating Scale (BCRS)
- Allen Cognitive Level Screen
- ACL Leather Lacing or Placemat Tests
- Clock Drawing Test
- Mini-Mental State Exam
- Functional Assessment Staging (FAST)
- Montreal Cognitive Assessment (MOCA)
- Self-Administered Gerocognitive Exam (SAGE)
- Ross Information Processing Assessment (RIPA)
- Mini-Cog Test
There are lots of different mental status exams. I have listed many of these here for you. Some of these are available online for free, and some you may have to purchase. There are also a few that require certification for you to give them. For example, MOCA is one.
Dementia or Decline?
- Patients with a dementia diagnosis should be on our radar immediately
- Patients whose recent disease process may raise “red flags” to the potential for a decline
- SLPs aren’t treating actual dementia, but the symptoms related to decline
- We can enhance neuroplasticity to assist the patient!
When we talk about dementia or decline, does it really matter? Does it matter if our patients have an actual dementia diagnosis or not? I am here to tell you that the diagnosis does not change what you do. If there is an existing diagnosis that we see in the medical record, this should send up the red flags. We should look at those patients to see where are they stage-wise and see if there has been a major change in function. We have also discussed today some of those reversible dementias or red flag conditions that may cause decline. We may want to evaluate a patient who has those red flag conditions, but it is important to note that we are not treating dementia itself.
We are treating the symptoms related to decline and helping the client to develop compensatory strategies. We are using evidence-based treatments in order to help that patient function as high as possible within their level. And in those reversible cases, we may be able to help the client to get back some of that recent decline that occurred. Our therapy enhances neuroplasticity and helps the patient's brain generate new neurons and synapses. We want those dendrites and axons to sprout and be very flexible. We want them to essentially grow and take over for the networks of the brain that have deficits. This is how I explain it to patients. I always tell them brains are a very remarkable thing, and they really are.
Who Should We Evaluate?
- Patients with s/s language or cognitive deficits
- Patients with a history of cognitive decline
- Patients whose family report a decline in function
- Patients whose staff report a decline in function
- Patients whose recent illness/etiology could indicate a potential safety risk or cognitive decline
Who should we evaluate? Any patients who have signs or symptoms, a history of decline, or whose family or staff is reporting a decline in function. We also need to look at patients who have that recent illness or etiology that we know poses a risk.
Can You Slow Decline?
- The American Academy of Neurology produced a study in 2009 that suggests that people who are “destined to develop dementia” can delay the onset of accelerated memory decline by doing brain exercises
- Reading
- Writing
- Crossword Puzzles
- Board Games
- Card Games
- Group discussions
- Music
- Current events recollection
- Participants who didn’t do these type of activities lost their memory 3 times as quickly as those who did cognitive exercises 7 days per week
A study about slow and cognitive decline shows that people who do 30 minutes a day, seven days a week of cognitively stimulating tasks progress three times slower into dementia.
Questions and Answers
If you see in the chart someone with a brain CT that states there are chronic ischemic changes, is that something that would correspond perhaps to vascular dementia?
Yes, that would be my initial reaction.
Some people are a little bit afraid to discuss Alzheimer's with their doctor because they are afraid that if the diagnosis is dementia, then some nursing homes will not take these individuals. They don't want it on their record so to speak. Do you have any advice for those patients?
I have never encountered in my practice a nursing home that denied a patient because of Alzheimer's diagnosis. I know that certain assisted living facilities will try to look up a patient's cognitive stage because once they are at a certain stage, they require more care. However, I have never actually known a nursing home to deny patient admission due to a specific diagnosis. I sure would hope not. I would be on a soapbox if I heard that.
How long would you wait for spontaneous recovery from a reversible cause before beginning treatment for deficits?
There is research that is out there stating how long spontaneous recovery is for each etiology. For example, after anesthesia, symptoms should resolve in three or four days. For something that is more infectious, you need to wait until that infection is gone and then give at least a few days after that to allow for that spontaneous recovery to occur. The great news is that we are never going to hurt our patients by evaluating them. When in doubt, err on the side of patient well-being.
With the drugs that you discussed that are used to help slow the progression of Alzheimer's, such as Namenda and Aricept, and so forth, do those also work for other types of dementia?
I have not heard of them necessarily being used for other types of dementias. I know several of the types we talked about today do not have any pharmacological intervention. I think most of the research on drugs out there are specifically for Alzheimer's type.
How would we advise patients about lifestyle changes that can also help like exercise and neuroprotective activities?
We will discuss these cognitive stimulation approaches in upcoming talks, but we absolutely should be getting that information out to patients and their families. There is a huge link between physical well-being, physical exercise, and mental acuity.
Here's an example for you of a situation someone has run into. A neurologist completed a mini cognitive test on my dad and said he passed. He told my dad that he was experiencing the normal forgetfulness that happens with aging. What do you suggest we do at this point? Do we get a second opinion or do we try some of the brain stimulation activities and so forth that we were just talking about and check again in six months? What would you do in that situation?
I would definitely really try to do some cognitively stimulating tasks and improve his physical exercise. The more you get your blood pumping, the more oxygen gets to your brain. If you are seeing major signs and symptoms that are interfering with his activities of daily living, as his daughter, I would ask for a second opinion. When in doubt, always get a second opinion.
Citation
Heape, A. (2020). Dementia diaries part 1: Understanding the types of dementia. SpeechPathology.com, Article 20393. Retrieved from https://www.speechpathology.com/
