Introduction
Hello, this is Jenny, and I am with Carrie. A quick disclaimer is that all the images used within this course are commercial-use stock photography. We are happy to be here today to talk about interventions for the early brain and the NICU.
Early Development
When babies are born early or have a complication at birth, there is a focus within the medical community on survival. But, as therapists, we know that they do not stop developing just because they came early or were compromised at birth. Development is multi-dimensional. It is happening all the time, and it is based on the sensory information that our bodies are receiving. It is also experience-based, and the brain matures based on that. The last six weeks of gestation is a very important period of growth and development for the brain and lungs specifically. It is worth noting that the critical period is defined in the neuro world as a time-sensitive, irreversible point in the development of a neural structure or system. Deprivation, during this time, interrupts the maturational trajectory of the entire structure or system. Thus, when we take that brain and lungs out of that environment that they are supposed to be in (the womb), we get chaos.
"What fires together wires together." Every experience from birth onward has an impact on brain development. Premature Infants experience birth trauma and lengthy hospitalization, and this affects how they develop long-term. This introductory course will educate the OT working in a hospital setting on how to start providing NICU interventions.
Let's first do this by looking at the normal environment. When the fetus is in utero, there is movement in fluid, muted sound, flexed positioning, limited light, and it is environmentally controlled. The temperature remains consistent, and there is never any hunger. Our dilemma then is that when they come out early this very critical fetal development period occurs outside of that protective environment of the womb.
Womb (Intro-uterine) Vs. Extra-uterine Environment
We are going to look at the stark difference between the intro-uterine and the extra-uterine environment as noted in Figures 1 and 2.

Figure 1. Womb environment.

Figure 2. NICU environment.
In a Neonatal Intensive Care Unit (NICU), there are beeping alarms, fluorescent lights, hard surfaces, movement against gravity, pain, and, probably the biggest stress for a baby, is isolation from mother. There is a constant assault of stressors, that can ultimately lead to motor delays, cognitive deficits, and behavior disorders that we see long-term in outpatient pediatric therapy. Imagine instead of waking up in your lovely bed at 10 a.m. on Saturday morning, you wake up at Walmart at 3 a.m., naked, and it is Black Friday. It definitely feels different. When you think about that scenario, you could feel some stress I imagine. And remember as an adult, you have intricately organized and matured neuronal processes that help you cope with those sensations. Interestingly, adults, in their highest moments of stress, sometimes will revert back to a fetal position.
The Fetal Brain
Here is a look at that early brain (Figure 3).
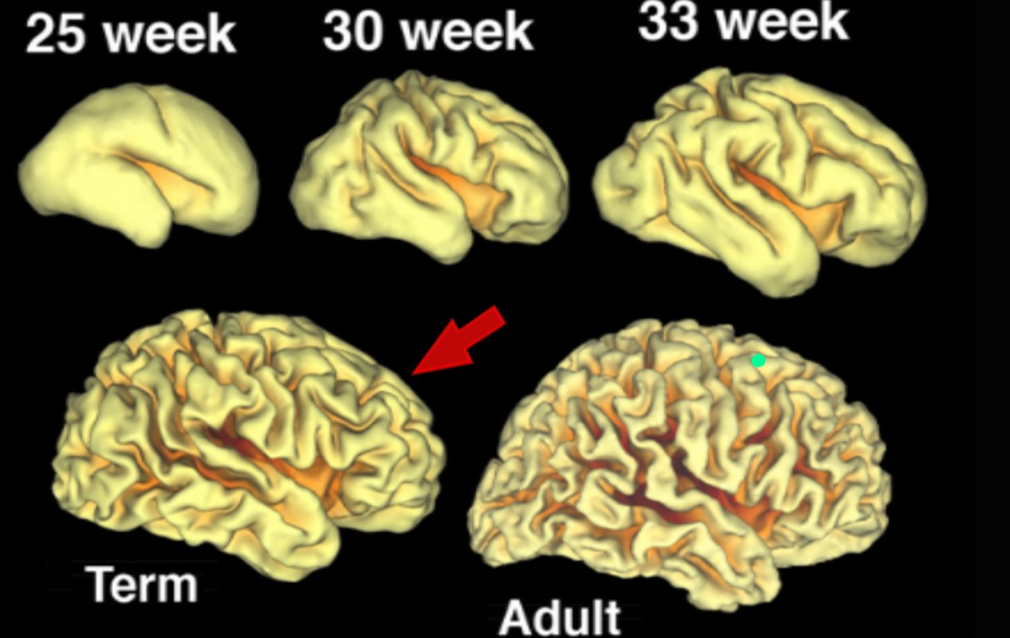
Figure 3. Early brain development.
As you can see, the brain between the 33-week mark and term looks drastically different. You can then see how premature birth can affect long-term developmental outcomes, and also why it is so important to have therapeutic interventions in the NICU. Obviously, we know that those babies born at 26 and 27 have issues developing, but even the babies that come closer to term are still struggling. There is five times the brain growth between 33 and 40 weeks. The difference between a term brain and an adult brain is not huge, but there is a huge amount of brain development happening late in the pregnancy. This is often overlooked in the NICU. In the third trimester, there is a neurological brain growth spurt. Prematurity is a little bit like pulling the cake out just a little too soon.
We also know that the cerebellum is responsible for learning, social-behavioral functions, and complex motor skills like speech and muscle function. Cerebellum development happens in the eight to nine-month window. The Early Childhood Development Center at Harvard came up with a study that looked at this neurological pathway as a way to educate about the importance of early infant experiences. Even up to three months before birth, a fetus is having sensory connections happening with a very steep growth incline leading up to birth.
Neuroprotective Care
No matter what, every baby in the NICU is going to experience some form of an altered foundation in his or her development. This means that every baby in the NICU could benefit from an evaluation by a therapist, and yet, we know is not the common practice. A therapist can provide neuroprotective care. Synaptic functions can be protected from the beginning. When a therapist is involved, we can help the team understand that everybody working with an infant can make a difference in how their brain is going to develop.
As mentioned earlier, in addition to the high risk infants that are born very early with low birth weights, infants that are moderately preterm, born between 32 to 36 weeks, have double the risk for neurodevelopmental disabilities at two years of age as compared to babies born at 40 weeks (Johnson et al., 2015). In another study by McCormick, Mao, and Smith in 2015, 4900 full-term babies and 950 late preterms (37 weeks) were compared for kindergarten readiness. Of all these children, the late preterm babies were 52% more likely to be unprepared for kindergarten. They missed that window of early intervention, zero to three years old, most likely because they did not show any overt developmental delays. But, when they were screened and reviewed for those kindergarten readiness skills, they were not as ready to enter into the academic rigors as their peers. I am sure many of you know people who have had babies at 37 weeks. In fact, inductions are even happening at 38 weeks routinely now in obstetrics. So, this issue that is growing because of how advanced our medical world is getting.
As NICU therapists, we can provide neuroprotective care. It is like an antibiotic for developmental delay, later on. It is what prevents it from happening, and it has to start as soon as that baby arrives. How do we provide this neuroprotective care when a baby is in an intensive care unit? I am going to turn it over to Carrie to address the Neonatal Developmental Care Model.
Neonatal Developmental Care Model
This is Carrie. I wanted to mention that Jenny and I are sisters and are both pregnant with our second child. The Neonatal Developmental Care Model was developed out of the Phillips Healthcare System. It is an amazing measure to follow. It consists of seven core measures and all the measures help to promote normal development, optimal synaptic neuro-connections, and prevent disabilities. When we break this down, we are looking at family involvement, positioning, and handling of the infant, protection of skin, minimizing the stress and pain that they experience, optimizing nutrition, and safeguarding their sleep.
Healing Environment (Core Measure #1)
In the center of the model (Figure 4) is the healing environment.
- Touch
- Smell
- Taste
- Sound
- Light
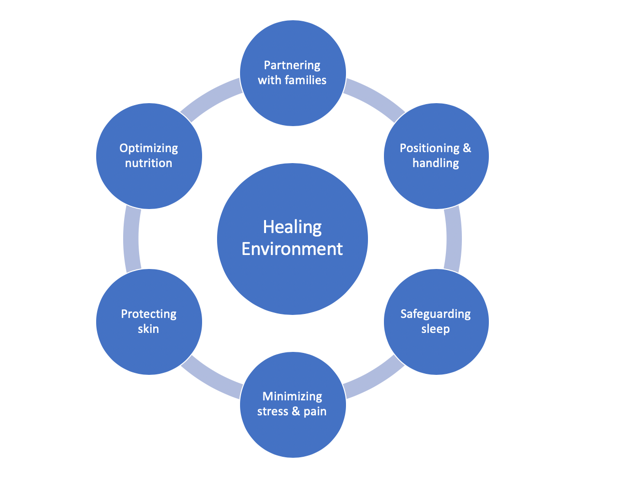
Figure 4. The Neonatal Developmental Care Model.
Again, the NICU is far from a healing environment from a physical and sensory standpoint (Figure 5).

Figure 5. Components of a healing environment.
OTs can go in and address all of the sensory-based sensations that babies experience through touch, smell, taste, sound, and light. Sensory receptors are the connection between our nervous system and the external world. They help us process all the sensory information, and then, that in turn creates behaviors that will develop new skills and begin to regulate attention. When we are looking at the extra-uterine environment, we are looking at a lot of negative sensory inputs that have replaced the positive sensory inputs in the developing brain. This is due to the number of fluctuations that these preemies are experiencing in the NICU. These fluctuations include temperature, touch, movement, smells, noise, light, nutrition, pain, everything. The preterm infant is not prepared to come into this world when they do, and because of that, they are exposed to high levels of inappropriate sensory input repeatedly in the NICU. These changes ultimately can alter normal brain development, how they are able to organize their brain, and eventually adapt to sensory stimuli. When we look at what makes a healing environment, we are not only looking at the physical space, but we also have to address the sensory environment as mentioned above.
An intervention that seems so simple and common sense yet can get overlooked is to use of gentle touch when we are doing all caregiving interactions (Figure 6).

Figure 6. Tactile intervention.
Every time we touch an infant, we have to be aware of the amount of pressure we are giving and how we are engaging with this infant. It starts with an extremely soft and gentle touch. You also want to facilitate skin-to-skin care as soon as possible with a parent or a designated caregiver right after birth. We also need to educate the caregivers about the skin sensitivity of the preterm infant.
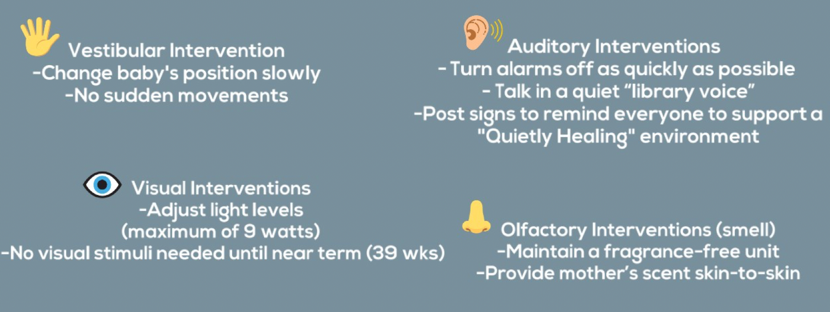
Figure 7. Other interventions in a healing environment.
Some vestibular interventions are changing the baby's position extremely slowly with no sudden movement. Auditory interventions include educating families on how to turn alarms off as quickly as possible and talking in quiet library-type voice. Post signs to remind people that they are in a quiet healing environment. There are extremely bright lights in hospitals, but these light levels can be adjusted in the NICU. The suggested maximum of nine watts. Perhaps, a blanket can go over an isolette. When we are looking at olfactory interventions, smell, you want to always maintain a fragrance-free environment. Using scent from the mother is also extremely important and can be a great tool for a preemie. An example is a breast pad from the mother placed with the baby in the isolette as smell is so strongly linked to memory and calming.
Partnering With Families (Core Measure #2)
Partnering with families is the single most important factor affecting neurodevelopmental outcomes. We know that premature babies have premature parents. Parenting a preemie comes with a level of stress that was completely unexpected. This stress affects the parental bond. Ultimately, the care of even the very sick newborns is the responsibility of the parents and the medical and nursing staff exist to assist them in doing what needs to be done while not usurping the parents' role (Brimblecombe, Richards, & Roberton, 1978). Even in the '70s, we were trying to empower parents to be the caregivers and not feel so much like an outsider. The parents have to take the baby home, and they have to know how to care for it. There was another study (Fawcus, 2004) that found that mothers are superior to incubators, and then this was repeated in 2016 to confirm the results (Luong, Nguyen, Thi, Carrara, & Bergman, 2016). Mothers, again, were found to stabilize preterm infants at birth. All mammalian species studied suffer in the absence of intimate contact with their mothers. They need that bonding and attachment time. Many hospitals, nurseries, and NICUs are built without much consideration of these findings. We need to support the experience of the baby and the family by having everybody, all the disciplines, on the same page to provide a high standard of care.
- Parents viewed as vital members of the caregiving team.
- Supported in their role as the most important caregivers (not visitors).
- Facilitate parents in having medically and developmentally appropriate interactions with their baby.
- Explain the medical and developmental needs of the baby.
- Teach baby's behavioral cues of stress, calm, and self-comfort.
- Encourage early, prolonged, and frequent STS (skin-to-skin) care.
- Remember that those that inspire our confidence the least: need our education the most.
Parents need to be viewed as vital members of the caregiving team, and they need to be supported in their role as the most important caregivers. They should not be considered visitors, which we know is the standard many times. We need to help parents to have medically and developmentally appropriate interactions with their babies. This would involve the therapist explaining the medical and developmental needs of the baby and modeling what the caregiving should be doing, and then practicing it with them. You can also teach the parents about the baby's behavioral cues of stress, calm, and self-comfort. Babies communicate from the very beginning even if they come out early. You want to also encourage early, frequent, and prolonged skin-to-skin care. Remember, there will be all kinds of different patients and families that come from different backgrounds, socioeconomic status, and education so we need to be able to modify interventions as needed.
These are things that only parents can provide as interventions.
- Breastmilk: unique ingredients are neuroprotective
- Skin-to-skin contact
- The comfort of a familiar voice: decreased stress is neuroprotective
- Parental love and attachment: emotional stability is neuroprotective
- Advocacy for life: a more secure future is neuroprotective
- Training parents about neurosensory needs of babies improved white matter development (Milgrom et al., 2010)
If the mother can either breastfeed, and I do not know, depending on where the baby's at in that stage, or pumping is great, because of the unique nutrients that are neuroprotective. Again, skin-to-skin contact is extremely important. The comfort of a familiar voice is shown to decrease stress and is neuroprotective, as is parental love and attachment. Parents are also advocates for life especially when they feel empowered and educated as parents of a premature baby. Lastly, there was a study that showed that training parents about the neurosensory needs of babies improved white matter development (Milgrom et al., 2010).
Positioning and Handling (Core Measure #3)
- Reference is position in the womb
- Flexed, midline
- 360 degrees with well-defined boundaries
Positioning and handling is core measure four. We want to mimic positioning in the womb. Their position in the womb is flexed, midline, and with 360 degrees of well-defined boundaries. They go from that to probably the most common position we see in the NICU, which is an unsupported position where the baby is flattened, abducted, externally rotated due to gravity and the dominance of extensor tone that is present. You can also see a lack of boundaries in Figure 8. There is also a severe head turn preference.

Figure 8. Typical position in the NICU.
Many NICU babies are unable to keep their head in the midline and have a very severe head turn preference. This has been linked to poor developmental outcomes. You can also see the scapular traction and the hip abduction. This baby is also on a hard surface in a very well lit space.
How does therapeutic positioning help?
- Musculoskeletal development
- Neuromotor development
- Physiologic function and stability
- Thermal regulation
- Energy expenditure
- Skin integrity
- Sleep facilitation

