Introduction
Carrie: We are excited to be here. Thank you for having us back. As Fawn mentioned, I am Carrie Molder. I am going to be speaking first today, and then my sister Jenny will be coming on in just a little bit. You heard a little bit about us just a second ago, but what you do not know is that we just had our second babies. On our first presentation, we were nine months pregnant, and basically huffing and puffing through that, but it is a great introduction to this topic on developing in the NICU. It reviews the neurodevelopmental care model. If you have not viewed that, you should check it out. Today is Part 2, and we are going to dive into some interventions.
How Does Stress Feel?
We love this quote. "All living things are in constant communication with their environment. The trick is learning their language." How does stress feel?
- Shortened respirations & SpO2 saturation
- Flood of cortisol suppresses the immune system and inflammatory pathways
- HR + BP increase
Under stress, the body goes into fight or flight and the beginning of adrenaline, noradrenaline, and cortisol responses. Your body experiences shortened respirations and oxygen saturation. A flood of cortisol suppresses the immune system and inflammatory pathways. Your heart rate and blood pressure can increase. Repeated stress becomes chronic stress. Repeated stress, especially that occurs during that critical last trimester of infant development, has profound and long-lasting effects on several physiological systems, especially the central nervous system. This is also true of stress that the infant can experience in the NICU. Caregiving procedures can disturb rest and often bring discomfort or pain daily. Preterm infants are particularly sensitive to handling and pain, compounding the impact of stress-related procedures.
- Caregiving procedures disturb rest and often bring discomfort or pain. Daily.
- Preterm infants are particularly sensitive to handling stress and pain, compounding the impact of stress related to procedures.
- So what would chronic stress feel like?
What would chronic stress feel like for these newborns? Perhaps, this would feel like a live wire. They have come into the world early, and their systems have not matured. They are developing in a fight or flight state. Stress is the single most individualized pathogen for a compromised infant. We found this extremely important to realize because these infants are developing in an already compromised hospital setting with a plethora of germs and pathogens. They are finding that stress tops anything else that they go through.
- Chronic stress
- Reduced brain size in frontal and parietal regions
- Alteration in functional connectivity within the temporal lobes
- Reduced maturation of white & subcortical gray matter
And, the research finds that chronic stress can reduce brain size in the frontal and parietal regions, cause alterations in functional connectivity within the temporal lobes, and reduce maturation of white and subcortical gray matter. This also affects executive functioning, speech and communication issues, and cognitive abilities down the road.
Development of the Human Cerebral Cortex
The two worst things for brain development are stress and pain. There are many brain connections that develop in the last five and six weeks.
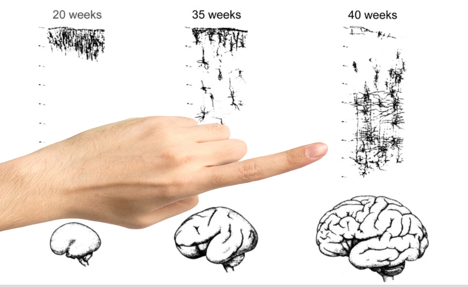
Figure 1. Brain development.
By the time we get to a 40-week brain, the amount of connections has grown. As you can see, this is an extremely critical time in development for just brain growth. Babies that even come 1-3 weeks early are missing a significant amount of intrauterine growth. On top of that, some preemies may have exposure to a stressful NICU setting. Thus, the connections that are being made now under painful procedures in a stressful environment. This is an important concept to be aware of as OT can have an impact on brain development within these five weeks by helping to control the environment. The brain makes connections by going through sensory experiences, positive or negative. The role of an OT is really to try to minimize as many negative connections that they can within the NICU environment. Essentially, what is firing together is wiring together over and over again. They are getting their sensory system set up from the beginning.
Sources of Stress
- Respiratory
- Nutritional
- Infection
- Sensory
- Maternal separation
- Pain
There are many sources of stress. We have identified there are six sources: respiratory stress, nutritional stress, infection stress, the stress of sensory stimuli, maternal separation stress, and stress from pain.
Respiratory
Respiratory stress is when an infant is experiencing respiratory stress. They may have an increased effort in breathing which results in fatigue, hypoxia, and additional calorie consumption. Basically, if you cannot breathe, you cannot eat. And, part of what gets a baby discharged out of the NICU is being a good feeder. So, if a baby is having to work extremely hard just to breathe, they are going to have a longer stay.
Nutritional
There is nutritional stress. Immature receptors in the skin make the experience of handling stressful. However, handling is necessary for feeding. Think of touch in these infants like a "live wire." The baby is experiencing discomfort as they are being held. Their skin receptors are not mature enough. If you pick up a baby and start feeding them without understanding how they are experiencing those stimuli then the baby is going to have issues. Traditionally, volume intake has been emphasized over safe, individualized practice. Techniques such as nipple twisting, nipple milking, and pushing the baby to finish a feed are now known to be stressful with long-term consequences. We know this is a huge area that OTs can help address. In part three of this series, we will explore feeding more in-depth.
Infection
There can be stress from infection. Procedures involving tissue injury heighten the susceptibility of infection, which in turn causes additional invasive procedures to be necessary. This all can lead to chronic stress.
Sensory
One that OTs love to hang their hat on is the sensory environment. Light, noise, smell, touch, taste are all vastly different from an intrauterine environment, where everything is cushioned and minimal. These babies are thrust into fluorescent lighting and a hard isolette. Again, early negative input on a developing brain and nervous system has long-term developmental outcomes. We like to think that the genes are the brick and mortar to the brain, and the environment is the architect. The environment is so impactful on the long-term developmental outcomes of these babies.
Maternal Separation
Stress from maternal separation is another factor. In utero, the mother's biorhythms support the CNS and the acquisition of sensory input. They have found that early life adversity in animal models with maternal separation and pain exposure induces long-term consequences.
Pain
One of the most common factors is the stress of pain. Pain in newborns is both underrecognized and undertreated. Early repetitive pain is demonstrated to have permanent changes in peripheral, spinal cord, and supraspinal pain processing, neuroendocrine function, and neurological development (Ranger & Grunau, 2014). These changes later manifest as abnormal pain states or pain thresholds, increase anxiety and stress disorders, attention deficit disorders, or atypical behaviors, such as hypervigilance and exaggerated startle responses. If you work with pediatrics outside of the NICU, these abnormal responses are absolutely the precursors to sensory processing disorders. It all starts in the very beginning where everything is getting fired and wired together in a negative way.
Predicting Later-Life Outcomes of Early-Life Exposures
Children who had NICU experience, regardless of developmental age at which it took place, were shown to have altered basal nociceptive processing indicative of altered neuronal organization (Boekelheide et al., 2012). This is a really great study. We encourage anyone who is really interested in this area to take a look at it. The title is "Predicting Later-Life Outcomes of Early-Life Exposures.". Without going too far into this, it looks at epigenetics or the expression of genes in the DNA. They found that developmental exposures early on, such as clinical events, are actually mapping and changing genes for later-life outcomes and susceptibilities. This is directly connected to neurobehavior. It is just saying that what babies are experiencing can have a negative effect on actually changing their genes and DNA. What does this mean? This early stress is not just affecting physiological stability but later outcomes as well. Say your NICU baby goes through a painful procedure like a routine heel stick. The baby then tries to process that painful procedure. Then, after about 10 minutes, it is time for their first feed. However, the baby has a poor feed because they are still processing what had just happened. During the feeding, they may have low oromotor skills and the feeding experience is not optimal. Remember, what fired together and wired together. This first negative experience carried over into its first feed. This may then continue to spiral so that it affects many later sequelae like their first smile, ability to roll and so on. Everything can have a snowball effect in the NICU. It is not just a simple heel stick as the baby will get over it. Rather, it is these repeated negative exposures that are changing the brain. How do we handle a baby under all this stress? I am going to pause and let Jenny take over from here.
Positioning and Handling
Jenny: We are going to bring it all together here in this next part. The reason you have to understand stress sources is because this will guide your handling. You have to be aware of the aforementioned six areas of stress to help you to lay your groundwork. And, if you are ever interested in working in the NICU environment, the previous information and the following theory will change the way you do your work.
Synactive Theory
The synactive theory was created by Dr. Heideliese Als. She came up with these brilliant five states of regulation. She studied infant behavior in these stressful environments, like NICUs, and came up with a way to understand what the baby is telling you within the moment. This is the "language of the neonate."
- Autonomic
- Motor
- State
- Attention/Interaction
- Self-regulatory
We are going to start at the bottom which is physiological stability or the autonomic state. This is going to influence the motor organization of the baby, which then obviously influences their behavior state, attention and interaction, and then self-regulation, or the top of the pyramid. All of these systems are dependent on them working harmoniously.
Autonomic. The autonomic system is expressed in all basic physiological functions necessary for survival.
- Respiration
- Cardiac
- Digestion/elimination
- Thermoregulation
One is respiration which is the rate, the saturation, and the expenditure of breathing. Cardiac is the beats per minute and the circulation pressure. For cardiac, if their heart rate goes above160 beats per minute or less than 100 during handling, that is definitely a stress sign being sent. There are digestion and elimination. Occupational therapists play a huge part in babies transitioning to oral mouth feeds. Digestion and elimination also include the smooth intake of nutrition, bowel movements, and urination. Finally, there is thermoregulation. When this system is stressed, there are many changes. For example, in respiration, you are going to see significant changes in the infant's breathing rate. Respiration rates dropping below 40 or going above 60 breaths per minute or a change in the breathing pattern are examples of stress responses. Most OTs know that if the oxygen saturation drops below 90, the client is having a problem. This also applies to the NICU. There can also be changes in skin color. Identification of this becomes much clearer as you begin to practice in the NICU. There can be oddly timed coughing and sneezing or even hiccuping. These usually happen during a stressful feed. A baby will pause and start coughing or sneezing suddenly. And, if you missed earlier stress signals, these are a definite red flag to you as a therapist. "Something is not right." They may also demonstrate gasping or gagging during feeding with excessive spitting up. They can strain without a bowel movement or have excessive residual feeding left. We deal a lot with babies who are not digesting at the rate that we know is normal.
Technology in the NICU setting focuses only on identifying autonomic stress because those are the basic survival mechanisms. However, this is at the expense of the motor, state, organizational, and the self-regulatory systems which are interdependent and rely on that bottom pyramid. When we affect one state, we affect another. However, only the physiological or autonomic system is monitored by the beeping alarms.
Motor. The next system is the motor subsystem, and this is observable through the infant's muscle tone, movement, activity, and posture.
- Finger splaying
- Taut mouth
- Nasal flaring
- Furrowed brow
- Stiffening or flopping of musculature
These are the stress motor signs that are most observable. You might see a finger splay. This has been nicknamed the stop sign, and this is when a baby stretches out its hand in full extension. A taut mouth is another stress sign. Usually, if they are awake or asleep, they are going to have a relaxed mouth. Any tightening of oral musculature is definitely a sign of stress. They can also demonstrate nasal flaring and a furrowed brow. This next sign takes a little bit of practice to notice, but once you see it once or twice, you know exactly what it is. A baby being handled will suddenly stiffen, almost in like a spasm in response to the handling that they are receiving. Or, they will do the exact opposite. They kind of melt and go floppy. This can happen quickly.
State. The next area is the state subsystem.
- States of arousal
- Deep sleep
- Light sleep
- Drowsy
- Quiet alert and active alert
- Cry
This is the level of central nervous system arousal. Is the baby drowsy or sleeping, alert, awake, fussing, or crying? This is the subsystem that gets abused the most in the NICU because people can be so procedure-driven and on a time clock. "I have to do what I have to do right now." This almost never gets paid attention to by general caregiving. Sometimes, a therapist is the only one intervening on behalf of the baby based on their state. In part one of this series, we talked about the importance of sleep for brain development and infant growth. You would think that would be the number one thing that a hospital would protect. However, again due to time schedules, people do not always take this into consideration. Thus, many procedures are completed at the expense of important brain growth.
Therapists will often leave a baby sleeping and check on another instead. And, when you begin to treat a baby, you should be watching them transition between different states in a smooth and predictable manner. This is sometimes hard to observe at first. In infants with birth trauma or drug exposure, you may see these transitions more readily as they are often more twitchy. However, the more you practice within this environment, the easier you can identify the different states of arousal.

