Cara: This is a topic that is near and dear to my heart. I have a very intimate knowledge of it as a parent and also as a professional. I am really glad to be here and to be sharing this information with you.
Introduction
Some of you taking this course may be thinking, "I do not see a lot of kids with mitochondrial disease." My answer to that is you may see more than you know. We see it in many kids with autism because it mimics some other conditions. I challenge you to think about it in a different way because it may be present, but no one is aware. Today, I hope to give you some strategies to use in your clinic, whether you are working in school, home, early intervention, or in any setting.
My son, Joshua, has mitochondrial disease. Both of my children have autism spectrum disorders. My younger one is GJ tube fed. We will talk about what that specifically means in a little bit. This is a picture on the slide of my son Joshua. This is about four years ago, and he is now 15 years old.
Figure 1. Cara and her son, Joshua.
Mitochondria
What does mitochondria do, and why is it so critical? Here is the way I think about it. Think about food as a foreign currency that must be converted in the mitochondria. When you are in another country, you may need their currency. It is useless; it is the same thing with the mitochondria. The foreign currency is cash and coins that we might be using, and in this mitochondria example, the currency is glucose. We all know that glucose is a form of sugar. Food is broken down by the body into building blocks. We create energy from these building blocks, and there is a lot that can go wrong in that process.
The mitochondria's primary function is to provide energy to our body. Cells that require a lot of energy have a high number of mitochondria. We do not carry battery packs on our backs, like this picture of Joshua in Figure 2.
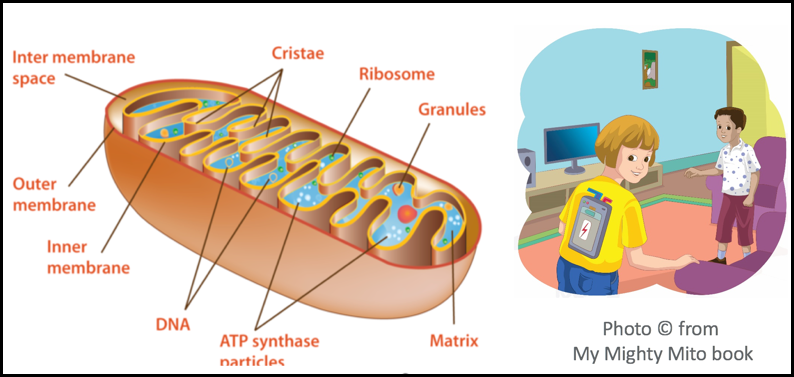
Figure 2. Mitochondria provide energy.
Joshua always says, "Can't we just plug me in to give me energy?" Unfortunately, that is not the case. It can be very frustrating because most of us do not even think twice about the process.
Case Study 1: Joshua
Joshua is medically complex. He has Ehlers-Danlos, which is a connective tissue disorder, autism, and speech issues. He has had 8 years of OT, PT speech, ABA and psychology. Many children with mitochondrial disease present like Joshua because they have an "energy crisis" throughout their body, and it affects a lot of different systems/organs. They may have seen a plethora of physicians and therapies in their life. I am a trauma-informed clinician, and many of these kids have a lot of anxiety due to all these medical processes and constant testing. You may see posttraumatic stress disorder type issues in these kids.
One thing that is interesting about Joshua is that his hair, nails, and skin change color throughout the day. For example, his feet turn purple when he sits in a chair. This is called dysautonomia or an issue with blood pressure. If your blood is pooling, the heart is not pumping effectively. Temperature issues, fatigue, limited activity are all very common.
Let's talk about the digestive system briefly. The first portion of the stomach is the duodenum. The jejunum is where absorption of food takes place. Many children with dysmotility of the stomach need a GJ or G tube, and then maybe the placement of additional tubing down through the small intestine. When kids have these sudden decreases in function, they might be called MELAS, or a metabolic stroke. I encourage you to look that term up after this course because that is one of the big complications of this disorder.
Case Study 2: Mary
Let's look at Mary. She is eight years old and has a genius IQ. She loves to socialize, but she has fatigue and migraines that prohibit her from attending school. She also has a lot of anxiety. She also has a decreased ability to gain weight, and she feels full despite having taken only a few bites of her meal. She has decreased interoceptive awareness, and her stomach is not working as it should. She also has a thyroid disorder. She misses a lot of school because of her fatigue.
Over the course of this talk I will refer back to these cases for reference.
Mito Facts
Let's talk about the mito facts specifically.
- The mitochondria can quickly change shape and move around the cell when needed.
- The mitochondria can reproduce by growing and then dividing, when the cell needs more energy.
- If the cell needs less energy, the mitochondria will die.
- Different mitochondria organelles produce different proteins, and they can be used for various functions.
- The energy form of ATP also produce small amounts of carbon dioxide.
- The mitochondria are found in both animal and plant cells.
- Mito cells are responsible for creating 90% of the energy needed to sustain life and support organ function.
- The parts of the body that need the most energy, such as the heart, brain, muscles and lungs, are the most affected by mitochondrial disease.
- When mitochondria malfunction, organs start to fail causing sickness and even death.
- OTs are uniquely poised to help with energy conservation, optimize functional outcomes, and provide quality of life for those affected by Mitochondrial Disease.
- Mitochondrial disease is an inherited chronic illness that can be present at birth or develop later in life.
- It causes debilitating physical, developmental, and cognitive disabilities with symptoms including: poor growth; loss of muscle coordination; muscle weakness and pain; seizures; vision and/or hearing loss; gastrointestinal issues; learning disabilities; and organ failure
- It is estimated that 1 in 4,000 people has Mito. It is progressive, and there is no cure.
These kids are going to need ongoing tips, tricks, and techniques. For arthritis, we teach energy conservation. We can do the same thing with mitochondrial disease. We need to teach them how to use the energy that they have in a good way and how to conserve energy for future.
Fast Facts
My son was diagnosed 10 years ago when he was 5 years old. We knew a whole lot less about the disorder back then. We did not know about some of the treatments that he would need to keep him functioning at his best.
- Can occur across age groups
- Deficits in mitochondrial structure or enzymes contained within organelle
- One of the fastest growing areas of genetics
- Linked to rare childhood disorders and even heart disease, Parkinson’s, diabetes, and dementia
If the mitochondria are not working, recovering from an illness might be really hard. For example, when you are recovering from the flu, you need a lot of energy. This is why your body rests during an illness because it is fighting germs and bacteria. What about posture? When we are sitting upright for a long time, our posture and our core musculature require a lot of energy. When you are cold, your body has to shiver, and it is an entire body process to warm up. Likewise, when you are hot, your body needs to use entire body systems to cool down. What about stress? If we are not monitoring stress levels, children with mitochondrial disease can experience many physiological effects, such as heart issues. The release of cortisol in long-term cases can really cause autoimmune conditions. It is amazing to think how this disease can affect a lot of systems. The interesting thing is it affects many age groups. This is simply because kids that have mitochondrial disease turn into adults. A lot of people ask me, "Is your child going to live a normal life?" I say, "Well, there's nothing normal about anybody and his life expectancy is same as anyone else."
There are different forms of mitochondrial disease that are typed. We will talk about the types in a little bit here, but there is a type that is very degenerative and can cause defects in heart valves. There are also some areas that are more severely affected than others in the disease. It has been linked to heart disease, Parkinson's, diabetes, dementia, and other things. This is similar to the rise in autism. Do we have more autism these days or is it just our ability to detect it is getting more sophisticated? It is the same thing with mitochondrial disease. It is still rare, but it is the fastest growing area of genetics.
However, not every geneticist is familiar with it. We live in South Carolina, and we travel to Georgia for a geneticist. She charges $500 per hour, and our insurance covers none of that. One of the stresses for families is going to be financial, and it can take a huge toll on families. We sold our house a few years ago because the formula and medical supplies needed to keep my son alive was more than our mortgage, so we lived in a one-bedroom apartment. I have two boys. We lived in a one-bedroom apartment for two years, until Medicaid picked up the copay. You can see how this can be a financial burden.
Diagnosis
Diagnosis is one of those things that I get a lot of questions about. It takes a long time to diagnose mitochondrial disease as it can look like dysautonomia, where you have pooling of blood and unregulated heart rate. It can also look like thyroid disorder. What about asthma or autism? Some of it can come from not enough energy getting to the brain.
- Detailed history
- Battery of complex tests
- Muscle biopsy
- Genetics
- Blood testing
- Maternal line of inheritance
- Retinal pigment
- Heart diseases
There is a battery of tests, but there is no official test for mitochondrial disease. This is like lupus and even autism. There are many symptoms that correlate with the disorder. This disorder has things like decreased use of energy on certain blood tests. In the Diagnostic and Statistical Manual (DSM), there are four points of clinical signs and symptoms of muscles, central nervous system, metabolic issues and imaging studies. Then, there is histology, meaning tissue biopsy. An invasive test is a muscle biopsy, which is extremely painful. I have never had a muscle biopsy for my son because he was typed. I have mitochondrial disease as well (maternal line of inheritance).
Signs and Symptoms
Here are some signs and symptoms that we did not discuss.
- Poor growth
- Loss of muscle coordination, muscle weakness
- Neurological problems, seizures
- Autism, autism-like features
- Vision problems
Poor growth is one of the major signs and symptoms. When my son was little, I saw an article on mitochondrial disease. There was a girl in high school that was only 3 1/2 feet tall. It was just so disheartening to me that that was how he was going to look. This is not necessarily true anymore because there is now supplemental care. My son and most of the kids I work with are low on the growth curve. Seizures are also common. Seizures can happen when there is not enough oxygen to the brain or there is an insult to the head. Most of the kids that I work with and live with have seizures. There can also be vision problems as the eye requires a lot of energy. There is a lot of real estate in our brain just dedicated to the eye.
- Hearing problems
- Developmental delays & learning disabilities
- Heart, liver or kidney disease
- Diabetes
- Neuropsychological changes characterized by confusion, disorientation, and memory loss
We can also see hearing problems, learning disabilities, and heart, liver or kidney disease. I have had kids describe disorientation, memory loss, and something they they refere to "brain fog".
- Increased risk of infection
- Thyroid and/or adrenal dysfunction
- Autonomic dysfunction
- Gastrointestinal disorders, severe constipation, GI motility issues
Another problem is an increased risk of infection.

Figure 3. Joshua under the weather.
Protecting these kids from infection is critical. This is one of the reasons a lot of these kids are either home bound or caregivers have to sterilize their environment. Gastrointestinal disorders and autonomic dysfunction are other issues commonly seen. Autonomic function is the way that our body controls our hormones. When we are in a fight or flight mode, we release cortisol and stress hormones. But when we are in a rest and digest mode, we can metabolize what we have eaten. This one of the reasons why our body needs extra rest when we have these disorders.
Nutrition Support
To support these kids, it is important to work with a dietitian.
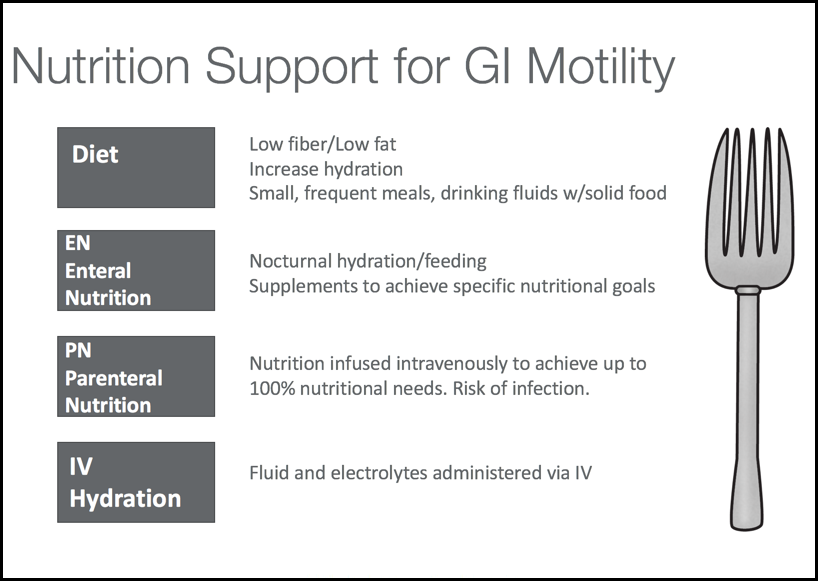
Figure 4. Nutrition support.
We want advise a low fiber and low fat diet with a lot of protein and usable things that they can convert to ATP. An example of a daily food log and fluid log for a child with mito.
- 6-8 a.m.: Cheerios, peanut butter toast.
- 8-10 a.m.: a Popsicle and some crackers.
- 10 a.m.-12 p.m.: Egg salad sandwich
- 12-2 p.m.: Cheese stick.
This is about small doses of food rather than large amounts. It takes too much energy to digest a large meal. Smaller and frequent foods and drinks are going to help these children. Per oral, or PO, nutrition is by mouth.
Enteral nutrition, in contrast, is providing food directly into the stomach and the GI tract. We could do enteral nutrition through several ways, and we will talk about those next. Parenteral nutrition is when you give through an IV. It is nutrition infused intravenously through a cental line. Many kids using this get infections. Infections in the central line are dangerous because it is directly feeding into the neck. Additionally, many kids' GI systems ultimately shut down in times of crisis thus IV hydration is a nice option to have. Anytime we can get fluids for my son via IV hydration when he is sick, it always pumps him up.
I use Thrive Rx, and they have some great information for us on dietary fat that we can share with families. Remember, we want to offer small amounts at each meal. Extensive research has demonstrated that patients on a high-fat diet experience more abdominal pain, discomfort, nausea, and vomiting.
Hydration is so important for all of our bodies, especially for these children. I think it is wonderful that schools are now allowing water bottles. Fluids can be delivered through their feeding tube or through the mouth. We use a lot of Pedialyte through my son's tube. It is very nice for him because it gives him a little pump of energy. When we do it enterally, we can reduce the volumes that they need and really rehabilitate their intestines. We can pump up the intestine with fluids and a little bit of nutrients, like sugar and other electrolytes. This helps the child to get a little bit more absorption. Go to Thrive Rx to get more details.
