Beth: Hello and thank you all for taking the time today to advance your knowledge base on the role environment plays in aging in place. I am a postdoc associate at the University of Pittsburgh, and I am working on research to promote quality geriatric care and increase recognition for person and family-centered care. Before earning my PhD, I worked in an inpatient rehabilitation setting and a home heathcare agency, primarily serving older adults.
Aging in Place
Aging in place is the ability to live in one's home and community independently, safely, and comfortably, regardless of age, income, or functional ability level (CDC, 2013). Aging in place further means that the adults are actively seeking and engaging in daily activities, both within their home and their larger community. A recent report from Home Advisor on aging in place notes the following statistics related to aging in place (Cusato, 2016). It found that 68% of older adults feel independent in their home, and 66% feel safe in their own home and that their home is conveniently located. It was also reported that 38% live close to their family, and 54% are familiar with their community. These statistics alone provide us some insight into areas that occupational therapy providers may want to consider assessing and potentially addressing.
Distinct Value of Occupational Therapy
Occupational therapy providers have a distinct value from other healthcare professionals. We can play a significant role in helping aging adults remain in their homes. Occupational therapy providers are skillfully trained to examine the relationship among person factors, occupation (discreet task factors), and environmental factors. The interaction between these factors determines the client's level and quality of occupational performance. It is critical that we think of these factors together, but today we are going to focus our attention on the environment. The environment is particularly important to assess and address because occupational therapy providers are trained to understand the person environment interaction. Many other healthcare disciplines tend to concentrate solely on person factors, especially body structure systems and functions. To help guide our professional decision-making and actions when working with clients, we, as providers, need to blend theories, models, and personal experiences. There are several types of models that occupational therapy providers can refer to, but because we are focused on environment today, we are going to discuss ecological models.
Ecological Models
What are ecological models? These models embody the person environment interaction. The distinguishing characteristics of ecological models include the dynamic and distinct relationship between people, occupations, and environment, and dynamic here means that these factors are not static, and are instead, active and can fluctuate in the moment or over time. Distinct means that each of those domains, person, occupation, and environment, have their own meaning and contain unique elements. Another feature of ecological models is that environment is a major factor in determining success. With that said, it is often more efficient to change environmental factors than person factors. We will get into some specific case stories a little later to illustrate this point.
A more recently developed model that was derived by occupational therapists in Canada is the Person-Environment-Occupation, or commonly referred to as the PEO model. This model symbolizes that person-environment-occupation relationship that I just shared. In addition, this model stresses that this interaction is dynamic and that people are always involved with or in their surrounding environment. This connection can be depicted as either enabling or constraining on our client's ability to perform desired occupations. We can see in Figure 1 that when there is congruency among the person in their environment and the occupation being performed, it is a good fit.
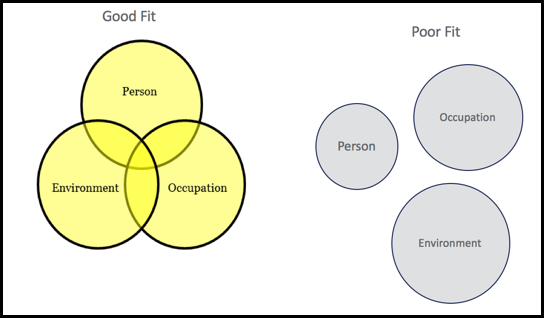
Figure 1. PEO model.
For example, an older adult with diabetes is provided the necessary equipment and training to manage his chronic condition at home independently. On the other hand, when there is incongruence, or a poor fit, a factor or multiple factors are not supporting one another in the moment or even over time. An example could be when an older adult was discharged home after a hip replacement with no social support and is unable to safely complete his activities of daily living and instrumental activities of daily living because of his standard hip precautions. Now that we have a basic understanding of one commonly used ecological model, the PEO model, let's dive into the explicit terms used in practice.
Context and Environment
The third edition of the Occupational Therapy Practice Framework and domain articulates definitions for both context and environment. Context refers to elements within and surrounding a person that influences how they perform an occupation, or more broadly, the situation at hand. Environment refers to the natural and built physical surroundings and other humans who may have a potential influence on a situation. These terms are very similar by their definitions and can often be used interchangeably (AOTA, 2014). To better understand these terms for use in practice, it helps to think of categories nestled under each as in Figure 2.
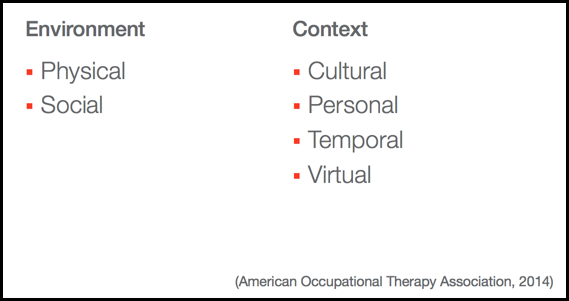
Figure 2. Categories of environment and context.
Two categories under environment are the physical and social environment. Physical includes both the natural and built surrounding, as well as objects. This can be everything from furniture, a width of a doorway, or to a grassy slope of a backyard. Social environment includes the presence of relationships or expectations of persons, groups, or populations with which that older adult has contact. This includes family, friends, pets, and expectations of a living setting such as an assisted living facility. There are four context categories: cultural, personal, temporal, and virtual. Cultural includes customs, beliefs, expectations of a society of which that older adult is a member, and this is different from social environment in that it does not require direct contact like the social environment does. Personal includes the features not part of health. This generally refers to those demographic pieces such as age, gender, socioeconomic status, and educational status. Temporal context refers to considerations such as time of day, time of year, how long it takes to complete an occupation, or even the speed at which the occupation is being completed. Lastly, the virtual context is a growing consideration for many of our older adults and includes communication that occurs in the absence of physical presence.
Aging in Place Examples
Let's apply these category descriptions to some real-world examples of aging in place. I want you each to think about those categories we just learned and try designate which category each of these examples represent.
- An older adult can no longer ascend or descend the small spiral stair to access and participate in their church choir (Physical environment).
- An older adult stops driving and doing their laundry because their family insists, not because they cannot do it (Social environment).
- Older women may not feel dressed unless they can put on their girdle, and older men might need to be able to put on their suspenders (Cultural context).
- An older adult has more difficulty figuring out how to navigate signs related to a traffic detour because of cognitive changes related to age (Personal context). This is an example of a personal context in particular because it is age-related, not necessarily health status-related.
- An older adult has difficulty crossing the street in the 10 seconds allowed by the light (Temporal context).
- An older adult interacts with their grandchild who lives across the country via Skype (Virtual context).
Now that we know the distinction and categories of environment and context, I want to share some practice considerations to guide your treatment planning and implementation to support successful aging in place.
Physical Environment Considerations
Some questions to think about related to the physical environment can include:
- Does the client live in their own home?
- Is the home a one story or a two story?
- Are they living with others?
- What type of living situation is it?
- Is it an apartment?
- Even more specific, what type of apartment is it? Is it a senior apartment, independent living, or assisted living? These each have distinct amenities within.
- More notably for our older adult population and whether they are involved in the community is where is their home located, or the physical environment in which they live?
- Is it an urban setting? A suburban setting? Or rural?
Social Environment Considerations
Social environment considerations can include:
- Is the client married and living with their spouse? If they are not, are they single or are they widowed?
- Does the client have family? Is that family close by and able to assist?
- Are there friends or neighbors nearby who can support your client that wants to age in place?
Contextual Considerations
Culturally, we should think about instrumental activities of daily living in particular, especially expectations based on gender and age. Personally, we should be thinking about formal education and ability to understand the information that is being presented to our older adult clients, or their health literacy levels. You should also be thinking about their financial status and their ability to buy any equipment or make home modifications that we are suggesting. Some temporal considerations include the varying ability of our clients completing activities of daily living and instrumental activities of daily living based on the time of day and the length of the activity. This is particularly important for our older adults with endurance restrictions. Are they spacing out their activities throughout the day? Are they trying to complete everything in the morning and rest during the afternoon? These are all things that can help to shape our interventions. Virtual considerations include all the advances in technology. This encompasses those features or objects that people want versus those that may expected of us to use, such as a cell phone or computer. Not all older adults will want or know how to use technology to stay in touch or to check their medical care.
Environmental Assessments
There are a significant number of tools to assess the environment surrounding our client, and these tools can range in settings in populations served.
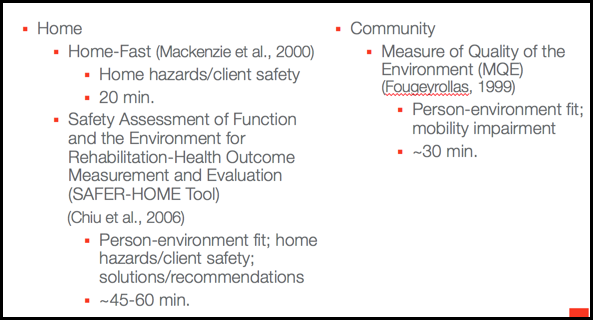
Figure 3. Examples of assessment tools.
I do want to note that there is no gold standard for occupational therapy providers for an environmental assessment to help support our clients age in place. However, I do want to point out several existing environmental assessments that occupational therapy providers can use in practice to gauge safety, comfort, and independence when aging in place.
The Home-Fast Assessment (Mackenzie et al., 2000) takes about 20 minutes to complete and is focused on home hazards and the client safety perspective. Another home-based assessment is the Safety Assessment of Function and the Environment for Rehabilitation-Health Outcome Measurement and Evaluation Tool, or SAFER-HOME Tool (Chiu et al., 2006). This assessment takes a bit longer and can range from 45 to 60 minutes. It goes beyond assessing home hazards and safety and includes domains focused on that person environment fit that we discussed earlier and suggests solutions based on different responses. Because aging in place also involves community participation, I wanted to suggest the Measure of Quality of the Environment (Fougeyrollas, 1999). This tool takes about 30 minutes and is focused on that goodness of fit with the PEO model but tends to have more of a focus on mobility impairment and ability level of getting around within the community.
Assessment Tools to Promote Aging in Place
There are also several assessment tools to promote aging in place. One is the Assessment of Life Habits and is designed specifically for adults, and this tool assesses the level of performance in life habits within various contexts, and contexts meaning situations. It could be within the community or within their home. And certain areas that are specifically addressed include the older adult's nutrition, their fitness, communication and social rapport with others, their housing, community, and then some of those demographic pieces, including their education and employment status as well. Another one that comes to mind that has been around for quite a long time is the Instrumental Activities of Daily Living Scale, from Lawton. He introduced that scale way back in the late '60s, so that is more commonly used in practice as well. There have been several adaptations to that tool. It is specifically for older adults, so 65 years plus, and assesses independence particularly in the different instrumental activities of daily living categories that are outlined in the Occupational Therapy Practice Framework.
Now that we know some environmental and contextual considerations, along with examples of assessment measures, I want to transition to learn some types of intervention approaches that occupational therapy professionals can implement.
Intervention Approaches
Occupational therapy providers use their clinical reasoning to determine which intervention approach to use with their clients. Our clinical reasoning refers to the processes that we use to plan, direct, and perform the care we provide our clients. The three types of approaches that I think are most relevant for the environment or contextual characteristics include the modify, alter, and prevent approaches.
Modify is a change to the environment or task to enable our client's performance range. This can include providing our clients assistive devices such as an adaptive car for driving or a built-up spoon for eating. These examples change the physical environment. Another example of a modify approach is to provide education on healthy routines to our clients involved in a senior center or perhaps an adult day center. This is a modify strategy because the social environment is being changed. A last example of this approach is to change the daily household routine for our clients with endurance problems. We can suggest that physically demanding tasks are spread out throughout the day instead of our client trying to get everything done in the morning.
The alter approach does not change the person, task, or environment, but it makes it a better fit. An example would be suggesting to a client to move their bedroom from the 2nd floor to the first if the client has limited endurance. Another example is suggesting to the client that they move to a ranch home, if feasible. We can help our clients find an organization to join based on values or interests, and this could include workout centers, church groups, or community art centers to name a few.
The prevent approach is when we change the course of events when a negative outcome is predicted. This approach is implemented before a problem develops with our clients. An example could be using a special cushion in a wheelchair to prevent pressure ulcers. Another example could be showing our client how to use a front wheeled walker for home and community mobility to provide more stability for our clients, as well as prevent falls.
There is a fine line between the modify and alter approaches, and they can overlap. Just because you are using one approach, does not mean you are not using the other approach as well. As an example, you may suggest altering something, and then if they do decide to change their daily routine and implement that social activity into their routine, they are moving toward a modify approach.
