Overview
This webinar was really inspired by my time at the 2018 AOTA Conference in Salt Lake City. I was fortunate enough to be a part of a group of clinical educators as well as academic clinicians, and we were talking about the value of culture. We use a lot of jargon in our profession, but it is really hard to conceptualize exactly how to address culture when it comes to clinical practice. Here is a quick disclaimer. Any reference to religious and or ethnic content in reference to clinical practice are the sole subjective perceptions of myself and reflect prior professional experience and/or are used for discussion matters only. I really want to use this as a discussion tool as opposed to me just giving you some new content. Second, any image-based content related to religion and/or ethnic backgrounds is derived from online sources and are not objective in any form. Images are to be used as reference tools to give you a little bit of a visual. Lastly, the entire presentation is around improving the understanding of cultural considerations during professional practice. It is to foster thought.
How is Culture Defined?
According to the Merriam-Webster's Dictionary,
- The customary beliefs, social forms, and material traits of a racial, religious, or social group; also, the characteristic feature of everyday existence shared by people in a place or time
- The set of values, conventions, or social practices associated with a particular field, activity, or societal characteristic
What does that mean to me? I presently live in Queens, one of the five boroughs of New York City. Every borough of New York City has its own culture. Even though we share the similar trait of being New Yorkers, we may express our cultural values much differently despite living within two or three miles of each other. That is an example of what culture can be as opposed a more objective feature such as with race or color.
Culture Within OT/AOTA
I have a series of definitions and examples, so let's see if we can figure this out together.
- Is dynamic and complex and is influenced by outside forces such as technology and globalization.
- Influences one’s identity, but identity is multilayered and is derived from multiple sources.
- A client’s identity is a product of intersections of race/ethnicity, education, socioeconomic class, sex, age, sexual orientation, disability, religion etc.
-American Occupational Therapy Association (https://www.aota.org/Practice/Manage/Multicultural/Cultural-Competency-Tool-Kit.aspx)
All of these definitions of culture are derived from the AOTA. The single most important question that I continue to see within research and from the AOTA is, "How do we use our knowledge, skills, and attitudes to provide culturally responsive and culturally effective care?" That is likely one of the hardest questions to answer. We understand what culture is to some degree, but how do we make that a component of our clinical care?
Culture and the OTPF
According to the Occupational Therapy Framework (OTPF):
- The cultural context includes customs, beliefs, activity, patterns, behavioral standards, and expectations accepted by the society of which a client is a member.
- Influences the client’s identity and activity choices, and practitioners must be aware, for example of norms related to eating or deference to medical professionals when working with someone from another culture.
For example, I was working with an adult client who unfortunately had a CVA. His biggest concern was to regain his fine motor skills in order to use chopsticks as that was a part of his culture. Within my clinical practice in the VA, we focus on utensil use whether it be adaptive utensils, standard utensils, lightweight utensils, and so forth. Chopsticks are definitely more complicated to use and require a greater deal of dexterity and fine motor skills than standard utensils. The use of chopsticks became the center of my intervention as 1) it is client-centered, and 2) it is still using fine motor skills, dexterity, and in-hand manipulation. That is an example of the context and an aspect of culture within a practice setting.
To sum up what the AOTA and the OTPF state, there are a series of inter-correlating factors that influence culture when it comes to clinical practice. We have the context of being a major player. We have ethics, performance patterns, and client factors (Figure 1).
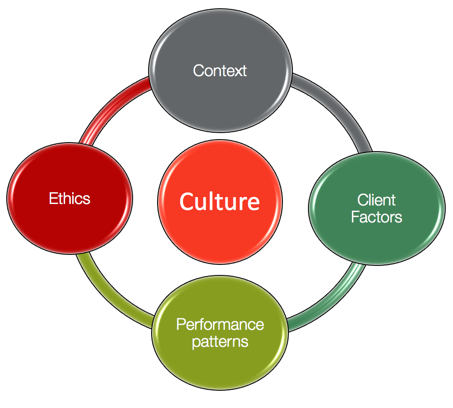
Figure 1. Inter-correlating factors influencing culture.
AOTA- Cultural Competency Tool Kits
AOTA has cultural competency toolkits available. I tell my students that it is not enough to just assess the range of motion, strength, or sensation. They also need to assess a patient's culture as it is going to be a huge factor in determining what type of intervention they are going to implement and what outcomes they are going to see. The toolkits are nice resources to use to incorporate culture into a day to day practice. Cultural competence includes responsiveness, humility, intelligence, and safety, and we will speak about these a little bit later in the presentation.
How do you measure, evaluate, assess, and gauge the impact of a client's culture during an evaluation?"Again, it is not something that we can objectively measure as it is something that is expressed in multiple ways. As another example, when working with someone of the Jewish Orthodox faith, there are certain boundaries or barriers, that have to be addressed during an initial evaluation. This will impact the type of performance patterns or outcomes that you might gain from treating this client. Some of these barriers are gender interactions and touch.
My opinion is that an interview is the best way to gauge the impact of culture on any client and practice setting. The interview is 95% of the time informal and helps to design an intervention plan. One strategy to assess culture is to speak about it openly to educate the clients on why it is an important aspect of the evaluation process. Within this presentation, there are going to be two case studies, and these case studies are based on real experiences.
Case Study #1
An OTS needs to evaluate your new client, a 36-year old Muslim woman diagnosed with multiple sclerosis. The OTS decides to use a culturally sensitive interview assessment to get her narrative. However, her brother, with whom she resides, answers all your questions with his interpretation. Although she is capable of responding, the client does not attempt to. How can the OTS provide client-centered or culturally effective care when they are not able to obtain her personal story?
- Matters of ethics?
- How can the OT make this a learning experience?
- Should the OT intervene?
- Should the OTS redirect back to the client?
- What professional skills can you reinforce to your student?
This situation is a template based upon multiple experiences I have had working in certain parts of New York City and with an array of Level II students. Where do ethics come in? Ethics is something we have heard about since school. Looking at ethics, specifically autonomy, how do we remain ethical but still deliver the best care?
The second question is how can you as a fieldwork supervisor, make this a learning experience? Every single experience within either Level I or Level II is going to be somewhat of a learning experience as I am sure everything is to some degree as most things are novel for the students. However, how can you provide your students with some type of template to base their reactions?
Should OT intervene? I have always thought this was a challenge based upon the number of weeks the students have completed. I usually step back and give them an opportunity to figure things out and understand the impact of their actions and their clients' reactions.
Should the OTS redirect back to the client? This is a really popular choice for some reason. Many of my students direct all of their attention to the client and not to anyone else, even if family members or a health proxy are available. Does that still adhere to cultural sensitivity for example?
The last aspect that I want you to consider is what professional skills can you reinforce to your students? We teach our Level I's and Level II students, not just clinical skills, but we also teach ethics and professional conduct. Professional skills may include customer service, active listening, and cultural sensitivity. There may be an abundance of professional skills that you might be able to reinforce from this particular situation. Take a look at the case study and kind of react to these questions and figure out what you would do as to make it a positive experience while still adhering to the aspect of culture within clinical care.
Cultural Competence
An Interpersonal Skill
I call cultural competence an interpersonal skill for many reasons. Culture is not something that is protocol based. Culture and cultural sensitivity cannot be easily learned or memorized, nor is it applicable to a multitude of situations. It is very individualized. How someone would react to a Muslim woman with MS would not be the same as another situation within similar parameters. Culture competence requires a different reaction every single time. Acquiring cultural competence reduces the chance of stereotyping, starts with awareness, grows with knowledge, is enhanced with specific skills, and is polished through cross-cultural encounters (Murden, Norman, Ross, Sturdivant, Kedia & Shah, 2008). Polished means that it is refined, and it is a foundational skill that most health care workers do have to some degree. However, it is enhanced or polished through our experience. It is our role to some degree to speed up the process, in my opinion, for our students. We can help them to facilitate their interpersonal skills by fostering such encounters. As a fieldwork educator, I purposely would choose clients with a strong cultural background. I would have my students perform particular parts of an evaluation, such as the Canadian Occupational Performance Measurement, or COPM. I also like my students to interact verbally, through socially and through body language to understand how a particular patient's culture comes into play. Facilitating such encounters will make a big impact on the overall experience during fieldwork.
Improved Outcomes
Another reason why cultural considerations or cultural sensitivity is important is that it improves outcomes. OTs and other health care professionals strive towards client-centered practice, and they need to be aware of how cultural competency affects their practice. Practitioners, both OTRs and OTAs, must educate themselves in aspects of cultural competence in order to design the most appropriate therapeutic interventions and to achieve better patient outcomes. One study with Eliminowski, 2015, found that educational workshops that build cultural competence skills and improve communication between patients lead to better patient health outcomes. Educational workshops may not be the most practical solution. I believe communication between colleagues and collaboration with other individuals, different from your own cultural background, is really the best way to really start honing in on your cultural awareness. I think that is the first step to really understand how approaches might differ just based on the individual's culture or background. For me, there are an array of hospitals that have a number of healthcare professionals from different backgrounds in the NYC area. I might work with a nurse from the Philippines, a speech-language pathologist from Russia, or a doctor from Africa as examples. I can observe how they interact with their clients verbally, socially, and professionally. This type of interaction has built my awareness and understanding of different cultures during service delivery.
Influence of Context
Occupational therapy is a person-centered profession whose primary focus is occupation and its array of meanings. An individual in the occupation they engage are the primary products of a sociocultural environment. Whiteford and St. Clair (2002) stated that ignoring these environmental influences and their meanings are probably to miss the point of intervention. The impact of one's society, socioeconomic status, primary and secondary context, and family are huge factors when delivering health care services. As occupational therapists, we need to know such information in order to design an actual, legitimate, and meaningful treatment plan.
Culture and the Student
I found these three studies extremely important and relevant to this webinar.
- “The findings suggest that there is not enough exposure to cultural issues in both university-based education and in fieldwork”- Murden et al., (2008)
- “Some students felt that certain aspects of culture such as language, race, and religion positively influenced their ability to relate to their clients” - Sonn & Vermeulen (2018)
- “Students need to consider their own sociocultural identity as a prerequisite to beginning to understand that of others”- Fitzgerald and Mullarvey-O’Byrne (1996)
The first one summarizes that it really does start within the curriculum. Students are in their novel stage. They are blank slates that we can really mold into amazing professionals. A lot of their foundation comes from undergrad and grad school. The topic of culture is becoming more and more an essential part of OT academia.
The second study sheds a positive light on understanding how language, race, and religion positively correlates with client care. It is important to understand that your students' culture may help them relate to clients during Level I and Level II fieldwork. It is an aspect of the therapeutic use of self, and it can build confidence and self-esteem. It also definitely builds communication skills.
The last study highlights that sociocultural identity is a prerequisite for understanding other aspects of culture. Being more aware of your own culture, cultural biases, and your ways of thinking is a great place to start when learning about others' cultures. Again, you have to know yourself before you can get to know someone else. This is something that happens innately, but it definitely can be refined during fieldwork practice.
Fieldwork Students' Cultural Identity
How do you account for your fieldwork student's cultural identity within their clinical affiliation? This is looking at their own cultural identity, not that of the client. There are certain questions to consider before proceeding.
Questions to Consider
- What is the cultural identity of your student?
- How do you facilitate their development of the therapeutic use of self?
- How do you account for the influence of the context?
- How do you account for the attitudinal and societal perceptions of your clients?
What is the cultural identity of your student? Can you answer that question or does your student answer that question? It is something that you should discuss within the first few days of fieldwork. A short discussion about their own identity would be a great way to find out more information about them as students, but also, it is a way to see how they perceive their culture as a part of professional care.
Second, how do you facilitate the development of the therapeutic use of self? I teach this term within academia. The concept of therapeutic use of self-means several things and culture is definitely a strong part of the therapeutic use of self. It drives the way we individualize treatment and focus on improving outcomes. It signifies who we are and how we practice OT. How do you facilitate that within your students? How do you facilitate experiences? How do you gauge their reactions? How do you build confidence or therapeutic use of self? These are a few things that you want to consider before engaging them in full-blown fieldwork.
