Editor's note: This text-based course is a transcript of the webinar, Fostering Meaning And Purpose For Individuals In Senior Living, presented by Kathleen Weissberg, OTD, OTR/L.
Learning Outcomes
- After this course, participants will be able to identify how meaningful and purposeful activity can help occupational therapy practitioners address the needs of individuals in senior living.
- After this course, participants will be able to identify how to develop a workplace culture to support person-centered care to improve QOL and satisfaction.
- After this course, participants will be able to list novel approaches to meet facilitate person-centered engagement.
Introduction
Thank you, everyone, for tuning in today. This is an important topic that is near and dear to my heart. As I age and think about what we are doing in long-term care these days, I want it to be a little bit different for senior living, assisted living, independent living, and home health types of settings, like adult day health.
One of the things that we are going to talk about is how to engage our nurses in our frame of reference. As occupational therapy practitioners (OTPs), activity is important and a means to an end. It is also a way to increase coordination, strength, or whatever. Our users thrive on this, and we must carry this over.
Stephen Covey Quote
- “There are certain things that are fundamental to human fulfillment. The essence of these needs is captured in the phrase ‘to live, to love, to learn, to leave a legacy.’ The need to live is our physical need for such things as food, clothing, shelter, economic well-being, health. The need to love is our social need to relate to other people, to belong, to love, and to be loved. The need to learn is our mental need to develop and grow. And the need to leave a personal legacy is our spiritual need to have a sense of meaning, purpose, personal congruence, and contribution.”
-- Stephen Covey
I am going to start with this quote. It is an oldie but of goodie, and Steven Covey wrote the book, "The 7 Habits of Highly Effective People." The last sentence is the one that speaks to me because I still treat in a clinic. It helps me when I structure my activities and what I do. I always think of how an activity helps a person. Is it congruent with their values, thoughts, beliefs, and what they want to do? We will talk more about that as we go along.
Loneliness and Social Isolation
- Social isolation refers to the objective absence or paucity of contacts and interactions between a person and a social network.
- Loneliness refers to a subjective feeling state of being alone, separated, or apart from others, and has been conceptualized as an imbalance between desired social contacts and actual social contacts.
I thought we would start out just by talking about loneliness and social isolation, especially as it relates to the pandemic. We are on a trend outward, but I am still hearing of outbreaks and different things. I may be completely off base, but I think the pandemic helped us to understand the life experience of a senior.
Occupational therapy practitioners, along with our activity personnel, rec therapy, life enrichment, et cetera did a lot to combat this social isolation.
Oftentimes we use loneliness and social isolation interchangeably, but they are two different concepts. Social isolation is the objective absence, that paucity of not having contact or interactions between people. Loneliness is the subjective state of being alone, separated, etc. It is an imbalance between how many social contacts we have and what we would prefer.
- Social isolation is certainly not just an American phenomenon or a COVID issue.
- Before the pandemic began, studies indicated that nearly 25% of older Americans were socially isolated.
- 43% of those age 60 and older report feeling lonely
- Loneliness and social isolation impact health
- 26% increased risk of dementia
- Increase the risk of mortality by up to 29%
- Chronic conditions – CAD, CVA, HBP
Loneliness and social isolation are not an American phenomenon or a COVID issue. A study was done in 2017 looking at 11 high-income countries, similar to the United States. They reported that anywhere between 10 and 30% of adults aged 65 and older report feeling isolated from others. Obviously, this was before the pandemic began, and similar studies show the same results.
Another study found that 24% of individuals in the US, 65 years of age or older, were socially isolated. They did not have the social relationships that they wanted. Additionally, 35% of individuals, 45 years of age or older, and 43% of those 60 or older report feeling lonely. Again, these numbers are all pre-pandemic in 2017.
A meta-analysis in 2015 showed that loneliness and social isolation can impact health.
We are looking at meaning and purpose as a way of combating loneliness and social isolation. With these populations, there is a 26% increased risk of dementia and an increased risk of mortality up to 29%. They also have an increased risk of other chronic conditions, like high blood pressure, coronary heart disease, stroke, et cetera.
Impact of Socialization
- Isolation and loneliness from physical restrictions affect mental and physical well-being.
- Residents show symptoms of mental illness and depression following isolation and quarantine.
- Access to technology helps buffer that loneliness and isolation.
- Social networks that promote resilience help with stress and trauma.
This study came from a 2020 study at the beginning of the pandemic. It showed that physical restrictions affected physical well-being, mental health, mental illness, and depression. If we did not have depression prior to the pandemic, we surely do now.
On the flip side, we saw increased access to technology. Access to social networks and other types of activities was a buffer against social isolation. It helped individuals to develop resilience and deal with stress and trauma.
Importance of Activity
- Participation in activities has a direct correlation to well-being in older adults.
- Activity fills a void, maintains social roles, enables positive expression, reduces frustrations, and enhances the continuity of self-identity and feelings of connectedness.
Participation in activities has a direct correlation with the well-being of our seniors. They fill a void, maintain social roles, and are positive expressions. What I choose to do is how I express myself; it is who I am.
We also see reduced frustration, enhanced continuity of self-identity, and improved self-esteem. They have a sense of purpose that they accomplished something and feelings of connectedness.
All of these things together not only enhance function by improving motor and cognitive skills, but they also help us to reduce depressive symptoms that we often see.
Why Foster Purpose?
- Protects against ill health
- Prevents decline in occupational performance
- Fewer disturbing behaviors and less help with self-care
- Boosts mood
- Reduces depression
There is a lot of research in this area, dating all the way back to the early 1990s. It suggests that maintaining purpose in life and setting goals can protect against ill health and prevent the progression of Alzheimer's disease or related dementias. It can also protect against early mortality. It is two-fold with both having a purpose in life and setting goals to develop resiliency. They have a purpose for living if you will.
Aging is natural. Our elderly are repositories of culture, tradition, knowledge, and skills. They bring so much to the table. Individuals coming into senior living have residual skills, but they are not always fostered. Typically, people come in very able and well-bodied, but over a certain amount of time, even those without a diagnosis of dementia, Parkinson's, etc., have a decline in occupational performance. As an example, we may see a decline in continence for no reason other than the fact that we did not engage with them.
Individuals who are occupationally active show fewer disturbing behaviors. particularly with dementia. They need less help with their self-care and basic ADLs, like feeding, grooming, etc. We also see better mood and self-expression with reduced depression.
At a Crossroad
- As we age, do we continue our roles? Or find new roles?
- Seniors prefer active engagement.
- Purposeful occupation remains important across all phases of the life span.
Think about who you are and what your roles are. You may be a student, employee, caregiver, mother, father, sister, brother, neighbor, or whatever your roles are and how often those dictate what your purpose is in life. I hear often, "I am an empty nester now. I do not know what to do with myself." Or, "I have retired, and I do not know what to do with all of my time. Your roles dictate what we do and who we are. However, as we get older, as I am alluding to here, our roles change so much.
Many of our seniors are at a crossroads. Do they continue with their same roles? Some of them may, but others may not. Do they find new roles in their communities? Without some level of guidance or help, they may find their roles slipping away and not have anything to fill that void.
Research shows that our seniors do in fact prefer active engagement and some form of purposeful occupation across all phases of the lifespan. We will talk about the different areas where that may happen.
Consider This...
- What activities do you enjoy?
- What are your roles, values, interests, and occupations?
- How does this compare to what you offer at your facility?
- Are your activities organic or are they contrived?
Think about who you are and what you enjoy. I love to bake. We are around the holiday season right now, so I am getting ready for that. I also like to play tennis. Think about your roles, values, and interests. Now, if you are working in senior living, how does that compare? How do your preferred activities line up with what is offered in a senior community? Are activities organic or are they contrived? Are activities being developed because seniors want them or are we doing things to meet therapy goals? If you go into the activities department, are they playing bingo or painting sun catchers?
I have a national role with Select and cover 40-plus states. I love to go around the country and see some of the creative and different things that people are doing. There is one community that I can think of in the Pacific Northwest where they are brewing beer and serving that at sport watching events. That is a very organic activity.
Fostering Engagement
- Set up daily activities that:
- Stimulate the mind and body
- Are culturally and socially relevant
- Match interests
- Are age-appropriate
When looking at activities, we want to make sure they foster engagement. Our clients in senior living are isolated. They are often in their room for long periods of time and may not have family coming to visit. When they come for OT services, are we stimulating their mind and body with culturally, socially relevant, and age-appropriate activities? Do they match their interests and what they want to do?
I will ask, "Hey, what do you want to work on today? What's your goal, and how do you want to accomplish that?"
- Connect individuals to their environment
- Make it more than just a place to sleep and eat
- Include residents in decisions and events within the environment
- Creating and modeling purpose
I like the idea of connecting our seniors to their environment. It is more than a place to go to get their meals, sleep, and shower. Are there ways that we can include our clients? This is not just during the occupational therapy process. For example, is there a way that this person can be part of a "welcome wagon," for new individuals?
I have done some creative things in both assisted and independent living communities. We had a car safety day, and one of the residents was a mechanic. We involved him in the planning, and it gave him a sense of purpose. Someone may have worked in healthcare and could help with policies and procedures or marketing.
We can model purpose by having residents reach out to other residents.
- Involvement in the local community
- Tutoring, teaching, intergenerational mentoring
- Promotes feelings of self-worth
I do not have a slide specifically on intergenerational types of things, but this is a huge opportunity to work with the local community. For example, seniors can teach younger children how to cook, teach them how to read, or how to sew buttons on a shirt. There is also a great opportunity for our kids to teach our seniors things, like social networking online, how to set up a Zoom call, or how to access Facebook. We can match individuals with common interests and get them involved. It promotes a feeling of self-worth.
- Help individuals to lead
- Leadership opportunities in the facility
- Resident committees
- Fosters a sense of purpose
I also love the idea of helping individuals to lead and incorporating this into our OT plans of care. A committee may be a great place to start related to interior design, groundskeeping, or dining. These tasks require higher level cognitive skills and give them the opportunity to feel purposeful as they are serving a greater cause.
What Makes a Successful Activity?
- Client-centered and individualized
- Based on preferences
- Meaningful versus rote
- Graded to abilities
- Volume and content
- Staff attitude
- Nursing support
What makes an activity successful? It is an activity that is based on preferences that are meaningful, not rote, and graded to their abilities. We all know how to grade activities as occupational therapy practitioners.
Volume and Diversity
- Social and productive activities are just as effective as fitness.
- Intensity, frequency, and duration are not as important to our clients as volume and diversity.
Research shows that the intensity, frequency, or duration of the activity is not as important as the volume and diversity. Our bodies do not care if the whole activity is done or just a part, like baking a cake versus only measuring the flour. The body does not care if we do an activity as a sport, an exercise, a leisure activity, or as a household chore, like sweeping the floor.
Social and productive activities are just as effective in reducing the risk of death as our fitness activities. I think this is what sets us apart as occupational therapy practitioners apart. We look at productive activities.
Alongside this is a sense of control. This is a real sticking point for me. I do not think I have ever in my over 30 years of practice completed any sort of rote exercise with an individual. For example, I do not think I have ever done a TheraBand program or used an arm bike.
I assess what I want to accomplish or what muscles I want to activate, and then devise an activity that could help me to accomplish that. This is what we are talking about. I almost liken it to a cruise ship. You get a daily calendar of all the activities that are going on. You are not going to go to all of them, but you love knowing that they are out there. You want them to have a choice as I think that is so important.
Client-Centered and Individualized
- Continue to support the 5 domains of life: recreation, social, community activities, civic activities, and personal development
- Offer meaningful activities that reflect preferences
- Offer choice and control over activities
We want to continue to support the five domains of life at a bare minimum, including recreation, social, community things, civic, and personal development. I love the idea of personal development because it incorporates the occupational role.
To individualize this and how we keep it going is to use meaningful activities that reflect preferences and interests. Often, when entering senior living, there is a narrowing of choices. Whether it is OT, activities, or whomever, we do not always have information about their preferences. A recent study showed that inadequate choice and lack of control over daily activities were consistently noted as strong concerns of nursing home residents.
Practical Ideas
- Caring opportunities (e.g., a pet)
- Lifelong learning
- Encourage participation
- Foster a sense of community – everyone has a role in the activity
The sky is the limit here. Can someone help with a facility pet or at a bare minimum fill the bird feeder?
There could be lifelong learning classes hosted and taught by our staff. I worked with a community years ago where every single person on the staff was queried about what they like to do to see what skills they could teach others. Then, on a weekly or monthly basis, one person led an activity. There also may be opportunities to partner with local community colleges, parks and rec departments, or something like that.
Can our seniors teach? My father-in-law was living in an assisted living and taught art classes. He wanted to learn how to bee keep and another resident taught him how to do that. There are many interesting stories and examples.
We want to foster that sense of community where we are helping each other. Many of you are probably doing groups in our communities, and that is also a great opportunity where one person can plan, somebody else organizes, somebody gets the supplies, somebody sets it up, somebody helps clean up, and everybody has a role.
- One size does not fit all -- the purpose is individualized
We all know that one size does not fit all. This is the crux of person-centered care.
Assessment of History/Background
- What do they like to do?
- What is their history?
- Strengths and limitations?
- Environment -- what contributes to successful engagement and what hinders it?
- Relevant life experiences, values, interests
We should be using the Occupational Profile with every assessment. This includes what a person likes to do, their history, their strengths, and their limitations. We also want to know about their environment and contextual factors there that either contribute to or hinder their engagement.
We start there, but oftentimes, they may only come up with a small list like going to church, gardening and reading the newspaper. The conversation stagnates and you do not get a robust list. We may need more.
Soliciting Preferences
- A systematic narrative history of activities enjoyed prior to admission
- Directly interview residents about activity preferences and available choices
- Identify health-related or contextual obstacles
- Develop novel interventions to re-engage residents
In another study, they asked some questions about what they enjoyed in the past couple of months before coming to the facility. Then, what they enjoyed in the previous five to 10 years. They also asked about health-related obstacles like fear of falling or hearing, shortness of breath, or those sorts of things.
Consider the Following Activity Groups
- Games
- Reading
- Arts and crafts
- Gardening
- Culinary arts
- Religious activities
- Cultural activities
- New technology
- Communications
- Shopping
- Music
- Pets
- Exercise
- Television/movies
- Sports
- Travel/excursions
- Driving
- Socializing
- Dancing
- Photography
- Volunteering
- Classes
“If your health was not an issue, is there anything special that you would want to do in the next 6 months?”
We can also work with them to develop novel interventions. Above are some examples of activity groups. For example, you may have somebody who really loves to travel, but cannot travel now. Perhaps we can set up a virtual experience with a travel log. We can develop that into some sort of cognitive type of activity. We can try novel approaches to things that they used to enjoy.
You can also ask them if their health was not an issue, what they would want to do. People are getting involved in photography, cooking, gardening, and different things in their community, so the sky is the limit. We have a role in not just identifying what they enjoy, but also being creative to make it happen.
Assessments
Here are a few standardized assessments that we as OTs probably already know. We can use these to solicit preferences.
Modified Interest Checklist
- Gathers information on a client's strength of interest and engagement in 68 activities in the past, currently, and in the future
- Focus on leisure interests
The first one is the Modified Interest Checklist in Figure 1.
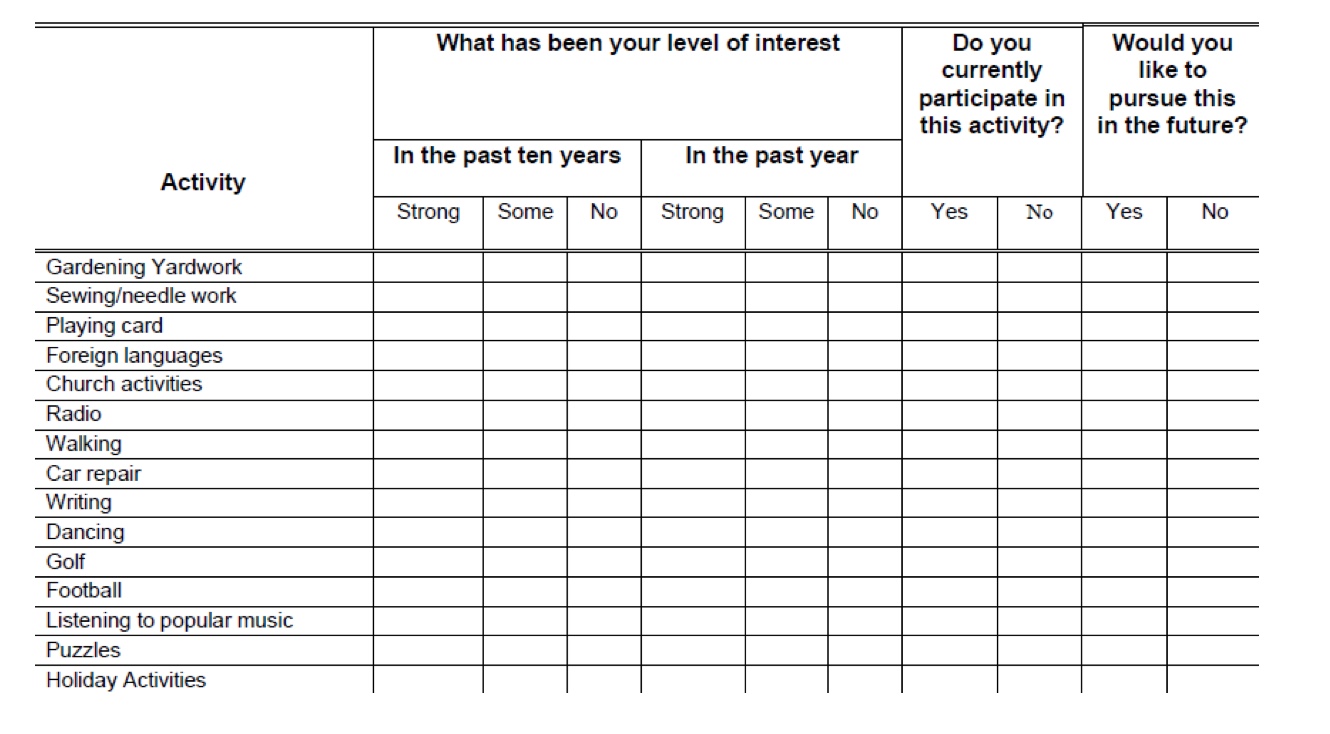
Figure 1. Modified Interest Checklist: Free download (https://moho-irm.uic.edu/products.aspx?type=free)
This has been around forever. It is a free download and thank you to OccupationalTherapy.com for putting the link up there to download that. It is 68 different activities and includes questions about each activity. Did you do these in the past, are you doing these currently, and would you like to do this in the future?
I used this many years ago with a group of individuals. I found a whole host of folks who loved football. As the OT, I helped them to pull together a football club. I am originally from Pittsburgh and I am a huge Steelers fan. This group organized Steelers' parties every Sunday. Sometimes you do not know until you ask the question about what a person wants to do.
Role Checklist
- Obtain information on client's perceptions of their participation in 10 occupational roles throughout their life
- Assesses value placed on occupational roles
- Looks at roles like a student, worker, volunteer, caregiver, home maintainer, friend, family member, religious participant
- Assesses participation in different roles in past, present, and future
- Role Checklist: Not free (https://uic.flintbox.com/technologies/b28ebf11-e747-45da-a6ee-a40da7f4b9c1)
Similarly, there is the Role Checklist with 10 occupational roles. I am sure a lot of you have seen this as well. It asks things like, did you do that in the past, are you doing it now, or do you want to do that in the future? It taps into what the person wants to accomplish or work on.
Canadian Occupational Performance Measure (COPM)
- Identifies issues of personal importance to the client
- Detects changes in performance over time
- Outcome measure as well as the basis for intervention
- COPM: Not Free (https://www.thecopm.ca/buy/english-copm-pdf-usa/)
The COPM, the Canadian Occupational Performance Measure, is another popular one but it is also not free. I have used it often in the past, and I love it. It identifies the issues that are of greatest importance to the client. This is so critical as it is the person's plan of care. It is what they think they need to do, combined with my input. We work collaboratively to work toward that person's goals.
We can also use it to detect changes in performance over time. This is a great opportunity for us to initiate those conversations about performance issues, provide the basis for our goals, and develop that person-centered care.
Preferences for Everyday Living (PELI)
- Is the activity important?
- What are your preferences?
- Combination Likert Scale and open-ended questions about routines, habits, and preferences
The PELI, or the Preferences for Everyday Living (seen in Figure 2) is free.

Figure 2. The PELI- Free Download.
If you work in long-term care, the minimum dataset (MDS) in the section on activity preferences is developed from the PELI. There is also a short version of the PELI. It consists of open-ended questions, Likert scales, and checkoff types of things. For the person who stagnates on what they like to do, this may be helpful. It can tap into some of the things that they do not always think of right off the bat like an Elks Lodge or a book club. You can also get some additional input regarding their activity preferences and how important certain activities are to them.
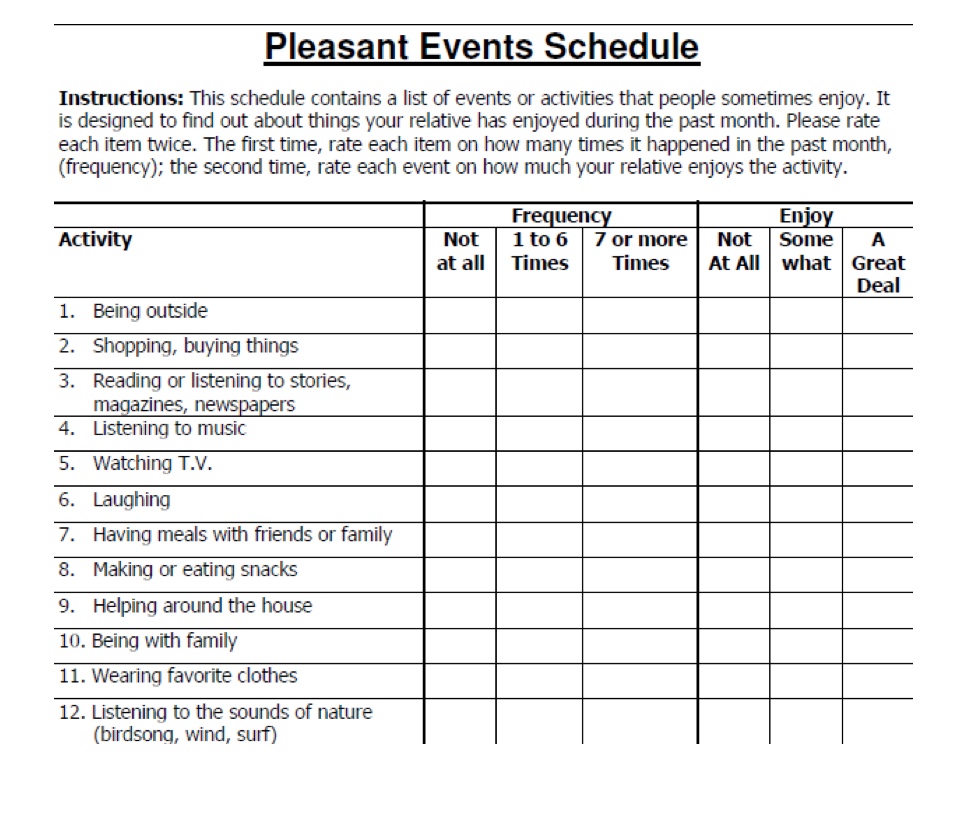
Pleasant Events Schedule
- Designed to find out about the things you have enjoyed during the past month
- Contains a list of events or activities which people sometimes enjoy
- A person goes through it twice
- First time rating each event or how many times it has happened in the past month
- Second time rating each event on how pleasant it has been
The final tool is the pleasant event schedule as seen in Figure 3.
 .
.
Figure 3. Pleasant Events Schedule (Free Download)
This is ideally used for individuals with dementia, but I have used it with others as well. It goes through this one twice. The first time the individual rates how often they did this within the past month, and then how much they enjoyed it. We all have those activities that we have to do and then the ones that we enjoy doing. This tool taps into how much a person likes doing an activity.
Before we move on, I just want to make a comment that when I look at some of these standardized assessments that are out there, I do not believe that this is a one-and-done thing. Activity preferences can change over time. I will use my father-in-law as an example. He was an artist and loved sports. He was an artist by background, and that is what he did for a living. However, at some point, he was done because it made him feel like he was going to work every day. He wanted to do something different, and this is where we can tap into lifelong learning and facilitate that. Thus, we need to go back sometimes and revisit the activities to see if they are applicable.
Activities
The Basics
- Use Everyday Materials
- Match Interests & Skills (group/individual)
- Use Past Experiences & Preferences
- Adapt According to Cognitive & Physical Status
- Simplify as Much as Necessary
Full disclosure, I took some of these slides I took from some of my dementia workshops, but I feel like they are also very appropriate for a community at large. Often, I hear that people do not have a budget, supplies, et cetera. I think some of the best activities can be done using everyday materials, like loading and unloading the dishwasher or snapping beans, one of my favorite activities, or sweeping the floor. These are also beneficial as they are familiar. T
We talked about matching interests and skills and using those past experiences and preferences. Again, do not always rely on that because those can change over time, particularly in a community where they are seeing other activities. "Ooh, I want to learn that."
If we know what the person's cognitive and physical status is, we can adapt, grade, and simplify an activity. This is what I love about our job. One example is a coupon activity. We can have them organize coupons, or I can make it a little bit harder and ask the person to walk out with me to get the Sunday paper. They can clip and organize them while standing. A higher level activity is going shopping and using the coupons. We can make it as challenging or as simple as we need to.
Meaningful Activities
- Based on reality orientation, environmental modification, sensory stimulation, reminiscence, cognitive interventions, caregiver education
- Social context and regular social contact
- Materials-based activity elicits more engagement than a rote exercise
I want to go back to meaningful activities. Social context is so important. If we look back to research from 30 years ago, they found that exercise programs were not the most important thing for quality of life. Instead, having the social context of a group was an important component. Another older study showed that subjects smiled and laughed more during an activity-based program versus doing exercise.
- Every activity must . . .
- Have a purpose that is obvious to the participant
- Be voluntary
- Be pleasurable
- Be socially and age-appropriate
- Be failure proof
Every activity should have a purpose, and be voluntary, pleasurable, and socially age-appropriate. It does not have to be failure-proof unless you are working with an individual who has Alzheimer's or related dementia. We want individuals to be successful to boost their self-esteem, and we do not want to frustrate or upset them. We want them to come to OT so we want them to be successful and happy. Most of us struggle with setting up activities with someone who has a middle-stage or end-stage dementia. We will talk more about this.
Considerations When Adapting Activities
I love this grid in Figure 4.
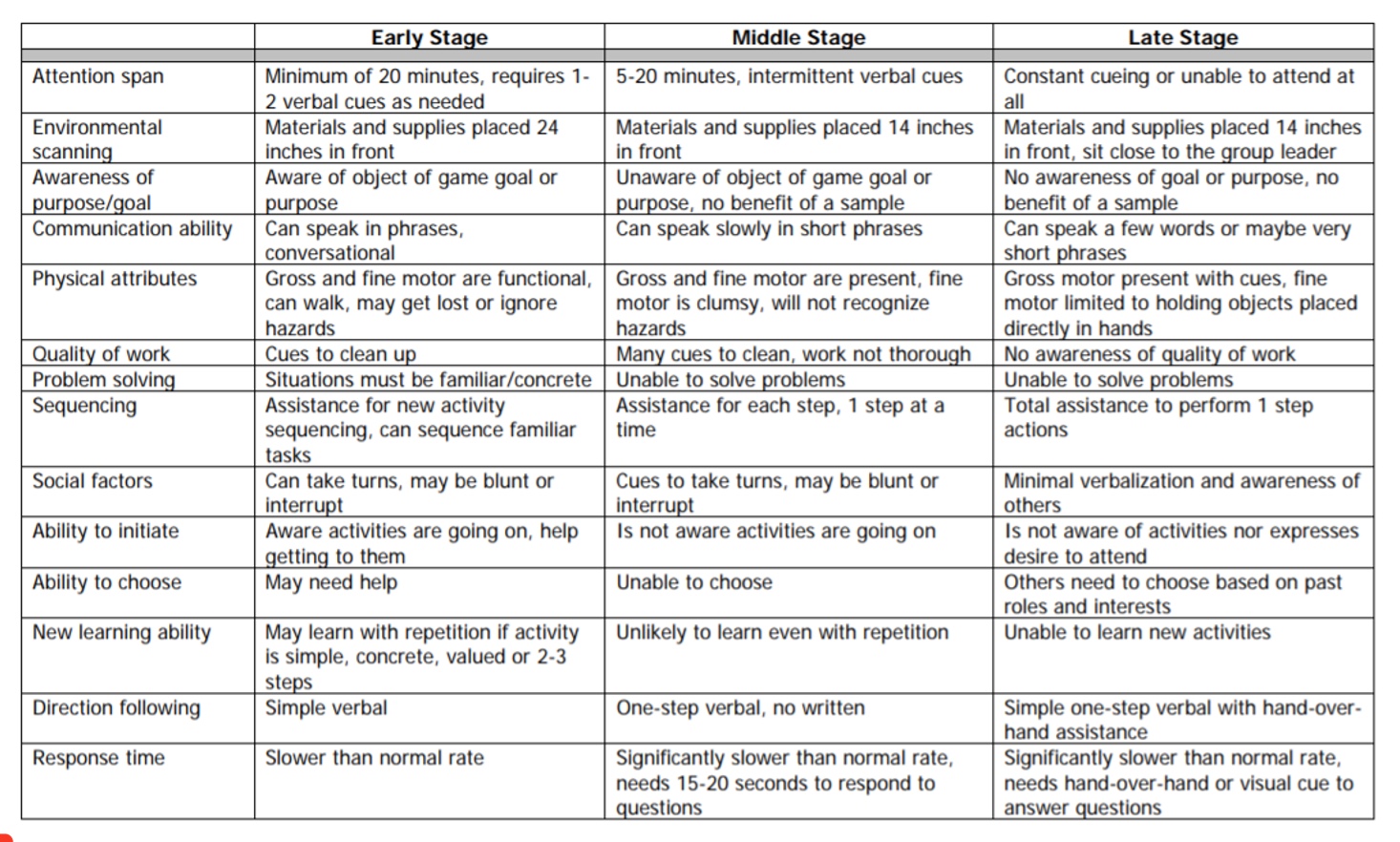
Figure 4. Dementia grid. Click here to enlarge the image.
I am not going to go over all of this, but it supports some of the important things we do when adapting activities, particularly for dementia. I am going to go through a couple of attributes here.
The first is attention span. In early-stage dementia, they may have about 20 minutes, but when they get to the middle stage of dementia, this is reduced to five to 20 minutes. Finally, in the late stage, they need constant queuing to attend. You have to think about this as you are setting something up.
Environmental scanning requires that we look at the placement of an activity. Somebody who has dementia, as they progress, start to lose some of their peripheral vision, and typically have a downward restricted gaze. Early on I can put something two feet in front of somebody, and they can see it. Or, if I am running a large group in OT, they can be further away from me. However, when they get to the middle stage, their scanning is about 14 inches. At the later stage, I am looking at significantly shorter vision like six to seven inches.
Direction following in later stages requires very simple directions with hand-over-hand guidance. We can also utilize these guidelines for individuals with traumatic brain injury or CVA.
Response time is one that resonates with me. The middle stage is about 15 to 20 seconds, and in the late stage, it is significantly slower like 60 seconds to upwards of three minutes. You can give a directive and wait for a long time for a response. Often, we say that a person does not follow directions, is belligerent, difficult, or whatever, when that is not the case at all. They just need the time to process, but it is a struggle for us to wait for that. Try waiting a full 60 seconds for someone to respond. It is very challenging to continue to have eye contact and all of those non-verbal cues to keep the dialogue going until that response happens. This is important to think about because some of the dementia activities are a bigger challenge.
Task Grading Considerations
- Performing the task or activity is the end goal
- Number of steps in the task
- Amount of time to be given to each step
- Must be appropriate to the client's abilities
- Utilize occupational history as a resource
The end goal with task grading is reducing or increasing the number of steps, the amount of time, or whatever. It has to be appropriate. We can go back to that occupational profile as a resource. What I mean by that is, we can use it to assess their level of anxiety or their expectation of performance. We want to set up an activity to match or mirror who that person is.
Task Adaptation
- Something that makes doing an activity easier
- Adapt the design or restructure the environment, tools, or task
- Instruction and education
- Will not change the end goal of the activity, but does provide a means to task accomplishment
Again, task adaptation can make it easier, harder, or whatever. What I think is important here is that it does not change the end goal, but instead, it provides a means to task accomplishment. As I work so much in dementia, this is vital. An accomplishment gives that person meaning, purpose, and esteem. Nothing is more frustrating than setting up an activity and not finishing it. We want to support them so that they can finish tasks.
Creating Activities
These next three slides actually come out of a Montessori type of training.
- Step 1
- Question why the person living with dementia is behaving in certain ways or demonstrating behaviors
Step one is asking what a person wants to do, likes to do, or needs to do. We are trying to ascertain why someone behaves a certain way. Do they need to do something?
- Step 2: CREATE
- C: Consider needs, interests, skills, abilities
- R: Remove clutter
- E: Error-free
- A: All materials are modifiable
- T: Templates to support declarative memory
- E: Evaluate the activity
When creating an activity, we talked about considering their needs, interests, skills, and abilities. If they have had a traumatic brain injury or residual effects from a CVA, we may want to remove clutter or distractions from the environment. We also want to set up the environment to ensure that the materials can be seen and are recognizable. We talked about error-free learning. We can modify tasks if someone has a cognitive impairment. We can use templates or structure activities to tap into the declarative and procedural memory that they have retained. Lastly, we want to evaluate the task to see if it met their needs.
- Step 3: PRESENT
- P: Prepare the environment
- R: Room set up
- E: Extend an invitation
- S: Show the activity
- E: Error-free
- N: Needs, interests, skills, abilities (modification)
- T: Thank you
How do we present the activity to the person? It is all about setting up the room and preparing the environment. We need to extend an invitation and not just say, "We are doing this." We should say things like, "Would you like to help me do X, Y, Z?" Or, "I thought maybe we would do this today. Would you like to help me?" We want to make them a part of the activity. We then show and demonstrate the activity, modifying it if needed. Lastly, something that I have taken away from Montessori, is thanking the person. "Thanks for coming down today. How do you think you did? How do you think we are doing on our goals?" It is important to have that dialogue to collaborate with them on their plan of care. It is important to remember to extend the invitation and thank them after because I see this almost like a customer service thing. We want this person to engage and participate.
Activity Kits
- Five domains of function
- Cognitive stimulation
- Life skills
- Motor movement and fitness
- Sensory stimulation
- Socialization
This is where these kits come into play. It is also a nice leave-behind to share with other disciplines, a person's family members, or volunteers. There are five domains of function.
For cognitive stimulation, you may have puzzles, word searches, or a newspaper every day. The sky is the limit with life skills like polishing shoes or silverware, washing windows, deadheading plants, or something like that. Motor movement and fitness do not have to be only exercise. This could be a beanbag toss, sweeping, vacuuming, raking leaves, or whatever. For sensory stimulation, there are many things in nature. One of my favorite things to do is have them slice an orange, ream it, and make orange juice. This activity works on fine motor control and sensory stimulation. We could have them set up a small table for a social gathering. They can also use fill-in-the-blank expressions, jokes, holidays, humor, and all sorts of things during groups.
Tailored Activity Programs/Kits
- Tailored Activity Programs reduce behaviors and increase engagement.
- Activity kits improve the quality of visits and QOL.
- Individualized and meaningful activities show positive results.
The wonderful thing about these kits, from a dementia perspective, is they reduce behaviors and increase engagement. From an individual perspective, they have something to do when not in therapy, and it can be carried over to interact with others as stated earlier. Often, they do not know how to have a good meaningful visit with their family member, but an activity kit may help. I found a YouTube clip a while ago that showed a person engaging with another individual over a bag of buttons. "Where would you sew this?" or "What would you have done with this?" And, "Did you sew when you were younger? And if so, what types of things did you like to sew?" It starts a conversation that can increase the quality of visits.
The evidence is out there showing positive results and a 57 to 67% improvement in well-being just by engaging in an activity.
Technology
- High tech, low tech
- High cost, low cost
- Virtual opportunities
I now want to talk a little bit about technology. I conducted a large focus group in the state of Minnesota during the pandemic asking about what people were doing for meaningful engagement. One thing that came up over and over was technology. From my own personal side, I learned so much from individuals because I used to think that technology was too expensive, or I could not do it. However, there are different levels: high tech, low tech, high cost, and low cost. If this is something that you have a passion for, I would encourage you to pursue this. There are also many grants available.
Virtual opportunities can be powerful as we can take them to a place where they have never been. If they love to travel, we can take them someplace online and have a dialogue about it. For example, we had an individual who had never skied but took up virtual skiing during the pandemic. It was such a joy to watch him. He had to use a lot of gross motor movement, which he needed, and he did it in a virtual way.
There are a lot of different things out there. One I am thinking of is where they can catch butterflies with a net, and another is identifying home hazards. Often we think because they are a senior, they do not use technology. Nothing could be further from the truth.
Older Adults & Technology Use
- Among older adults with an annual household income of $75,000 or more, 90% go online and 82% have high-speed internet at home.
- For older adults earning less than $30,000 annually, 39% go online and 25% have high-speed internet at home.
- Among older adults who have not attended college, 40% go online and 27% have broadband at home.
- 67% of adults over 65 access the news on a mobile device
- 4 in 10 adults over 65 own smartphones
- 34% of people over 65 use some form of social media
Here are some statistics. Ninety percent of individuals with a reasonably large household income are online. For individuals at $30,000 or less, 39% are going online. Many folks (4 out of 10) have a mobile device or smartphone and are engaged in social media. They are out there with Facebook, Instagram, and all of those sorts of things.
Benefits of Using Technology
- Making social connections
- Provides cognitive stimulation
- Encourages exercise
There are many benefits to technology. Using technology for social connections is at the top of the list. They can see their kids, grandchildren, other family, and friends who might live far away. Setting up technology is a cognitive and fine motor activity. They can use technology for e-mail, especially if they used to love to write letters or cards, or to play games. There are many fun programs like virtual hiking, exercising, and gardening. The sky is the limit.
Staff Attitude
- Attitudes of the staff have a significant impact on the success of an activities program.
- Participation in activities of interest reduces caregiver burden.
- Positive outcomes when staff were positive, had ability to grade tasks to meet varying group needs, and had activity resource kits.
Staff attitude has a big impact on success. "I do not have the time to set up that activity," or We do not have the supplies" are common refrains. It could be our attitude or the staff in our communities. Ultimately we want whatever we are setting up, we want the individual to be able to carry that over when we are done, and their reality is, again, the research is out there. There are a lot of positive outcomes when staff members are positive and have the skills. This might be a role for us where we teach how to grade the activities to the other staff. Again thinking about this from a Montessori perspective, you can set up an activity that engages a person and then they are not asking repetitively when is lunch over or doing other negative behaviors.
Trends in Nursing Care
- The amount of social interaction is limited.
- Emphasize a task-based work system despite acceptance of person-centered care
- Most nursing communication focuses on caregiving.
- Some patients are more “popular” or well-liked than others.
- Engagement is an issue of therapy/activities and not within the role of nursing.
There is a decrease in the amount of social interaction by nursing. There is an emphasis on a task-based work system, and they are focused on getting the stuff done, like passing medications and getting people up and dressed. Thus, they are not engaging in true social communication.
One of the things that came out of the focus group is that nursing said, "This is our job too. This is not just therapy or activities, we have to do some of this engagement as well." Nursing does not really learn this in school, it is not ingrained in their daily routines. One study I saw asked 24 nurses if activity engagement was part of their role, and only three people said that it was.
Nursing Engagement and Support
- Many residents are inactive/passive and the TV is a popular activity offering no socialization.
- When nurses incorporated meaningful activity and socialization into their day-to-day roles and professional values, a hope-fostering environment develops.
- Hope-fostering environment: where meaningful and empathic relationships involve active listening, and affirmation of the person’s dignity and self-worth despite functional limitations.
How can we develop that culture? I think to some degree we need to make it easy on them. We need to find ways that they can get involved that are easy, cost-effective, and not time-consuming. If patients are only sitting in front of the tv, they are not doing much.
Consider for a Moment
- How does your facility address the occupational needs of its residents?
- Do you have a formal philosophy of care?
- Do your schedules for resident care take precedence over other activities?
- What are your popular activities? Are they formal or informal?
- Think about your morning routine … what do you do?
Here are some questions to consider about your workplace. Are you addressing occupational needs? Do you have a formal philosophy of care? I think most of you would say, "Yes. We have person-centered care." However, when you really drill it down, are the therapy, dining room, or shower schedules more important? Are we offering things that our clients want to do?
Trends and Themes
- The philosophy of care was not always reflected in the way that activities were completed.
- Basic care needs were always addressed before occupations and activities.
- The nurse holds the key to how the residents’ schedules are structured and to the activities that were provided and attended.
- Nursing programs do not prepare the nurse to enact this type of program focused on occupations and activities.
While we strive to engage patients socially, the reality is that many remain reluctant to leave their rooms post-pandemic isolation. As occupational therapists, we must meet them where they are. Nurses are key partners, so collaborate with them to understand each patient's needs and motivations.
Appreciate that some desire solitude right now. This does not mean abandoning engagement. Provide personalized activity kits for in-room interests, from puzzles to crafts. Work with patients to develop kits tailored to their roles and preferences pre-pandemic. Virtual programming via CCTV or Internet is another option for solitary engagement.
Yet also gently encourage community, if desired, through preferred activities. Maybe cooking, exercise, or gardening will draw them out. Get creative - there are opportunities between complete isolation and large groups. Offer choices: a quiet shared movie night or 1:1 chats over coffee, for instance. Flexibility and compassion are essential as we coax patients back into rhythms of social living. Meeting them where they are now is the first step.
Perceived Barriers
- Staffing/Changes in staffing
- Budget – cost and funding
- Supplies
- Schedules
- Education and training
- Creative activity choices
- Empowering all staff, especially nursing
Engaging patients in activities requires creativity and commitment from all staff. With tight budgets and limited resources, we must get innovative. Look around for supplies already on hand that could be repurposed. Collaborate with nurses, volunteers, and families to integrate engagement beyond formal programming.
Scheduling is also key - activities shouldn't be limited to 8 to 4 on weekdays. Incorporate evening and weekend options when more patients are available and energized. Understand that activity preferences may shift after retirement - what interests someone at night or on weekends now? We must accommodate altered schedules and find new ways to stimulate patrons when traditional programming lulls.
This takes education and dedication across departments - activities staff can't do it alone. But with a collective passion for patient engagement, we can enhance well-being and connection. On a shoestring budget, we can still foster community, spark interest, and give meaningful purpose to days. Patients deserve rich lives at any age or ability - together, we can make it happen.
Staff Feedback
- “I can see they are much happier after the group. I thought they were slow and irresponsive, now I know I was wrong.”
- “I would not have thought to give them that activity before.”
- “Now I know that if we give them a chance, they can achieve something after all.”
- “Staff can give these residents something to do where they feel useful and they’re enjoying their time as opposed to, you know, maybe looking for negative attention.”
Feedback from patient focus groups shows that small engagement opportunities can work wonders. Simple activities gave residents with dementia a sense of purpose and achievement. Where staff previously saw behaviors, they now see potential.
A nurse shared: "I wouldn't have thought to give them that activity before. Now I know - if we give them a chance, they can thrive. We can spend time responding to behaviors, or give them a two-second activity and see them work joyfully. It's not time-consuming, but totally transforms their experience."
This mindset shift spread through functional maintenance programming from OT. Nurses who initially felt activities weren't their role saw the impact firsthand. The key for busy staff is efficiency - engagement opportunities must be seamlessly woven into care.
When it works, the rewards speak for themselves. Residents light up, enjoying a tailored "just-right challenge." Families reconnect through meaningful shared activities even when cognition is impaired.
The takeaway? We engage human to human, not task to task. Every interaction unveils resident interests, preferences, and strengths. Support these, and you support the person. With compassion and creativity, we can enrich each moment of every day.
Key Take Aways
- Productive engagement may include solitary activities.
- ‘Doing’ things accumulates more social contacts than watching or listening to things.
- Activities that presented a challenge are most appropriate.
- Promote a sense of purpose
- Individuals with a sense of purpose are less likely to experience the effects of social isolation.
Productive engagement need not occur in groups or clinics. Solitary activities also have merit, provided they spark active participation rather than passive observation. Aim for an optimal blend of solitary and social pursuits.
The key is appropriate challenge. Tasks should stretch skills while ensuring success. This imparts a sense of purpose and achievement. Residents gain confidence checking items off their daily to-do lists.
With tailored engagement, individuals feel less socially isolated. Meaningful activity counters the adverse effects of loneliness. Doing trumps watching, but balance is ideal.
As occupational therapists, our mission is clear: foster community while honoring introversion, and craft purposeful challenges that build self-efficacy. By honoring patient preferences, we can curate days brimming with validated productivity.
- As individual needs change, a flexible environment and a wide interpretation of activities are required.
- OTs can work as consultants for a program.
- Staff training, environmental modification, ID client needs, support groups, and community resources
- Occupation remains critical for everyone throughout their life span.
- Needs must be met in non-traditional ways.
As our seniors change, we need to adapt. If you go back to our practice framework, we need to adapt an activity, the context, the environment, and what have you. We can also act as consultants to a community to help them through these interventions. Occupation and staying engaged are important all the way through the lifespan. We need to tackle this as OT practitioners and how we can do this in non-traditional ways.
Summary
Thank you to all of you. Please see the following list of references.
References
Chakrawarty, A., Ranjan, P., Klanidhi, K. B., Kaur, D., Sarkar, S., Sahu, A., Bhavesh, M., Baitha, U., Kumar, A., & Wig, N. (2021). Psycho-social and behavioral impact of COVID-19 on middle-aged and elderly individuals: A qualitative study. Journal of Education and Health Promotion, 10, 269.
Fields, B., & Smallfield, S. (2022). Occupational Therapy Practice Guidelines for adults with chronic conditions. American Journal of Occupational Therapy, 76(2), 7602397010. doi: https://doi.org/10.5014/ajot.2022/762001
Fritz, H., Seidarabi, S., Barbour, R., & Vonbehren, A. (2019). Occupational therapy intervention to improve outcomes among frail older adults: A scoping review. American Journal of Occupational Therapy, 73(3):7303205130p1-7303205130p12. doi: 10.5014/ajot.2019.030585
Lewis, E. & Lemieux, V. (2021) Social participation of seniors: Applying the Framework of Occupational Justice for healthy aging and a new approach to policymaking. Journal of Occupational Science, 28(3), 332-348. DOI: 10.1080/14427591.2020.1843069
Proffitt, R., Abraham, M., & Hughes, C. (2018). Experiences of people with arthritis who participate in quilting-related leisure activities. American Journal of Occupational Therapy, 72, 7211515273p1. doi:10.5014/ajot.2018.72S1-PO6032
Citation
Weissberg, K. (2023). Fostering meaning and purpose for individuals in senior living. OccupationalTherapy.com, Article 5615. Available at www.occupationaltherapy.com
