Krysta: Thank you so much for having me back. During my time working for an orthopedic hand surgeon in the greater Philadelphia area, I had the opportunity to learn about an in-office procedure used to free the median nerve within the carpal tunnel. I am excited to share this information with other clinicians who also have an interest in hand therapy, and specifically in treating Carpal Tunnel Syndrome.
What is Carpal Tunnel Syndrome (CTS)?
Carpal Tunnel Syndrome (CTS) is a common medical condition affecting hand function. It Is caused by compression of the median nerve at the wrist. The median nerve becomes inflamed, and the pressure on the nerve results in a person experiencing carpal tunnel symptoms. Carpal tunnel symptoms can be associated with certain tasks such as repetitive hand motions, awkward hand positions, vibration, strong gripping, and mechanical stress on the palm. There are several occupations that can lead to carpal tunnel symptomatology, including secretaries, mail carriers, clerks and hair dressers. Doctors used to think that CTS was just caused by repetitive motions or overuse injuries, but recent research shows that it is also caused by a congenital predisposition. Some people simply have smaller carpal tunnels than others. It has also been linked to pregnancy, diabetes, thyroid disease, and rheumatoid arthritis.
Signs and Symptoms
Symptoms of CTS usually come on gradually, and they can be in one or both hands. Typically, symptoms first appear in the morning with people often claiming that they have to shake out their hands. This is most likely because of sleeping with some flexion in the wrists. Other symptoms:
- Numbness and pain
- Burning sensation
- Muscle weakness
- Muscle wasting
- Hand cramping
- Disrupted sleep
- Impaired sensation
People with CTS often claim they cannot open things like medication bottles and jars, and they frequently drop items as well. Muscle wasting may occur in their thenar atrophy. Sometimes you may see a little bit of an indent or a divot where the thenar eminence is. There can be some hand cramping during functional activities, disrupted sleep, and impaired sensation. This combination of symptoms is called Carpal Tunnel Syndrome, or CTS. As we know, CTS can impair a person's ability to complete their ADLs and IADLs, such as dressing, cooking, medication management, and sleep.
Wrist Anatomy
Let's look at the anatomy in Figure 1.
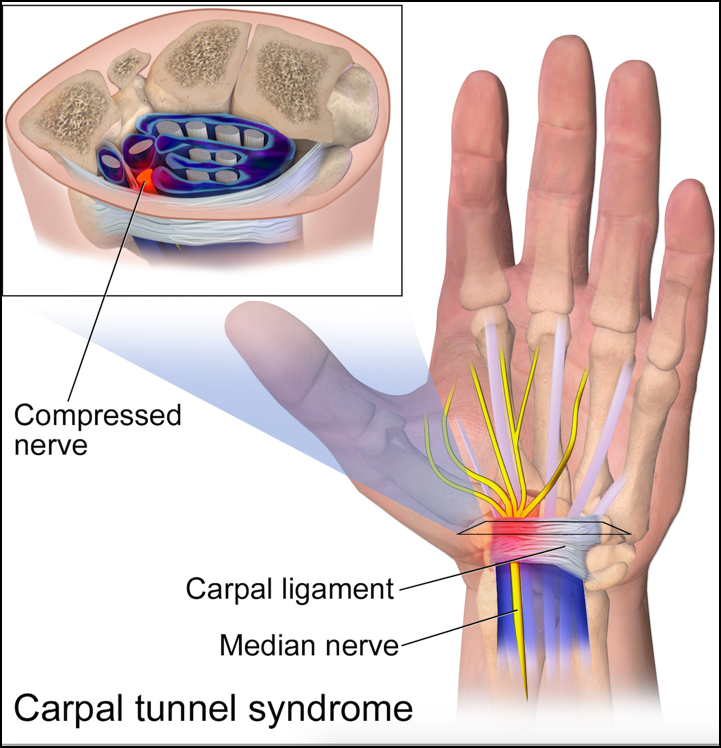
Figure 1. Wrist anatomy. (Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. (Own work) [CC BY 3.0 (http://creativecommons.org/licenses/by/3.0)], via Wikimedia Commons)
The median nerve and flexor tendons pass through the small tunnel. These tendons then attach muscles to bones within the hand and control the movement of the fingers. The median nerve transmits signals from the brain to control the actions of the fingers and the hand and also carries sensory information to the brain pertaining to temperature, pain, and touch. The thumb, index, middle, and ring fingers are all affected by the median nerve. Within the carpal tunnel, the tendons of the fingers surround that median nerve. When these tendons swell, the space within the tunnel is reduced and pressure can be put on the median nerve.
Median Nerve
In the upper arm and near the shoulder, the median nerve branches off of the brachial plexus shown in Figure 2.
Figure 2. Median nerve distribution (Henry Vandyke Carter [Public domain], via Wikimedia Commons).
It runs down the length of the arm parallel to the brachial artery. Part of its path covers the medial side of the arm near the biceps brachii and the brachialis muscles. Most of the nerve runs lateral to the artery. However, it does cross over into the cubital fossa of the elbow. The median nerve also extends downward through the forearm and ultimately runs into the carpal tunnel as it enters the hand. Since the nerve is so long, it contains many major branches. It also innervates a number of muscles along the entire length of the arm. People who believe they have CTS typically consult a physician once their symptoms get to be a little bit too much.
Tests
Evaluation may include identifying workplace risks; looking at their job duties; having them bring in a job description; looking at the frequency, duration, and intensity of the work required; and by performing certain tests to determine if there is damage to the median nerve.
Phalen's Test
The first test is the Phalen's test. To perform this test, the patient places their flexed elbows on a table and allows their wrists to fall into maximum flexion. The patient is then instructed to push the dorsal surface of their hands together and hold this position for about 60 seconds. This position increases pressure within the carpal tunnel causing compression on the median nerve. There is also a reverse Phalen's test. For this test, the patient is asked to maintain a position of full wrist and finger extension for two minutes. The pressure in the carpal tunnel begins to increase after about 10 seconds with this test, and the longer this position is held, the more pressure there is on the wrist and carpal tunnel. Both the Phalen's and reverse Phalen's tests are considered positive when the patient's carpal tunnel symptoms are reproduced, especially the burning, tingling, and numbness. If the test is negative then the patient will feel no pain or any other symptom.
Tinel's Test
The next one is the Tinel's test. The practitioner taps on the median nerve at the wrist to illicit the sensation of tingling or the pins and needles feeling. The test is positive when it produces symptoms such as tingling in the thumb, index, middle finger, and then that radial half of the fourth finger. If the nerve is not compressed, then the patient will have a negative result and feel no pain and symptoms.
Dynamometer
A dynamometer can be used to assess wrist strength and for a comparison of both hands, especially if only one is effected by CTS. This is going to help to establish a baseline strength. It is also a useful test to determine progress or decline over time and after interventions.
Quick DASH (Disbilities of the Arm, Shoulder, and Hand)
Next, we have the Quick Dash or the Disabilities of the Arm Shoulder and Hand.
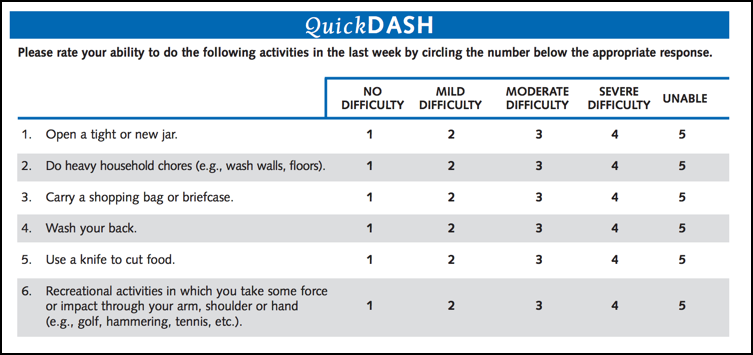
Figure 3. Example of part of the Quick DASH.
This is a commonly used assessment in hand therapy. The Quick DASH is an 11 item questionnaire which looks at a person's ability to perform certain upper extremity activities. This is a self report where patients can rate their level of difficulty with tasks that interfere with their daily life on a five point scale.
Semmes Weinsten Monofilaments Test
The Semmes Weinsten Monofilaments tests is a sensory assessment tool which consists of a set of monofilaments which vary in thickness and diameter. If you have not had the opportunity to use this test in practice, I am sure that many of you remember this one from school. The monofilaments are used to help map out sensory loss that a person may have. This is a systematic procedure where the evaluator begins with the smallest monofilament and then works up to the largest one.
Nerve Conduction Study
Another test that may be conducted, depending on insurance coverage, is a nerve conduction study. This is used to determine whether or not there is nerve damage and dysfunction. The procedure measures how quickly electrical signals move through the peripheral nerves which are located outside of your brain, along the spinal cord. These nerves help to control muscles and pick up sensation. Undamaged nerves will send strong electrical signals quickly, while a damaged nerves will have weaker signals that move in a much slower rate. This study will determine if there is an injury to the fiber or the myelin sheath surrounding the nerve. It can also help to differentiate between a nerve disorder and a condition where a nerve injury has affected the muscles.
EMG
An EMG test is often performed at the same time as a nerve conduction study. The EMG records the electrical signals that are firing through the muscles. This helps to locate the nerve damage and assess the extent of it. This test is performed by placing two electrodes in the skin, one to stimulate the nerve and one to record the sensation. The nerve then receives a brief electrical shock from the stimulating electrode. This is usually a pretty unpleasant experience for the patient. A nerve conduction velocity or a speed between 50 and 60 meters per second is considered within the normal range. A velocity outside of the norms suggest that the nerve is damaged or diseased. The big advantage of a nerve conduction study is that it is considered an objective measurement as compared to the other tests we talked about which are more subjective.
Surgery
There are several surgical options to treat CTS. Today, I am going to discuss three of them. We have the open release, the endoscopic release, and then a noninvasive alternative, the hydroneurolysis. Typically, before any of these procedures are performed, conservative measures are recommended. The main purpose of treatment is to reduce or eliminate repetitive injury to the median nerve. In some cases, CTS can be treated with a wrist splint to minimize or stop pressure on the nerve. If that does not work, some patients may benefit from antiinflammatory medications, icing the wrist, or possible injection in the wrist to reduce the swelling. Specific hand and wrist exercises are also helpful. Treatment or management of medical disorders such as diabetes, thyroid problems, and sometimes even weight loss are also appropriate. It helps the patient improve their symptoms. Therapy along with avoiding activities that are going to aggravate the symptoms whenever possible are recommended. These conservative measures are going to continue for about two months or longer.
Once a surgery is selected and performed, a dressing will be applied to the patient's hand. He or she may require a little extra assistance at home with every day activities because the post-op hand is going to need to be protected while it is healing. For optimal healing, they want to avoid getting the stitches or the skin wet for a little while. Stitches are going to be removed about two weeks after surgery. They also want to avoid both repetitive use of the hand and hyperextension of the wrist for about a month after surgery. Pain and numbness often improves pretty soon after. Tenderness in the area of the incision for several months is pretty common.
Pre-Op Therapy
Some pre-op therapy can usually help to determine if a patient has been performing appropriate exercises. Some people think that any kind of exercise of their hand is good for treating CTS, but we know that this is not true. There are some common exercises that people think are helpful, but they only make the symptoms worse. Hand exercises that patients should not be doing are squeeze ball exercises, hand gripping exercises, or things like that. Most people with CTS are already doing a lot of gripping type activities during their daily activities, so we really want to reduce that. It is important to make sure the client has exhausted all other options before they go for surgery. Once it is determined what patients have been doing to aggravate their symptoms, we can then recommended appropriate exercises and then maybe even some splints. We want to document whether or not there have been any improvements over the time that we have seen them. From there, the surgeon can decide whether to proceed with surgery.
Some other reasons that a doctor would recommend CTS include non-relief of the pain, muscle weakness and wasting, and symptoms that have lasted for six months or longer with no relief. The CTS is usually an outpatient procedure so the patient can go home the same day. There are two surgeries besides the new one that I am going to review with you.
Surgical Options
Open Release CTS
The first one is the traditional method, the open release. The surgeon cuts open the wrist about 2 inches to perform the surgery. They use surgical instruments to cut through the ligament that is pressing down on the carpal tunnel. This allows more room for the median nerve and tendons to pass through the tunnel with the goal of improving pain and function.
Endoscopic CTS
The second procedure is the endoscopic carpal tunnel release. This is where a thin flexible tube that contains a camera is inserted into the wrist through about a half inch incision. The camera is meant to guide the surgeon once he gets in there to cut the ligament. The surgery is completed with another tool which is put into the wrist through another small half inch incision.
For both procedures, general anesthesia is often used. After the surgery, the surgeon will stitch up the incisions, bandage the patient's hand, and possibly provide a splint for them. The dressing is meant to be changed and worn for about one to two weeks. At that point, the patient attends a follow-up visit to remove the sutures. Some pain in the hand and the wrist after surgery can be controlled with pain medication if they have any, and once the sutures are removed, the doctor will probably recommend some therapy. The recovery period lasts anywhere from a few days to a few months. If the nerve has been compressed for a long time period of time, and they have had the CTS for a while, then recovery is going to take even longer. This means that patients often have to take additional time off form work or adjust some of their job duties. It is also not recommended that they drive until they have some improved grip strength. Of course, these limitations can get in the way of patients completing functional activities while they are healing. With any of the invasive carpal tunnel surgeries, the success rates are pretty low. Studies show that a first time carpal tunnel surgery only has a success rate of about 50 to 60%. Some people choose to or need to have a second surgery, and the success rate of that procedure is even lower, calculated at only 35 to 40%. Overall, research shows that CTS comes back in over 85% of people, even when the surgery is considered successful (Statistics retrieved from: MyCarpalTunnel.com).
Additionally, as with any surgery, there are some risk factors. The anesthesia poses risks for some individuals as well as complications from bleeding, post-op infections, wound care, injury to the median nerve or the nerves that branch out from it during the surgery, injury to blood vessels nearby, and then even some scar sensitivity.
Carpal Tunnel Median Nerve Neurolysis (Hydroneurolysis)
There is a new option, other than the open surgeries I reviewed, called Carpal Tunnel Median Nerve Neurolysis under ultrasound guidance, known as Hydroneurolysis for short. This procedure is safe, predictable, is an in-office procedure, and can be performed while the patient is awake. The Hydroneurolysis procedure, sometimes referred to as hydrodissection, is a technique using a pressured fine stream of fluid acting like a jet to develop tissue planes or divisors in soft tissues less traumatically than with ordinary sharp dissection. It is completed with no incisions and offers the same results statistically as traditional open surgery. In addition, hydroneurolysis is a procedure that addresses nerve pathology and scarring that occurs in carpal tunnel and other compression problems. The median nerve is freed from any surrounding adhesions and the area is decompressed using the fluid pressure to do what is typically done with the scalpel dissection. The procedure is performed by using a probe to emit ultrasonic waves, which produce pictures of the structures within the wrist. This allows the movement of the muscle, joint, ligament, the tendon, the blood vessels, and the nerves to be assessed in real time. When this is done, it allows surgeons to evaluate the pathology with ease and give someone an opportunity to observe how the tissues and structures within the wrist change with movement, allowing for the development of a more effective treatment plan.
