Krista: I am excited to be sharing information about incontinence today. We are going to do this in a two-part series. When you walk away from this course, I hope that you will have some practical tips to integrate into your treatments when you go back to your setting, no matter where you work. I am an occupational therapist, and I specialize in pelvic health and am board certified in pelvic muscle dysfunction. I also work on home safety issues, low vision, cognitive therapy, and primarily spend most of my time with adults and older adults. I started Covell Care and Rehabilitation about 12 years ago. It is a mobile outpatient practice that offers occupational, physical, and speech therapy, counseling, fitness training, private care management, driving rehabilitation, and of course pelvic floor therapy to adults and older adults. We primarily see people in their home and out in the communities. When I first started Covell Care and Rehab, I did not have any of the training that I am going to share with you today. As I got more involved with clients, I started realizing that there were so many issues related to incontinence that needed to be addressed, and that was where our journey started and how we integrated it into our program. Hopefully, it sparks some creative thoughts for you guys wherever you may work.
Incontinence Facts
Anything that deviates from voluntary control over urine and fecal discharge is considered incontinence. The inability to stop from passing gas is also a form of incontinence. We will not go over all of these facts, but I want to just highlight a couple on here so you can start really realizing how many people this affects.
- One-third of men and women ages 30-70 believe incontinence is a part of aging.
- Information on healthy bladder function can help promote the understanding that incontinence is not a normal part of aging but a symptom of another problem.
- The social sacrifices of urinary incontinence (UI) are high and even mild symptoms affect social, sexual, interpersonal, and professional function.
- UI affects 200 million people worldwide.
- Based on expert opinion, 25 million Americans experience transient or chronic UI.
- Consumer research reveals that one in four women over the age of 18 experience episodes of leaking urine involuntarily.
- Of men and women ages 30-70 who awaken during the night to use the bathroom, more than one-third get up twice or more per night to urinate, fitting the clinical diagnosis of nocturia. Of these adults, one in eight say they sometimes lose urine on the way to the bathroom.
- Two-thirds of men and women age 30-70 have never discussed bladder health with their doctor and do not receive treatment. Men are the least likely to talk about it.
- On average, women wait 6.5 years from the first time they experience symptoms until they obtain a diagnosis for their bladder control problem(s).
If you been in OT for a while, especially working with older adults, you have probably started to feel like this is a major problem. Of men and women ages 30-70 who awaken during the night to use the bathroom, more than a third of those people are actually getting up twice or more per night to urinate, which is the clinical diagnosis of nocturia. And of these adults, one in eight say they sometimes lose urine on the way to the bathroom. As an occupational therapist, that is going to make our radar go up as this can be a risk for falling. I see clients that are a little bit older than this 30-70 range most often, and sometimes my clients are getting up four, five, six times a night. On average, women wait 6 1/2 years from the first time they experience symptoms until they obtain a diagnosis for their bladder control problems. Men are even longer. We are in a really unique position as occupational therapists because we have the time to spend with people, and people end up feeling really close to us. They share information that they may not share with their doctors. We are in a good position to start that conversation.
What is Incontinence?
We have already touched on this. Incontinence can be any loss of urine or stool, and it can be a little bit or a lot. Some people will say, "I am kind of incontinent." If they are having loss, that means they are incontinent. Stats from the U.S. Centers of Disease Control and Prevention state that "half the population experienced urinary leakage or accidental bowel leakage." And, about 25% had moderate, severe, or very severe urinary leakage. Additionally, about 8% had moderate, severe, or very severe bowel leakage. We know it is a problem that affects a lot of people.
Impact of Incontinence
Some of these things will be obvious to you.
- Depression
- Social Withdrawal
- Anxiety
- Fatigue
- Increased fall risk
- Restricted sexual activity
- Increased expenses for supplies
- Higher risk of infection
- Skin irritation
Clients with incontinence deal with it 24/7. They are constantly thinking about it, and that can become quite depressing. There can be social withdrawal. My own grandmother was devout with her faith, and she went to church every Sunday. When she started dealing with urinary incontinence, she stopped going because she did not want to disrupt the service to go to bathroom. We can start to see anxiety and nervousness creep in. Can I make it to the drugstore and back today without having an accident? We can also see a lot of fatigue. This is because of nocturia. A person may be up and down every night to go to the bathroom. This also increases their risk of a fall. People can have restricted sexual activity. Supplies for incontinence are very expensive, and as such, folks can be very motivated to reduce their incontinence to reduce their expenses. People with incontinence have a higher risk of infection. We see more urinary tract infections and skin irritation and breakdown with folks that have bowel or bladder incontinence.
Why Should OT Address Incontinence?
Incontinence negatively impacts occupations. When urinary and bowel leakage are in the mix, it can definitely reduce people's goal achievement, and their quality of life. Obviously as OTs, we want to improve that. Forty-five percet of clients receiving home health care reported having difficulty with bladder and bowel control. We are seeing this a lot in home care, skilled nursing facilities, and hospitals. OT evaluations address multiple areas of occupational performance directly related to incontinence including:
- Context
- Cognition
- Safety
- Transfers
- Musculoskeletal deficits
- BADL and IADL routines
- Activity tolerance
- Mood
- Positioning
- Pain
- Fine motor control
- Hygiene
- Balance
- Equipment needs
We want to address whether they can safely get to and from their toilet. We want to also look at cognition to see if they can sequence through a toileting routine safely and well. We look at transfers, ADL routines, activity tolerance, mood, positioning, and pain. These are all the things that we should be addressing in a standard OT evaluation. With pain, you can take it one step further and ask if they ever have pain during a bowel movement or when they cannot go to the bathroom. Do they have pain with urination? If somebody has Parkinson's or an issue with their hands, can they get their buttons and zippers undone, pull their pants up and down, and can they open the package that the incontinence products come in? We also want to look at hygiene. How are they bathing and are they doing a good job in the shower? Can they get cleaned up well when they are on the toilet? If you add incontinence on top of that, things can become even more challenging.
Unique Roles of OT in Different Settings
Let's now talk about the different roles of Occupational Therapy professionals in different settings.
Hospital
It depends on what type of hospital setting, but you may not feel like you have the time to address incontinence in this setting. However, if you are in a rehab type hospital setting, you might be able to talk about incontinence. It might be as easy as grabbing your client's hand and letting them know, that with the onset of an illness or with surgery, that they can have an increase in bowel and bladder disfunction. You can go over this with them, and it may reduce their anxiety. You can begin to educate them on their options as they go through rehab, even if you are only going to be seeing them for a short period of time. We may be the only one disseminating this type of information. We are obviously already addressing ADLs, and so it is a natural segue into addressing bowel and bladder health in a practical, nonthreatening way.
Skilled Nursing Facility
I have done a lot of programming around incontinence in skilled nursing facilities. There are lots of opportunities for OTs here. We spend a lot of time talking with clients and building relationships. We end up getting a lot of that personal information from them that they may not be sharing with other medical professionals or their families. We can integrate incontinence issues into our goals. We can take some leadership opportunities here to start talking about incontinence with nursing, dietary, and the activities department. Of course, there has to be a team approach where people are open-minded to discuss incontinence with you. I have had several presentations with these disciplines that have been very helpful and has enhanced the programming at different skilled nursing facilities.
Home Care
I mentioned that we do mostly mobile outpatient, but I do also work in home care as we contract with different home care agencies to supplement their staffing. Home care agencies will bring me in sometimes to talk about incontinence with clients. They want their clients to have an increased quality of life and be better functionally when they come off of home care. If they do not address the incontinence issues, they may not get better. When you are working with people in their homes, it is so much easier to establish trust. It gives us a unique stance. For example, when we are observing their environment, we may notice pads on the back of the toilet or soiled clothes in the corner of their bedroom. It gives us an opportunity to see what is really going on behind the scenes.
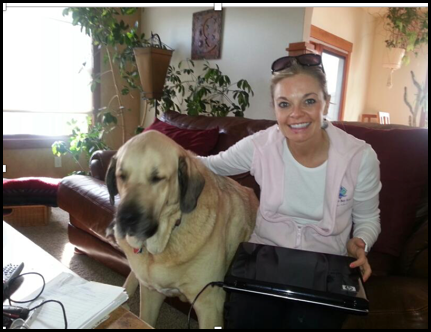
Figure 1. This image shows me at a client's home.
This was a gentleman that was in his late 30s. He was at Craig Hospital originally, which is one of the best rehab hospitals in the country. He had an incomplete spinal cord injury, had come home, and was having to straight cath to void on a regular basis due to tone and other issues related to the spinal cord injury. With some advanced treatment of biofeedback and electrical stimulation, we were able to get him to the point where he no longer needed to straight cath anymore. In this picture is his giant dog who had to sit on the couch with me through every single one of our treatments. You can really make a positive impact with people when you can improve their bowel and bladder health.
Outpatient
In outpatient, it can be a little bit different. Typically, you address more specific things, and the client may be more advanced in their training. However, this does not mean that you cannot start integrating an incontinence program in an outpatient setting as this is where those, with incontinence that is more advanced, are referred. Pelvic pain and prolapse are treated by a specialist, but an OT would look at things more holistically by tying clients' abilities to engage in their ADLs. We can really enhance our treatment plans around incontinence using that framework.
Evaluation and Inquiry
Normalize the Conversation
Now that we have reviewed the different settings, let's talk about how we can start opening up this conversation with clients. The first thing that you have to do is normalize the conversation and start to build rapport. The more comfortable that you are with having conversations about bladders, rectums, and bowel movements, the easier time they are going to have communicating with you. These are some questions that I think you can take right off the page and start using them in your evaluations when you see people today or tomorrow.
- Do you ever have a hard time getting to the bathroom on time? This is less invasive than saying, "Are you incontinent?" or "Do you have accidents?" Those things can be a little off-putting to clients and feel very personal.
- When you need to urinate, do you feel a strong urge and feel that you need to rush to the bathroom? This is a good indicator too. If somebody is rushing to the bathroom, they may be having some issues with an overactive bladder, which we will talk about. Rushing to the toilet really puts them at a higher risk to fall, and you want to make a note of that on your evaluation.
- Do you ever experience leakage when you cough or sneeze or going from sitting to standing? Ask about these things. People are very open with this type of approach. It also helps you build some trust with the patient.
Assess the Environment
You always want to assess the client's environment related to incontinence. If somebody has had a recent back surgery for instance, they may have a hard time getting out of bed, whether it is by themselves or they need staff assistance. That extra time is going to sometimes make their ability to manage their incontinence worse. You will often hear people say, "I got out of bed on my own because I could not wait for the nursing staff to come and get me." Those are all good indicators that somebody is struggling with some level of incontinence, and these are things that OT can definitely address.
Identify Risk Factors
When you are doing your medical review, these are some risk factors to look for that may be related to incontinence.
- Medication
- Stress
- Neurologic diseases
- Diabetes
- Pelvic floor disorders
- History of childbirth
- Hemorrhoids
- Smoking
The opposite of incontinence is constipation. If anybody has had surgery or taken narcotics, you will understand that medication can cause constipation. You want to talk about that with your clients. Stress can make the bladder and bowel issues worse. Neurological diseases like Parkinson's and multiple sclerosis can sometimes wreak havoc on people's bowel and bladder health. Diabetes is another, and sometimes people are surprised about that. Pelvic floor disorders can be related to childbirth. Difficult deliveries, related surgeries, or larger babies can definitely play a role into incontinence issues later. Hemorrhoids and smoking also can cause problems with bowel and bladder health.
Identify if Further Assessment is Needed
I think that many of you are thinking, "Gosh, like I do not even time to cover everything in my regular evaluation, let alone an evaluation for incontinence at this point." That is okay. If you are noticing some risk factors, then you want to make a note of it in your evaluation and come back and do a further assessment later or gets passed on as they transition from perhaps the hospital to a SNF or from SNF to home.
Request Additional Info/Communicate with the Physician
You can always request additional medical records related to incontinence. If you know your client has seen a urologist, you can get that information, but you may have to directly request that. You always want to communicate with the doctor to determine the treatment and type of incontinence.
