Krista: I am excited to do our Part 2 of Incontinence: Practical Tips for the OT Practitioner. If you did not take Part 1, hopefully you will still walk away today with some practical tips. My name is Krista, and I specialize in home safety, low vision, cognitive therapy, and incontinence. I am board certified in biofeedback for pelvic muscle dysfunction, but I started out just like most therapists do as a generalist practitioner. After learning more about pelvic muscle dysfunction during various webinars, I decided to become board certified to be able to treat these issues. If this is an interesting topic for you, I encourage you to continue with your education. I started Covell Care and Rehabilitation because a lot of clients were at home that could benefit from OT, but they did not necessarily fit into a home health model or it was not really advantageous to go to an outpatient practice. I was seeing people at home in our mobile therapy practice that had issues with bowel and bladder health. My guess is that anybody that is listening to us today is probably feeling like they want to know more information about these topics. If you took in our first course of the series, you will see a few slides that are duplicated. We are not going to spend a ton of time rehashing some of those, but for people that have not taken that, I want to be sure that we get everybody at least on the same starting page today.
What is Incontinence?
Incontinence is any non-intended loss of urine or stool, and it can be large or small. About 25% of Americans have had moderate, severe, or very severe urinary leakage. This number comes from the U.S. Centers for Disease Control and Prevention for the National Center for Health Statistics. Incontinence is not a normal part of aging. Some of our clients are actually under the impression that it is a normal part of aging. We may have diseases or issues that contribute to incontinence, but it should not just be thought of as something that is going to definitely come as we get older, so make sure that you advocate for people to know that it's not a normal part of aging.
Educating Clients on Pelvic Floor Dysfunction
Our pelvic anatomy is shown in these pictures in Figure 1.
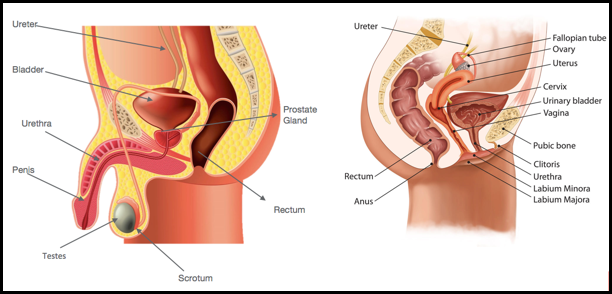
Figure 1. Pelvic anatomy.
I carry 8x10 laminated pictures that are very similar to this of the male and female anatomy. I use these to help clients understand the different components of pelvic anatomy. These images help them understand a little bit about what is going on internally, and I use this throughout treatment. I encourage you to also print these out and use these when you are talking to your patients. I like to point out that between the pubic bone and the tailbone that there are pelvic floor muscles. The muscles are deep and help to keep all of our organs up inside. If we see people complaining of pelvic muscle issues and/or pelvic organ prolapse, we know that something is going on with the muscles. For men, I always point out that the urethra goes through the prostate gland. Thus, when somebody is having issues with an enlarged prostate, the urethra tends to be pushed on and causes difficulty getting the urine out. You may hear men complain about a slow stream, difficulty urinating, frequency, or they cannot get everything out at the same time. With women who have had a hysterectomy, it is helpful to talk about how things can shift and move. This can contribute to urinary and bowel dysfunction. Here are some resources for you to review on your own:
Review of pelvic floor anatomy: https://www.youtube.com/watch?v=P3BBAMWm2Eo
Micturition: https://www.youtube.com/watch?v=US0vNoxsW-k
https://www.youtube.com/watch?v=qMR-rAVlbV0
Defecation: https://www.youtube.com/watch?v=37a_CXKEj5M
The more comfortable that you are with anatomy and how systems work, the better you can explain it to your patients.
Evaluation and Inquiry
Typically, therapists are working in home health, hospitals, or skilled nursing facilities. We do not see patients just for urinary incontinence. That is ok as we can add this as a layer to our evaluations. This enables us to accurately assess incontinence in a better way than what we are probably doing now. There are a few examples here of questions that I ask when I am doing an evaluation.
- Do you ever have a hard time getting to the bathroom on time?
- When you need to urinate do you feel a strong urge and that you need to rush to the toilet?
- Do you ever experience leakage when you cough or sneeze?
You also always want to look at the client's environment. You can pick up great clues up there. You might find incontinence products around, soiled clothing, or a soiled chair. There are also risk factors to look for when you are reviewing the client's medical records.
- Medication
- Stress
- Neurologic diseases
- Diabetes
- Pelvic floor disorders
- History of childbirth
- Hemorrhoids
- Smoking
These things might be a red flag that they could be experiencing some urinary incontinence. If they are taking Lasix or another diuretic, they may have excessive urination. If somebody has a history of childbirth, especially with multiple children, we would want to talk to them about how that has affected them long term. Diabetes and smoking can also contribute to incontinence. The most important thing to find out during the evaluation is if further assessment is needed. There are many times where we go into an evaluation and cannot cover everything in great depth, but if we can identify that further assessment is needed, we can always circle back in a subsequent treatment and address it further. If your patient has described to you that they have any history with needing to see a urologist or gastroenterologist, then you would want to get those medical records from their physicians. Finding out about their background in more in detail can help guide your treatment.
When to Refer to a Specialist
If they have issues like pelvic organ prolapse, pelvic pain, urinary retention, or other neurological dysfunctions, they may need to see a specialist. If somebody is having chronic urinary tract infections, you definitely want to refer them back to their physician or to a specialist, but if somebody is just coming in with a urinary tract infection, you will want to wait until after their UTI has resolved until you treat them. Specialists have advanced training, can provide digital exams, and can integrate biofeedback and electrical stimulation into a treatment plan.
Different Types of Incontinence
You should be able to educate your patients on what type of incontinence they are experiencing.
- Stress
- Urge
- Mixed
- Overflow
- Bowel (Covered in Part 1 of this 2 part series)
- Functional (Covered in Part 1 of this 2 part series)
We covered bowel and functional incontinence and constipation in Part 1 of this 2-part series. We always have to address bowel issues first when a client complains about urinary incontinence. For our purposes today though, we are going to assume that when we are talking about urinary incontinence. We have already addressed the bowel issues or our patient did not really have any bowel issues. In order to figure out what is going on and what type of incontinence somebody has, I always initiate a voiding diary. This is in your handout, and we are going to talk about that a little bit later in the presentation.
Figure 2 shows a graphic that I think is helpful.
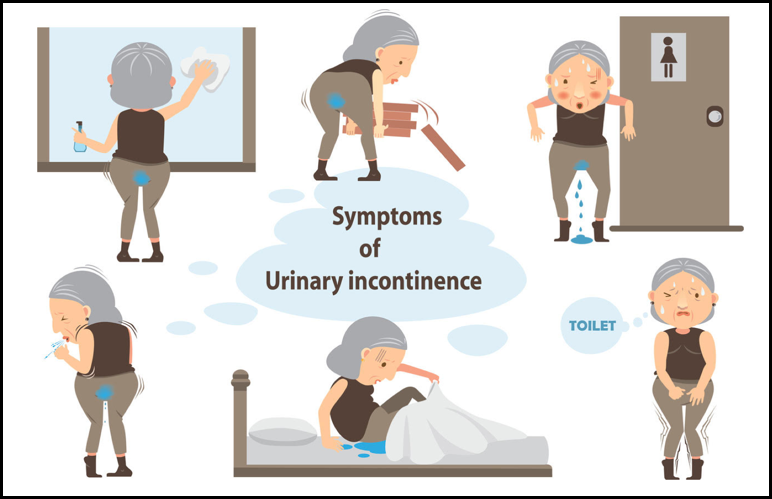
Figure 2. Symptoms of urinary incontinence.
I use something similar with my patients because it is a great conversation starter. It also takes the spotlight off of somebody else talking about when they wet their pants. Some people can be very self-conscious about those conversations. The lady in the top left is wiping off a whiteboard, and it looks like she has had an accident. Sometimes when people are busy and they are going too long without using the toilet, they will have an accident. We oftentimes refer to this as a teacher's or a nurse's bladder because those are typically careers where people cannot get away to use the bathroom. We could probably call it a therapist's bladder as well because I know a lot of us are under productivity requirements or running around doing home health and do not have some place to stop. Keep that in mind when you are needing to go to the bathroom that you definitely want to go when you need to go. The lady in the top middle is picking up something heavy and then having an accident at the same time. The lady in the top right is sweating as she has a very strong urge to go to the bathroom. You can have people experiencie that strong urge to go to the bathroom, and they do not actually leak urine. The lady in the bottom middle is having nocturia. Lastly, the other picture shows incontinence with coughing. This is a great conversation starter and good tool to have with you when you go in to talk to your patients.
Figure 3 is a voiding diary.
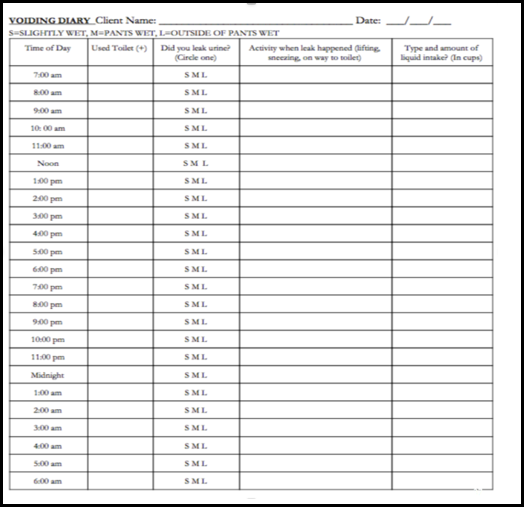
Figure 3. Voiding diary.
Once I have identified that a patient is having urinary incontinence, I want them to fill out a voiding diary for three consecutive days. This is also available in a handout. Usually I do three days, but once in awhile, I will do five if I really feel like I need to do that. It goes from 7 am to 6 am the next day. In the second column, they mark off if they have used the toilet. Once they have used the toilet, they can mark that off, and then we also want to know if they have leakage: small, medium, or large amount. You can have leakage in between going to the toilet or you might have it at the same time. We want to know that, too. The next column shows what activity they were doing when they had the leakage. Finally, in the last column, they mark the type and amount of fluid they are drinking. I will mix this up sometimes and will include a column for when the patient had a bowel movement as well. I sometimes include a column for food intake and what they have been eating. You can tweak this any which way you want, but this is what we use on a daily practice in our treatments and evaluations.
Where to Start
A reminder that you are always going to want to address bowel incontinence, constipation, or a combination of both prior to treating urinary incontinence. Sometimes you may see that pop up in the voiding diary, and it may not have come up in your conversation with the patient.
- If a client is experiencing bowel and bladder issues, the clinician should begin with treating the bowel issues first.
- The bowel can irritate the bladder and reduce the effectiveness of interventions for the bladder if they are not addressed. Sometimes, urinary function will improve as bowel issues improve.
- When the rectum is full of stool, it may disturb the bladder. Chronic constipation and/or straining can lead to excessive stress on the pelvic organs and nerves. This condition also contributes to bladder dysfunction.
- Address these issues first when someone experiences bowel and bladder incontinence:
- Bowel incontinence
- Constipation
- A combination of bowel incontinence and constipation
Bladder Health Review
These are great talking points with patients, and it helps them understand what is considered normal and where they fit into the normal category with their bladder or where they might be on the outside of that.
- The average bladder can hold 2 cups of urine before needing to be emptied.
- We should urinate 6-8 times in 24 hours. As we age, we may need to go more because our bladder shrinks but should not need to go more than every 2 hours.
- Urine should flow out easily without straining and should come out in a steady stream.
- An urge is the sensation you feel as the bladder stretches and fills. It does not always mean your bladder is full and urges should be controlled.
- Your bladder should be completely emptied when you use the toilet. Relax and be sure you have completely voided.
- Holding your bladder for an excessive time (more than 4 hours) may be more convenient for you, but it is NOT healthy for your bladder.
An average bladder can hold two cups of urine before needing to be emptied. Think about your patients that are going often to the bathroom. They may not be voiding very much each time. You can talk about that with them. We should all be urinating between six to eight times in 24 hours, and you can pick that up on the voiding diary. I have had patients going to the bathroom 24-26 times in a 24 hour period because they feel like they constantly need to go. In contrast, I have had some patients that are going as little as four times in 24 hours. They are probably dealing with some dehydration. As we get older, we may need to go a little bit more often than six to eight times in 24 hours because our bladder does shrink, but I do not want you to think it is ok for a client who is 95 to go to the bathroom 12 times a day. Do not go in with those assumptions. We do not want to treat the age but rather the individual. My oldest patient has been 103.
Urine should flow out easily without straining and should come out in a steady stream. Urge is the sensation that we feel as our bladder stretches and fills. It does not always mean that the bladder is full, and urges should be controlled. We often think of a bladder as being round, but the bladder is actually flat on the bottom. Once we get all of the urine out and our bladder starts to fill up again, there starts to be a little pool of urine in the bottom of the bladder. Some of us are so hyperactive to that stretching happens just after it starts to fill again. We think we need to go to the bathroom, and that is not accurate. We need to have to teach our patients about that so that they understand that they should not have to go to the bathroom within 30 minutes of already having gone. If you are in a skilled nursing facility, the patients that feel like they constantly have to go to the bathroom may be dealing with this type of issue.
Your bladder should be completely emptied. This seems sort of obvious, but we have patients that sometimes will only void a little bit because then they feel relief, and then they get off the toilet. You see this a lot in people that have high anxiety or little kids that are too busy to stop and go to the bathroom. We always want to make sure people are sitting on the toilet long enough in order to be able to void. This is true for your nursing home and hospital patients. When a CNA comes in and helps somebody to the toilet, there might be pain, anxiety, difficulty with getting pants down, etc.
