Chronic Obstructive Pulmonary Disease (COPD)-Definition and Pathophysiology
Definition
- A pulmonary disease that is common, preventable, and treatable
- Persistent respiratory symptoms and airflow limitation
- Mixture of:
- Alveolar abnormalities
- Small-airway disease
- Difficulty with getting the air out of the lungs
Chronic obstructive pulmonary disease (COPD) is a condition that all of us are familiar with, however, pulmonary rehab is traditionally a place where few OTs exist or practice. Currently, the literature on best practice for COPD management has been clamoring for an individualized approach, as each COPD individual is unique in their needs. This is where we step in as OTs. To best serve the needs of this population, it will be very important for us to know the disease process itself, as well as, the ways that we can help these individuals with COPD.
COPD, in the realm of pulmonary diseases, belongs in the category where individuals are able to get air in but they have difficulty with getting the air out of their lungs. It is a disease that is common, preventable, and treatable. It is a mixture of alveolar abnormalities and small-airway diseases. There are different subtypes of COPD, as this is an umbrella term. An individual may present primarily with emphysema or chronic bronchitis symptoms and sometimes a mixture of both. To help us visualize how all of these may be different from each other, let's look at our respiratory system up close in Figure 1.
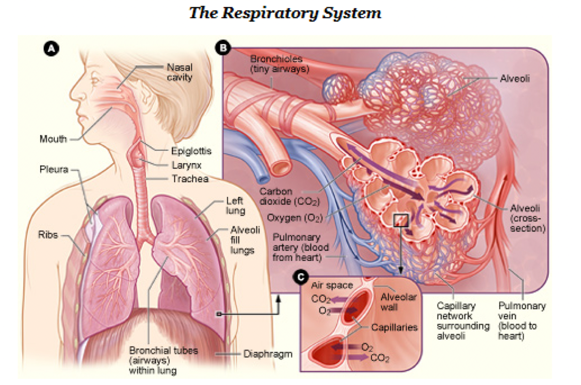
Figure 1. Overview of the respiratory system (http://www.nhlbi.nih.gov/health/health-topics/topics/hlw/system.html).
With emphysema, the airways will be chronically inflamed and narrowed, and there will be a reduced number of tiny airways that are participating in air exchange. The alveoli will have wall destruction, and instead of them being very small, they become bigger, thus reducing the surface area that participates in air exchange. In chronic bronchitis, there is mucus hypersecretion that blocks the airways and the ability of the air to flow out because of the mucus plugging.
Risk Factors
- Main risk factor: tobacco smoking
- Environment: air pollution (indoor and outdoor)
- Occupational exposure: dust, chemical agents, fumes
- Genetics: alpha-1 antitrypsin deficiency
- Age and female gender
- Lung growth and development
- Socioeconomic status
- Asthma and airway hyperactivity
- Chronic bronchitis
- Infections
[Global Initiative for Chronic Obstructive Lung Disease, Inc. (2019). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. ( No. 2019 Report).Global Initiative for Chronic Obstructive Lung Disease.]
What are the risk factors for developing COPD? Worldwide, it is mostly accepted that the main risk factor for COPD is tobacco smoking. However, non-smokers may also develop COPD. It can either result from exposure over time to noxious gases and particles. It can also be a result of an individual's genetics, airway hyper-responsiveness, or poor lung growth during childhood. Other risk factors are outdoor and indoor air pollution, from burning wood or other fuels used for cooking and heating in a poorly ventilated area. And, if you work in an environment with organic and inorganic specks of dust, chemical agents, and fumes, this is considered occupational exposure and a risk factor. This may surprise everybody but the female gender is actually a risk factor for developing COPD. It is largely unknown why, but it could be a combination of different factors such as the airways of women being relatively smaller. So, if they smoke cigarettes, there is more concentration of cigarette smoke. It could also be from the different way that they metabolize cigarette smoke or a different inflammatory response to cigarette smoke. Age is also a risk factor. As we age, there are age-related changes in our respiratory system, and this may increase our risk of developing COPD. Socioeconomic status is also consistently associated with airflow obstruction and an increased risk of developing COPD. This may be due to exposure to indoor and outdoor air pollutants, crowding, poor nutrition, infection, or other factors. Asthma and airway hyperactivity has also been linked in studies to a 12-fold higher risk of acquiring COPD. Chronic bronchitis may also contribute to the frequency of total severe exacerbations, and infections can also reduce the lung function and increase respiratory symptoms.
Pathophysiology
- An airflow limitation and gas trapping
- Gas exchange abnormalities
- Mucus hypersecretion
- Pulmonary hypertension
[Global Initiative for Chronic Obstructive Lung Disease, Inc. (2019). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. (No. 2019 Report).Global Initiative for Chronic Obstructive Lung Disease.]
What happens when we have COPD? First, it is the airflow limitation and gas trapping, or air trapping. As our airways are inflamed, the fibrosis reduces the FEV1, or the forced expiratory volume, in one second or the FEV1 over the FVC ratio, which is the forced vital capacity. So, forced vital capacity is the amount of air a person can exhale during a forced breath. When exhaling, limitations in the peripheral airway reduces the amount of air that can be exhaled and this leads to hyperinflation. There are two types of hyperinflation, which we will be discussing later. Hyperinflation develops early and is the main mechanism for exertional dyspnea or shortness of breath. Bronchodilators reduce gas trapping, and that is why it is very important to know how bronchodilators affect a client's ability to breathe and function.
COPD also results in gas exchange abnormalities. When you have COPD, it typically results in hypoxemia or an abnormally low level of oxygen in the blood. It also causes hypercapnia, which is carbon dioxide retention, CO2 retention, and abnormally elevated carbon dioxide levels in the blood. There are several mechanisms that contribute to this, but primarily, gas exchange, or the ability of your body to exchange oxygen for carbon dioxide, decreases as the disease progresses.
Not everybody will have mucus hypersecretion. Mucus hypersecretion is primarily a feature of a person with chronic bronchitis.
Pulmonary hypertension may develop late in COPD, and this is due to the hypoxic vasoconstriction of small pulmonary arteries.
COPD Common Tests
- Pulmonary function tests (PFTs)
- Spirometry is the gold standard for COPD diagnosis
- Spirometry, lung volumes, diffusing capacity
- Forced vital capacity (FVC), Forced expiratory volume in one second (FEV1), and FEV1 /FVC ratio.
- COPD: FEV1 /FVC = < 0.70
- Chest imaging: chest X-Ray, CT, MRI
(http://www.nhlbi.nih.gov/health//dci/Diseases/Copd/Copd_WhatIs.html)
There are different tests that you will encounter as you are reading through a person's chart. Spirometry is the gold standard for COPD diagnosis. In spirometry, they measure the lung volumes and the diffusing capacity. The frequent results and terms that you will see will be the forced vital capacity, or the FVC, the forced expiratory volume in one second, or the FEV1, as well as, the FEV1/FVC ratio. To have a diagnosis of COPD, the FEV1/FVC ratio should be less than 70% of the predicted for the population with the people that are matching your age and your gender. Chest imaging, such as chest X-rays, CTs, and MRIs are also used, as well as ABGs (arterial blood gas), and this is very helpful in determining if a person is hypercapnic, or a CO2 retainer with elevated CO2 in the blood.
Classification of Airflow Limitation Severity
- FEV1/FVC < 0.70
- Gold 1: Mild FEV1 ≥ 80% predicted
- Gold 2: Moderate 50% ≤ FEV1 ≥ 80% predicted
- Gold 3: Severe 30% ≤ FEV1 ≥ 50% predicted
- Gold 4: Very Severe FEV1 < 30% predicted
(Han, M., Dransfield, M. & Martinez, F. (2019). Chronic obstructive pulmonary disease: Definition, clinical manifestations, diagnosis, and staging. Retrieved from https://www.uptodate.com/contents/chronic-obstructive-pulmonary-disease-definition-clinical-manifestations-diagnosis-and-staging#H18807517)
There are different ways of classifying COPD. The classical way is through the use of the FEV/FVC ratio, which is something that the GOLD or the Global Initiative for Chronic Obstructive Lung Disease Organization has used. However, we know that participation or an individual's appearance or symptoms are more than their FEV/FVC1, so just to familiarize yourself, these are the different GOLD stages and what it means in terms of the FEV1 values.
Assessment of Symptoms
COPD can also be described in terms of symptoms. We will be discussing three commonly used assessments.
Modified British Medication Research Council (mMRC) Questionnaire
- Grades 0-4
- 0: breathless only with strenuous exercise
- 1: breathless when hurrying (level) or walking up a slight hill
- 2: because of breathlessness, slower than people of the same age on level ground, have to stop for breath when walking on own pace on level ground
- 3: stop for breath after 100 meters or after a few minutes
- 4: too breathless to leave the house, breathless when dressing or undressing
(Han, M., Dransfield, M. & Martinez, F. (2019). Chronic obstructive pulmonary disease: Definition, clinical manifestations, diagnosis, and staging. Retrieved from https://www.uptodate.com/contents/chronic-obstructive-pulmonary-disease-definition-clinical-manifestations-diagnosis-and-staging#H18807517)
Since COPD is a disease characterized by breathlessness, the Modified British Medication Research Council, or the mMRC questionnaire grades the breathlessness a person experiences. It is from zero to four, and these the different levels that you have. So it comes from breathless only with strenuous exercises to being breathless as they are leaving the house or when they're or dressing or undressing.
COPD Assessment Test (CAT)
- Patient report of the impact of COPD on health status.
- 8 questions: cough, phlegm, chest tightness, breathlessness when walking up a hill or flight of stairs, activity limitation at home, confidence in leaving home, sleep, energy
- Scale of 1-5
- 0-40 with higher scores indicating more impact of COPD symptoms on health status1
[American Thoracic Society. (2016). COPD assessment test (CAT). Retrieved from https://www.thoracic.org/members/assemblies]
The next one would be the CAT or the COPD Assessment Test. This is a comprehensive assessment of symptoms. The patient reports on the impact of COPD on their health status. There are eight questions that ask about the quality of their cough, phloem, chest tightness, breathlessness when walking up a hill or a flight of stairs, activity limitations at home, confidence in leaving their home, sleep, and energy. It globally looks at the patient's day-to-day activities on a scale of one to five. You score it from zero to 40, with the higher scores indicating more impact of COPD symptoms on their health status.
Clinical COPD Questionnaire (CCQ)
- 10 items, health-related quality of life questionnaire
- Quantifies the clinical status of the airways
- Understanding of the activity limitation and emotional dysfunction experienced by the individual
- 3 domains: symptoms, functional state, mental state
- 0-6 (least to worst impairment)
- 2 minutes to complete
- MCI: -0.4 points
2.van der Molen, T., Miravitlles, M., & Kocks, J. (2013). COPD management: Role of symptom assessment in routine clinical practice. International Journal of Chronic Obstructive Pulmonary Disease, 8, 461-471. doi:10.2147/COPD.S49392]
The other questionnaire is the Clinical COPD Questionnaire or what they call the CCQ. This is a 10 item health quality of life questionnaire and quantifies the clinical status of the airways. It also gives an understanding of the activity limitations and emotional dysfunction experienced by an individual. It has three domains: symptoms, functional state, and mental state. It is graded from zero to six, with zero being the least impaired and six is the worst impairment. It usually takes two minutes to complete, and there is a minimal clinical difference improvement of minus 0.4 points. In order to indicate that the person has improved, their score, or clinically important difference, must decrease by 0.4 points.
Combined COPD Assessment
- Spirometry: severity of airway limitation
- Dyspnea assessment with mMRC or CAT™
- History of moderate and severe exacerbations (and prior hospitalizations
- Airflow limitations: 1-4
- Symptom burden and risk of exacerbation: A-D
Now recently, as they have compiled research on COPD, they have realized that categorizing COPD is really more than a client's ability to forcefully exhale, air out from their lungs in one second. In response, they have developed this GOLD Combined COPD Assessment into categories from A to D. GOLD stands for the Global Initiative for Chronic Obstructive Lung Disease. It involves the spirometry or the severity of their airway limitation, their dyspnea assessment with either the mMRC or the CAT, the history of moderate and severe exacerbations, and prior hospitalizations, the degree of airflow limitation, and then, the symptom burden and risk of exacerbation. To make it easier for everybody to understand, I have plugged these areas into each of the boxes in Figure 2.
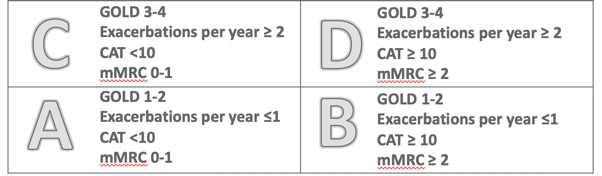
Figure 2. Overview of the GOLD Combined COPD Assessment.
(Global Initiative for Chronic Obstructive Lung Disease, Inc. (2019). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. ( No. 2019 Report).Global Initiative for Chronic Obstructive Lung Disease.)
The GOLD 1 to 2 categories, or A and B, are the individuals that are experiencing fewer symptoms either with dyspnea or have less of an impact of COPD on their quality of life. Then on the top levels, these are those that have had experienced exacerbations two or more times every year.
Bode Index
- Assessment of COPD severity and prognosis
- Survival prediction in 4 years
- Calculation based on FEV1, 6MW, mMRC dyspnea scale, and BMI
- 0-2 points 80%
- 3-4 points 67%
- 5-6 points 57%
- 7-10 points 18%
The Bode Index is an assessment of COPD severity and prognosis. It calculates the individual's risk of hospitalization and death from COPD. The calculations are based on the FEV1, the Six-Minute Walk Test, the mMRC, The Dizziness Scale, and the BMI. It predicts survival in four years based on the points. There is an online calculator where you plug-in the points, and it gives you the result.
COPD Foundation System
- This is based on spirometry, regular symptoms, number of exacerbations in the past year, oxygenation, emphysema on CT scan, chronic bronchitis, and comorbidities.
- 0: spirometry normal
- 1: mild, FEV1 /FVC < 0.70, FEV1 ≥ 60% predicted
- 2: moderate, FEV1 /FVC < 0.70, FEV1 30-60% predicted
- 3: severe, FEV1 /FVC < 0.70, FEV1 <30% predicted
- U: undefined, FEV1 /FVC > 0.70, FEV1 <80% predicted
The COPD Foundation has developed its own system as they recognized that there were different ways of classifying COPD. They also wanted to recognize that sometimes the results of the tests do not indicate whether a person has COPD or not. Their staging system provides recommendations on who would benefit from spirometry tests and provides therapeutic recommendations. The domains are based on the assessment of spirometry, the regular symptoms that the person experiences, the number of exacerbations in the past year, their level of oxygenation, the degree of emphysema that they have seen on the CAT scan, and the presence of chronic bronchitis and comorbidities.
Within all of these domains, they have developed five grades. The spirometry grade zero, or SU zero, means that their spirometry values are normal, but they have symptoms that require treatment. The spirometry grade U is undefined. They have their FEV1/FVC ratio at more than 0.7, which normally you would not classify these people as having COPD. Classically, they have also been categorized under a restrictive lung disease, but they have seen that some of these people do need treatment that is relevant for people with COPD. Then, the other grades,1-3, are based on the FEV1/FVC ratio.
