Ken: Thank you very much for having me back. It is my pleasure to complete a two-part course series on maintenance therapy in the home health practice setting I hope that the participants listening in are able to use this material immediately after we are finished today.
Review of Part 1
I want to review Part 1 to start today's course. Maintenance therapy is a very narrowly defined benefit that not many people get. Less than 1% of the home health claims are these types of claims. I believe that there are a number of people that are receiving care that is maintenance-level care, however, it is being billed as restorative care. Often, these end up getting denied by Medicare as a claim that does not meet the improvement standard. Like we talked about last week, if it is a restorative case, the goal is to restore, in part, the whole previous loss of function. This is something that we need to keep in mind as we go through these slides. Maintenance is a limited benefit. We have to clearly define what the patient's deterioration risk is and then be able to justify the skill that we are providing through the documentation.
OASIS, Functional Reassessments and Maintenance
Q. Do I still have to perform functional reassessments on maintenance cases?
A. YES. All reassessments (restorative and maintenance) are to determine the effectiveness of the plan of care for the established goals.
Q. Do we still need to complete OASIS Assessments?
A. YES. Nothing has changed regarding home health agency requirements for OASIS submission at SOC, ROC, Transfer, Follow up and DC.
Do we still have to perform functional reassessments on maintenance cases? The answer, that is yes. We talked about this last week. All cases, regardless whether it is restorative or maintenance, require a functional reassessment to determine the effectiveness of the care plan either to maintain a patient where they are or to improve the patient from a previous loss of function. As far as OASIS, nothing has changed in that regard. Start of Care, Resumption of Care, Transfer OASIS, Follow-up OASIS, which would be a recertification, and Discharge OASIS are still in place, regardless of whether it is a maintenance or restorative case. You may have a case that is restorative for one discipline and maintenance for another discipline. One discipline might be working on maintaining something, whereas the other discipline is working on restoration. It is not mutually exclusive that the patient is one type of episode or another. It can vary. And, you can move back and forth between restorative and maintenance, depending on the patient's condition.
Let's say you start with a restorative case. The patient makes a little bit of progress. That is great. But then you do a functional assessment, and the patient seems to have what we call plateaued, and if you do not continue, they are at risk for deterioration. This can then become a maintenance case. While you are titrating down your therapy visits, maybe twice a week to once a week to once every other week, you notice that the patient has a regression. If you need to increase the frequency, you could treat as a restorative case again. It can get very complicated within an episode. I just wanted the share that the regulations do not say it has to be one or the other and that it cannot change back and forth within an episode.
Home Health Therapy Coverage
- Medicare Part A – CHHA
- 3 options for coverage once COP’s and eligibility criteria are met.
- Homebound criteria, medical necessity, reasonable and Necessary, under the care of a physician, an Intermittent need for services. (Medical Necessity Resource available for free from Home Health Section of APTA website…www.homehealthsection.org).
- Restorative – Expectation for material improvement.
- Maintenance - When designing or establishing a maintenance program, the qualified therapist must teach the patient or the patient's family or caregiver’s necessary techniques, exercises or precautions as necessary to treat the illness or injury.
- Maintenance - Skilled therapy services are covered when an individualized assessment of the patient’s clinical condition demonstrates that the specialized judgment, knowledge, and skills of a qualified therapist (“skilled care”) are necessary for the performance of a safe and effective maintenance program.
There are three options, two maintenance benefit options, and one restorative. Before we even get into whether it is a restorative or maintenance-type case, they have to first qualify for care. Under the Part A benefit or the CHHA (Certified Home Health Agency) benefit, the person has to be homebound, have a medical need, and the care you about to provide needs to be reasonable and necessary following standards of practice. As far as the number of visits you are expecting to make, your frequency, duration, and your interventions, they all need to follow standards of practice, be under the care of a physician, and then have an intermittent need for services. There is a medical necessity resource that is free at homehealthsection.org. I highly recommend that.
Once they meet all of the eligibility criteria, there are different definitions for each level. With restorative, there is an expectation for a material improvement. In the first maintenance option, when designing or establishing a maintenance program, the qualified therapist must teach the patient, or the patient's family or caregivers, necessary techniques, exercises, or precautions as necessary to treat the illness or injury. The other maintenance option is skilled therapy services are covered when an individualized assessment of the patient's clinical condition demonstrates that the specialized knowledge, judgment, and skills of the qualified therapist are necessary for the performance of a safe and effective maintenance program. When you have cases in your agencies and do not know if they qualify or not, come back to these slides and ask the question, "Does this patient meet all of these elements? It will help you with your justification of care and your notes will reflect the appropriateness of the care provided.
Figure 1 gives an overview of the two options for maintenance.
Maintenance – 2 Options
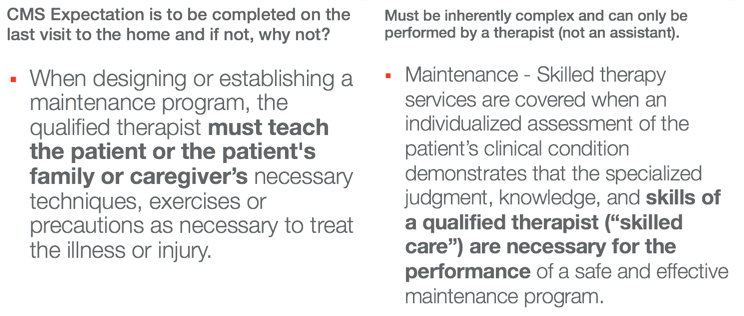
Figure 1. Two options for maintenance.
For option 1, the expectation is that caregiver education will be completed on one visit to the home. And if not, they will want to know why you could not complete the education related to the caregiver or patient on one visit? That would need to be documented if you are going to make more than one visit. In the other option, you have to document in the record what you are doing that is inherently complex that requires the skills of a therapist to perform those tasks. It has to do with what you are specifically looking to do to help the patient. Is it inherently complex? Or are there dangers to what you are doing that you do not feel that it is safe for a family member to perform with the patient? I think the examples we will go through will make this a little bit easier to understand.
Utilization of Maintenance Therapy
Here are the utilization numbers for maintenance therapy.
- PT maintenance – 2017 – 0.72%
- OT maintenance – 2017 – 0.75%
- SLP maintenance – 2017 – 0.48%
*data provided by Poltilove J. Home Health Line. Home health agencies’ use of maintenance therapy 2013-2017. Decision Health. June 18.2018 Vol 43. Issue 25.
- Why so low?
- Two possible reasons – Impact on STAR Ratings and Value-Based Purchasing Program
In the U.S. under the Medicare benefit, maintenance cases are pretty low for all three disciplines. If you add it up, you get 2% of all the cases. One of the reasons is that maintenance therapy affects the facility's star ratings and has an impact on value-based purchasing. The expectation is for improvement with those payment methodologies, yet patients that have maintenance care, will not show improvement. However, they are still calculated into these numbers. That is a reason why agencies may not look to expand this type of care, although it is a benefit the patients do have.
Who Provides Maintenance Therapy?
- Only PT’s, OT’s and SLP’s are allowed to provide maintenance therapy visits as each visit consists of an ongoing assessment of the patient’s condition.
- PTA’s and COTA’s are not allowed to perform maintenance therapy by CMS regulations in home health.
Maintenance therapy in a home setting specifically says that PTs, OTs, and SLPs are the only disciplines allowed to provide care. Assistants, by their scope of practice, are not allowed to do assessments. With a maintenance-level case, the patient is at risk for deterioration, and thus, they need to have an ongoing assessment every visit. This is different than the regulation for maintenance therapy under the SNF benefit. However, we will not be talking about the differences between the benefits for home health and skilled nursing facilities for the purpose of today. I really want to focus on home health so we can keep it pretty clear as to what is covered and not.
Frequency and Duration
- The amount, frequency, and duration of the services must be reasonable.
- Not specifically defined by CMS.
- However, the general consensus is fewer total visits with lower frequencies.
- For example, 1-2x per week x 1 week then taper to 1x per week to 1x every 2 weeks.
Frequency and duration must be reasonable, but they are not specifically defined by CMS. I remember a few years ago, orthopedic cases were typically not seen for daily visits or five times a week-type visits. However, with a lot of patients now going directly home from their acute hospital stay post-op day one or two or even on the same day, there has been an expansion in the industry for therapy to be provided daily for the first few days. This is because the patient has more needs of monitoring and a greater need because of the acuity of their recovery. As they are going directly home, we have been able to justify that need. However, CMS does not say daily treatment is not covered or that one time a week or one time every other week is not covered. It is up to what the patient's needs are. However, with the maintenance care, the consensus that I have seen around the country is the frequency is generally less total visits with lower frequency. These cases may actually be LUPA cases, or Low Utilization Payment Adjustment cases. For example, if you are going into the second episode of care, the patient may be recertified, and you may not even get up to five or more visits. A LUPA is defined as four or less total visits. Agencies try to encourage clinicians to make visits to avoid a LUPA. My comment on that is that you have to have cases that are LUPAs because there will patients who have one visit all the way up through 20-plus visits. And as clinicians, your goal is to provide exactly what the patient needs, not more and not less.
Codes
Billing G Codes- Restorative
- G0151 – Services performed by a qualified physical therapist in the home health or hospice setting, each 15 minutes;
- G0152 – Services performed by a qualified occupational therapist in the home health or hospice setting, each 15 minutes;
- G0153 – Services performed by a qualified speech-language pathologist in the home health or hospice setting, each 15 minutes;
- G0157 – Services performed by a qualified physical therapist assistant in the home health or hospice setting, each 15 minutes; and
- G0158 – Services performed by a qualified occupational therapist assistant in the home health or hospice setting, each 15 minutes.
I want to cover what the billing codes are because some of you may have never seen them. All of the codes I am showing you are for 15-minute increments. The billing code G0151 is for physical therapists. G0152 is the G-code for restorative care for occupational therapists. Thus, if you made a visit to a patient and the visit was 45 minutes, then that would be considered three units. If you made a visit to a patient and the duration of your visit was 40 minutes, it would count as three units of G0152. If any of you work in outpatient therapy practices, the billing is not G-code billing but CPT-code billing. CPT-code billing is where you would bill for the procedure codes of what you are doing as in therapeutic activities, modalities, and therapeutic exercise. They also have 15-minute unit blocks of time for the CPT-codes. In home health, you can go in for a 40-minute visit, and it is not asking you to define that you did 15 minutes of therapeutic exercise and 10 minutes of therapeutic activities. That is not how the codes are done in home health. It is just total time, and it is discipline-specific. However, one thing that is important to know is we have the eight-minute rule. If you provide eight minutes of a 15-minute block of time, then that would count as a unit. If you went into the house and you had a patient for 37 minutes, it would be two units. In contrast, 38 minutes would qualify for three units. When you are making your visits, be accurate with your time. Do not just say 50 minutes for every visit. Adjust that time to what is actually reflective of the true time, and that will be better for you. As far as payment to the agencies, because home health Part A is built under a bundled payment arrangement (an episodic payment arrangement), if you make a visit for two units, four units, eight units, that does not change the billing or the payment. What does change the payment is how many therapy visits you make. That is a factor in the overall episodic payment rate. Unfortunately or fortunately, however you look at it, in 2020, that goes away. As we move into a new payment methodology for 2020.
Billing G Codes- Maintenance
- G0159 – Services performed by a qualified physical therapist, in the home health setting, in the establishment or delivery of a safe and effective physical therapy maintenance program, each 15 minutes;
- G0160 – Services performed by a qualified occupational therapist, in the home health setting, in the establishment or delivery of a safe and effective occupational therapy maintenance program, each 15 minutes; and
- G0161 – Services performed by a qualified speech-language pathologist, in the home health setting, in the establishment or delivery of a safe and effective speech-language pathology maintenance program, each 15 minutes.
If a physical therapist is doing the visit, under maintenance, it is G0159 and G0160 for an occupational therapist. When you are submitting your visits, you are probably not submitting visits based on a G-code. You probably have some internal mechanism in your EMR that has a code next to it, a service code. But in the background, that service code gets converted to a G-code.
Service Codes
- Be clear to explain service codes to staff:
- Restorative Therapy Visit
- Connected to G0151, G0152, G0153, G0157, G0158
- Maintenance Therapy Visit
- Connected to G0159, G0160, G0161
- Billing and IT must be involved in setting up billing and EMR – the point of service – codes
