Editor's note: This text-based course is a transcript of the webinar, Occupational Therapy And Fatigue After Cancer, presented by Jantina Kroese-King, Occupational Therapist/Clinical Epidemiologist.
Learning Outcomes
- After this course, participants will be able to recognize the impact of fatigue after cancer.
- After this course, participants will be able to identify fatigue symptoms to educate clients.
- After this course, participants will be able to list steps to provide treatment to cope with fatigue after cancer.
Introduction
Hello, everybody. I'm delighted to meet you all the way from Holland. Isn't it fantastic that it is so easy nowadays to meet and inspire each other from across the world? I'm working as an OT and as a clinical epidemiologist; I'm quite interested in not only OT but also groups of people and how to diagnose and intervene.
Overview
0-5 | Introduction |
5-10 | Facts fatigue |
10-30 | Explaining model energy |
30-35 | Energy module and measurement |
35-45 | Sleep-cognitive function |
45-55 | E-health |
55 – 60 | Take home message/Questions |
Here is an overview of today's course. I already started a bit of an introduction. Next, I want to reveal something more about the facts of fatigue. Then, I want to explain a model of energy. I also want to provide some information about the measurement of fatigue and intervention, specifically looking at sleep and cognition. Nowadays, E-health is used, so I think it is also good to focus on that as well. At the end of the course, I will leave time for questions.
US Facts
- Sleight et al., 2022
- Systematic review of functional outcomes in cancer rehabilitation
- The number of cancer survivors is increasing steadily, with more than 26 million by 2040
- Affects physical, psychosocial, and cognitive domains
- Guidelines based on evidence are limited, but developing
In the United States, Sleight developed a comprehensive system at Greenview in 2022 to assess functional outcomes following cancer rehabilitation. While the primary focus of the article is on these outcomes, it also provides valuable insights into the growing number of cancer survivors, a trend that is particularly noticeable in smaller regions like Holland.
The increase in the population of cancer survivors can be attributed to several factors, including advancements in the diagnostic phase, the aging population, and continuous improvements in cancer treatments. However, it's crucial to acknowledge that cancer's impact extends beyond the physical aspects, affecting psychosocial and cognitive well-being.
Holland already has guidelines related to cancer rehabilitation and survivorship care. Still, it's evident that these guidelines can be further developed to provide more comprehensive support. As the number of cancer survivors continues to rise, the OT community in Holland can contribute to expanding and enhancing these guidelines to meet the evolving needs of this growing demographic. Developing a more robust framework for cancer survivorship care is a crucial mission for occupational therapy in Holland.
AOTA: Cancer Rehabilitation with Adults
- Fatigue
- A distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferences with usual functioning (National Comprehensive Cancer Network- NCCN, 2016)
The wonderful book Cancer Rehabilitation with Adults, from AOTA, emphasizes the importance of addressing fatigue in cancer rehabilitation. It defines cancer-related fatigue as a distressing and persistent subjective experience of physical, emotional, and cognitive tiredness. This fatigue is often not directly proportional to recent activities and can interfere with a person's usual functioning. The subjective nature of this fatigue highlights the need for collaborative approaches with clients.
Sleight's article also discusses long-term problems faced by cancer survivors. Even after successful cancer treatment, individuals may continue to experience health issues. This highlights the ongoing need for support and rehabilitation in cancer survivorship.
Late-Term Problems After Cancer
(Sleight, 2022)
- Number 1: Health-related quality of life, up to 80% report problems
- Number 3: Fatigue, 40% report problems
- A systematic review of functional outcomes in cancer rehabilitation research (Sleight, 2022)
Another article, though somewhat dated, bears a memorable title, "It's Over, But It Isn't." This title resonates with the fact that a substantial percentage of cancer survivors continue to face health-related quality of life issues. In some cases, this can affect up to 80% of survivors. Notably, fatigue plays a significant role in these issues, impacting 40% of survivors. This statistic underscores the importance of addressing both significant and non-significant fatigue in the context of cancer survivorship.
Fatigue (Sleight, 2022)
- Variations in the type of cancer and phases of treatment
- Five community-based, most hospital-based
- Exercise helps
- Yoga, Tai Chi, and dance programs show improvement
- Positive results for fatigue and quality of life
- Five community-based, most hospital-based
This article highlights the significance of addressing fatigue, a prevalent issue in many articles related to cancer survivorship. These articles encompass various cancer types, such as breast cancer or hematology, and different phases of treatment. Some individuals are undergoing curative treatments, often involving chemotherapy, while others are in long-term, primarily hospital-based care. It's crucial to approach these articles from the perspective of the specific cancer type and treatment phase they discuss.
However, what emerges from these articles, particularly Sleight's findings, is that interventions can make a difference. One key revelation, which has been known to some extent but bears repeating, is the positive impact of exercise. This applies not only after a cancer diagnosis but even when there is a suspicion of cancer. Exercise is emphasized repeatedly. The interesting aspect is that exercise doesn't necessarily mean hitting the gym, which may not be everyone's preference. Activities like yoga, Tai Chi, and dance have shown significant benefits. They offer alternative ways to promote movement and alleviate fatigue, providing diverse options for individuals who may be uncomfortable with traditional gym workouts. Importantly, these activities don't just combat fatigue but also enhance overall quality of life.
Poll: What Does Fatigue Influence (the Client/Patient)?
Let's look at this poll. Do you go through an explanation with the client about fatigue factors? Could you please all vote? I see that most of you do that. I am glad as I think it's so important.
Factors That Impact Energy
- Biological (Disease/ Treatments)
- Psychological
- Social
It's interesting to note that when discussing factors that impact energy levels, many individuals affected by cancer tend to focus on psychological and social aspects rather than the disease or treatment itself. This highlights the profound psychological and social impact that cancer can have on a person's life. Understanding these aspects is essential for providing comprehensive support and care to individuals dealing with the aftermath of cancer, particularly in the long-term phase when treatments are often completed. It's heartening to see that extensive research is being conducted in this area, which can help inform more effective interventions and support strategies.
Fatigue: Factors to Consider
- Functioning before the cancer
- Other diseases
- Fear/process
- Thoughts (cognition)
- Sleep pattern
- Activity regulation
- Social support/ interaction
Functioning before cancer can have a significant impact on the experience of fatigue during and after treatment. Pre-existing conditions or fitness levels may either mitigate or exacerbate the effects of cancer and its treatment. Understandably, a cancer diagnosis often brings about fear and anxiety, both of which contribute to feelings of tiredness. The entire process, from diagnosis to treatment and recovery, is unfamiliar and can be mentally and emotionally exhausting.
Additionally, cognitive factors, such as thoughts and beliefs about one's energy levels, play a role. Patients may believe they are too tired to engage in certain activities or that they need to take it easy, which can affect their behavior and overall fatigue.
Sleep patterns are another essential aspect that influences fatigue. Disrupted or irregular sleep can worsen fatigue, making it important to maintain a consistent sleep routine. Activity regulation is something occupational therapists often work on, helping individuals avoid rushing through tasks and learning to conserve energy.
Social support is valuable but can also be energetically demanding. While it's not about complaining, it's essential to recognize that interactions with family, friends, or colleagues, while supportive, may require energy.
Effective communication about fatigue, or more appropriately, "energy," is crucial. Constantly using negative terms like "tired" can reinforce a person's perception of fatigue. Therefore, reframing the conversation to focus on managing one's energy can be a more constructive and positive approach to addressing this issue.
Reflect On What We Do: Communication
- How do we speak as a professional?
- Fatigue, tired or…
- Energy?
Instead of fatigue, I would like to reframe this as energy management.
Module: Energy Management
- Role of OT!!
- Keep moving (Rock et al., 2012)
- Activity analysis
- Aims (COPM)
- Body awareness
- https://shop.iknl.nl/behandelprogramma-medisch-specialistische-revalida.html
- Keep moving (Rock et al., 2012)
It's evident, as proven by Rock and other researchers, that movement and physical activity are pivotal in managing and boosting one's energy levels. I often start by asking clients how frequently they engage in physical activities such as walking, Tai Chi, dancing, or any form of movement. Through this discussion, we identify what activities provide energy and which ones consume it.
What's interesting, and perhaps not surprising, is that people tend to overlook the importance of taking time to rest and recover. Even when they do sit down, it's often with a mobile device, an iPad, or in conversation with family, which still expends energy. It's rare to find individuals who dedicate a substantial amount of time during the day to proper rest.
Another aspect that often gets overshadowed is the shift in values and priorities that can occur when facing a disease like cancer. Many people enter a survival mode and prioritize the necessary tasks, but they lose sight of what's truly important to them. The Canadian Occupational Performance Measure (COPM) offers an excellent framework to help individuals identify their most important areas of focus. It's not about trying to do everything, but rather discerning what "everything" means to them personally.
One particularly crucial topic is body awareness, as emphasized by the Dutch website link provided at the bottom. Developing body awareness is essential because it enables individuals to recognize when they are fatigued. In cases where people can't perceive their fatigue, it becomes challenging to regain control over their energy levels. Thanks to advancements in medical imaging, such as PET scans, we now have more evidence to support the role of body awareness in effectively managing energy.
Energy Management IKNL
- Module IKNL: Palliative and After Cured
- Measurement; MVI-20
- Registration Time/Level of Intensity of Activity (Activiteiten Weger)
- https://www.meandermc.nl/zorg/behandelingen-onderzoeken/activiteitenweger/?urile=wcm:path:/mmc2021-bestanden/folders/9
- Education/Health Counseling (Koke)
- Body Awareness (Dixhoorn)
- Coping/Behavior (Acceptance and Commitment Therapy/Mindfulness)
In this same guideline from the International Cancer Registry in Holland (IKNL), there's a specific module for managing energy, which has been developed with the input of many OTs in the country. This module involves a daily registration where individuals not only record their daily activities but also label them according to the amount of energy each activity requires. This is often color-coded as yellow, orange, red or numerically as 1, 2, 3, or described as light, medium, or heavy. This process helps people recognize the activities that give them energy (usually marked as -1 or green) and those that consume energy. The time of day doesn't matter as much as the energy cost of the activity, but late in the day, when energy reserves are lower, activities can feel more exhausting.
To delve deeper into this concept, two individuals in Holland have developed a practical system for this energy management approach. They've also translated it into Norwegian, and it might be a valuable tool for English speakers once it becomes more available.
Effective education on health and teaching people how to regain control over their well-being is essential. Health counseling or education plays a crucial role in this process. Graded activity, as highlighted by Koke, is a concept that can help rebuild energy. It involves measuring the energy expended during an activity and gradually increasing it to build stamina. The book by Dixhoorn also proves useful for body awareness.
Various courses and exercises, including breathing, body scans, mindfulness, and other practices, can help individuals regain control over their bodies. It's a learning process, especially for those who may initially find it challenging. It's about training the body to find balance and rest, creating awareness about the physical responses to daily activities. This kind of body awareness is highly valuable.
Another key aspect is understanding how individuals cope with their situation. Some people are accustomed to powering through without reflecting on their thoughts and actions. This coping process can be complex, and it may require involvement from a psychologist or colleague. However, it's important to recognize that our thoughts influence our actions, and this is where occupational therapy can play a role. The field of acceptance and commitment therapy is gaining importance and can help individuals take steps toward acceptance and flexibility in thinking.
Poll: Do You Measure Fatigue as an OT?
When assessing fatigue in your clients, there are several methods you can employ. I'd like to inquire about your practices in this regard. Do you simply ask clients if they are tired without using any specific measurement? If that's the case, please select the "No, not specific" option.
Alternatively, do you employ a 1 out of 10 score, with 10 representing extreme tiredness and 1 indicating feeling fine (or the reverse scale if you prefer)? If you use this numerical scale, choose the second option.
Another approach is to use a specific questionnaire like the MFI-20 (Multidimensional Fatigue Inventory) at the beginning of your intervention. If you do this, select the third option.
Lastly, do you use a questionnaire like the MFI-20 at both the beginning and the end of your intervention? If you do this, choose the fourth option.
It's worth noting that some research articles recommend specific tools for assessing fatigue, so it's essential to align your approach with these recommendations if necessary. I appreciate your input, and it's interesting to see the various methods used by professionals.
MFI 20, Multi Fatigue Inventory
- Which measurement is used?
- Information in advance
- Subscales: General fatigue, physical fatigue, reduced motivation, reduced activity, and mental fatigue
- “2 points after treatment” are needed.
(Smets, AMC)
https://www.med.upenn.edu/cbti/assets/user-content/documents/Multidimensional Fatigue Inventory (MFI).pdf
It's excellent to see that many of you use measurements for assessing fatigue in your clients. These measurements often provide subscales that can help you pinpoint the specific aspects of fatigue your clients may be experiencing, whether it's general fatigue, physical, reduced motivation, reduced activities, or mental fatigue. Some of you might use automatic systems where you can see the changes right away, which is highly beneficial for tracking progress.
Seeing a 2-point difference in fatigue levels from the beginning to the end of your intervention is a significant indicator of progress, though it's essential to consider natural recovery as a factor as well. Commitment to using these measurements is a valuable aspect of your practice.
Energy
- Alert:
- Sleep Pattern
- Nutrition and Lose Weight
There are some crucial aspects that are often overlooked when addressing energy and fatigue in individuals dealing with cancer and its treatments. First and foremost, sleep patterns play a significant role. Sleep disturbances are common during and after cancer treatment, and they can contribute to increased fatigue. It's essential to assess and address sleep issues to ensure patients are getting the rest they need.
Diet and nutrition are also vital factors to consider. As you've mentioned, patients may have specific dietary goals or concerns, such as weight loss. In some cases, it's important to collaborate with a physician to determine the right timing for weight loss goals, as focusing on weight reduction when the body needs to recover and maintain energy may not be appropriate. Ensuring patients are well-nourished and hydrated is crucial, and your observations about the importance of regular snacks and proper meals are valuable.
Your holistic approach to energy management takes into account not just physical activity but also the broader lifestyle factors that can impact a person's energy levels. This is essential for providing comprehensive care and support to individuals dealing with cancer and its aftermath.
Sleep and Energy
- Several factors are involved:
- High level cortisol; Stress response system out of balance; Activity of parasympathetic nervous system
- Activity during the day
- Sleeping hygiene
The importance of understanding sleep patterns in the context of occupational therapy cannot be overstated. This revelation comes from an experienced OT who recognizes that numerous factors affect an individual's sleep, particularly those who have experienced cancer or are currently battling the disease.
Post-cancer, and during the ongoing struggle, the body often produces an excess of cortisol, a stress hormone. This is because the body's stress response system remains unbalanced. Individuals grappling with a cancer diagnosis and its implications are subjected to continuous stressors, which include fear and the upheaval of their previous way of life. As a result, their stress response system goes into overdrive, leading to heightened cortisol production. This can manifest as stress, discomfort, headaches, irritability, and a sense of being off-balance.
To redress this imbalance, it is essential to understand that the stress response system and the parasympathetic system, responsible for relaxation, must be in equilibrium. In many instances, people become so engrossed in their daily activities, juggling work, family, household responsibilities, and future planning, that they remain in a state of constant alertness throughout the day. This persistent vigilance and engagement prevent the parasympathetic system from activating as it should. Consequently, the stress response system continues to operate, maintaining cortisol levels at an elevated state, and negatively impacting an individual's ability to relax and sleep well.
The solution lies in creating opportunities for individuals to "zone out" during the day, fostering the parasympathetic system's activation. Implementing relaxation techniques such as yoga, savoring a cup of tea, or going for a brief afternoon walk can prove transformative. This not only helps during the day but also reflects positively on nighttime sleep. It's the small, consistent steps that matter most in this process.
Furthermore, a noteworthy practice was shared by a Dutch scientist who advocated making appointments with oneself to pause and relax. This notion resonates with the OT, suggesting that individuals, and even professionals themselves, should set aside time to "zone out" and recharge, fostering balance between the stress and relaxation systems.
Sleep hygiene, a term frequently employed to describe habits conducive to a good night's sleep, is another critical facet of this discussion. Establishing a pre-sleep routine can signal to the body that it's time to unwind. This routine may include a soothing bath or foot soak, reading a calming book, or taking a leisurely walk. The sleeping environment should be conducive to rest, maintaining an ideal temperature and minimizing distractions. Additionally, it's advisable to limit screen time close to bedtime, as exposure to screens can overload the brain with information and hamper relaxation, making it difficult to attain restful sleep.
In the realm of energy management, sleep patterns should be a focal point of consideration. By addressing these aspects, individuals affected by cancer can achieve a more balanced and restorative sleep, contributing significantly to their overall well-being and energy levels.
Energy and Cognitive Problems
- “I can’t read a book or document work.”
- “I can’t keep up with a conversation.”
- “I can’t start a task.”
- “What do I do or say…”
- ? Chemobrain…..
Another intriguing aspect that has been the subject of discussions with colleagues and a conversation with a professor from a specialized cancer hospital in Amsterdam is the connection between cognition and energy. This correlation is quite apparent, as many individuals affected by cancer report cognitive challenges. These challenges manifest as difficulties in tasks like reading, maintaining attention, participating in conversations, initiating tasks, or recalling what they were doing or intending to do.
People often describe their experiences by saying things like, "I struggle to read a book; my attention wanders after just a couple of pages," or "I can't keep up with conversations when multiple people are talking simultaneously; I feel lost." They might also express that starting a task is overwhelming, leaving them standing aimlessly, or that they frequently forget simple things like why they went from one room to another.
While some individuals attribute these cognitive challenges to "chemo brain," there's more to the story. These cognitive difficulties aren't solely caused by chemotherapy but can be linked to several factors impacting brain function.
"Chemobrain"
- Several causes
- Discussion
- Functioning before cancer
- Influences hormonal therapy
- Side Effects on the Brain
It's important to recognize that cognitive challenges aren't limited to chemotherapy; various cancer treatments like radiotherapy and immunotherapy can also affect a person's cognition and how their brain functions. This broader perspective can lead to more meaningful discussions.
While the term "chemo brain" is commonly used, it can create the misconception that these cognitive issues are solely related to chemotherapy. However, when you engage in conversations with individuals in the long-term phase of cancer survivorship, they often attribute their cognitive challenges to factors beyond just chemotherapy. They may describe feeling overwhelmed because they are trying to do too much in a single day.
Instead of narrowly focusing on "chemobrain," it might be more beneficial to discuss the side effects of these cancer treatments on the brain. The following model illustrates the relationship between energy levels and cognitive function:
When a person's energy is depleted due to the harsh treatments they undergo, such as chemotherapy or hormone therapy, they don't instantly return to their pre-cancer energy levels. It takes time for the body to recover. The lowered energy directly impacts their alertness and their ability to process information. So, it's essential to consider that cancer treatments have a broader impact on both energy and cognitive function.
Hierarchy of Cognition
The functions of the brain can also be impacted (Figure 1).
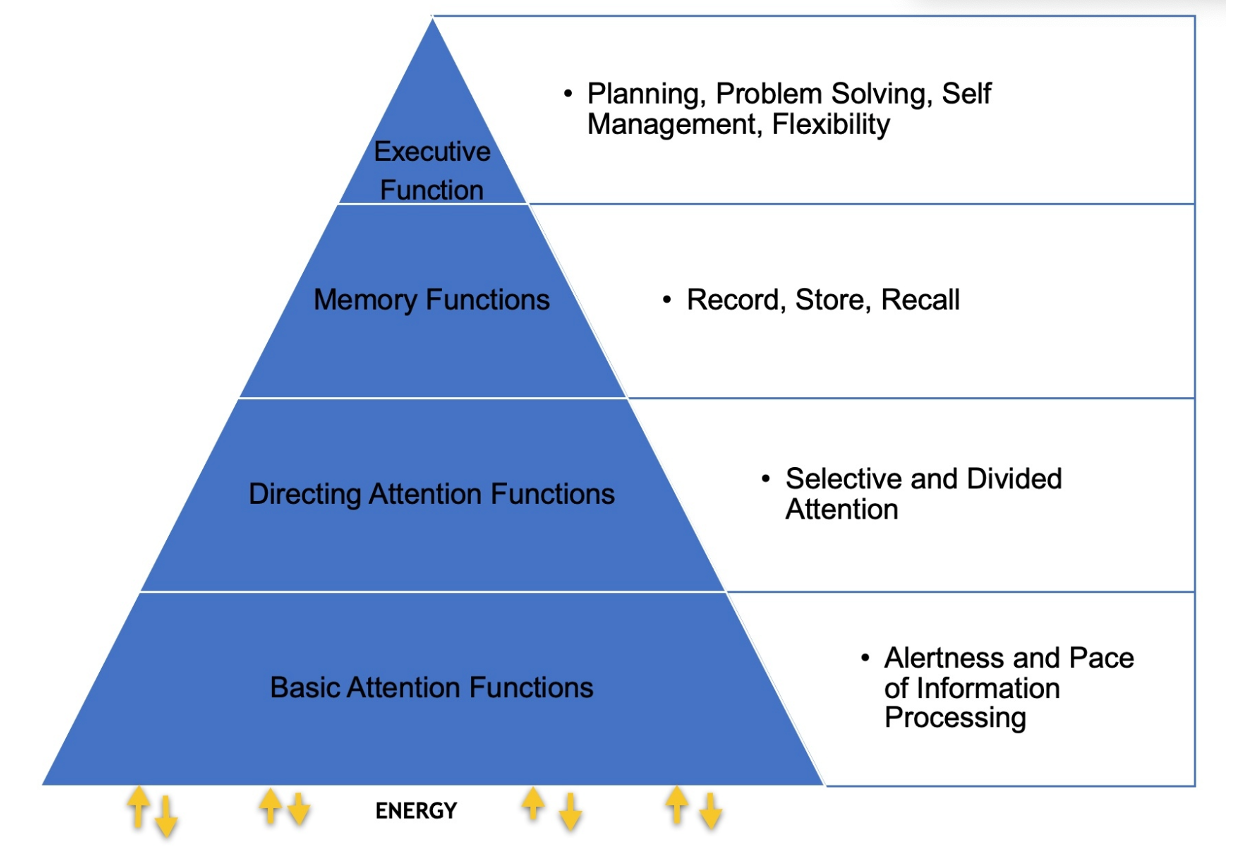
Figure 1. Hierarchy of Cognition.
The changes in cognition, particularly information processing and alertness, can be quite pronounced. It's not just the memory and recall of information that is affected, but also one's ability to multitask, concentrate on tasks, and maintain executive functions. This can make returning to work, especially in demanding roles like teaching, nursing, or leadership positions, particularly challenging. People often want to bounce back to their pre-cancer energy levels, but it takes time to recover, and they need to adapt to this new reality.
The key message is that, post-cancer, individuals may need to slow down and adjust their pace of life. In the fast-paced Western world, it's important to recognize that there's a need for a more measured approach to energy management. By adapting their daily activities to their current energy levels, individuals can experience fewer cognitive challenges. Adjusting to a slower pace, taking the time to recover, and allowing the body to adapt can be empowering.
An example of a lady's experience illustrated how cognitive problems can manifest due to energy management. She had difficulty deciding how many of a particular item to order at the end of the day. After discussing her energy management, it became clear that her energy was depleted by the end of the day due to work and a challenging conversation with her mother, making her less flexible in decision-making. By managing her energy better, she was able to regain clarity of thought and function more effectively.
Understanding these cognitive challenges and their connection to energy management empowers individuals to adapt and regain control over their lives.
Do You Use ‘E-Health?’
- App?
- Special program?
- Online session (indirect)?
- Pdf?
When it comes to eHealth, occupational therapists working with individuals who have experienced cancer and fatigue use a variety of methods. The survey results show that:
- 26% of respondents use apps to provide information or tools.
- 17% use specific online programs for distance support and guidance.
- 26% utilize video conferencing platforms like Zoom or Microsoft Teams.
- 31% make use of written materials delivered via email, such as PDF documents.
The use of eHealth tools, including apps and online programs, has become increasingly common, and video conferencing platforms have seen widespread adoption, particularly during the COVID-19 pandemic. This suggests that OTs are embracing digital methods to provide information and support to individuals dealing with cancer-related fatigue.
It's also worth noting that special programs, including those with built-in measurement tools, are being employed to enhance the support provided. These programs can streamline the process and offer more personalized guidance for clients dealing with fatigue.
The survey results reflect a diverse range of eHealth tools and methods used by occupational therapists to address the unique needs of individuals recovering from cancer and managing fatigue.
Using E-Health
- Clients using an app combined with intervention (cognitive, psychological, and functional) showed more improvement than using the app only.
- Effect of mHealth (mobile health) plus occupational therapy on cognitive function, mood, and physical function in people after cancer: Secondary analysis of a randomized controlled trial.
- Lozano-Lozano et al., 2022
- Effect of mHealth (mobile health) plus occupational therapy on cognitive function, mood, and physical function in people after cancer: Secondary analysis of a randomized controlled trial.
Research conducted by Lozano-Lozano highlights the significance of combining mobile health (mHealth) apps with the support and guidance of OTs for individuals recovering from cancer. While the app alone can be beneficial, the study demonstrates that the real power lies in the synergy between the app and the personalized intervention delivered by an OT. This combination results in more substantial improvements in areas like cognition, mood, and physical function compared to using the app in isolation.
This research reinforces the idea that a multifaceted approach to healthcare, one that utilizes both technological tools like mobile apps and the expertise of healthcare professionals, can have a remarkable impact on patient outcomes. The collaboration between mHealth and OT interventions seems to create a unique and highly effective strategy for supporting individuals on their journey to recovery from cancer. In this context, one plus one truly equals three, illustrating the enhanced benefits of a combined approach to patient care.
Telehealth (Hwang, 2020)
- The review explored and confirmed the usefulness of TH approaches in the scope of OT practice for adult survivors.
- Conclusion: More research is needed.
The use of eHealth and telehealth in the field of occupational therapy is invaluable. This study highlighted the increasing effectiveness and relevance of these approaches, particularly in light of the current global context that has seen a rise in remote healthcare services. The advantages of eHealth, such as reducing the need for physical travel and addressing challenges like traffic congestion and distance, were underscored.
While there is a growing body of evidence supporting the efficacy of eHealth in occupational therapy, more research is necessary to further validate and optimize these approaches. The combination of eHealth tools with the expertise of occupational therapists holds significant promise.
Staying informed and engaged in research is important. A proactive approach to healthcare delivery, embracing the use of eHealth, aligns with the evolving needs and expectations of both practitioners and patients in the modern age.
Community-Based (Petrusevicience et al., 2018)
- Community-based OT and various societies vs. only societies
- Non-acute phase
- Better quality of life, role functions, physical, emotional, cognitive, and social functioning.
- Meaningful activities >
- EORTC QLQ C30, QLQ BR23 and EMAS
One more important topic to explore is the focus of research within hospitals, which often concentrates on the acute phase of illness. While this is logical due to the immediate needs of patients, it's equally crucial to delve into the long-term effects of energy, particularly for OTs working in the community.
This research demonstrates that community-based OT significantly improved the quality of life for patients, enhancing their role function, physical and emotional well-being, and cognitive and social functioning. It presented a holistic approach to patient care, encompassing meaningful activities, and highlighted the growing role of occupational therapy in promoting well-being.
Take-Home Message
- Fatigue is an important topic within the treatment of OT
- Measure fatigue
- Specific module for cancer (survivors)
- Fatigue has an influence on cognition
- E-health can be valuable for the treatment of fatigue
The central message is the significance of addressing fatigue, especially in the long term, as it significantly affects patients' lives. Many of you already include energy measurement in your practice, and I encourage others to consider its inclusion. The importance of managing energy effectively in order to prevent cognitive issues cannot be overstressed.
I want to conclude with an inspiring story of a cancer survivor, as shown in Figure 2.

Figure 2. Author with her client.
This is a woman who had faced the challenges of her illness, including losing her job, yet emerged from the experience with remarkable resilience and determination. Despite the fatigue and joint pain she experienced, she decided to start her own catering company. Her story serves as a testament to the power of the human spirit and the role we play in supporting individuals on their journey to recovery.
Questions and Answers
What role does sleep quality play in managing fatigue after cancer?
Sleep quality is a fundamental factor in managing fatigue after cancer. Poor sleep can exacerbate feelings of tiredness and decrease overall energy levels. It's essential to address sleep patterns and potential disruptions to ensure better energy management.
How do stress, anxiety, and depression affect a person's energy levels during cancer recovery?
Stress, anxiety, and depression often accompany a cancer diagnosis and treatment. These psychological factors can have a significant impact on energy levels. They can lead to increased fatigue and decreased overall well-being, making it crucial to address and manage them alongside physical aspects of recovery.
Can you elaborate on the collaboration between occupational therapists and psychologists in cancer recovery?
Collaborative efforts between occupational therapists and psychologists are valuable. When mental health concerns or past issues arise during the recovery process, psychologists can provide essential support and treatment. This collaboration ensures that clients receive comprehensive care that addresses both physical and psychological aspects of their recovery journey.
How can clients measure and manage their energy levels during and after cancer treatment?
Clients can measure and manage their energy levels through self-assessment tools and interventions provided by occupational therapists. These may include questionnaires, apps, or eHealth programs that help clients monitor and improve their energy management. Additionally, discussions with healthcare providers and occupational therapists can guide clients in managing their energy more effectively.
What role does cognition play in the context of energy management after cancer?
Cognition is closely linked to energy management. Fatigue can impact cognitive function, leading to issues like decreased memory, attention, and alertness. Managing energy well can help alleviate cognitive problems. Taking breaks, prioritizing rest, and using relaxation techniques can contribute to better cognition and overall well-being.
Citation
Kroese-King, J. (2023). Occupational therapy and fatigue after cancer. OccupationalTherapy.com, Article 5652. Available at www.occupationaltherapy.com
