Why is Our Role in Mental Health Housing Important?
Do we have a role in mental health housing? In the profession as a whole, about 3% of occupational therapists are practicing in a mental health area. I was just looking at a report that states that suicide rates have increased by 20% over the past 20 years, with some states rising as much as 40%. When you look at all the things that are going on in this country with the increase in mental health issues and the increased awareness about these issues, our role in this area is greatly expanding, and there is a need for our services. Even though we are currently at 3%, as we look towards the future, we clearly have a role in areas of health promotion and possibly prevention of mental health issues on some level.
AOTA’s Identified Areas
The American Occupational Therapy Association has identified that we clearly have a role in these areas. Here are some of the fact sheets that they have created:
- Occupational Therapy’s Role in Mental Health Recovery Fact Sheet
- Occupational Therapy’s Role in Community Mental Health Fact Sheet
- Occupational Therapy’s Role with Posttraumatic Stress Disorder Fact Sheet
- Occupational Therapy Using a Sensory Integration-Based Approach with Adult Populations Fact Sheet
- Mental Health in Children and Youth: The Benefit and Role of Occupational Therapy Fact Sheet
When you look at these fact sheets, you can see we have a clear role and should be involved in mental health housing on some level.
Recovery-Based Care
We also want to think about recovery. Now is the time because the transition from our standard system of care, which was a very maintenance-based approach, stated that occupational therapy's role was quite limited. In this maintenance-based approach, we could not justify what we were doing with people with mental health. There was a shift that went from over 40% of OTs working in mental health care to less than 3%. Claudia Allen's work stems out of this need to be in a medical model with addressing some sort of neuro-physiological issue, and for where we were at that time, that made a lot of sense. However, now when we think about recovery, and we are going to review recovery in a minute, it allows for us to shift our role in to a very different position. Instead of this inability to justify why arts and crafts were very effective in working with clients with mental illness, we can now think about the use of occupation in order to justify why we are doing what we are doing.
SAMHSA defines recovery as "a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential" (SAMHSA, 2012, p.1). This is a fairly simple definition, but when you think about it, it says so much about how people with mental illness have been treated in this country, and really globally.
In 2012, we decided that recovery-based care is the route that we should really go in assisting people with mental illness. It really highlights that we were not doing this before, and that we did not help people to improve their health and wellness. The clients did not get to live a self-directed life, and we did not help them strive to reach their full potential. We held them back. We set goals for them. I can clearly remember early in my career having a client that was 45 years old with schizophrenia. When I asked him his goal, he said that it was to "improve his ADLs." He had chronic schizophrenia and was using the term ADLs; whereas, most people in society would not even know what that meant. It was not his goal, but rather, something that he had been trained to say over and over again. He had probably been saying that same goal for years, but he still presented as disheveled and dirty and not really understanding what that even meant.
10 Fundamental Components of Recovery
There are 10 fundamental components of recovery:
- Self-Direction
- Individualized and Person-Centered
- Empowerment
- Holistic
- Non-Linear
- Strengths-Based
- Peer Support
- Respect
- Responsibility
- Hope
(U.S. Department of Health and Human Services-2005)
These components highlight what our treatment should be based upon. Take the term non-linear. This process is not one where someone just goes from years of being debilitated by their mental illness to one where they are successful, working, and living independently. It is a process like going up a mountain. Sometimes we go up and do not take the right path, thus requiring us to go back down and around to find another way to go up. When you look at these concepts, what is interesting is how well they align with what we do as occupational therapists (Figure 1).
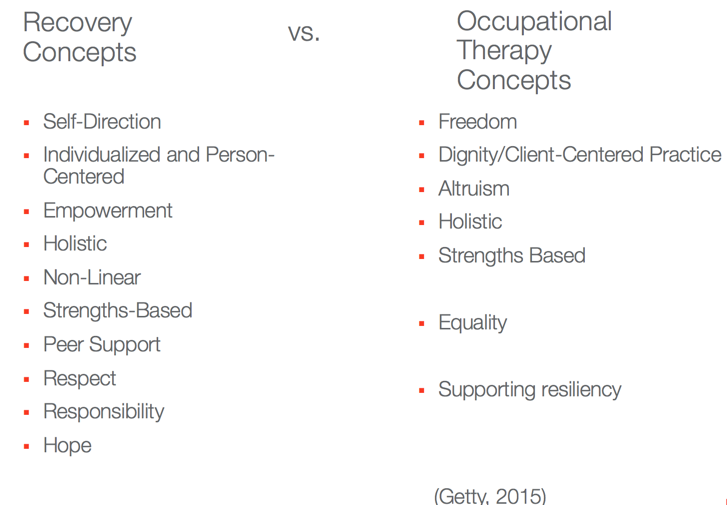
Figure 1. Recovery and OT concepts.
Think about about the concepts of freedom, client-centered practice, altruism, strengths-based approach, and supporting resiliency. It seems to line up perfectly with what we have been doing forever as occupational therapists. We have been practicing client-centered practice for over a hundred years. For other disciplines in the mental health arena, this is a fairly new term. It can sometimes get confused and misunderstood. I have heard clinicians talk about how person-centered care or client-centered practice is an approach where we let the client do what they want to do within their treatment. We, as OTs, know better than that. In the mental health spectrum, we have this really unique role. We can work with our clients very differently than other disciplines.
Public health services need to be:
- Person-centered
- Community integration focused
- Whole health focused
- Evidence-based and cost-effective
We need to be person-centered. We cannot use a cookie-cutter model where everyone receives the same type of treatments. They need to be community integration focused, not this siloed care that focuses on things like sheltered workshops, where we employ people with disabilities and keep them separated or segregated from the rest of the world. We need to be whole health focused as well so that we are not just looking at the person's mental health. We also know that these people, on average, die 20 to 25 years earlier than the general population. We need to address their high rates of diabetes, high blood pressure, and heart conditions. Finally, we need to be evidence-based and cost-effective. Those two go hand-in-hand. We need to be cost-effective because the money is not there to be able to sustain the system, especially not in a maintenance model. The best way to save money is to be evidence-based. For a long time, in this maintenance system, we were doing things that did not necessarily make sense. We were throwing treatments against the wall because they sounded good on a sheet of paper, but they never benefited our clients. For example, we ran things like men's and women's groups that had no evidence to support them.
Four Pillars of Mental Health Recovery
We have four pillars of mental health recovery that have been identified by SAMHSA, 2017.
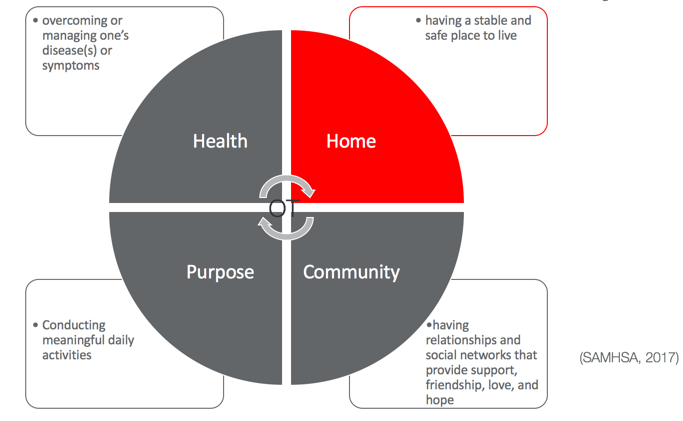
Figure 2. Four pillars of mental health recovery.
The four areas are health, purpose, community, and home. Home here is highlighted because it is a key component to someone's recovery. If we are not working within the home, then we are missing a quarter of what we really need to be focusing on. Home and community go hand-in-hand. If we are working with someone in the home, we can then help to link them better to the community than if we were just doing this in a clinic setting. Thus, supported housing is a key to recovery.
Supported Housing as a Foundation for Recovery
Think about what your house, your apartment, or your space means to you. What would happen if you had that taken away, or if you did not have your own place that you called home.
- Freedom to live independently
- Self-guided daily routines
- Sense of purpose and self-worth
- Community integration
- Decreased stress levels
- Ability to pursue future goals
(Kirsh, Gewurtz, & Blakewell, 2011)
Supported housing gives people the freedom to live independently. It allows for them to go in the direction that they want to go. It helps to establish daily routines for these individuals that are not externally structured. It gives them a sense of purpose and self-worth. It gives them the sense of identity; who I am and how I have my home set up. It facilitates community integration. It decreases their stress levels, because they are not living with other people or they are not homeless. It really helps them to identify future goals and things that they can move towards.
Key Supports in Housing
We have these key supports in housing.
- Connecting to Social Supports
- Goal Setting and Accessing Resources
- Managing Crisis
- Learning Skills for Independent Living
- Trusting and Supportive Relationships over the Long-Term
(Kirsh, Gewurtz, & Blakewell, 2011)
When we think about social supports, I think about my neighbors and my community and how that helps to make me feel like a part of something. Goal setting and accessing resources are other supports. Helping these people to manage crises is important. Something that seems simple to us is often a crisis to the person with a mental illness. An example might be when their lights go out, or they have no heat. These are daily things that we take for granted. We understand how the situation is going to play out, and the people that we should call. How do they manage that? Anpther example is getting a haircut. In order to get a haircut, you have to call ahead, make an appointment, and set time aside. People with a mental illness like schizophrenia might just walk in and expect that they will get their hair cut right away. Learning skills for independent living involves many occupations and sub-occupations. There are big global things like taking care of your house, but then there are other components that go into it. For example, when cleaning the bathroom, there are what I call sub-occupations. You have to clean the mirror, the toilet, the sink, etc.
Many mental illnesses fall under that serious, persistent category like schizophrenia, bipolar disorder, schizoaffective disorder, and severe anxiety disorder. People with these disorders have trouble functioning. Onset for these can be in late teens and early 20s. This is a crucial time period when skills for independent living are developing. Clients are consumed with their illness and are trying to be able to live day to day in their life. They miss out on learning how to do many of these things including: managing finances, using public transportation, regulating their emotions, developing a social network, ironing, cooking, doing laundry, and all of the basic things that we take for granted.
Many other disciplines work with people with mental health issues. These include social workers, psychologists, and mental health counselors. They all use the same medium, verbal therapy; however, they all use it a little differently. It is very hard to learn how to do laundry through a verbal therapy session as an example. Even if we sat in a room each week and discussed how to do laundry, we cannot expect that the client could then go to the laundromat and transition that verbal therapy into actual action. During recovery, occupational therapists have the ability to modify the person, the task, or the environment in order to facilitate this person's success. We use activity analysis and take the person to the laundromat or help them to do the laundry in their house so that we can help them to break down that task and master that skill. Finally, trusting in supportive relationships over the long-term is key to housing. For example, the client needs to be able to trust their landlord. Many clients with mental health issues have trust issues. We need to help them develop social interaction skills in order to facilitate their ability to have these supportive relationships.
Key Facilitators to Support Housing Needs
- Coordinated service delivery between housing and mental health agencies
- Continuum of mental health service options
- Engagement in service plans
(Kerman, Sirohi, Curwood, & Trainor, 2017)
There also needs to be coordinated service delivery between the housing provider and the mental health agency so that there is a connection. There needs to be a continuum of service options, and we need to have that person actively engaged in their service plan so that they are helping them to set their goals.
- A functional system with suitable accommodations
- Service efficacy
- Individualized service
- Promotion of social inclusion
(McCauley, Montgomery, Mossey, & Bailey, 2015)
There needs to be a functional system with suitable accommodations. I am going to talk a little bit later about the impact of the physical environment and where OT plays a role in that. Self-efficacy, individualized service, and the promotion of social inclusion are other key facilitators. When you review all of the services over the last three slides, they are all things that OT can do. OT needs to fill this gap.
Typical Housing Placement
In many states, including New York where I am from, they have transitioned to a housing-first model.
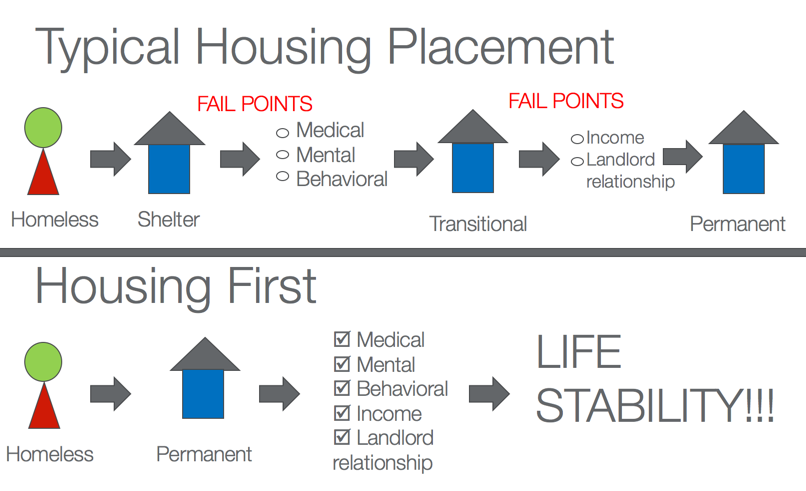
Figure 3. Housing first model.
The top graphic shows the typical progression that we have used for years and years. The person would go into a shelter, and then get their medical and mental health and behavioral services set up. We then would transfer them into some sort of transitional housing program. There they would secure some sort of income and develop a relationship with a landlord in order to maintain permanent housing. This model often failed because there were so many fail points as shown in the graphic. Going into a shelter is one of the big reasons why people remain homeless. They do not want to go into a shelter. A shelter is not necessarily seen as a positive place. There are a lot of negatives, like theft. Additionally, there is often a disconnect with getting medical/behavioral health services. These people do not know how to do that, and the service is not necessarily provided for them. The housing first approach is one that moves someone, who is homeless, directly into permanent-based housing. There, they get all those things that they need.
Housing First
The Housing First program has been shown to improve life stability. There has been some great evidence on this.
- Greater Quality of Life (Patterson et al., 2013)
- Cost-Effective (Tinland et al., 2013)
- Superior outcomes to establish stable housing (Aubry, Nelson, & Tsemberis, 2015)
- More cost effective- housing costs increases but not as much as a decrease in mental health, emergency shelter, emergency room, jail, and ambulance costs (McLaughlin, 2011)
There is a greater quality of life for that individual. It is more cost-effective. The housing cost might increase, but there are decreases in every other area that make up for that. There are decreases in mental health care, emergency shelter use, emergency room visits, time spent in jail, ambulance costs, etc. Ultimately, there are superior outcomes when establishing this person in housing. We are talking about someone going directly from a homeless setting into their own stable housing environment. What about the skills that are needed to be able to maintain that? How do we help them to develop those skills so that they can keep that housing long-term? This is where we can play a part.
