Editor's note: This text-based course is a transcript of the webinar, Occupational Therapy Practitioner's Role In Helping Women Live Fulfilling Lives After Spinal Cord Injury, presented by Natalie Rivera, OTD, OTR/L.
Learning Outcomes
- After this course, participants will be able to identify three gender-specific client factors women experience post-SCI.
- After this course, participants will be able to recognize three female-specific performance patterns impacted by an SCI.
- After this course, participants will be able to list three interventions for managing women’s health post-SCI.
Introduction
Hi everyone! My name is Natalie Rivera. I'm glad everyone's here. My presentation is about the role of occupational therapy practitioners in helping women live fulfilling lives after spinal cord injuries (SCI). I hope you find this information helpful to your practice.
Part 1: Demographics Among SCI
We will start with the general demographics of spinal cord injuries in general.
- Cause and Age
- Age: 16-30
- Risky sports
- Accidents
- Domestic violence
- Age: 60+
- Falls
(Teplitsky et al., 2019; Foy et al., 2011)
Out of all spinal cord injuries, only 20% of spinal cord injuries occur among the female population in general (Figure 1).
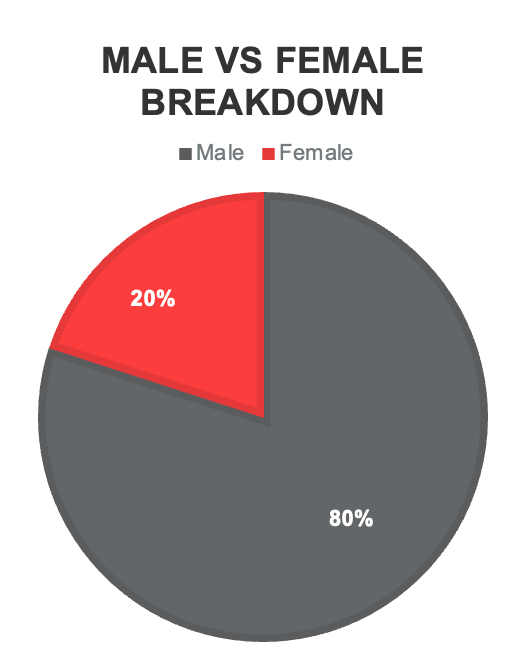
Figure 1. Breakdown of spinal cord injuries between males and females.
The most common injury site for females and males is around the thoracic and lumbar levels. In a systematic review, it was found that there are two predominant age categories more at risk for spinal cord injuries. The first group includes individuals between the ages of 16 to 30, often involved in risky sports, accidents, and other dangerous activities.
When focusing specifically on female-acquired spinal cord injuries, there is also a prevalence of domestic violence. Although research on the percentage of spinal cord injuries due to domestic violence is still limited, it is a significant cause among females. The second group at higher risk includes individuals aged 60 and above, where falls are the leading cause of spinal cord injuries. Many of my female patients in the trauma ICU were women 60 and above who had fallen and also had the comorbidity of osteoporosis.
Part II: Female Roles and Barriers to Occupation
Female Roles
- Mother
- Daughter
- Grandmother
- Sister
- Daughter-in-law
- Mother-in-law
- Wife
- Girlfriend
- Partner
- Friend
- Professional
- Family Members (aunt, cousin, etc.)
There are many roles that I might have to step into, each requiring unique responsibilities, characteristics, and routines. These roles could vary from mother, daughter, grandmother, sister, daughter-in-law, mother-in-law, wife, girlfriend, partner, professional, and more. Each of these roles comes with specific responsibilities. Roles are considered performance patterns under the OTPF. Any injury can significantly impact roles because these roles require certain routines and habits.
Occupations
Figure 2 shows specific occupations that are impacted after a spinal cord injury (SCI).

Figure 2. Areas of occupation affected by an SCI (Click here to enlarge the image).
I'm going to dive deep into each of the occupations and the limitations they may face after a spinal cord injury, starting with sexuality. Sexuality is considered an activity of daily living. Limitations in sexuality after a spinal cord injury can include mobility issues, lack of sensation, decreased activity tolerance and endurance, bowel and bladder incontinence, and autonomic dysreflexia.
For individuals with an injury at level six or above, toileting is another activity of daily living that can be significantly affected. Limitations can include bowel control issues, bladder management difficulties, overall menstrual care challenges, and a lack of menstruation post-injury.
Moving into the last two occupations, considered under the OTPF as health management, we first have pregnancy. Pregnancy in this context involves a more health management role, promoting routines, and self-care. Important areas include weight management, maintaining a bladder and bowel routine, making positional changes for skin integrity, and understanding reproduction with an SCI.
The second concept of health management is overall mental health. Women are statistically more at risk for experiencing mental health disruptions prior to a spinal cord injury. When a spinal cord injury occurs, the risk of experiencing difficulties with emotional regulation, psychiatric diagnoses, and routine management disruptions increases. As OT practitioners, our role involves promoting emotional health and assisting in developing healthier habits.
Part III: Sexual Participation
The first occupation we're going to discuss is sexual participation. As I stated before, it's considered an activity of daily living.
Limitation: Sensation
Biological Factors
•Psychogenic Lubrication T12-L2 •Reflex Lubrication Above S2-S4 •Orgasm can be achieved; however, it is less likely in injuries at cervical and sacral levels.
| Solutions
•Assistive Devices •Strong vibrating devices •T.E.N.S Unit with vaginal insert
|
(Hammond & Burns, 2009; Naphtali & MacHattie, 2009)
One of the strongest limitations that occur after a spinal cord injury is the lack of sensation. Usually, individuals with an injury at T12 or L2 can achieve psychogenic lubrication, meaning they can reach an arousal state through thoughts and fantasies. Though it may be hard for these individuals to achieve an ultimate climax, lubrication is still possible. For individuals with injuries at S2 to S4, they require what we call reflexive lubrication, which essentially means genital stimulation.
Orgasms and climaxes can be very hard to achieve, especially in injuries at cervical and sacral levels. Symptoms such as increased heart rate and the possibility of lubrication are still probable at these levels, but injuries at thoracic and lumbar levels have a higher probability of achieving full climax. As occupational therapy practitioners, we can provide interventions that include education on assistive devices to help with genital stimulation.
Individuals with S2 to S4 injuries have a harder time with reflexive stimulation. Research has shown that genital stimulation is actually easier to achieve arousal than psychogenic arousal. Some devices that can be provided include strong vibrating devices, and there are TENS units with vaginal inserts that help facilitate overall reflexive stimulation.
Naphtali & MacHattie created a manual supported by the American Spinal Injury Association that includes a comprehensive list of devices unique to different injury levels for both males and females. It's called "The Pleasurable Manual," and it is available in the resources section or handout provided. For those interested in exploring possible assistive devices, this manual includes a detailed list of what is available.
Limitation: Mobility
Physiological Factors
•C1-C6: No trunk control, limitations in UE depending on level •T1-T12: Upper extremity use and progressing trunk control •L1-L5: Full use of trunk and upper body, possible standing •S1-S5: Possibility to walk
| Solutions
•Positioning and Positioning Devices •C1-C6: Hoyer lift with partner standing, supine with support wedges and ankle weights •T1-T12: Supine with support wedges, intimate rider device, prone position with wedges, Hoyer lift •L1-L5: Same as T1-T12, intimate sitting with back support and possible positioning on top of partner with ankle weights •S1-S5: Possibility of positions prior to injury, with precautions to standing due to LE weakness |
(Hammond & Burns, 2009; Naphtali & MacHattie, 2009; Sexuality After SCI, 2018)
The next limitation that often occurs after a spinal cord injury is limitations in mobility. To refresh your memory on this topic, individuals with an injury between C1 to C6 usually lack trunk control and have limitations in the upper extremity, depending on the level of injury. If it's a lower-level cervical injury, there's likely more functional use of the hands and upper extremities, but it's still very limited compared to injuries at the thoracic or lumbar levels.
At T1 to T12, upper extremity use is probable and improving, with progressing trunk control as we move down the spine. From L1 to L5, there is full use of the trunk and upper body, and some individuals at lower lumbar levels may even stand. Lastly, at S1 to S5, these individuals might be able to walk but may have very limited activity tolerance and lower extremity strength for ambulation.
To address these mobility limitations, we can provide various interventions. For those at a C1 to C6 level, participation in sexual intercourse might be possible via a Hoyer lift with a partner standing or in a supine position with support wedges and ankle weights. It's important to consider personal factors such as sexual orientation and religious beliefs in these activities.
Individuals at T1 to T12 can still participate in intercourse in a supine position with support wedges or possibly in a prone position with wedges and ankle weights. They can also use a Hoyer lift if available.
At L1 to L5, with improved trunk control, they might use an intimate sitting position or engage in intercourse in a supine or seated position on top of the partner with ankle supports.
Those with sacral-level injuries can usually participate in the previous positions they had before the injury. Remembering that they have lower extremity weakness and decreased activity tolerance is crucial, so avoiding prolonged standing tasks should be encouraged and educated.
Limitation: Sexual Safety
Physiological Factors
•Autonomic Dysreflexia •Skin Integrity •Decreased Activity Tolerance/Pain •Bowel and Bladder Incontinence
| Solutions
•Education on and prevention of Autonomic Dysreflexia •Routine skin inspection •Practicing positional changes
|
(Hough et al., 2020)
Overall, there are specific sexual safety considerations due to a spinal cord injury, one of them being autonomic dysreflexia. This condition usually occurs in individuals with injuries at T6 and above. For those who may not recall, signs and symptoms of autonomic dysreflexia include sweating, a pounding headache, increased blood pressure, and an overall clammy feeling with shivers due to a noxious stimulus. When sexual intercourse occurs, the chances of having an episode of autonomic dysreflexia are quite high for individuals with T6 and above injuries.
Therefore, educating on the symptoms and the necessary safety considerations is crucial. If an episode of autonomic dysreflexia occurs during sexual activity, it's important to stop the activity immediately. The procedure involves holding the individual upright to help reduce symptoms. If the symptoms persist for five to ten minutes, calling 911 for appropriate medical attention is essential.
Another important consideration is the overall skin integrity of the patient. Sexual activity can involve a lot of friction and wear and tear on the skin, so routine skin checkups before and after intercourse are vital. Educating patients on how to perform skin checks and recognize red flags for skin breakdown is crucial.
Occupational therapy practitioners can educate patients on energy conservation strategies and appropriate positioning when it comes to activity tolerance. It is important to test and figure out the most comfortable and pain-free positions for the patient.
Lastly, bowel and bladder incontinence is a significant consideration. To prevent incidents during sexual activity, it's important to establish a bowel and bladder routine before intercourse. This can help avoid potentially embarrassing situations that negatively impact self-esteem during intimate moments.
Contraception
- Oral contraception pills and hormonal preparations need to be avoided within 1 year of injury.
- Progesterone-only pills are most common and have a lower risk of thrombosis.
- Intrauterine devices are not recommended due to at-risk causes of UTI.
- Combined hormone pills (progestogen/estrogen/ Depo-Provera) are not advised for secondary bone fragility.
Now, discussing contraception is crucial for women with a spinal cord injury. Once a woman starts menstruating again, she becomes fertile. While we don't provide contraception directly, it's important to understand how medications might interact after an SCI and how these interactions could present complications. It's also important to respect the individual's preferences and choices regarding contraception. However, it's essential to consider the increased chances of abuse and sexual assault, as discussed earlier.
Given these concerns, some individuals might prefer pharmacological options over barrier methods. One key point to remember is that oral contraception or any pharmacological forms of contraception should be avoided within one year of the injury. This is because patients with spinal cord injuries are at high risk of developing deep vein thromboses (DVTs), and hormonal medications can increase this risk even further.
After the first year post-injury, if individuals choose pharmacological contraception, they often opt for progesterone-only pills due to their lower risk of causing DVTs. Combined hormone pills (progesterone and estrogen) or injections are generally not advised because they increase the risk of DVT and bone frailty. Since individuals with SCI are already at a high risk of falls, these options could lead to fractures if a fall occurs.
Intrauterine devices (IUDs) are another option, but there are some important considerations. The placement of IUDs can significantly increase the risk of autonomic dysreflexia episodes. Additionally, IUDs can elevate the risk of urinary tract infections, so these factors should be weighed if a patient chooses this method.
Barrier methods are also acceptable, but they come with their own limitations. For example, male condoms require careful attention to skin integrity and the potential for latex allergies. It's also important to consider that individuals with reduced sensation might not feel if the condom is uncomfortable, which could lead to skin integrity issues. Female condoms or ring devices require good manual dexterity and fine motor skills to insert, which could be challenging for some patients.
Overall, it is crucial to educate and support individuals with SCI in making informed decisions about contraception that align with their health needs and personal preferences.
Part IV: Pregnancy
Pregnancy is possible with a spinal cord injury. We will now discuss the guidelines that occur with pregnancy and an SCI.
Guidelines Per Trimester
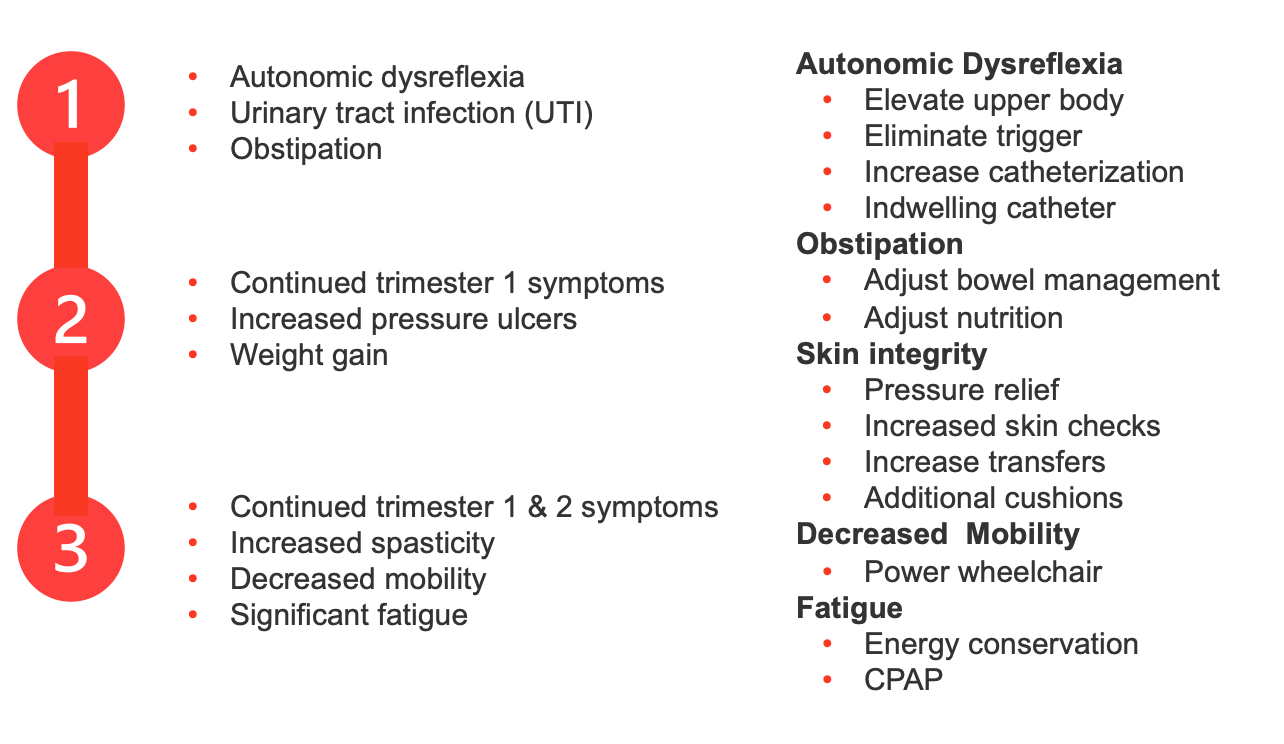
As we know, pregnancy has three trimesters, and some guidelines based on systematic reviews (Figure 3) need to be followed.
(Bertschy et al., 2020; Robertson et al., 2020)
Figure 3. Guidelines per trimester. (Click here to enlarge the image).
In the first trimester of pregnancy, one of the critical concerns for women with spinal cord injuries, particularly those with injuries at T6 and above, is the risk of autonomic dysreflexia episodes. Additionally, urinary tract infections (UTIs) are more likely to occur, and there is a heightened risk of obstipation. To clarify, constipation refers to difficulty having bowel movements but still being able to pass stool, whereas obstipation means a complete inability to have a bowel movement.
As we move into the second trimester, monitoring for autonomic dysreflexia, UTIs, and obstipation continues. However, we must also be mindful of the increased weight gain during this period, which raises the risk of developing pressure ulcers.
Along with the considerations from the first and second trimesters, we need to be particularly vigilant about increased spasticity, decreased mobility, significant fatigue, and heightened oxygen needs in the third trimester. Prolonged sitting can make breathing more difficult, so some women might use CPAP or other oxygen devices.
Several interventions can help manage these conditions. In the case of an autonomic dysreflexia episode, elevating the upper body and eliminating the trigger are essential steps. Increasing catheterization frequency and opting for an indwelling catheter can help prevent UTIs. While some may prefer intermittent catheterization, it is generally recommended to switch to an indwelling catheter during pregnancy to simplify management and reduce UTI risk.
Managing a stricter bowel schedule, ensuring appropriate nutritional intake, and maintaining a regular bathroom routine is crucial. Pressure relief strategies, conducting frequent skin checks, increasing transfers, and using additional cushions are vital to maintaining skin integrity. Switching to a powered wheelchair, if not already used, can also assist with skin checks and mobility changes.
Consulting physical therapy can help address spasticity and tone issues, especially in the third trimester. Occupational therapy practitioners can provide education on energy conservation strategies to manage fatigue, although this remains challenging due to the significant biological changes occurring alongside spinal cord injury.
It's also important to dispel the misconception that a C-section is mandatory for delivery. Vaginal deliveries are common, but the lack of sensation may prevent the patient from realizing they are in labor. One of the most significant signs of labor is a major episode of autonomic dysreflexia. Since contractions are hormonally rather than neurologically based, the patient might not feel them, and the body compensates in other ways, leading to autonomic dysreflexia.
Thus, it's imperative to educate pregnant women with spinal cord injuries about the signs of autonomic dysreflexia and the possibility that they may not feel labor beginning. Proper education and preparation are key to managing pregnancy and delivery effectively for these individuals.
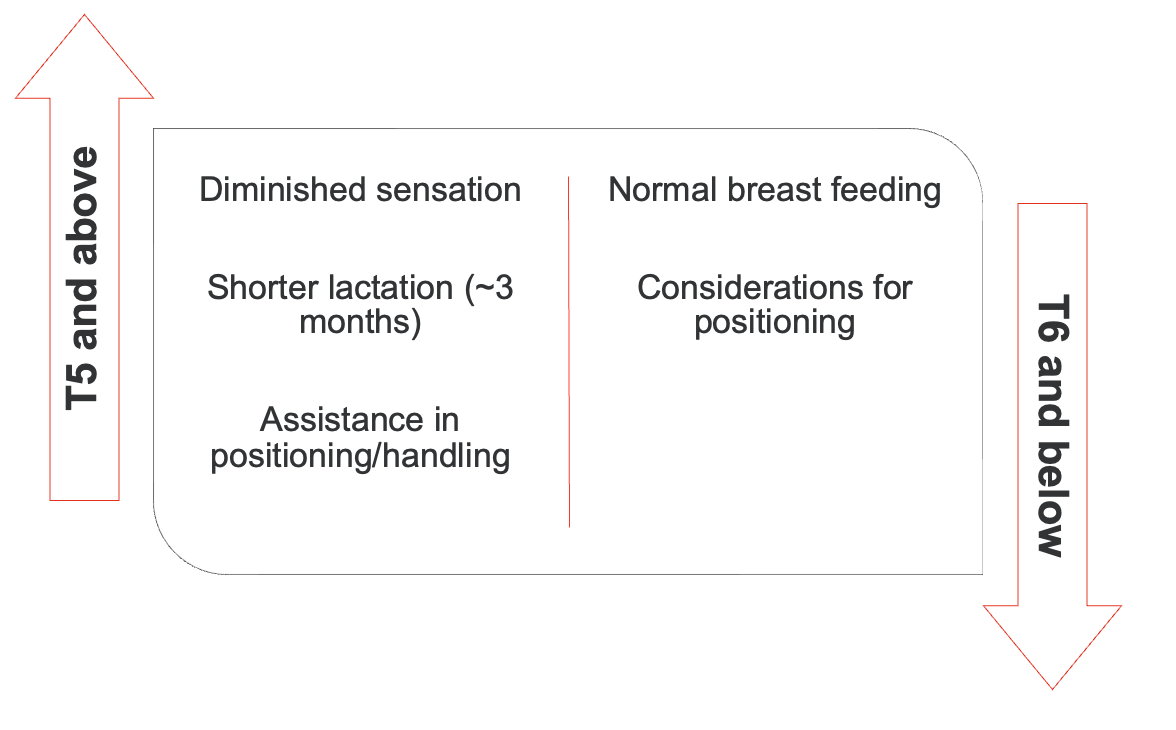
Breastfeeding
In regards to breastfeeding, it remains essentially the same for women with a spinal cord injury. The key difference is that there is typically a shorter lactation period for those with injuries at T6 and above. These patients may require assistance with positioning and handling during breastfeeding.
(Bertschy et al., 2020; Rosetti et al., 2022)
Figure 4. Considerations for breastfeeding.
As occupational therapy practitioners, we can provide education on assistive devices that facilitate the positioning and handling of an infant. For injuries at T6 and below, breastfeeding typically occurs for the same duration as it would without an SCI. The main consideration in these cases is ensuring the proper positioning of both the infant and the mother to make the breastfeeding process as comfortable and effective as possible.
Part V: Toileting
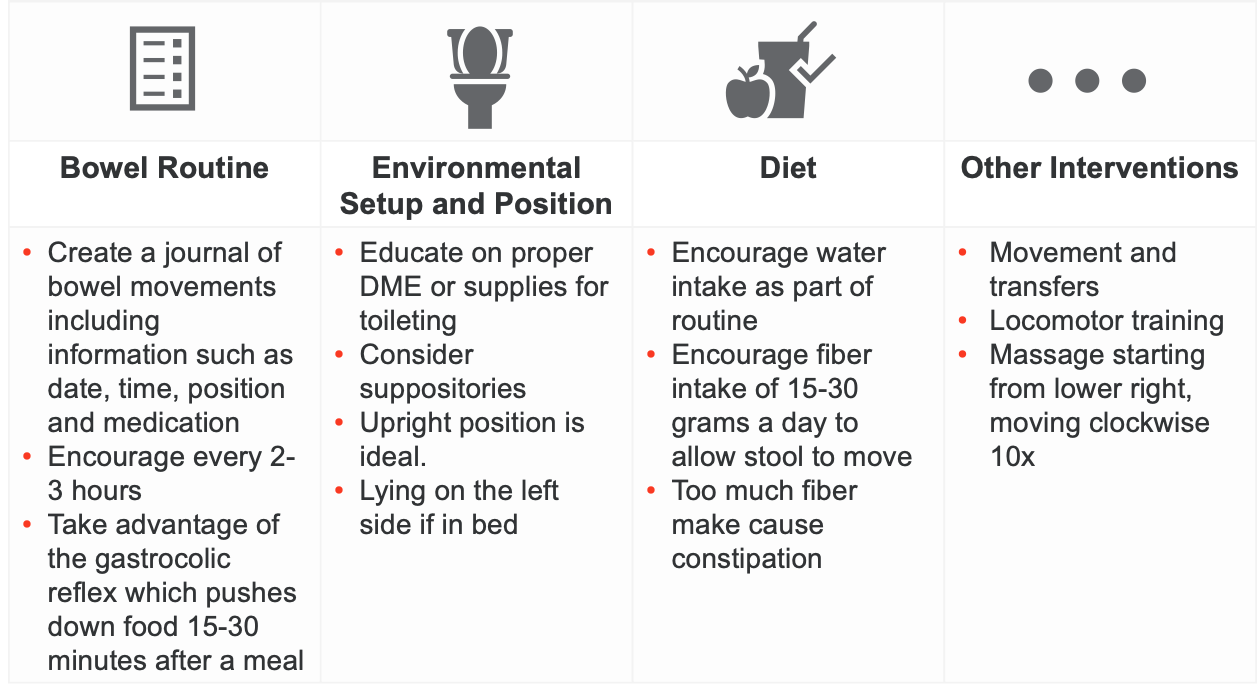
Our second activity of daily living we will discuss is toileting (Figure 5).
Bowel Intervention
(Slocum et al., 2020; Hammond & Burns, 2009; Hubscher et al., 2018)
Figure 5. Toileting considerations (Click here to enlarge the image).
Let's start with bowel interventions. These interventions are generally the same for both females and males. Here are some general strategies you could educate on:
One key intervention is establishing a routine, including keeping a journal. This journal should record the time and day, the positioning used, and any medication facilitating bowel movement. Encouraging attempts to go to the bathroom every two to three hours is also important. For those with neurogenic bowel movements, particularly injuries at T12 and below, individuals may need physical assistance to retrieve the bowels. It's crucial to remember that injuries at T12 and below often require this extra assistance. Taking advantage of the gastrocolic reflex, which occurs 15 to 30 minutes after eating, can also be beneficial.
Other areas of intervention include proper positioning recommendations and durable medical equipment (DME) setups. For example, besides a bedside commode or drop-arm commode, you can educate on using bidets to assist with toileting. Upright positioning is usually encouraged for bowel movements because gravity aids the process. For individuals struggling with constipation or obstipation, considering medications or suppositories can facilitate bowel movements. For those without trunk control, lying on the left side can promote digestion and aid bowel movements.
Regarding diet, it is important to encourage healthy habits such as adequate water intake and appropriate fiber intake (15 to 30 grams a day). However, be mindful of not consuming too much fiber, as it can lead to constipation.
You can also educate on functional movement and safe transfer techniques for spinal cord injury. Locomotor training, which involves using a harness and treadmill to walk, is often handled by physical therapy and has been shown to significantly help bowel movements.
Lastly, a specific type of manual therapy or massage can be beneficial. This involves starting from the lower right-hand side, working your way up to the upper right-hand side, then to the left, and finally down to the bottom left in a circular motion. This massage technique can aid in promoting bowel movements.
Urine Output/Catheterization
(Slocum et al., 2020; Teplitsky et al., 2019; Hubscher et al., 2018, Hammond & Burns, 2009; Linsenmeyer & Kirshblum, 2015)
Figure 6. Catheterization considerations (Click here to enlarge the image).
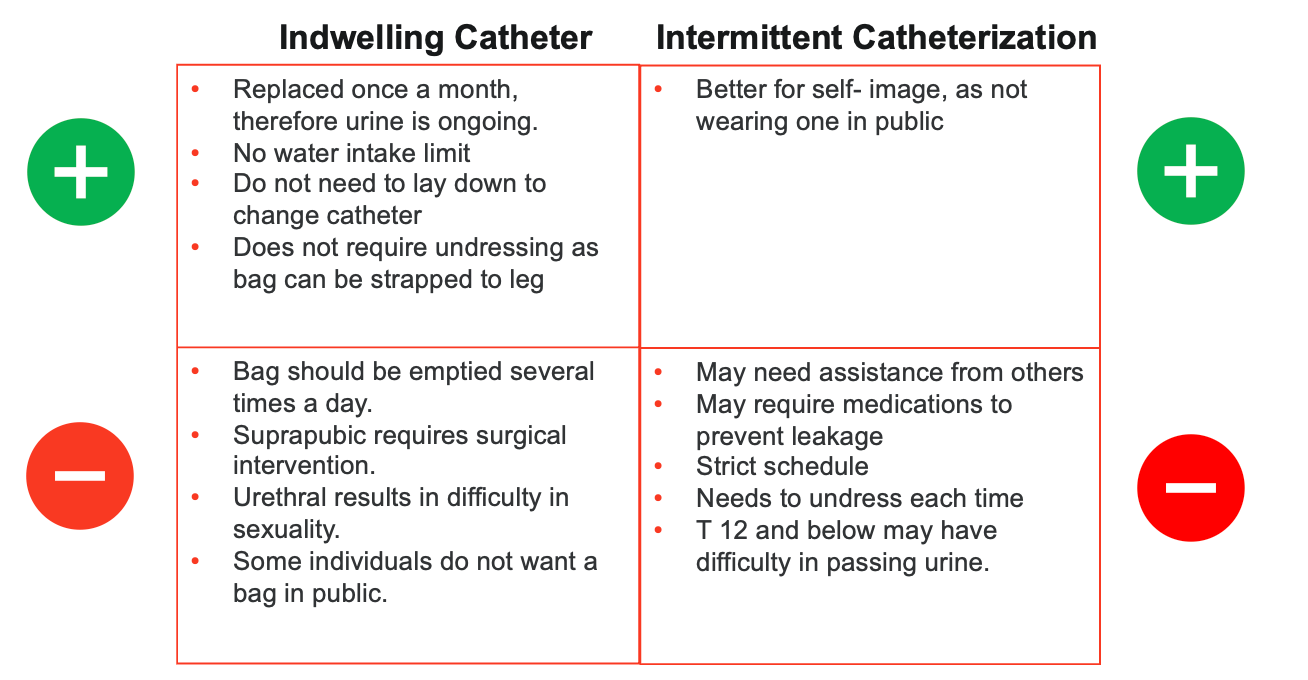
This is where there will be a complete difference between male and female urinary management options. It's possible to use either an indwelling catheter or intermittent catheterization, each with its own benefits and drawbacks. Let's explore the different options, their side effects, and their pros and cons.
Starting with an indwelling catheter, often called a continuous catheter or Foley catheter, has several advantages. One major benefit is that it can be replaced once a month, providing continuous urine drainage. This means there is no need to limit water intake because of an ongoing urine flow. You don't need to stop and sit on a toilet or commode to empty the bladder; instead, the catheter bag can be emptied at your convenience. Additionally, it doesn't require undressing and dressing, making it more convenient and fast-paced.
However, there are some cons associated with indwelling catheters. For example, the suprapubic approach, which involves a surgical procedure to insert the catheter above the pubic area, can lead to complications like autonomic dysreflexia or changes in medical status. Surgical interventions are generally recommended only when medically necessary to avoid these adverse side effects. The urethral approach, which involves insertion through the urethra, can impair sexual intercourse and activity. Some individuals feel self-conscious about having a catheter in public, impacting their self-esteem and self-image. Additionally, the catheter bag must be emptied several times daily, which can be inconvenient.
Now, let's discuss intermittent catheterization, which also has pros and cons. The primary advantage is that it does not involve a permanent tube, so there is less impact on body image and self-esteem. It also allows for more natural bladder emptying and can reduce the risk of some infections compared to continuous catheterization.
However, intermittent catheterization requires regular attention and planning. You need to catheterize several times a day, which can be disruptive and time-consuming. It also requires access to a clean environment each time to reduce the risk of infection. For women, this can sometimes be more challenging due to anatomical differences and potential difficulties with positioning.
Both options have their place depending on individual needs and circumstances, and it's important to weigh these pros and cons when deciding on the best approach for urinary management after a spinal cord injury.
Intermittent Catheterization
- Complete hand hygiene and clean genital area from top to bottom
- Lubricate catheter and place the other end over basin or toilet
- Spread labia and find urethra
- Gently insert until urine comes out. When urine starts to come out, cease insertion
- When urine flows, slowly remove
- Wash hands and clean catheter and environment
(St Lukes, 2023)
Moving into intermittent catheterization, one of the biggest advantages is the improved self-image, as individuals do not have to wear a catheter in public. However, this method often requires assistance, especially if the patient lacks fine motor skills, which is why intermittent catheterization is usually not recommended for individuals with cervical-level injuries.
Patients choosing this approach may need certain medications, such as Botox, to prevent leakage. They must follow a strict schedule, typically every two to four hours, and may be cautious about drinking water to avoid frequent bathroom trips. Each time they go to the bathroom, they need the appropriate assistive devices, such as a commode, toilet, or basin, along with the necessary tools for the procedure. This can be less convenient than simply switching out a bag.
Individuals with injuries below T12 may have an areflexic bladder, making it difficult to pass urine. Intermittent catheterization is generally not recommended for those at C6 and above. The procedure requires thorough hand hygiene and cleaning of the genital area, usually from top to bottom. The catheter, which looks like a small stick with a spout at the end, must be lubricated. The patient or caregiver will spread the labia, locate the urethra, and slowly insert the catheter until urine starts to flow. Once urine begins to flow, the catheter is slowly removed.
Proper hand hygiene before and after the procedure is crucial. Catheters can be costly, and insurance coverage may vary. The more hygienic approach is to dispose of the catheter afterward, but some people may clean and reuse it. If choosing to clean and reuse, it is imperative to clean it thoroughly, ensure it is dry, and store it in a closed container to prevent bacteria growth. Improper cleaning can lead to UTIs.
Women with spinal cord injuries are at a higher risk for developing UTIs compared to males, making it essential to follow proper hygiene and catheterization procedures to minimize this risk.
UTI Prevention Strategies
- Replace catheter when halfway full
- Intermittent catheterization every 2-4 hours
- Avoid catheter touching floor
- Change clothing with leakage
- Appropriate water intake
(Klebine & Kirksey, 2017)
Here are some UTI prevention strategies to keep in mind. One important strategy is to replace the catheter when it is halfway full. Often, I've seen patients with catheters that look like balloons because they are completely full, which is not ideal. The catheter should be emptied and cleaned when it is halfway full. For those using intermittent catheterization, it's crucial to maintain a routine of catheterization every two to four hours. Ensure the catheter does not touch the floor, change clothing and underwear whenever leakage occurs, maintain appropriate water intake, and practice proper hygiene.
Signs and symptoms of a UTI can vary from person to person. They may include fever, increased fatigue, nausea, dark and cloudy urine, headaches, back pain (for those still with some sensation), mucus in the urine, and autonomic dysreflexia for those with T6 injuries and above. In my personal experience, women with spinal cord injuries above the age of 60 often exhibit changes in mental status, appearing excessively confused and not mentally their usual selves.
Menstruation
- Amenorrhea - The lack of menstruation is common post-SCI.
- Return of menstruation averages between 3 months to 1 year.
- Changes can also include reduced duration and flow.
(Charls et al., 2022; Wilbur et al., 2019)
In regards to menstruation, it doesn't completely go away after a spinal cord injury. Usually, there is a temporary cessation of menstruation, a condition known as amenorrhea. It typically takes about three months to one year for menstruation to return. Once it resumes, many women report changes in flow, duration, and overall differences compared to their pre-injury menstrual cycles. These changes can also be influenced by whether the woman chooses contraception.
Menstruation Hygiene
Menstrual Pads
•Better for individuals with poor fine motor skills (Cervical levels) •Higher chances of skin breakdown •Less hygienic, higher risk of UTI
| Tampons
•Better for skin integrity •Cleaner with catheterization •Lower chances of UTI •Frequent changing •Difficult with patients that have fine motor limitation (can use the TINA device) •Can be placed wrong due to lack of sensation
|
(Charls et al., 2022; Hough et al., 2020)
Regarding menstrual hygiene for individuals with spinal cord injuries, there are several options to consider.
Menstrual pads are most commonly recommended for individuals with cervical-level injuries due to limitations in fine motor skills. However, pads can lead to skin breakdown because of friction and rubbing, and they tend to be messier and less hygienic than tampons. This increased messiness can elevate the risk of developing a UTI when using menstrual pads.
Tampons, though preferred by many for their cleanliness and better skin integrity, can be difficult to place for individuals with fine motor skill limitations. Assistive devices such as tampon inserter applicators can help with this. Tampons are advantageous because they keep the menstrual flow contained within the vaginal area, separate from the urethra, where a catheter might be placed. This separation can help maintain hygiene during catheterization. However, tampons require more frequent changing than pads. For those with a lack of sensation, placing a tampon correctly can be challenging, so they may need assistance or use a mirror to check placement.
The menstrual cup is another option that has gained popularity in recent years. However, it is usually not recommended for individuals with spinal cord injuries. The cup's insertion angle can increase the risk of urinary spillage, adding to the messiness and hygiene concerns associated with menstruation and urine leakage.
In addition to these options, using either diapers or menstrual underwear/panties is highly recommended. These look like normal underwear but are made from material that absorbs leakage. They can be less embarrassing than using a diaper and provide additional protection against leaks.
Each method has pros and cons, and the choice will depend on the individual's abilities, preferences, and specific needs. Encouraging proper hygiene practices and frequent product changes is essential to minimize the risk of infections and maintain comfort.
Part VI: Psychosocial Considerations
As we move into our last occupation, which will be health management due to psychosocial concerns, we're going to discuss some of the considerations that happen.
Psychological Considerations
Common psychosocial considerations post-injury
•Depression •Anxiety •Decreased body image •Decreased self-esteem
| Interventions
•Mindfulness education •Therapeutic exercise •Group facilitation •Routine management •Self-regulation
|
(Robinson-Whelen et al., 2014; Kunze & Palmer, 2020)
Some of the most common psychosocial considerations post-injury include depression, anxiety, decreased body image, and reduced self-esteem. As occupational therapists, we can provide several interventions to address these issues.
Mindfulness education can be highly beneficial, incorporating activities like seated yoga, grounding exercises, journaling, mood identification, and tracking. Encouraging therapeutic listening is also important. In my experience, the ORS approach has been particularly effective. ORS stands for open-ended questions, affirming what the patient is telling me, reflective listening, and summarizing at the end of the session. This approach fosters effective communication and builds a strong rapport with patients.
Additionally, encouraging journaling can help patients track their moods, identify triggers, and note what strategies help them improve their mood. It's helpful to record the time of day, the situation, and the specific interventions used.
As OTPs, we should also promote group facilitation through group exercises or meetings with others in similar situations to build a sense of community. Encouraging healthy habits and routine management is crucial. This includes promoting regular exercise to prevent skin integrity issues and breakdown, especially if the patient is pregnant or experiencing weight gain.
Domestic Violence
39% of women with disabilities experience violence. The most common SCI injury from abuse is in the upper lumbar level due to gun violence. | ||
Sexual
•Forces sex/assault •Makes client dress in sexual way •Makes client feel that they owe them sex
| Physical
•Abandons client in places •Attacks with weapons •Keeps clients from eating, sleeping, or getting care •Punches/bites | Emotional
•Criticism •Making threats •Yelling •Throwing items •Telling client what to wear
|
(Hough et al., 2020; Watane et al., 2021; AOTA, 2017)
It's crucial to discuss domestic violence, especially since females with spinal cord injuries are at higher risk. In younger age groups, some patients obtain their spinal cord injury due to violence from their partner. In general, about 39% of women with disabilities experience some form of violence or abuse. When it comes to spinal cord injuries caused by abuse, the most common site is the upper lumbar levels, often resulting from gun violence, firearm violence, or direct physical trauma such as being kicked by a partner.
As practitioners, it's important to recognize the signs and symptoms of abuse, which can take various forms: sexual, physical, and emotional.
Sexual abuse includes assault, non-consensual engagement, making a patient dress provocatively, or making them feel obligated to have sex. I once had a patient with a C6 level injury who felt obligated by their partner to engage in sex, leading to repeated hospital visits for UTIs. This case highlights the importance of being aware of and sensitive to these issues. Each state has different protocols for handling such situations, so it's important to use therapeutic listening and follow local guidelines.
Physical abuse can manifest as hitting, biting, or other injuries, but it also includes depriving the patient of basic needs such as hygiene, proper nutrition, medical attention, and abandonment in situations where they feel helpless.
Emotional abuse includes criticism, yelling, throwing things, and exerting control over the patient's actions or appearance in a way that induces fear and insecurity.
As OT practitioners, according to AOTA, we can identify and assess injuries and evaluate the patient's demeanor to determine if they are experiencing abuse. We can educate patients about local domestic violence shelters and hotlines. It's crucial to provide support and resources to those who may be experiencing abuse, ensuring they know they have options and are not alone.
Case Study
- A 28-year-old female was admitted to a level I trauma hospital. She presents with a complete SCI at the L2 level secondary to an altercation with her former significant other. Both physical and occupational therapy have been consulted, and she has received PT and OT for 3 weeks. Throughout her admission, she has been highly distraught. During one session with the OTR, the patient reports, “My ex did this to me, and now I will never have a real life. No guy will like me, I can’t move well or do anything. I can’t even have kids since I am going to be in a wheelchair. Who will ever want to be with me?”
- What are some barriers the patient is experiencing?
- What are some interventions or education the OTR can provide this time?
In this case study, a 28-year-old female was admitted to a level one trauma hospital with a complete spinal cord injury at the L2 level, resulting from an altercation with her former significant other. Both physical and occupational therapy have been consulted, and she has received PT and OT for three weeks. Throughout her admission, she has been highly distraught. During one session with the OTR, the patient reported, "My ex did this to me, and now I will never have a real life. No guy will like me. I can't move well or do anything. I can't even have kids since I'm going to be in a wheelchair. Who will ever want to be with me?"
The barriers the patient is experiencing include her emotional distress and trauma, decreased self-esteem and body image, misconceptions about her prognosis, and anxiety about not meeting expected roles. She discussed her limitations in mobility, her self-esteem, and overall feeling like she has no purpose. Misconceptions about her ability to have children and her overall prognosis are significant barriers.
Some interventions the OTR can provide include therapeutic listening and emotional support. The ORS approach, which involves open-ended questions, reflective listening, and summarizing at the end of the session, helps build and foster effective communication. This approach can validate her feelings and reassure her that her emotions are understandable.
Education on the possibility of having children and maintaining relationships is crucial. Referring her to a specialized OB-GYN who deals with high-risk pregnancies and SCI patients can help address her concerns about having children. Discussing the possibility of maintaining and building new relationships and emphasizing that many people with SCI have fulfilling relationships and families can provide her hope and reassurance.
Group therapy and peer support are essential. Encouraging her to participate in support groups for individuals with SCI can provide a sense of community and shared experiences. Connecting her with role models or mentors who have successfully navigated life after SCI can also be beneficial.
Self-esteem and body image workshops can help her develop a positive self-image. Referring her to a counselor or psychologist specializing in body image and self-esteem issues and introducing mindfulness practices such as seated yoga, grounding exercises, and journaling can support her emotional well-being.
Education on mobility and independence is crucial. Providing education on assistive devices and adaptive techniques that can enhance her independence in daily activities can build her confidence. Incorporating skill-building activities can help her manage daily tasks and participate in meaningful occupations.
Health and wellness education is also important. Educating her on maintaining a routine for bladder and bowel management, skincare, and overall health can prevent complications. Offering advice on healthy eating habits that support her well-being and prevent secondary conditions can also be beneficial.
Addressing her misconceptions through realistic goal setting and providing educational resources about SCI, including success stories and advances in rehabilitation and assistive technology, can help her develop a more positive outlook on her future. These interventions and education can empower her to lead a fulfilling life despite her injury.
Summary
As I wrap up, I hope we have met all the learning outcomes. Now, we are going to test some of the things we learned.
Exam Poll
1)According to the SCI demographics,
Twenty percent of the SCI population are women. That is a small number and why there is limited information on how to address spinal cord injuries among the female population.
2)What is a client factor or barrier to sexuality for those with an SCI?
The correct answer is all of the above.
3)For contraception, which is a TRUE statement for those with an SCI?
The correct answer is that oral contraception should be avoided when you're post-injury.
4)What is an issue noted in the first trimester of pregnancy for those with SCI?
All of the above is the correct answer.
5)Which of the following is NOT a UTI prevention strategy?
The correct answer is A. You do not want to wait until the catheter is all the way full.
References
Please see the attached handout.
Citation
Rivera. N. (2024). Occupational therapy practitioner's role in helping women live fulfilling lives after spinal cord injury. OccupationalTherapy.com, Article 5710. Available at www.occupationaltherapy.com.
