Introduction
This is an area that is very personal to me as I live with chronic pain. I have arthritis and have been diagnosed with fibromyalgia. I do not always believe it. I also have a kidney condition that causes me to produce kidney stones, which obviously causes chronic pain.
The CDC Limited Access to Opioid Pain Meds
- CDC Guideline for Prescribing Opioids for Chronic Pain (2016). Bottom Line:
- Key Points for Practice:
- “Chronic pain should be managed primarily with nonpharmacologic therapy or with medications other than opioids.
- Physicians should routinely discuss the risks and benefits of therapy and the mutual responsibility to mitigate risk with patients who are receiving opioids.
- When opioids are prescribed, they should be titrated to the lowest effective dosage.
- Treatment should be offered or arranged for patients with opioid use disorder.”
- Key Points for Practice:
(Bredemeyer, 2016)
In 2016, the CDC issued guidelines that limit access to opioid pain meds. I do not have a slide on this, but in 2014, they recategorized hydrocodone. As a result, all of a sudden, people did not have their pain meds. This is because not all doctors were licensed to give that level of pain medication. The other thing with hydrocodone is that it required a different way of storing and distributing it.
A quote from the National Fibromyalgia and Chronic Pain Association study stated, "This makes a legitimate chronic pain sufferer feel as though they're criminals. And all we want is to live life pain-free and be our normal selves again without being treated like pill addicts."
After that, the CDC changed the way they looked at all opioids. The key points for practice are that 1)chronic pain should be managed primarily with non-pharmacological therapy or medications other than opioids. It sounds like they are talking about OT a little bit here. 2)Physicians should routinely discuss the risks and benefits of therapy and the mutual responsibility to mitigate the risks with patients who are receiving opioids. 3)When opioids are prescribed, they should be titrated to the lowest effective dose, and 4)treatment should be offered or arranged for patients with opioid use disorder. I have to point out that opioid use disorder became the term for people who take opioids regularly. If you have chronic pain and need opioids, why is it called opioid use disorder? I am involved in several consensus panels and studies looking at older adults with opioid use disorder. People used to take opioids when they were in pain. However, now, if you use them, you have an opioid use disorder. The bottom line is that they are trying to get everybody off of opioids.
Impact of Limited Access to Pain Medication
- People with legitimate pain conditions can’t get medications for their pain.
- This may affect their participation and occupational performance
- Patients will not perform well if they are in pain
- Pain may further limit them - physically as well as psychologically
- May be referred to Occupational Therapy because of pain
- This opens the door to a whole area of practice for Occupational Therapy that we need to market to physicians
When people with legitimate pain conditions can not get medications, this may affect their participation and occupational performance. Patients will not perform well if they are in pain, and pain may further limit them physically and psychologically. They may be referred to occupational therapy because of pain. This opens the door to a whole area of practice for occupational therapists that we need to market to physicians. It has been four to five years since they rescheduled hydrocodone, and I have not really seen an uptick in occupational therapists treating pain. We need to promote that.
Occupational Therapy Roles in Chronic Pain Management
- A Canadian Scoping Review (52 sources) found OT’s roles as:
- Activities and Participation:
- Enabling occupational engagement
- Addressing occupational performance
- Providing vocation rehabilitation
- Promoting participation
- Promoting functional independence, mobility, and autonomy
- Addressing occupational balance
- Restoring occupational identity
- Limiting occupational injustice
- Body functions and structures:
- Improving/Restoring function
- Improving body mechanics and activity tolerance
- Environmental factors
- Modifying the nonhuman environment and ergonomic approach
- Enhancing social support
- Activities and Participation:
(Lagueux, Depelteau, & Masse, 2018)
A Canadian scoping review looked at what is out there about occupational therapy roles in chronic pain management. A scoping review does not analyze it or look at the best evidence, but rather it looks at what evidence is out there. It is a little different from a systematic review. This scoping review found were three things. For OT's role is in activities and participation, it showed that we enable occupational engagement. We address occupational performance. and provide some vocational rehabilitation. We help people go back to work by changing how they do their jobs and giving them other ways to do things, so it does not hurt. We promote participation in all kinds of things and facilitate functional independence, mobility, and autonomy. We address occupational balance and restore occupational identity. We also limit occupational injustice. Occupational injustice could be participating in some occupations like work or daily activities while in pain. If you have to do it, that would be considered occupational injustice.
Body functions/structures is another area. We improve and restore function. We improve body mechanics and activity tolerance. We encourage people to do things a different way. This is a classic one that most of us are taught in school.
We also modify the non-human environment and use an ergonomic approach. We also want to enhance social support. There are many roles for occupational therapy, and we have not just been taught to think about pain within this framework.
- Results pointed to the main role of OT being improving activities and participation (76.9 %).
- Within the 30 reported interventions,
- 73.3% related directly to the person,
- 20% pertained to occupation (activities and participation), and
- 6.7% addressed environmental factors.
- Conclusion: As an expert in enabling occupation, occupational therapists are particularly interested in how individuals living with Chronic Pain can perform and engage in their daily occupations….with a better emphasis on occupation as an end and as a means.
The results of this scoping review pointed to the main role of occupational therapy as improving activities and participation. With the 30 reported interventions, 73.3% related directly to the person, maybe body mechanics or changing how people do things. Twenty percent pertained to occupation, activities, and participation, and 6.7% addressed environmental factors. The conclusion was that, as an expert in enabling occupation, occupational therapists are particularly interested in how individuals living with chronic pain can perform and engage in their daily occupations with a better emphasis on occupation as an end and as a means. This means that occupation can be used as a form of pain management. This is how they do their occupations and what they accomplish.
Pain Interference
- Study of ”Pain Interference” defined as “a construct of the self-reported consequences of pain on activities and participation,” due to Musculoskeletal Disorders, found among other things:
- “Pain Interference (PI), psychosocial and motor factors were associated with disability.”
- “PI is how pain affects engagement, satisfaction, and meaning of activities.”
- “PI had the strongest association with self-reported disability.”
- “Rehabilitative interventions should address PI to improve disability.”
- “Our results suggest rehabilitation programs need to be tailored to patient's goals and activities including work and social aspects that impact the meaning, satisfaction, and social relationships associated with activities and participation to modify the effects of pain interference.” (Pelletier, R. et al., 2020)
This study defined pain interference as a construct of the self-reported consequence of pain on activities and participation due to musculoskeletal disorder. This is when a musculoskeletal disorder interferes with your ability to function and do your activities and participate in the things you need to do.
They found that pain interference, like psychosocial and motor factors associated with disability, affects engagement, satisfaction, and meaning of the activity. Pain interference is strongly associated with self-reported disability. When people say, "I have a disability," what are they saying? They are saying, "My pain doesn't allow me to do something," and "I can't do this because it hurts."
Rehabilitation intervention should address pain interference to improve disability. How can I do this activity without the pain interfering? What is another way to do it? Pelletier and colleagues said, "Our results suggest rehabilitation programs need to be tailored to patient's goals and activities" (what did the patient want to do, what is their goal) "including work and social aspects that impact the meaning, satisfaction, and social relationships associated with activities and participation to modify the effects of pain interference."
What can we do to work with our clients to modify how pain interferes with their ability to do what they want to do and when they want to do it? Part of my research is the theory of occupational autonomy. My colleagues and I looked at the quality of life of those with pain. This did not look at whether a person got eight hours of sleep at night or ate three meals a day. Quality of life is the ability to do what you want to do when you want to do it. And, pain is something that interferes with quality of life.
What is Pain?
- An unpleasant or noxious feeling
- “Pain is a uniquely individual and subjective experience that depends on a variety of biological, psychological, and social factors, and different population groups experience pain differentially” (IOM, 2011)
Pain is an unpleasant or noxious feeling. The Institute of Medicine (IOM) is now a part of the National Academies of Science, Engineering, and Medicine. When they started the Institute of Medicine, they did not believe that medicine was a science yet. In the last few years, they have agreed that medicine is a science.
They reported on pain in 2011. You can download a free copy if you go to the National Academy of Science, Engineering, and Medicine. You can also buy a hard copy. They said, "Pain is a uniquely individual and subjective experience that depends on a variety of biological, psychological, and social factors, and different population groups experience pain differently." As OTs, I think we see that. People experience pain differently.
Acute Pain
- Normal sensation triggered by the CNS to alert you of something you need to know about (AAPM, n.d.)
- Sudden onset and expected to last a short time.
- Usually related to an illness or injury
- Kidney stone, sunburn, muscle strain
- Usually treated with over-the-counter or short-term stronger meds, i.e., root canal.
- (IOM, 2011)
Acute pain is different from chronic pain. Acute pain is a sensation that is triggered by the central nervous system to alert you of something you need to know about. A classic example is putting your hand on a stove. The stove is hot, and it alerts you to take your hand off of the hot surface.
Acute pain is also sudden onset, and it is expected to last a short time. It is usually related to an illness or injury. I threw kidney stones in here because that is acute pain to which I can relate. Other examples include sunburn and muscle strain.
Acute pain is usually treated with over the counter or short-term, stronger meds. For example, the doctor will give you a few strong pain medications for a root canal.
Recurrent Pain
- Acute pain can be recurrent with episodes of pain and periods without pain.
- Migraines, sickle cell, dysmenorrhea
- (IOM, 2011)
- Migraines, sickle cell, dysmenorrhea
Recurrent pain is acute pain that can have episodes of pain and then periods without pain. Some examples of that are migraines, sickle cell anemia, and dysmenorrhea. Again, this comes from the Institute of Medicine report. They classified pain to make it easier for everybody to understand what they were talking about.
Chronic Pain
- Lasts more than several months (variously defined as 3 to 6 months, but certainly longer than “normal healing”)
- Chronic pain can be a disease in itself.
- Chronic pain has a distinct pathology, causing changes throughout the nervous system that often worsen over time. It has significant psychological and cognitive correlates and can constitute a serious, separate disease entity. (IOM, 2011)
They also defined chronic pain. Chronic pain lasts a long time. It could be three to six months. There are several different definitions, but it is longer than what we would consider normal healing of something. If you cut yourself, you have an expected period of pain. Chronic pain is different.
According to the Institute of Medicine, chronic pain can be a disease in itself. It has a distinct pathological, causing changes throughout the nervous system that often worsens over time. It has significant psychological and cognitive correlates and can constitute a serious and separate disease entity. It can be exacerbated by certain things and cause other psychological problems. Chronic pain can be fatiguing as it really has a significant impact on your ability to function.
Neuropathic Pain
- A type of chronic pain that results from a disease of the peripheral or central nervous system that arises when
- a person’s nerves, spinal cord, or brain is damaged or fails to function properly for any of a large number of reasons. (IOM, 2011)
- All neuropathic pain is associated with poor general health, comparable with other severe chronic diseases.
- It is associated with worse health and quality of life than non-neuropathic pain, and its incidence, prevalence, and impact are likely to increase with the aging population. (Smith & Torrance, 2012)
Neuropathic pain is a type of chronic pain that results from a disease of the peripheral or central nervous system. This arises when your nerves, spinal cord, or brain are damaged or fail to function properly. It could be because you have a spinal cord injury. It could be due to a traumatic brain injury. A peripheral nerve could be cut.
- All neuropathic pain is associated with poor general health, comparable with other severe chronic diseases.
- It is associated with worse health and quality of life than non-neuropathic pain, and its incidence, prevalence, and impact are likely to increase with the aging population. (Smith & Torrance, 2012)
When you have neuropathic pain, you are considered to be in poor health. Neuropathic pain is going to affect your participation in many things. You are not going to exercise as an example. It is going to interfere with many day-to-day activities.
Neuropathic pain is comparable to other severe chronic conditions. It is associated with worse health and quality of life than non-neuropathic pain. The incidence, prevalence, and impact are likely to increase with the aging population. This is because there are different neurological conditions as we age. A stroke, for example, causes neuropathic pain like shoulder-hand syndrome. And as you get older, you are more likely to experience some of those kinds of things. This is going to interfere with your ability to function.
- The cause may be
- an underlying disease process (as in diabetes) or injury (e.g., stroke, spinal cord damage),
- but neuropathic pain may not have an observable cause and can be considered
- maladaptive “in the sense that the pain neither protects nor supports healing and repair” (Costigan et al., 2009, p. 3; IOM, 2011)
The cause of neuropathic pain can be from an underlying disease process, like diabetes, that can cause peripheral neuropathy. However, neuropathic pain may not have an observable cause. It can be considered more maladaptive in the sense that pain neither protects nor supports healing and repair. Often the pain is a warning signal. You do something that hurts, and then you do not do it anymore. We need to be aware of this and let our clients know that this is very normal. "You may have this pain, and other people cannot see it." We can explain to them how neuropathic pain works.
Impact of Pain
- “Pain is a universal experience.” (IOM, 2011)
- Pain affects people of all ages, including children (King et al., 2011)
- Acute & chronic pain affects a lot of Americans, with at least 116 million U.S. adults burdened by chronic pain alone.
- The annual national economic cost associated w/ chronic pain is estimated at $560–635 billion. (IOM, 2011)
What is the impact of pain? The Institute of Medicine said that "Pain is a universal experience." It affects everyone of all ages. Everybody can experience pain. We know that acute and chronic pain affects a lot of Americans, with at least 116 million adults burdened by chronic pain alone. It may be more than that even. I do not think our data is as accurate as it used to be because we used to look at the medications prescribed for chronic pain to get the numbers. We do not do that anymore because we are not prescribing as much. The annual national economic cost is between $560 and $635 billion. That was in 2011. That number has probably gone up a lot. I was not able to find any updated data.
- Chronic pain creates both physical and psychological problems that affect whether a person can engage in meaningful activities each day.
- Pain can decrease a person's strength, coordination, and independence in addition to causing stress that may lead to depression (AOTA, 2002)
Chronic pain creates both physical and psychological problems that affect whether a person can engage in meaningful activities. Physically, you may be concerned that a movement is going to hurt. We all have things in our lives that we do not do because it hurts or we are afraid it is going to hurt. The joke that I tell my rheumatologist is, "It hurts when I do this." He says, "You're an OT. Don't do that. Figure out another way to do it." He is right.
Pain can also decrease your strength because you may restrict specific movements. It can reduce your coordination because you are so concerned about the pain that you may not be able to focus. It can also decrease independence and cause stress that can lead to depression.
When we did the study with the National Fibromyalgia and Chronic Pain Association, we had 3,000 responses within 72 hours when they rescheduled hydrocodone. Within 14 days, we had 5,000 responses. I have never seen a study like that. That was pretty incredible. These people were so angry and frustrated that they responded to this survey as it really affected them. Many of them were depressed. You can imagine that if you live with chronic pain that that is going to cause depression.
Role of Occupational Therapy
What is the role of occupational therapy?
- “All people need to be able or enabled to engage in the occupations of their need and choice, to grow through what they do, and to experience independence or interdependence, equality, participation, security, health, and well-being” (Wilcock & Townsend, 2008, p. 198)
Above is a core belief of occupational therapy. This is what we are aiming for. We want people to be engaged in occupation. And if they are in pain, that is going to be tough.
- Look at how pain affects one’s everyday life and one’s ability to participate in the important everyday tasks of life and one’s occupations
- Structure interventions to facilitate participation in important tasks of life or occupations (AOTA, 2002)
- Finding from a systematic review: Occupational therapy interventions should start from the identified needs of the person with chronic pain. (Hesselstrand, M., Samuelsson, K., & Liedberg, G. 2015).
- A study of veterans with chronic pain who attended an interdisciplinary program for chronic pain “most frequently described adopting new self-care or lifestyle practices for pain management and health.” Veteran participants often described “accepting pain, being better able to adjust and set boundaries, feeling more in control, participating in life….” (Penney S. & Harro E., 2019)
We look at how pain affects everyday life and our ability to participate. What do people want to do? What are their daily occupations? We are supposed to ask our clients that. Based on what they say, we should be structuring our interventions on what they want to do. I told you my theory of occupational autonomy. Quality of life is the ability to do what you want to do when you want to do it. Ask people, 'What do you want to be able to do that you're having trouble doing?" We want to work towards that. That may sound kind of basic or crazy. However, that is what people in pain want, and that is what this study showed.
We take pain meds to function and do what we want to do in our daily lives. When you are working with pain patients, ask them what they want to be able to do. Based on their responses, try and figure out ways to change the way the task is done and how the person is to find that match. How can we do it differently? Is there another way?
The findings from a systematic review show that occupational therapy intervention should start with the identified needs of the person with chronic pain, which is basically what I just said. You need to assess the following. "What do you need? You are coming to me because you are in chronic pain. How is this pain affecting your day-to-day life? How can we intervene and figure out ways to promote how they do things?
A study of veterans with chronic pain, who attended an interdisciplinary program for chronic pain, most frequently described adopting new self-care or lifestyle practices for pain management and health. The veteran participants often described accepting pain, being better able to adjust and set boundaries, and feeling more in control to participate in life. Again, that is what people in pain want. They want more control. They want to be able to have strategies. They want to know how to do things differently.
I remember being in somebody's kitchen, and she said, "Oh, when I reach for this dish above the sink, it hurts. I use this dish every day." This should seem obvious to our OT brain, but it was not obvious to her. I said, "Do you have to keep it above the sink? If it hurts when you get it, why don't you put it somewhere else?" And she said, "Well, I never really thought about that." It was the most obvious thing to me. Some of these things may seem obvious to us. If we do not ask and do not know, we cannot intervene. The interventions are sometimes as simple as moving things around.
- The aim/goal/focus of occupational therapists in pain management is “to enable individuals with chronic pain to participate in the activities that have value and meaning to them, despite their pain.” (Hill at 451)
- Occupational Therapy intervention include using “strategies including activity management, activity adaptation, the development of coping strategies and vocational rehabilitation,” work simplification, pacing, etc. (Hill at 451+)
- This may involve working with patients/clients in their homes, school, or workplace in addition to the clinical setting. (Hill at 451)
- Hill discusses ergonomics, energy conservation, goal setting, assessments, problem-solving, and pacing. This article is an excellent tool to use to promote your pain practice to physicians.
The aim, goal, and focus of OT and pain management are to enable individuals with chronic pain to participate in the activities they value and that have meaning to them despite their pain. What does the patient want to do? How can we enable it? OT intervention includes using strategies including activity management, adaptations, coping strategies, vocational rehab, work simplification, pacing, and all these things. We do not always think about having these capabilities. For example, I am a certified pain educator, but you do not have to be a certified pain educator to do these things. This is in our OT bag of tricks. If something hurts, how can we enable them to do it differently? Is there equipment? Are there strategies? How can we do it? Now, this may involve working with patients in their homes, work, or school in addition to the clinical setting. What causes them pain at work? It may be as simple as moving something on their desk to a different location or moving it to the left side instead of the right.
Hill and colleagues discuss ergonomics, energy conservation, goal-setting, assessments, problem-solving, and pacing. This is a great article to use to promote your pain practice to physicians. It goes into a lot of detail about what we do and how we do it. What we do to intervene with pain is obvious to us, but it is not always obvious to everybody else. Sometimes, it takes some week-long pain conference for you to realize how obvious this is.
- The therapist assesses the individual’s current performance and the barriers to successful participation to plan appropriate intervention. Those barriers will include barriers internal to the individual and those external barriers like those in the social and physical environments in which they need to function.
- The therapist will help the client understand the biopsychosocial nature of their pain and the importance of self-management.
- The therapist will teach techniques that enable the individual to successfully engage in occupation. These techniques can include things like problem-solving, grading activities, education regarding pacing, goal setting, ergonomics, and energy conservation.
- Although their goal may be to return to work/school, it is important that clients understand the effect their activities have on their pain and fatigue and their actions to minimize those effects. (Hill & Macartney, 2019)
Hill's study also said that to plan appropriate intervention, we have to look at people's current performance and barriers. Those barriers can be internal to the person. They may be worried that they are going to be hurt. Or, it could be external. Something may be too high, and they cannot reach it. Or, their chair hurts their back. They may need a different chair. We help clients understand the biopsychosocial nature of the pain and the importance of self-management. What do I need to do? How can I take charge as a patient and do things differently to eliminate my pain? They have to start thinking that way.
We obviously teach techniques that enable clients to engage successfully in occupation. This could be using problem-solving, grading activities, or educating people about pacing, goal-setting, ergonomics, and energy conservation. You are going to see more of all of these things from the other lectures this week. Although the goal may be returning to work or school, clients need to understand how activities can affect their pain and fatigue and minimize them. For one example, they can use pacing and do a little bit at a time. I run support groups for the National Fibromyalgia and Chronic Pain Association. I had someone come on once and say, "Ugh, every Monday, I do four loads of laundry, and on Tuesday, I'm in bed all day." And I said to her, "Why don't you do one load of laundry a day so then you won't be in bed on Tuesday?" She said, "Wow, why did I not think of that?" I was using my OT skills. I ended up doing a whole article for the National Fibromyalgia and Chronic Pain's website on how to do laundry. As crazy as it is, you do not have to put all the laundry in the basket, lift, and carry it. If it is heavy, it will hurt your back. I went into detail about how to do that differently.
Impact of Pain on Everyday Life Activities
- A person is unable to perform specific activities – self-care, work, leisure
- Results in loss of independence in various roles
- May have both physical and psychological problems
Pain can impact everyday life. People are unable to perform specific activities, complete self-care, work, or participate in leisure interests. It can result in a loss of independence, and it may have both physical and psychological ramifications. I am sure you see those. I described some of those to you. The example of the four loads of laundry all at once put my client in bed the next day. It is obvious to me to break that down because I am an OT, and I think that way. You may also be thinking that this is obvious. However, it is not obvious to people that we see who are in chronic pain. If you have a routine, and suddenly, it is causing you pain, we need to change that.
Occupational Therapy Evaluation
- Occupational Therapists look at the:
- Person
- Environment - Context
- Occupation or Task (Law, et al. 1996)
- A qualitative study of occupational therapists who treat clients with pain found that activities of daily living, social participation, and meaningful activities were the areas they found their clients reported as the most limited by pain.
(Lucio, Laney, Lake, Kornblau, & Mbiza, 2018)
We look at the person, environment and context, and the occupation or tasks during an evaluation. In 2018, I completed a qualitative study of occupational therapists who treated clients with pain with my students. We found that activities of daily living, social participation, and meaningful activities were the areas that clients reported as most limited by pain.
Person
- Occupational Profile
- Understand the client’s history, prior level of function, experiences, patterns of living, interests, values, and needs
- Look at a person’s roles – i.e., mother, worker, student, caretaker, etc.
- Occupational Performance Analysis
- Looks at problems in task performance skills and underlying body functions/structures which limit occupational performance
We evaluate people and complete an occupational profile to understand the client's history, prior level of functioning, experiences, and living patterns. We do all of these things to find out information about their pain and how their occupational profile may have changed. Are they not doing the things they used to do? We are looking at their roles as people, mothers, fathers, workers, students, and caretakers.
We also analyze occupational performance and look at any task function problems, skills, and underlying body function structures. What is limiting their occupational performance? When we find that out, how can we get around that? Can we do it a different way?
Environment-Occupation
- Context
- What are the person’s occupations?
We then look at occupation and context. What are the person's occupations? What do they do? What do they want to do? What did they use to do before the pain set in? And, how can we adapt that so that they can do it again?
Assessment Tools
- Interviews – structured and unstructured
- Observations of task performance
- Informal and formal testing
- Pain scales
- Environmental assessments
We can use various assessment tools to gauge pain. We can use interviews, structured and unstructured. We can also observe task performance. There are also both informal and formal testing. It may be assessing their range of motion. It may be just touching to see where the pain is. Where does it hurt? There are various pain scales out there that measure pain and environmental assessments to look at how people are doing in their environment. They can look at how the environment impacts their pain. Figure 1 shows an example of a universal pain assessment tool.
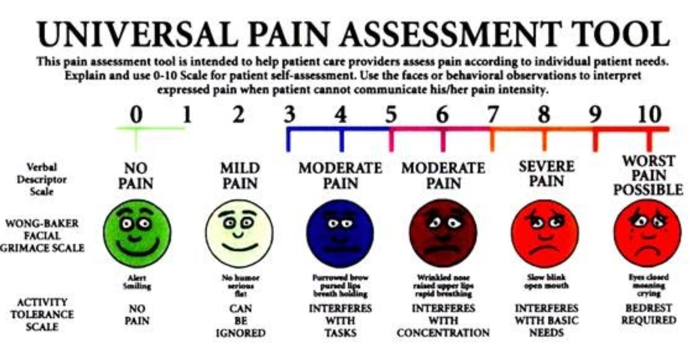
Figure 1. Universal Pain Assessment Tool.
You can find this online. You can also ask people to rate their pain. After an intervention, you can rate their pain again to see if and how it may help them. It gives people something to relate to and understand what their pain is and how you are assessing it.
Interventions and Approaches
- Interventions
- Person – “change the person”
- Environment – “change the environment”
- Occupation – “change the way the task is done”
- Intervention Approaches
- Health promotion
- Remediation and restoration
- Maintain
- Teach compensatory techniques or adaptation
- Prevent further disability
(AOTA, 2014)
Person
- A person learns new ways of doing things – e.g., use proper body mechanics, ergonomic principles, pacing, assertiveness, relaxation techniques. Research shows:
- Body Mechanics:
- the efficacy of instructions on body mechanics was significant during work-hardening treatment; (Hesselstrand, Samuelsson, & Liedberg, 2015).
- Pacing: by itself is not a panacea:
- “The current evidence supports the use of pacing as a tailored intervention for adults with chronic pain to reduce the interference of fatigue, reduce joint stiffness, and decrease variability in physical activity.”
- “The current evidence does not support the use of pacing as a learned strategy to reduce pain or influence psychological traits.”
- “The evidence is not sufficient to determine whether pacing can improve a person’s average activity level, participation in life roles, participation in social functioning, or reduction in fatigue severity.” (Guy, McKinstry, & Bruce, 2019).
- Body Mechanics:
We can change the person, the environment, or the way the task is done for interventions. That is OT. When looking at pain, we do the same thing. We have to look at what is causing the pain and how it affects the person, the environment, and health promotion through remediation and restoration. We may want to maintain someone's ability to do something. We can teach compensatory techniques or adaptation, and we can prevent further disability. These are our roles and approaches. The person can do new ways of doing things. We can instruct on proper body mechanics, ergonomic principles, pacing, assertiveness, and relaxation. I keep mentioning the same things, but I really want to get that across. Other people are going to be going into detail on some of these things this week.
In the study by Hesselstrand, Samuelsson, and Liedberg (2015), they found that the efficacy of instruction on body mechanics was significant during work-hardening treatment. Pacing by itself, according to Guy, McKinstry, and Bruce, was not a panacea. Current evidence supports pacing as a tailored intervention for adults with chronic pain to reduce interference of fatigue, joint stiffness, and variability of physical activity. It does not support pacing as a learned strategy to reduce pain or influence psychological traits. The evidence is also not sufficient to determine whether it improves a person's activity level, participation, or social function. It is worth trying, but the evidence is iffy.
- Person incorporates new ways of “doing” into routine and/or habit
- Person restructures daily activities to provide a balance of activity and rest
- Person’s perception of disability changes through engagement in occupations
For the person, we can incorporate new ways of doing things. The person restructures daily activities to provide a balance of activity and rest. Lastly, the person's perception of disability changes through engagement in occupations.
Environment-Context
- Modify/rearrange furniture or equipment
- Modify social situations to facilitate participation
- Modify cultural expectations/behaviors
- Modify temporal aspects
The environment and context can also be assessed. We may modify and rearrange furniture or equipment. We can modify social situations to facilitate participation. We can modify cultural expectations, behaviors, and temporal aspects. Somebody may have issues in certain social conditions. They may need to sit down instead of standing. Maybe, everybody else also needs to sit down instead of standing. We can also reorganize the room. Perhaps, an activity is hurting more because they are doing it at the end of the day. We may need to reorganize things, so it is not done at the end of the day. We look at the context and ask, "Where's your pain? Where's it coming from? What time of day is it? And can we do it a different way or at a different time?"
Occupation
- Use of tools, adaptive equipment, and/or assistive devices to make it easier to participate in meaningful occupations
- Change type of materials used
- Modify timing or sequence of occupation/task
- Eliminate steps in a task
- Change the way occupations are performed
- i.e., put things on wheels
- Use meaningful occupation to improve health
- Lifestyle redesign
We know that clients can use tools, adaptive equipment, and assistive devices to make it easier to participate in meaningful occupations. We sometimes change what we are using to participate. We modify the time. We eliminate steps or change the way we do it. My favorite one is putting things on wheels. Why do you have to carry the laundry when you can put it on wheels? We want to use meaningful occupation to improve health. What is meaningful to that person? Can we find occupations that do not cause them pain? Can we have them do their occupations differently because it is important to them? It may be necessary for the person to do laundry or walk their dog. Lifestyle Redesign is another one. I am going to mention that because somebody else is doing a whole presentation on that this week. Lifestyle Redesign is a wonderful way to change how you do things and decrease pain.
Outcomes of Occupational Therapy
- Occupational performance
- Improvement or enhancement
- Adaptation
- Health and Wellness – occupational balance
- Participation
- “Achieving health, well-being, and participation in life through engagement in occupation is the overarching statement that describes …occupational therapy in its fullest sense” (AOTA,2014)
What are the outcomes of occupational therapy? We hope to improve or enhance occupational performance. We want people to be able to do things and have occupational balance. We want to balance health and wellness and improve pain-free participation. People want to participate in things that do not hurt.
AOTA defines participation as achieving health, wellbeing, and participation in life through engagement in occupations. This overarching statement describes occupational therapy in its fullest sense. I like to say that we give people their lives back. We look at what they want to do, and we figure out ways for them to do it. And in the context of pain, we figure out ways for them to do activities with as little pain as possible. We take a different approach to it, and we find a better way to do something.
- Prevention
- Quality of life – “occupational autonomy”
- Role Competence –
- “The ability to effectively meet the demands of roles in which the client engages.”
- Self-advocacy (AOTA, 2014)
We also want to prevent pain. I mentioned my theory on quality of life and the idea of occupational autonomy. We want people to do the things they want to do, when they want to do them, without pain or with decreased pain. Role competence is the ability to effectively meet the demands of roles in which the client engages. What are the person's roles? How can we facilitate participation in those roles with as little pain as possible? Self-advocacy is an important factor because if someone is doing something, and it causes them pain, we want them to advocate for themselves to be able to do it without pain. For example, if they are doing something at work while standing, but would rather sit to decrease the pain, they should advocate for themselves and explain why they need that.
- Occupational Therapy can teach people with chronic pain to learn to manage their pain's physical and psychological effects and lead active and productive lives.
- Medication, surgery, heat, cold, nerve stimulation, and massage are not enough.
- What they need to learn is
- How to manage daily activities and
- Change their lifestyle to successfully cope with long-term pain (AOTA, 2002).
In occupational therapy, we can teach people with chronic pain to learn to manage physical and psychological pain. The bottom line is that we can help people manage this stuff. Medication, surgery, or massage may not be enough because they need to perform everyday activities. They need to learn how to manage their daily activities and to change their lifestyle to cope with long-term pain. What can we do to decrease that?
- Identify specific activities or behaviors that aggravate pain, and suggest alternatives activities or ways to perform them.
- Teach methods to decrease the frequency and duration of painful episodes.
- Implement therapy interventions that may decrease dependence on or use of pain medications.
What can OTs do? We can identify the activities that aggravate pain and change the way they do them. We can teach people methods to decrease the frequency and duration of painful episodes. And we can implement interventions that may reduce dependence on the use of pain medication. Most clients are not going to be getting opioid pain medication because the physicians have stopped prescribing that. They stopped teaching it in medical schools. Pain medication may be limited to things like aspirin.
- May include
- Relaxation techniques
- Guided imagery
- Yoga
- “The results of our study shows 8-weeks of group yoga sessions contributed to improvements in multiple occupation-based out-comes in people who are living with chronic pain.” (Schmid et al., 2019)
- Biofeedback
- Mindfulness
- “Utilizing mindfulness techniques allowed for more responsive approaches to pain management and a conscious choice about whether or not to engage with the experience of pain within the occupational performance.” (Goodman et al. 2019)
We can do things like relaxation techniques, guided imagery, and yoga. A study showed that eight weeks of group yoga sessions improved multiple occupation-based outcomes in people living with chronic pain. Mindfulness also allowed for more responsive approaches to pain management and a conscious choice about whether or not to engage with the experience of pain within occupational performance.
- Facilitate the development of better function for daily activities at work and home.
- Collaborate with the client’s team of health care professionals, such as physicians, physical therapists, psychiatrists, and psychologists, to determine the best course of treatment and intervention.
- Recommend and teach clients how to use adaptive equipment to decrease pain while performing tasks, such as reaching, dressing, bathing, and perform household chores.
We can also facilitate the development of better function for daily activities. We can collaborate with the health care team to determine the best treatment and intervention course or recommend how to use adaptive equipment to decrease pain. It is amazing how much pain can be reduced by using a reacher. That might be obvious, but it works.
Case Studies
Case Study- Valerie
- Valerie is a 35 y/o woman with Lichen Sclerosis.
- She has burning and itching in the anogenital area.
- She is referred to occupational therapy because she is no longer able to participate in her normal occupations.
- In particular, she can no longer ride her bike - her hobby and major exercise outlet.
- She is having other difficulties with activities in sitting.
Valerie is a 35-year-old woman with lichen sclerosus. She has burning and itching in the anogenital area. She was referred to occupational therapy because she is no longer able to participate in her normal occupations. She cannot ride her bike, and that is her hobby and major exercise outlet. She is also having other difficulties in sitting.
- The Occupational Therapist evaluates Valerie to see what she needs to do, what she wants to do, and what barriers prevent her from doing them.
- The occupational profile shows that Valerie can’t ride her bike or exercise. She has difficulty with certain tasks while sitting. She is having difficulty with sexual relations and feels very “stressed out.”
What does Valerie want to do? What is important to her? What is preventing her from doing things? What are the barriers? The occupational profile shows that Valerie cannot ride her bike. She has difficulty with certain tasks while sitting. She is also having difficulty with sexual relations and feels very stressed out.
- Together, Valerie and the Occupational Therapist look at the tasks she wants to accomplish and her environment to see what they can change to enable her performance.
- They decide on
- a recumbent bike,
- an adapted seat cushion for work,
- practicing mindfulness, and
- referral to a closed, online support group on Facebook for women with Lichen Sclerosus to look for solutions to Valerie’s issues with sexual relations.
- The occupational therapist teaches Valerie relaxation techniques and mindfulness.
Together, they came up with a plan. They decided that she could use a recumbent bike with an adapted seat cushion. She also engaged in mindfulness and was referred to an online, closed support group on Facebook for people with lichen sclerosus to look for solutions for sexual relations. The occupational therapist taught Valerie relaxation, mindfulness, and other related techniques.
Case Study- Allen
- Allan has XYY. “Supermale syndrome.” He hurt his back and has low back pain. He wants to return to work but is concerned that his job as a grocery store cashier will aggravate his back.
- He is referred to occupational therapy to see if he can return to work and do some lifestyle redesign to learn to change how he does things so he can manage and rearrange the tasks that cause him pain.
This is my step-son. Allan has XYY, which is the super male syndrome. When he was born, we did not know he had this. He is very big and has a large frame. He hurt his back and has low back pain. He wants to return to work but is concerned that his job as a grocery store cashier will aggravate his back. He was referred to OT to see if he could return to work, look at some Lifestyle Redesign, and identify changes in how he does things. We need to rearrange things to manage the things that cause him pain.
- The evaluation shows that Allan has difficulty standing. Standing and bending exacerbate his pain. (person) His back hurts when he stands at the sink to brush his teeth (task or occupation). An onsite job analysis (occupational performance analysis) provides a look at the tasks Allan must do in the (tasks or occupations) environment in which he must do them. (environment)
- Reasonable accommodations to the workplace are discussed to enable occupational performance.
The evaluation shows that he has difficulty standing. Standing and bending exacerbate his pain (Person). His back hurts when he stands at the sink to brush his teeth (tasks/occupation). Onsite job analysis and an occupational performance analysis provided a look at the tasks he must do in the environment in which he must do them. Reasonable accommodations to the workplace were discussed to enable his occupational performance.
- Allan will need to sit while performing his job as a cashier. A specific chair was obtained for Allan, and this was discussed with his employer. Allan needed a reacher to avoid bending. Body mechanics were discussed, demonstrated, performed, and practiced within different contexts because of his size and XYY issues.
He will need to sit while performing his job as a cashier. A specific chair was obtained for him and discussed with his employer. A reacher was added. Body mechanics were discussed, demonstrated, and practiced within different contexts because of his size and XYY issues. Figure 2 shows him trying to brush his teeth, and he has to bend over. It hurts when he bends like that.

Figure 2. Allen has pain when he bends to brush his teeth.
We told him to open up the cabinet and put his foot up as this changes the relationship between his lower back in the sink. Figure 3 shows a position that causes less pain in his lower back.

Figure 3. This position with his foot up causes less pain.
We also gave him a reacher to not bend down when he plays with his dog, as shown in Figure 4.

Figure 4. Using a teacher to play with his dog.
Case Study- Lila
- Lila has Rheumatoid Arthritis. She is referred to occupational therapy because she has difficulty with daily living activities – particularly meal preparation and other household tasks. She can no longer shift her car out of the park because of the pain in her wrist.
- Her occupational profile and activity diary show Lila has difficulty opening cans and handling pots and pans in the kitchen. Both cause pain and are contributing to her deformities. Other household chores cause pain and fatigue. The deformities in her wrist and pain interfere with shifting her car out of park.
Lila has rheumatoid arthritis. She was referred to occupational therapy because she was having difficulty with some ADLs, particularly meal preparation and other household tasks. She could no longer shift her car out of park because of pain in her wrist. Her occupational therapy profile and activity diary showed she had difficulty opening cans and handling pots and pans. Both of these tasks cause pain and contribute to her deformity. Other household chores cause pain and fatigue.
- Lila and the occupational therapist look at her kitchen and how she performs the tasks in her home. Her pots are very heavy.
- Lila is given a can opener that uses a grip that doesn’t hurt and a tab-can opener. She agrees to change to a different, lighter set of pots, which have hollow handles that she can lift with 2 hands and/or have a cart with an adjustable height that will allow her to slide pots to the stove, oven, and storage
The OT looked at her kitchen set up and how she performed tasks. Her pots were very heavy. She was given a can opener that does not hurt and a tab can opener. She agreed to change to a different, lighter set of pots that have hollow handles. She can lift them with two hands and also uses a cart to move them with an adjustable height that will allow her to slide the pots to the stove, the oven, and storage.
- Lila and the occupational therapist review the patient’s activity diary. Lila attempts to clean her entire house in one day, including 4 loads of laundry. The OT and Lila discuss energy conservation and review a new schedule to divide the tasks and distribute them over the course of a week to decrease pain and fatigue.
- The OT adapts the automatic shift knob in Lila’s car to a ball grasp with a sponge and duct tape to change the grip so Lila can shift without pain.
They reviewed her activity diary and her attempts to clean her entire house in one day, including the four laundry loads mentioned earlier. They discussed energy conservation and reviewed a new schedule to divide the tasks and distribute them over the course of a week to decrease pain. The OT adapted the automatic shift knob in her car to a ball grasp with a sponge and duct tape to change the grip so she can shift without pain. Figure 5 shows the new got can opener.

Figure 5. New can opener.
For lifting tabs, she used this new device (Figure 6).

Figure 6. Tab opener.
Now, people are also using this device to be "hands-free" during COVID.
Case Study- Marie
- Maria has fibromyalgia. She is referred to occupational therapy because her pain and fatigue make it difficult to do her job as a teacher. She is also having difficulty coaching her daughter’s volleyball team.
- Her occupational profile shows her pain increases with carrying her briefcase and purse and other tasks on her job, and she is not sleeping at night.
Maria was referred to OT because her pain and fatigue made it difficult for her to do her job. She was also having difficulty coaching her daughter's volleyball team. Her occupational profile showed her pain increased with carrying her briefcase and purse and other tasks on the job. She was also not getting sleep at night.
- Maria and the occupational therapist complete a job analysis of Maria’s job as a salesperson. They also review Maria’s sleeping habits and coaching.
- The occupational therapist suggests putting Maria’s sample case on wheels. She also suggests a smalle
