Occupational Therapy's Value
- Health care systems are prioritizing the quality of outcomes over the quantity of services provided, and health care payers and other stakeholders are focusing on preventing hospital readmissions.
- This priority supports the effort to reduce the cost of health care by avoiding the most expensive care type and improving the quality of health care by promoting a sustained return to the community and remaining in the community.
- Occupational therapy practitioners have expertise that is critically important in this effort.
- Occupational therapy places a unique and immediate focus on patients’ functional and social needs, which can be important drivers of readmissions if they are not addressed.
- By addressing,
- Activities of daily living
- Instrumental activities of daily living
- Functional cognition
- Psychosocial needs
- Vision
- Fear of falling
- Safety
- occupational therapy practitioners can be a valuable addition to the effort to keep people out of the hospital and participating in their lives.
Pamela: Today, we are excited to present to you this topic. When we think about occupational therapy's value, we need to think about the healthcare system and how healthcare systems are prioritizing the quality of outcomes over the quality of services provided. It is no longer about how many services are provided, but rather it is the quality and the value you provide. The priority is to reduce costs and avoid the most expensive type of care and improve the overall quality of healthcare. We want to get people back into the community and living their lives to the fullest. Occupational therapy practitioners have expertise that is very critically important in this effort.
Occupational therapy provides a very unique and immediate focus on patients' functional and social needs. These are important drivers of readmissions if they are not addressed. Today, we will be talking about occupational therapy's value in the following areas: activities of daily living, instrumental activities of daily living, functional cognition, psychosocial needs, vision, fear of falling, and safety. We need to think about our valuable role in helping to keep people out of the hospital. By no means is this everything we do, but this is what we will be highlighting today.
The first thing I would like to do is to get a sense of your thoughts. If you can think of some words that come to mind when you think of readmissions in the facility in which you work. I am seeing some words (from the live event):
- frequent falls
- failure to thrive
- psychosocial issues
- repeat issues
- need for a higher level of care
- more money per admission
- dehydration, great
- "frequent flyers"
Hopefully, we will cover OT's value in addressing some of these areas in our presentation today.
Trends and Policies Influencing Quality Measure Reporting
I want to start by talking about the trends and policies that influence quality measure reporting, and why there has been so much hype about looking at readmissions.
Quadruple Aim
I want to talk about the quadruple aim in Figure 1. This is the new normal for health and healthcare.
Figure 1. Quadruple Aim graphic.
Organizations across the country now support four different goals. They are reducing healthcare costs, improving the patient experience, improving the health of people, and preventing practitioner burnout. Addressing the first three goals was known as the "triple aim." The quadruple aim now adds practitioner burnout. This is challenging, especially given the fragmented system and the payment system within the United States. And, there is really no one single way to measure progress. Hospital readmission rates are often used as a proxy for overall care and to address quality of care, especially when patients are sent to post-acute care and end up being readmitted within 30 days. Answering the question, "Was that the most optimal care?"
Healthcare Reform Laws
- Patient Protection and Affordable Care Act (P.L. 111-148), signed March 23, 2010, as amended by the Health Care and Education Reconciliation Act, signed March 31, 2010, is referred to as the Affordable Care Act (ACA) or federal health reform.
- Health Care and Education Affordability Reconciliation Act (P.L. 111-152)
Two laws really discuss healthcare reform. The first is the Patient Protection and Affordable Care Act, which is Public Law 111-148. It is often referred to as the Affordable Care Act, the Federal Healthcare Reform, or the ACA. The second is the Health Care Education and Affordability Reconciliation Act, which is Public Law 111-152. I have provided a link if you want to read the detailed pieces of this.
Healthcare Reform Readmission Penalties
- Hospitals were penalized for excessive readmissions for CHF, MI, and pneumonia effective October 1, 2012
- Payment reduction has expanded to other Medicare inpatient discharges
I do want to highlight a couple of areas. Hospitals can be penalized for excessive readmissions. It originally started on October 1st of 2012, with congestive heart failure, myocardial infarction, and pneumonia. It has further expanded to other Medicare inpatient discharges.
Community-Based Care Transitions Program: ACA Section 3026
- To pay for improved transitions of care for Medicare beneficiaries from the inpatient hospital setting to home or other care settings
- Improve the quality of care
- Reduce readmissions for high-risk beneficiaries
- Document measurable savings to the Medicare program
The community-based care transition program, which is part of the ACA (Section 3026), is used to pay for approved transitions of care for Medicare beneficiaries from the inpatient hospital to home or other care settings. Other care settings include skilled nursing, inpatient rehabilitation, and long-term care acute hospitals (LTACs). The idea is to improve the quality of care and reduce readmissions, especially for the high-risk Medicare beneficiaries. It is also important to document any measurable savings to the overall Medicare program. For example, if we are sending a patient from the acute care hospital to a post-acute care site, we want them to get their care in the post-acute care site and then go home from there. We do not want them to bounce back to the hospital.
Medicare's Hospital Readmission Reduction Program (HRRP)
The Medicare hospital readmissions program is on the acute side. More information can be found on this poster in Figure 2.
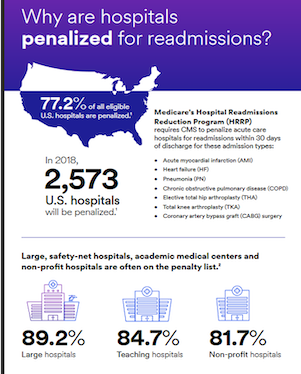
Figure 2. Infographic from the Medicare's Hospital Readmission Reduction Program (HRRP). Click here to view this image larger.
The HRRP requires that the Centers for Medicare and Medicaid Services penalize acute care hospitals for readmission within 30 days. And initially, it was for acute myocardial infarction (AMI), heart failure, pneumonia, chronic obstructive pulmonary disease (COPD), total hip arthroplasty (THA), total knee replacement (TKR), and coronary artery bypass graft (CABG). In 2018, the penalties were huge. There were 2,573 penalties within the United States. However, based on the type of hospital, there were some differences. Large hospitals had 89.2%, teaching hospitals had 84.7%, and nonprofit hospitals had 81.7%. Any way you look at it, there is still a lot of work that can be done to help reduce readmissions. After I go through some of the literature, we want to focus on OT's role and value in reducing readmissions.
Post-Acute Care Evolution
- Demographics and Demand for Post-Acute Care Services
- Aging Demographics
- Post-Acute care utilization is increasing
- Increasing incidence of chronic diseases
- Focus on getting patients home more quickly and coordination of the delivery of care
- Post-Acute Care is a Critical part of Quality Improvement and Patient-Centered Care
- Patient satisfaction
- Quality and clinical outcomes
- Care coordination across sites of care
- Reduce hospital readmissions
- Post-Acute Care can help reduce costs in a changing payment environment
- Value-Based purchasing
- Readmission penalties
- Episodic/bundled payment
- Accountable care and risk payments
When you start thinking about the post-acute care evolution, the demographics and the demand for post-acute care services is there. Post-acute care services are a critical part of quality improvement and patient-centered care. Post-acute care can help reduce costs in changing the payment environment. There are aging demographics. We also have to think about post-acute care utilization. It is increasing, and not only for one site but often for more than one site. People are living longer with more chronic diseases. The focus needs to be on getting these folks home quickly and the coordination/delivery of the care to do this.
We also want to make sure patients are satisfied. We want to make sure that there is quality in the clinical outcomes. Care has to be coordinated across the different sites.
We want to make sure there is value for creating the bundles in value-based purchasing.
Looking at post-acute care, you need to see how that fits into your network of services as this is critical to understanding accountable care and risk payments. How do we work together and partner between acute and post-acute care?
Readmissions Vary Among Post-Acute Care Providers
Readmissions vary among our post-acute care providers. As I mentioned, it is critical to understand and develop relationships between acute and post-acute care providers. Acute care organizations typically have preferred partners as 43% of Medicare beneficiaries are discharged to post-acute care. There could be one or two preferred sites for post-acute care, or even more. If you look at the first line in Figure 3, you can see the differences of readmission by the first site from acute to post-acute care at readmissions.
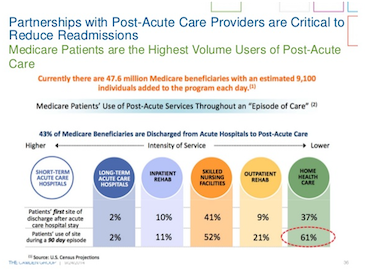
Figure 3. Medicare infographic about readmissions. Click here to view this image larger.
The stats show that readmissions for LTAC's are about 2%, inpatient rehab about 10%, skilled nursing at 41%, outpatient rehab at 9%, and home health at 37%. When you bump it up and start looking at episodes of care (during a 90 episode) and bundling, there are some differences. Although LTACs are about the same and inpatient rehab is a little bit higher at 11%, skilled nursing jumps up to 52%. Outpatient rehab rises to 21%, and home health moves to 61%. As you can see, there is a need to think about how to partner between these providers to help prevent readmissions. What is OT's role and how do we provide value in addressing some critical areas?
Impact of High Readmissions on Post-Acute Care Providers
- Two-percent reduction in Medicare payments started October 1, 2018, for higher-than-expected readmission rates the previous federal fiscal year
- A loss of referrals from hospitals that won’t send their patients to underperforming post-acute care providers
- A loss of referrals from patients and families who use publicly available readmissions data to make decisions about where to receive post-acute care
- Higher costs from providing additional medical care to patients who were not cared for properly during their post-acute care episode
Literature on Readmissions
Joint Replacement and Hip Fracture Readmission Rates: Impact of Discharge Destination (Riggs, Roberts, Aranow, & Younan, 2010)
- Retrospective cohort examined 606 orthopedic patients in acute care
- Outcome examined discharge destination and readmission
- Discharge to ARU was associated with a lower risk of hospital readmission
Hospital Readmission Among Older Adults Who Return Home With Unmet Need for ADL Disability (DePalma, Xu, Covinsky, Craig, Stallard, Thomas, & Sands, 2012)
- Unmet need for new ADL disabilities after return home from the hospital is particularly vulnerable to readmissions
- Patients’ functional needs after discharge should be evaluated and addressed
Functional Impairment and Hospital Readmission in Medicare Seniors (Greysen, Cenzer, Auerbach, & Covinsky, 2015)
- Functional impairment is associated with increased risk of 30-day all-cause hospital readmissions in Medicare Seniors especially those admitted for heart failure, myocardial infarction, or pneumonia
- Functional impairment may be an important but under-addressed factor in preventing readmissions
Functional Status Impairment is Associated with Unplanned Readmissions (Hoyer, Needham, Miller, Deutshendorf, Friedman, & Brotman, 2013)
- Functional status on Admission to CIIRP is strongly associated with readmission before planned discharge from CIIRP. Efforts to reduce hospital readmissions should consider patient functional status as an important and potentially modifiable risk factor.
Acute Rehospitalization During Inpatient Rehabilitation for Spinal Cord Injury (Hammond, Horn, Smout, Chen, DeJong, Sceiza, Jha, Ballard, & Bloomgarden, 2012)
- Approximately 11% of SCI patients experience Return to
- Acute (RTAC) during the course of rehabilitation for a variety of medical and surgical reasons.
- RTAC’s are associated with a longer rehabilitation length of stay.
Risk Factors for Discharge to an Acute Care Hospital From Inpatient Rehabilitation Among Stroke Patients (Roberts, DiVita, Riggs, Niewczyk, Bergquist, & Granger, 2014)
- Retrospective study of 783 stroke patients from 2008-2012 admitted to IRF
- Examined 60 who returned to acute care hospital
- Two significant risk factors were low motor FIM and enteral feeding
- Trends but not significant
- Younger age
- Longer onset time from stroke to IRF admit
- Presence of a tiered comorbidity
Transferring Inpatient Rehabilitation Facility Cancer Patients Back to Acute Care (TRIPBAC) (Asher, Roberts, Bresee, Zabel, Riggs, & Rogatko, 2014)
- Motor FIM score on admission is the best predictor for TRIPBAC in patients with cancer admitted to an IRF, followed by the presence of a feeding tube or a modified diet.
Thirty-Day Hospital Readmission Following Discharge From Postacute Rehabilitation in Fee-for-Service Medicare Patients (Ottenbacher, Karmarkar, Graham, Kuo, Deutsch, Reistetter... & Granger, 2014)
- Among post-acute rehabilitation facilities providing services to Medicare fee-for-service beneficiaries, 30-day readmission rates ranged from 5.8% for patients with lower extremity joint replacement to 18.8% for patients with debility.
- Higher motor and cognitive functional status were associated with lower hospital readmission rates across six impairment categories (stroke, lower extremity fracture, lower extremity joint replacement, debility, neurologic disorders, and brain dysfunction
- Factors that contributed most often to readmission in this study were heart failure, UTI, pneumonia, septicemia, nutritional and metabolic disorders, esophagitis, gastroenteritis, and digestive disorders.
Functional Status Outperforms Comorbidities in Predicting Care Readmissions in Medically Complex Patients (Shih, Gerrard, Goldstein, Mix, Ryan, Niewczyk...& Scheider, 2015)
- Readmission models based on functional status consistently outperform models based on medical comorbidities.
Higher Hospital Spending on Occupational Therapy Is Associated With Lower Readmission Rates (Rogers, Bai, Lavin, & Anderson, 2016)
- Occupational therapy places a unique and immediate focus on patients’ functional and social needs, which can be important drivers of readmission if not addressed.
- The only category where higher spending on OT had a statistically significant association with lower readmission rates for heart failure, pneumonia, and acute myocardial infarction.
Effects of Acute-Postacute Continuity on Community Discharge and 30-Day Rehospitalization Following Inpatient Rehabilitation (Graham, Bettger, Middleton, Spratt, Sharma, & Ottenbacher, 2017)
- Medicare beneficiaries in hospital-based rehabilitation units were more likely to be referred from a high-contributing hospital compared to freestanding facilities. However, the association between higher acute-post-acute continuity and desirable outcomes is significantly better in freestanding rehabilitation facilities than in hospital-based units.
Evaluating Hospital Readmission Rates After Discharge From Inpatient Rehabilitation (Daras, Ingber, Carichner, Smith, Levitt, & Andress, 2018)
- Examined facility-level rates of all-cause, unplanned hospital readmissions for 30 days after discharge from inpatient rehabilitation facilities
- Results demonstrated the ability to assess 30-day, all-cause hospital readmission rates post-discharge from IRFs and the ability to discriminate between IRFs with higher and lower than average hospital readmission rates
- The mean number of days to readmission was 13.0+/- 8.6 days and varied by rehabilitation diagnosis
Hospital Readmissions Reduction Program and Post-Acute Care: Implications for Service Delivery and 30-Day Hospital Readmission (Li, Karmarkar, Kuo, Ottenbacher, 2020)
- Impact on readmission after Post-Acute Care (PAC) for selected impairment groups (acute myocardial infarction, heart failure, and hip/femur fracture) may be mediated by the type of PAC
Characteristics of Hospitalized COVID-19 Patients Discharged and Experiencing Same-Hospital Readmission-United States, March-August, 2020 (Lavery, Preston, Ko, Chevinsky, DeSisto, Pennington,...& Gundlapalli, 2020)
- 9% readmission within 2 months of discharge
- More than single readmission in 1.6%
- Readmissions increased with the presence of chronic conditions
- Readmissions:
- 15% SNF
- 12% Home Health
- 7% Home
Social Determinants Matter For Hospital Readmission Policy: Insights From New York City (Baker, Alberti, Tsao, Fluegge, Howland, & Haberman, 2020)
- The study suggests augmenting the CMS Readmission model for all readmission cohorts to include smaller geographic SDOH composites and individual-level data not currently used in the readmission program
- Comprehensive social risk factor data collection focused on specific risk factors rather than proxies such as patient race/ethnicity and payer could help achieve these goals
Function Summary
- One of the largest contributors to medical costs incurred by senior citizens is functional impairment after hospitalization.
- Understanding SDOH and its impact on function is an area for further study.
Addressing Quality in Key Areas of Occupational Therapy Practice
Marla: Reducing readmission risk requires clinicians and interprofessional teams to move patients through the continuum of care differently.
Change Management
- Strategies to Prevent and Reduce Medical and Functional Risk Factors Related to Readmissions
Change management strategies need to be implemented including organization, motivation, teamwork, and an integrated strategy. Post-hospital syndrome is a condition of generalized risk that results in about 2.6 million readmissions each year. The majority of these patients are readmitted for another condition than their index hospitalization. Contributing factors to post-hospital syndrome include pain and discomfort, nutritional issues, circadian rhythm disorders, and functional decline. Functional decline is where there is a loss of mobility, cognitive decline, and hospital-acquired disability or hospital-associated disability.
Hospital Associated Disability (HAD) (Loyd, Markland, Zhang, Fowler, Harper, Wright,...Brown, 2020)
- HAD is defined as loss of independence in activities of daily living (ADL) following acute hospitalization, is observed among older adults
- Approximately 1/3 of hospitalized older adults develop a new disability by discharge from acute care
- Independence in ADL was assessed using:
- Katz Index of Independence in Activities of Daily Living
- Barthel Index of Independence in Activities of Daily Living.
- Hospital-based programs to assess functional ability and identify at-risk older adults are needed
Hospital-associated disability is defined as a new inability to complete one or more ADLs post-discharge from the hospital. This places patients at risk for readmission, institutionalization, and even death. It happens in about one-third of all hospitalized older adults. And, hospitalization in acute care, as we have discussed, poses significant risks to the functional independence of our older adults. This risk is really unchanged, despite the shorter length of stay that we are seeing.
Prevention of Readmissions by Addressing Quality in Key Areas of Occupational Therapy Practice
- Rehabilitation providers need to demonstrate how their practice contributes to minimizing the risk of poor outcomes and enhance the likelihood of achieving desired outcomes
- Functional status is often associated with health outcomes, including post-hospital readmissions
- Engagement of patients and families to promote patient-centered, high-quality care is critical for occupational therapists to improve outcomes by targeting the care provided in key areas of practice
Prevention of readmissions is where OT demonstrates its value by addressing quality in key areas of our practice. Minimizing risk to hospital-associated disability and poor outcomes is one opportunity to engage patients and their families to promote patient-centered, high-quality care.
Occupational Therapy Practice Framework (AJOT, 2020)
- Occupational Therapy Practice Framework (OTPF-4) describes occupational therapy practice with a focus on achieving health, well-being, and participation in life through engagement in occupation.
- Practice areas are related to important quality measures that are important to patients, health systems, and payers and are connected to the distinct value of occupational therapy.
This past summer, AOTA published the fourth version of the Occupational Therapy Practice Framework. The OTPF describes occupational therapy practice with a focus on achieving health, well-being, and participation in life through engagement in occupation.
Distinct OT Practice Areas Associated with Decreased Hospital Readmissions
- Activities of Daily Living
- Instrumental Activities of Daily Living
- Falling
- Functional Cognition
- Social Participation
- Roles, Habits, Routines, and Rituals
- Vision
- Safety
Practice areas are related to important quality measures that are important to patients, health systems, and payers. These are all connected to the distinct value of occupational therapy. One of the areas that is highlighted in the fourth version is health management. This includes social and emotional health promotion and maintenance, symptom and condition management, communication within the healthcare system, medication management, physical activity, and nutrition management.
OT's Role in Reducing Risk
We are now going to talk a little bit more about the evidence supporting OT practice to positively impact hospital readmission risk. The areas that we are going to specifically talk about include activities of daily living, instrumental activities of daily living, fear of falling, functional cognition, social participation, roles, habits, routines, and rituals, vision, and safety.
Activities of Daily Living (ADL)
- Activities of daily living (ADL) are the basic activities needed to take care of oneself.
- ADL performance is directly connected to readmission to acute care.
- In a nationally representative retrospective study, the authors found that older adults who were dependent in three or more ADL had significantly greater odds of being readmitted (DePalma et al., 2012).
- Pisani and colleagues (2017) found that functional performance in ADL is a significant predictor of readmission to acute care following elective surgery. People who are more dependent in ADL are more likely to be readmitted to acute care.
Participation and optimization of function related to ADLs is a cornerstone of OT practice. ADLs are the activities needed for self-care and are directly connected to readmission to acute care. In 2012, DePalma, as Pam spoke about, found that older adults dependent in three or more ADLs had a significantly increased risk for hospital readmission. Pisani also found this with a population of patients admitted for elective procedures. This demonstrates the potential impact of hospital-associated disability that we spoke about earlier.
- Medicare is now using Section GG Functional items related to ADL to score and compare post-acute care facilities (skilled nursing facility, inpatient rehabilitation facilities, home health) on improvement in functional performance of ADL using outcome measures (Sandhu et al., 2018).
- Identifying, understanding, and addressing ADL is key to be evaluated and addressed.
- Activities of Daily Living (ADL) are critically important for occupational therapy practitioners to consider in evaluation, intervention, and discharge planning. Occupational therapy is effective at improving functional ability in ADL performance (Smallfield et al., 2017, D’Amico et al., 2018, & Wolf et al., 2014).
- Utilizing occupation-based interventions to address and improve a person’s ability to perform ADL independently or at their optimal level may decrease a person’s likelihood of readmitting to acute care.
For those working in post-acute care, Medicare is now using Section GG, functional items, to score and compare facility outcomes. OTs in all practice areas need to be comprehensively assessing patients and using occupation-based interventions to ensure optimal outcomes are achieved, thereby decreasing a person's likelihood of readmission to acute care.
Instrumental Activities of Daily Living (IADL)
- Instrumental activities of daily living (IADL) support daily life and are more complex than ADL. This includes activities such as financial management, health management, household management, driving and community mobility (Pisani et al., 2017)
- People who are more dependent for IADL are more likely to readmit to the hospital following discharge (Pisani et al., 2017)
- IADL independence is a predictor of acute care readmission and morbidity
- IADL performance in areas such as shopping, transportation, and financial management are associated with the progression from mild cognitive impairment to dementia (Bidzan et al., 2016)
IADL performance is complex, and it requires the integration of physical and cognitive skills. These skills include the care of others, care of pets/animals, child-rearing, communication management, driving and community mobility, financial management, meal preparation and clean-up, safety and emergency maintenance, and shopping. Social factors, such as depression, can also play a role in how a patient can complete their IADLs. Pisani found that people who are more dependent in their IADLs are more likely to be readmitted to acute care.
- Occupational therapy is uniquely positioned to assess these areas and address the skills and ability to integrate each to achieve improved independence in IADL performance.
- These factors and skills may be addressed through self-management, prevention, and community-based interventions (Hunter et al., 2018).
IADL performance is most often assessed using performance-based standardized tools, and OT is ideally prepared to assess and address skills required to enhance independence with these tasks, self-management, prevention, and community-based interventions. In the acute setting, this means ensuring that the appropriate next level of care is recommended and in place for discharge through communication with the interprofessional team, the patient, and the family. And once in the post-acute care setting, ensuring that the patient has the skills and the supports to not only survive but also thrive in whatever their ultimate environment is going to be. This will help reduce the risk for readmission.
Fear of Falling
- Falls are a significant contributor to readmissions (Galet et al., 2018)
- Fear of falling is associated with the judgment of individuals. Those with poor judgment may be associated with an increased risk of falls (CDC, 2019)
- Fear of falling may be protective, high-risk, or isolating.
- A patient who has a low fear of falling but a high risk of falling may be less likely to integrate safety into their habits around occupational engagement.
- A patient with high fear of falling but a low risk may undertake habits and routines that are unnecessarily isolating to avoid falls.
- A person with a protective fear of falling integrates safe habits and routines into daily occupations.
Let's now talk about falls and the fear of falling. Falls can significantly increase the risk for hospital readmission. The fear of falling is associated with judgment, and those with poor judgment may be at increased risk for falls. The fear of falling cycle includes reduced mobility or decreased activity and engagement in ADLs, resulting in muscle weakness. This in turn increases the risk for falling, and then a fall can occur.
Fear of falling can be categorized as protective, high risk, or isolating. A patient who has a low fear of falling, but a high risk of falling may be less likely to integrate safety into their habits around occupational engagement, therefore, not moving as much. A patient with a high fear of falling, but a low risk may undertake habits and routines that are unnecessarily isolating to avoid falls. And then finally, a person with protective fear of falling integrates safe habits and routines into their daily occupation. This is where OT has their true opportunity to help patients develop those protective fear skills to be able to keep them safe.
- The Centers for Disease Control now recommends referral to occupational therapy if home hazards are likely in their Stopping Elderly Accidents, Deaths & Injuries (STEADI) algorithm for fall risk screening, assessment, and intervention.
- Occupational therapy is uniquely qualified to address the habits and routines around fear of falling to facilitate a protective fear that supports optimal engagement and minimizes risk.
The CDC, the Center for Disease Control, now recommends a referral to OT if home hazards are likely in their study algorithm, which is stopping elderly accidents, deaths, and injuries. Through our unique lens, OTs are well-positioned to address the fear of falling to engage patients to develop a protective fear and optimize their engagement, while minimizing their risk.
Functional Cognition
- Functional cognition is a critical component of fear of falling and IADL performance. The skills, training, and framework of occupational therapy practitioners make a strong case that it is the ideal discipline to assess when and how cognition influences a person’s ability to function independently and safely (Giles, et al., 2017)
- Assessing, documenting, and incorporating functional cognition into interventions is critical to promote safe and independent engagement in occupations in the community contributing to a decreased likelihood of readmissions
Giles reported that functional cognition is a critical component of fear of falling and IADL performance. The skills, training, and framework of occupational therapy practitioners make a strong case that it is the ideal discipline to assess when and how cognition influences a person's ability to function independently and safely. When an individual with diminished functional cognition requires a caregiver for safe discharge, it is really essential that the caregiver fully understands how functional cognition impacts the patient's ability to be safe at home and is trained to support the patient as well as to promote the well-being within that new environment.
Social Participation
- Higher connection and participation in social activities are correlated with decreased readmission rates (Brewster et al., 2019).
- Social functioning is also an important factor to assess and address for persons with mild cognitive impairment (Bidzan et al., 2016).
- Awareness and integration of occupation-based interventions that are sensitive to psychosocial needs at discharge promote the distinct value of the profession.
When we look at connection and participation in social activities, this is correlated with decreased readmission risk. OT should identify factors that both support and prevent a patient's social participation. Awareness that integration of occupation-based interventions that are sensitive to psychosocial needs at discharge promotes the distinct value of our profession.
Roles, Habits, Routines, and Rituals
- Performance patterns (roles, habits, routines, and rituals) are critical elements to understand how a person engages in occupations and what elements may be adapted to achieve ongoing, optimal performance in the community (AOTA, 2014).
- Addressing performance patterns from the evaluation through discharge allows occupational therapy to collaborate with patients to promote occupational engagement in a contextually meaningful way.
A distinguishing feature of occupational therapy is occupation-based and contextually relevant evaluations and interventions. Performance patterns, roles, habits, routines, and rituals are critical elements to understand how a person engages in occupations and what elements may be adapted to achieve ongoing optimal performance in their community. Addressing performance patterns from the evaluation through discharge allows occupational therapy to collaborate with patients to promote occupational engagement in a contextually meaningful way. This should occur both throughout the continuum, from acute care through to post-acute care settings.
Vision
- Integrating a vision screen into all adult occupational therapy evaluations can identify when vision, sensation, and perception are a factor that practitioners should address in the plan of care
- Decreased functional ability due to low vision correlates with a higher likelihood of acute care readmission and higher overall costs of care (Morse et al., 2019; Jaffee et al., 2016)
Vision is another area where OT really can shine. Practitioners must understand how a person perceives the environment along with whether or not this perception has changed over time. Integrating a vision screen into all adult occupational therapy evaluations can identify when vision, sensation, and perception are factors that practitioners should address in the plan of care. Morse and Jaffee have both documented that decreased functional ability due to low vision correlates with a higher likelihood of acute care readmission and higher overall costs of care. Occupational therapy practitioners have multiple options to address vision deficits, including connecting patients with a vision specialist, such as an optometrist, ophthalmologist, or another OT who specializes in vision therapy skills.
Safety
- Understanding ADL and IADL performance, fear of falling, as well as functional cognition status, allows occupational therapy practitioners to identify potential safety concerns and address those concerns directly or refer for a follow-up assessment by occupational therapy in the community or other appropriate professionals (Pynoos et al., 2012).
- It is important to complete some type of a safety screen with the patient to understand if the practitioner needs to coordinate or refer to occupational therapy for an in-home assessment following discharge (Godfrey et al., 2019; Pighills, et al., 2019).
Occupational therapy practitioners are in a unique position to understand potential safety concerns for each patient in his or her specific discharge environment. We collect information from the patient's perspective in the occupational therapy profile. Matching the discharge environment and safety with the person's abilities is an important step to ensure safe discharges. Older adults and their caregivers have a considerable burden during transitions and would benefit from well-targeted, effective interventions.
Transitions of Care
Care Transitions
- Transitions in care have been defined as the set of actions taken to ensure that care is coordinated as patients are transferred from one clinical setting to another (Brown, 2018).
- These transitions are vulnerable periods for all patients and especially for older adults with multiple comorbidities, prior hospitalizations, poor social or family support, high medication burden, and lower health literacy (Barrell et al., 2015)
- Brown (2018) reported that in the 30-day post-hospital discharge period, 60% of Medicare beneficiaries made one transfer, 18% made two transfers, 9% made three transfers and 4% made four or more transfers.
Brown has described transitions of care as the set of actions taken to ensure that care is coordinated as patients are transferred from one clinical setting to another. It is well-documented that these transitions are vulnerable periods for all patients and especially for older adults with multiple comorbidities, prior hospitalizations, poor social or family support, and higher medication burden. In addition, lower health literacy levels also place them at risk. In 2018, Brown reported that in the 30-day post-hospital discharge period, 60% of Medicare beneficiaries made one transfer, 18 made two transfers, nine made three transfers, and four made four or more transfers.
- Each time a patient transitions from one post-acute care environment to another the potential for fragmentation in communication resulting in critical information being lost and care planning being fractionated.
- Creating processes that support patients and their families to improve transitions of care are of critical importance to prevent readmission to hospitals
- Transitional care programs have demonstrated reductions in readmission rates up to 45%.
(Albert, 2016; Brown, 2018; Coleman et al., 2006; Farrell et al., 2015; Hamar et al., 2016; Leland et al., 2019)
Transitional Care Programs
- These programs incorporate several processes including collaborative discharge planning:
- Detailed patient-centered discharge summaries
- Post-discharge telephone calls
- Home visits
- Primary care follow up
- Medication reconciliation
(Brown, 2018, Farrell, et al., 2015, Coleman et al., 2006; Albert, 2016; Hamar et al., 2016
Care Transition Processes
- Leland et al. (2019) identified five frequently implemented care transition processes and four of these were used in 74% of the studies
- These processes include:
- Medication self-management
- Scheduling follow up care
- Post-discharge telephone calls
- Medical self-management
- Patient and family education and care transition coaching
In a scoping review, Natalie Leland in 2019 identified five frequently implemented care transition processes, and four of these were used in 74% of the cases. These processes included medication self-management, scheduling follow-up care, post-discharge telephone calls, and medical self-management. In 60% of the studies, patient and family education and care transitions were also included. The literature supports that a single intervention will have a limited impact on hospital readmission rates; however, using a comprehensive bundled intervention approach has led to reductions in re-hospitalization, emergency care utilization, healthcare costs, and improvements in quality of life, and patient, family, and provider satisfaction.
Examples of Transition Care Programs
Now, we are going to highlight a few of these programs.
- Coleman et al. (2006) care transition intervention model
- A 4-week program focusing on patient engagement using a transition coach
- 4 Pillars:
- Patient-centered medical record
- Primary care follow up
- Medication self-management
- Alertness to red flags
The first one we are going to talk about was done in 2006 by Coleman and associates. They provided a care transition intervention model that was a four-week program focusing on patient engagement using a transition coach. They had four pillars to their intervention. They included a patient-centered medical record, primary care follow-up, medication self-management, and alertness to red flags that would put the patient at increased risk for hospital readmission.
- Naylor et al. (2011) transitional care model
- Interventions were provided over 1-3 months and targeted high-risk older adults.
- APN completes a pre-discharge assessment and then collaborates with the hospital team to develop a plan with telephone outreach, home visits, and primary care visits.
- Pillars include:
- Patient engagement
- Goal setting
- Comprehensive communication plan with all stakeholders
Naylor in 2011 developed a transitional care model where interventions were provided over a one-to-three month period of time and targeted high-risk older adults. In this particular program, a nurse practitioner completed a pre-discharge assessment and then collaborated with the hospital team to develop a plan that included telephone follow-up calls, home visits, and primary care visits. The primary pillars of this particular program were patient engagement, goal setting, and a comprehensive communication plan with all stakeholders.
- Society of Critical Care Medicine’s Project BOOST (Better Outcomes for Older Adults)
- The systematic model focuses on the discharge process and communication with the patient and receiving providers (Hansen et al., 2013)
- Primary Interventions:
- Discharge planning
- Medication Reconciliation
- Patient and family communication before discharge
- Discharge telephone calls
- Patient-centered discharge instructions that reflect appropriate health literacy level
The Society for Critical Care Medicine had a program called Project BOOST, Better Outcomes for Older Adults. This was a systematic model that focused on discharge processes and communication with the patient and receiving providers. The primary interventions in this model included discharge planning, medication reconciliation, patient and family communication before discharge, discharge telephone calls, and patient-centered discharge instructions that reflected the appropriate health literacy level.
- INTERACT (Interactions to Reduce Acute Care Transfers) (Ouster et al., 2014)
- Reducing readmissions from SNF and long term care facilities
- Multiple strategies that identify, document, and communicate early changes in medical conditions to allow providers to intervene earlier.
The last one we will look at is INTERACT, Interactions to Reduce Acute Care Transitions. This was by Ouster. Ouster looked at reducing readmissions from SNF and long-term acute facilities. Multiple strategies were including how they identified documenting and communicating early changes in medical conditions to allow providers to intervene before transfer to the hospital.
Transitional Care Program Team Members
- These programs leverage the expertise of care team members: nurses, providers, pharmacists, social workers, and care coordinators to implement the prescribed interventions.
- Occupational therapy practitioners were not included in the interventions (Leland et al., 2019).
- OT is well-positioned with a unique lens to provide and support meaningful interventions to optimize quality transitions of care.
When we look at these transitional care programs, these programs all leverage the expertise of the care teams, nurses, providers, pharmacists, social workers, and care coordination members to implement the prescribed interventions. What Natalie Leland found in her scoping review was that occupational therapy practitioners were not included in these interventions. Occupational therapy evaluations encompass the client's beliefs, values, contexts, and environments to develop a comprehensive, client-centered care plan that can identify and address risks for readmission during their acute care stay. This can hopefully provide recommendations for the discharge and follow-up so that those patients are supported in whatever post-acute care environment they are transferred to.
Occupational Therapy Empowers Successful Transitions of Care
- Assessing and identifying deficits in functional, psychosocial, and cognition that may impact the patient’s ability to successfully navigate and develop medication and medical self-management skills.
- Medication management skills can involve the functional

