Introduction
Christine: I am very excited to have arranged this conference of speakers that are all going to be talking about different aspects of occupational therapy's mental health response to the COVID pandemic. Each day, we'll be having a little bit different topic with a little different population. Each of the speakers comes from a different area of practice and from a different area of the country. They will each be presenting their own unique perspectives, but I think everybody will be able to take something from each of the presentations and apply it to your own practice or your own setting. I think that you will see their individual expertise with specific populations, but also some nice common themes that go across different topics.
Today's speakers will be Danny Shin, Simone Gill, and myself. I am an associate professor at the American International College in Springfield, Massachusetts, where I teach primarily in the doctoral program and teach research. My background is in mental health though. Danny Shin and Simone Gill are both from Boston University in Boston, Massachusetts. Danny is currently an occupational therapist and a PhD candidate in the Rehabilitation Sciences program at Boston University. His expertise is in neurorehabilitation and physical dysfunction. His work focuses on examining how physical, psychosocial, and environmental factors impact fall risk in people living with chronic conditions. Simone Gill is his mentor, and she is an associate professor in the Occupational Therapy Department at BU. She directs the Motor Development Lab, which examines how people's bodies and environmental demands influence walking and motor functioning across the lifespan. Her current research in her lab focuses on fall risk and how adults modify their walking patterns to cope with changes in their bodies before and after bariatric surgery. I have been working with the two of them on a project that Danny will be explaining in more detail, affiliated with Boston Medical Center, looking at the experience of falls.
Overview
- Learning Objectives
- Introduction to Medically Complex Client
- Overview of Research Context
- Fall Prevention Intervention
- Impact of COVID-19 and lessons learned
- Summary and Q&A
Medically Complex Client
- People living with HIV (PLWH)
- Highly active antiretroviral therapy (HAART)
- Viral load undetectable
- Less harm to the immune system
- Reduces the chance of passing HIV to partners
- Viral load undetectable
- Side effects
- Nausea
- Dizziness
- Fatigue
- Pain
Danny: We will be using people living with HIV as our model for the medically complex client. HIV, or the human immunodeficiency virus, is a virus that attacks the body's immune system. As of 2019, it was estimated 1.2 million people in the United States had HIV. HIV works by attacking and destroying the infection-fighting CD4s and the loss of these CD4 cells makes it difficult for the body to fight off further infections and also certain types of cancers. Without treatment, HIV can gradually destroy the immune system and advance to AIDS.
Since the start of the AIDS epidemic in 1981, there has been a Herculean effort to help control this virus. By 1994, AIDS was a leading cause of death for Americans age 25 to 44. One of the major breakthroughs was in 1995 with highly active antiretroviral therapy. This medicine works by controlling and suppressing the viral load. And if done and adhered to properly, it can also make it undetectable to test. This causes less harm to the immune system and reduces the chance of passing HIV to partners.
Unfortunately, some of the side effects associated with this lifesaving medicine are things such as nausea, dizziness, fatigue, and pain that may lead to falls.
Aging Population
- Estimated that half of the people living with HIV (PLWH) are 50 or older (Greene et al., 2013)
Due to the effectiveness of highly active antiretroviral therapy, people living with HIV are reaching older and older ages. It is estimated that half of the people living with HIV are 50 or older. As the ages of people living with HIV increase, the risk for age-related complications increases as well. There is a shifting HIV treatment focus from acute care to management of chronic conditions. Furthermore, people living with HIV demonstrate accelerated aging, which may lead to a higher risk of falls.
Accidental Falls
- An unexpected event in which an individual experiences a loss of balance and come to rest on the floor
- The most common cause of non-fatal injury (Englander et al., 1996)
- Serious medical consequences
- fractures and emergency room visitations for 2.8 million older adults (CDC, 2015; Wolinsky et al. 1997).
Falls are an unexpected event in which an individual experiences a loss of balance and comes to rest on the floor. Falls are one of the most common causes of non-fatal injuries, and they lead to serious medical consequences, such as fractures and emergency room visitations for 2.8 million older adults. These consequences are not only limited to the medical burden associated with falls, but it also takes a psychological toll.
Older adults who have suffered a fall exhibit a fear of falling again. This results in less physical activity, decreased socialization, and this further exasperates any existing risk factors. Due to this high incidence of falls in older adults, it has been extensively studied, and also fall prevention interventions tend to focus on this population.
PLWH and Falls
Statistics
- Up to a third of middle-aged people living with HIV infection experience a fall each year (Erlandson et al., 2012).
- Fractures following a fall are 40-60% more common in PLWH than in the normal population (Kim et al., 2018).
- Fall rates in middle-aged adults with HIV were as common as uninfected persons aged 65 and older (Erlandson, 2012).
- Consequences
- Fractures following a fall are 40-60% more common in PLWH than in the normal population (Kim et al., 2018).
People living with HIV (PLWH) experience a high risk of falls. Up to 1/3 of middle-aged people living with HIV infections experience a fall each year. This rate of falls, up to 1/3, is similar to what the older population experiences. And following a fall, fractures are 40 to 60% more common people in people living with HIV than the normal population.
Risk Factors for Falls
- Polypharmacy (Gnjidic et al., 2012)
- Five or more medications (Gnjidic et al., 2012)
- Multimorbidity (Kim et al., 2012)
- Presence of two or more chronic conditions
- Frailty (Erlandson et al., 2019)
- Fried Frailty Phenotype (Fried et al., 2001)
- Substance use (Kim et al., 2019)
- Alcohol, and drugs
Some established risk factors for falls are polypharmacy, which is the simultaneous use of five or more medications. This concept of polypharmacy affects people living with HIV because it typically takes three or more medications to reach that viral suppression to keep HIV in check. This leaves them vulnerable to additional polypharmacy when any additional medications are indicated.
Multimorbidity is the presence of two or more chronic conditions. In non-HIV infected people, multimorbidity is associated with decreased functional status, quality of life, and disability.
Frailty is an inability for the body to reach homeostasis following an external stressor. This concept of frailty will be talked about in further detail in a moment. One of the ways to conceptualize and capture this frailty is through the Fried Frailty Phenotype.
Lastly, substance use is bound to be elevated in people living with HIV. This is especially concerning because alcohol use has been shown to be associated with a decreased adherence to the highly active retroviral therapy, which may lead to increased virus and all the negative consequences associated with that.
Frailty
- Frailty (Collard et al., 2012; Morley et al., 2013)
- Vulnerability health outcomes
- Reduced capacity to stressors
- Loss of physiological function
- Fried Frailty Phenotype (Fried et al., 2001)
- Slowness
- Weakness
- Poor endurance and energy
- Unintentional weight loss
- Low physical activity level
Frailty is a vulnerability to global health outcomes. It leads to reduced capacity to stressors and a loss of overall physiological function. The way that frailty is captured is using the Fried Frailty Phenotype using five criteria. Using this phenotype, if you have three or more, you are labeled as frail. And if you have two or more, you are categorized as pre-frail.
Slowness is conceptualized as the slowest 20% of the target population as defined at baseline, and it is based on walking 15 feet. This is adjusted for gender and standing height. Weakness is similarly adjusted by gender and by BMI, and it is the lowest 20%. An unintentional weight loss of fewer than 10 pounds in the previous year would be categorized as unintentional weight loss. Poor endurance and energy and low physical activity level are captured by using self-report.
With this elevated fall risk and identified risk factors for falls in people living with HIV, there is no known fall risk intervention in this population. To adjust this, I will talk next talk about a recent study and a pilot intervention plan to use them as an example of how COVID-19 has affected the research with this population.
Research Study Overview
Overview
This collaboration between the Boston Medical Center and the Boston University, Sargent College Department of Occupational Therapy, came about because of this need. Our lab, specifically the Motor Development Lab, was reached by these collaborators who held expertise in studying people living with HIV with substance use. They wanted help with investigating fall risk and developing a fall prevention intervention with this population.
Conceptual Model
Figure 1 is the conceptual model for their ongoing cohort study from the past five years, and it is being conducted by our collaborators.
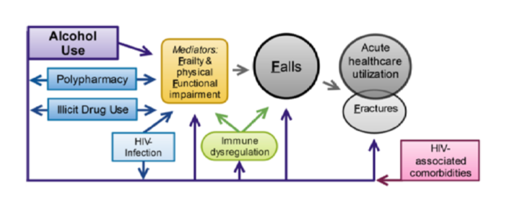
Figure 1. Conceptual model from HIV and falls study.
They are interested in studying the relationship between alcohol use and falls and want to see if frailty and functional impairment mediates this relationship and the similarity with polypharmacy on illicit drug use. Our lab was brought in to pilot test the feasibility of this falls prevention intervention, tailored to address the identified risk factors in this population. Christine will be talking a little bit about one of the first components we used to develop this intervention, which was the qualitative piece.
Research Study-Qualitative
Methods
Christine: I was invited to participate in this research because of my background in qualitative research and my background with many aspects of this population. I have worked with many people who are homeless, which is a factor for many of the people in this study. They are currently experiencing homelessness or have in the past as well as increased substance abuse with this group.
As Danny mentioned, we took a two-pronged approach. Both qualitative and quantitative approaches were used to collect data about the need for a fall intervention and what would be most attractive and useful to the people who were participating in the intervention.
The majority of the people in the study are in their 40s to 60s. And because it is a cohort study, people have been in there for a while. I did want to interview a few people that were younger to try to get that perspective as well. In addition to recruiting from the current study, the investigators are also recruiting new people. This is because the life expectancy is shorter than normal because of all the co-morbidities, and we wanted to make sure that we would have people that would be staying in.
I began by doing five individual qualitative interviews before the pandemic occurred. Those interviews were actually held in person. I interviewed five different people who ranged from their late 20s to their 60s. The five people that I interviewed represented a wide range of living situations and abilities. I interviewed one woman who was using a scooter could get up and transfer herself in a very sort of dangerous way, as well as people who used walkers and canes who were able to walk independently. We had the whole spectrum of people. We had people who were living alone, people who were living with a roommate, and people who were living in housing. And, we did have one man who was homeless. They also had various levels of drug and alcohol activity. In the previous study, everyone had been required to be an active drug or alcohol user. But this time, many of them were in recovery. However, there was nobody who was completely sober or clean entirely.
The interviews lasted from 40 minutes to an hour and a half. There was one that was only 40 minutes because that was as long I could get him to talk. The rest went the full hour and a half with me really needing to stop them because they enjoyed having this opportunity to talk and to describe what was going on in their lives. The interviews focused on their experience of falls, how recently they had fallen, and then to describe their last several falls to me in detail. This was one of the most illuminating pieces of information. For the quantitative data, research assistants asked these individuals every six months about falls. The data that I got from the narrative interviews was very different than what they were reporting on the structured interview forms. I think this had to do with my role as a researcher, not being a part of the regular team, and the way that I asked the questions. It was not a simple, "How many times have you fallen?" Instead, it was, "Tell me about that time you fell." This questioning would lead them to talk about other times they fell and discuss these in more detail. This illuminated the value of collecting data from a qualitative perspective and how you get different types of information.
I also asked them about the cause of their fall. We expected to hear a lot more about being intoxicated or drug and alcohol use. However, it was very interesting. They differentiated falls that were caused by intoxication versus falls that were caused by tripping, low energy, or the other things that I will be talking about in a few minutes. What was most striking was that the falls that were related to intoxication were really seen as just par for the course, or something that they were not really going to do much about. "Well, yeah, I was high and I passed out. When I went to stand up, I just collapsed and fell." They did not see these as the same kind of falls as when they tripped, were dizzy, or a result in a change in blood pressure. They took these falls from substance abuse for granted despite the fact that the injuries that they described were similar.
There was a woman that had one of the most unusual injuries. When she was intoxicated, she sat on a box. She fell through the box as it did not hold her weight and was stabbed in the arm by a screwdriver that was in the box. She had to go to the emergency room. She brushed this incident off completely. Again, this is the kind of data that does not show up in the quantitative data.
In addition to the causes, I also asked a lot about their strategies to prevent falls or what they did when they fall. How did they get help? Do they go to the hospital? Do they ask for help? Do their doctors know? Do they talk to their doctors? Out of the five people that I interviewed, there was only one that had regular conversations with their doctor about their falls. Another person that I interviewed had fallen twice, very severe falls with head injuries, and he had a number of other serious medical conditions. He did not go to the hospital or even call a doctor for two days. He lived in an apartment that was subsidized, and he had not had hot water for six months. He had the people planning to come to fix his water, and he did not want to risk missing that appointment to go to the hospital for a head injury. He was of great concern in terms of the severity and the implications of falls. Their insight and resources, in terms of being able to deal with what happens when they get injured, was very interesting as well.
In addition to the individual interviews, I also conducted four focus groups. The individual interviews were pre-pandemic, and the focus groups were after the pandemic. The focus groups were all conducted virtually via Zoom but without cameras. This was due in part to the research team's concern that people would not have the technology available to be able to call into Zoom and to be on camera.
The first big question I had for them was what was their interest in participating in the intervention. What would it take for them to participate? I found that they wanted incentives like pizza, gift cards, transportation, and those sorts of things. They all agreed that they could attend on a regular basis. I suspected that they would be interested based on the individual interviews and that they were looking forward to this contact with medical professionals as they were very isolated. The focus groups after the pandemic really highlighted this. They were all really craving contact. They were willing to participate, but they did not understand the language of, "Can you participate virtually?" I had to further explain, "Can you FaceTime on your phone? Do you have a video on your phone?" It turned out that they all could.
Again, there were some concerns about being on a camera aside from the technology piece. Confidentiality was one of them. It was very interesting to me that they did not all know that everyone in the study was HIV positive. They talked about it in code until they realized that, and they did not want that disclosed to anybody. They were very concerned that in a focus group that their HIV history would be revealed. They were not concerned however about their drug use in the least, even if it was illegal. It was their HIV history that they did not want to be revealed. They were also willing to come in and meet in person if transportation could be provided, despite the risks of the pandemic. These were conducted back in June and July of 2020 when things were unknown.
The other interesting thing that came out in the qualitative groups was how they talked about the experience of falling and how they interpreted that. In the 2nd focus group, I was talking to them about falling and saying, "When's the last time you fell?" And, "How many times have you fallen?" They all thought I was talking about falling off the wagon or their sobriety. This went on for probably 10 or 15 minutes with me trying to redirect it. I realized that I had to explicitly say physical fall to make sure that we were all on the same page. They were so used to talking about their drug use that a physical fall was an extra topic to them.
Findings
- Motor Function
- Assistive Devices
- Reminders
- Strategies for adapting the environment
When I analyzed all of the individual interviews and focus group findings, we were able to categorize them under four categories. Motor function related to losing their balance when they bent over or tried to stand up. There were also balanced-related issues to sitting up and getting out of bed. There were a number of people that would fall over and lose their balance when they were trying to get dressed or trying to get out of bed.
Their use of assistive devices was another area. This came up with both their grip strength and their ability to use assistive devices. Danny is going to talk more about grip strength, but it was fascinating to me from the very beginning that that was such a big factor in looking at why people fall. This is not my area of practice, but I realized how important grip strength is when using devices. For example, they would reach for a grab bar in the shower and not be able to hold themselves and fall.
They also needed many reminders for exercise, eating, et cetera. The last one was strategies for adapting the environment, and as an OT, this was of particular interest. We talked about strategies like putting all of their things in lower cupboards or at a height where they did not have to reach up too high in their kitchen. We also talked a lot about obstacles that were in the way like scatter rugs and boxes. We also the conditions that individuals were living in. The woman who used the scooter did quite well in her home, but she was not able to visit friends as the environment was not accessible.
I am now going to turn it back over to Danny to talk about some of the quantitative results.
Research Study-Quantitative
- Existing database
- Inform intervention
Danny: For the quantitative analysis, I was brought on to help look at their aims from their initial grant and analyzing to see if there was a relationship between any of the risk factors that they were interested in, like substance use and falls. I was personally interested in looking at the functional or physical activity piece.
Existing Database
- Descriptive Cross-sectional study (Baseline)
- Participants: 248 (Mean age= 52.3, SD= 10.4) PLWH and substance use
- Primary Care Clinic & Community Health Center
- Inclusion Criteria
- Documentation of HIV
- Past year substance dependence
- Ability to speak English
- 18+
- Willingness to provide contact information
To start, I looked at the baseline data collection. I looked at it as a whole sample, and then I divided it up into people who fell and people that did not fall to see if there were any significant differences in the assessments that they did to decide the best way to intervene.
From their baseline, I ran a cross-sectional study. There were 248 participants total that I analyzed, and the mean age was 52 years old. If you think back to when I was talking about my background, middle-aged participants, or middle-aged people living with HIV have a similar fall rate as older adults. Thus, this sample size was perfect to analyze people living with HIV and falls. These people were recruited from a primary care clinic, which was hospital-based, and a community-based health center serving the homeless population in downtown Boston. The inclusion criteria were documentation of HIV, a past year of substance dependence, the ability to speak English, 18 and older, and a willingness to provide contact information. Being able to provide contact information was very key for follow-up as this was a cohort study.
Experimental Procedure
- In-person interview
- Demographics
- AIDS Clinical Trials Group Fall History Questionnaire
- 14-Day Timeline Follow back
- Modified Falls Efficacy Scale
- Center for Epidemiologic Studies Depression Scale Short
As for the experimental procedure, when participants came into the study, they were first interviewed and then many assessments were conducted. I will just highlight a few of them. For demographics, they were asked about their education level, marital status, and level of social support. To gather information regarding falls, the AIDS Clinical Trials Group Fall History Questionnaire was used. It asks questions such as, "Have you had a fall in the last six months?" Following this fall, "Did you seek medical attention?" And, "Did these falls lead to a fracture?" To capture alcohol use, a validated 14-day timeline follow back was used. Looking at the fear of falling, the Modified Falls Efficacy Scale was used. This scale provides examples of a variety of ADL tasks and how confident you are that you can do the tasks without falling. Item examples were walking into a shower or cooking. Depression was captured using the Center of Epidemiologic Studies Depression Scale. Many of these things feed right into the frailty phenotype. Everything was embedded to address that mediator that was part of the conceptual model.
Physical Tests
- Short Physical Performance Battery (SPPB)
- Static balance
- Side-by-side
- Semi-tandem
- Tandem
- Single leg stance
- Dynamic balance
- Chair stands
- Repeated chair stands
- 4m walk
- Static balance
- Grip Strength
The Short Physical Performance Battery was used. It is a group of tests that combines the results of gait speed, chair stand, and balance tests. It has been used as a predictive tool for possible disability and to aid in monitoring mobility. For static balance tests, there was a Side-by-Side, Semi-tandem, Tandem Stand, and Single Leg Stance. For dynamic balance, there was a Chair Stand, Repeated Chair Stand Test, and the Four-meter Gait Test. Lastly, they measured grip strength using a handheld dynamometer.
Quantitative Findings
- Demographics
- 14.5% Experienced homelessness in the past 6 months
- Age: 52.28
- 75.4% Unemployed
- 35.5% Heavy drinking past 14 days
- Living environment
- Unstable/chaotic environment
- Precariously housed
- Accessibility/barriers
- Basic needs are a priority
- Support/Assistance unreliable/inconsistent
As for the quantitative findings, this is just the overall sample. Fourteen point five percent of the participants experienced homelessness in the past six months, and this was defined as at least one night out on the streets or without shelter. The average age was 52, and over 3/4 of them were unemployed. And, 35.5% experienced heavy drinking in the past 14 days. Taking all of this demographic information together, this speaks to what Christine said about how their living environment was very unstable, and they were precariously housed. They had a lot of barriers to accessibility, healthcare, and other support. It also highlighted that basic needs had to be addressed in fall intervention prevention strategies as well.
There was 34% of the cohort who fell in the past six months, with 65% experiencing a repeat fall within those six months. One-third of the people that fell were similar to older adults, and it is similar to what previous literature shows us about people living with HIV and what their fall rate is. Then, when we divided them up by people who fell and people that did not fall, and there was a significant difference in alcohol use in the past 30 days with people who fell, having more days of alcohol use as noted in Figure 2.
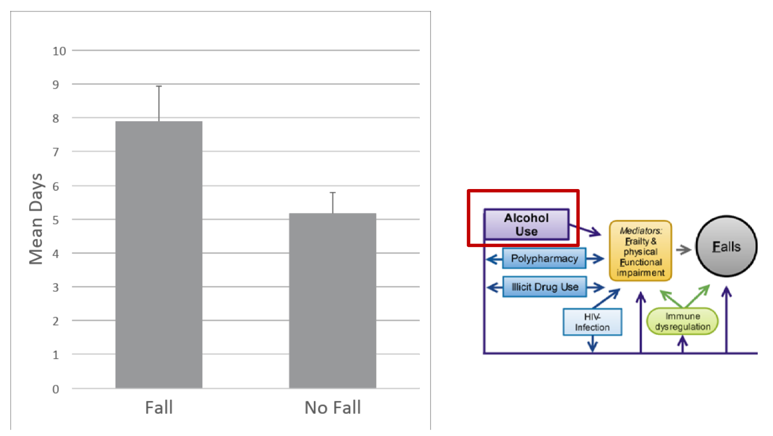
Figure 2. Graph showing falls with alcohol use.
As for the Short Physical Performance Battery, people who did not fall scored much higher, and there was a significant difference between people who fell and did not fall (Figure 3).
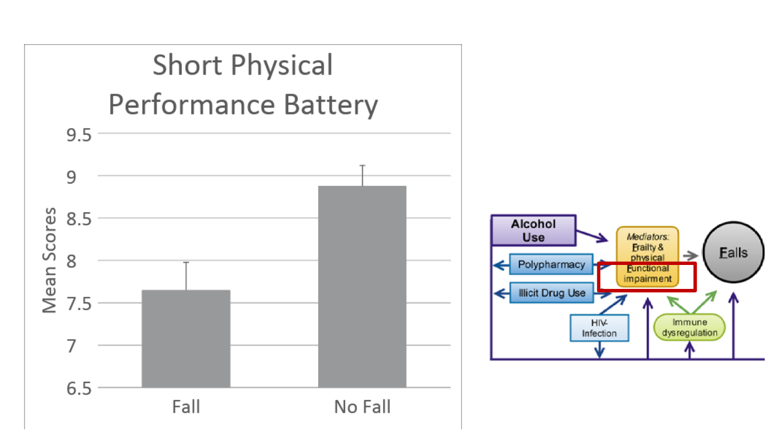
Figure 3. Graph comparing falls versus no falls using the Short Physical Performance Battery.
Interestingly, if you look at these results, people (who have HIV) who fell and did not fall scored under a 10, which is indicative of a lower extremity disability or mobility limitation. And, 14.5% experienced homelessness in the past months This was actually significantly different between people who fell and people that did not fall as noted in Figure 4.
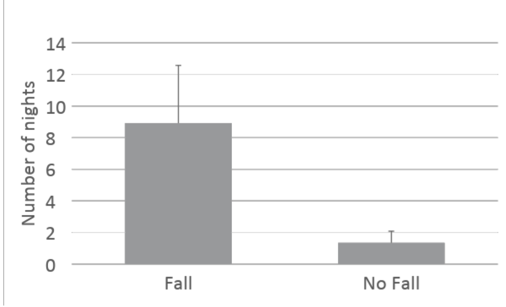
Figure 4. Graph comparing falls versus no falls with the number of nights homeless
In this graph, you can see that 14.5% experienced homelessness in the past months And, this was significantly different between people who fell and people that did not fall.
Fall Vs. Non-Fall Findings
- Sedatives
- Fatigue
- Light-headed
- Concerns with losing balance
- Depression
- Self-Efficacy
Above are some of the other findings that are significant in people who fell. The first is the level of sedative use, which is consistent with fall prevention literature. Sedatives and tranquilizers are highly associated with falls. Additionally, there is fatigue and a feeling of lightheadedness which were reported. Lightheadedness is a side effect of their medication. There were also concerns about losing balance, self-reported depression, and falls efficacy.
PLWH-OT Lens
Taking these results together and viewing them from an OT lens, it helps inform the intervention themselves (Figure 5).
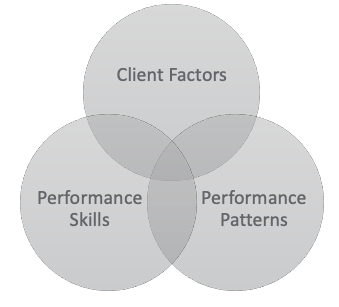
Figure 5. Occupational Therapy Practice Framework graphic.
Client factors are specific capacities, characteristics, or beliefs that reside within the person and influence their performance in occupations. The demographics of the sample, the interviews, and the focus groups informed us that many of these participants had a stigma due to their HIV status. Looking at the quantitative piece, we can see that many have frailty and decreased mobility, which might limit their interactions with their environment and also increase their likelihood of falls.
Performance skills are goal-directed actions that are observable as small units of engagement in daily life occupations. In our intervention, we hope that if we use home exercise to develop strength, coordination, and endurance to help mitigate fall risk, these aspects of exercise will be motivated by having goal setting. I will talk about this a little bit later in the presentation.
Lastly, performance patterns are habits, routines, roles, and rituals. There was much anxiety in this population. Additionally, there was a lack of social support. We must take a pretty expansive role when we are adjusting fall risk. We cannot just look strictly at physical limitations, but look at the person with a holistic view.
All these areas are used and considered as areas that we can intervene in our intervention.
Other Considerations
- Bhasin et al., 2020
- Limitations informed the intervention
- MOS-HIV
- Difficulty reasoning and problem-solving
- Trouble with attention
- Skip meals or insufficient resources
Some other considerations that we used to design our study and our intervention was a paper published in the New England Journal of Medicine by Bashin and colleagues this year. Their limitations informed the intervention, and I will talk about them throughout as I talk about the intervention itself. The recommendations that were made in this paper were unable to be followed by some participants because they had barriers due to travel, co-payments, and insurance coverage. This was especially pertinent in our population because we found that they are under-resourced and are dealing with homelessness and food insecurity. This was definitely a limitation that we hope to address in our intervention.
The MOS-HIV is a cognitive function questionnaire specifically for the HIV population. Through my quantitative analysis, we found that the sample as a whole had difficulty with reasoning, problem-solving, and trouble with attention. Like Christine mentioned, sometimes they need reminders because they might even skip a meal or have food insecurity.
Fall Risk Assessment
- CDC STEADI Algorithm for Fall Risk
- Stay Independent: 12 question tool
- Three clinical questions
- Feels unsteady when standing or walking?
- Worries about falling?
- Has fallen in the past year?
- If YES- ask, “How many times?” “Were you injured?”
The CDC STEADI is a screening tool that we use to test eligibility. What is presented in this slide is a standardized fall risk algorithm from the CDC. You can use either the validated 12 question tool, which is called Stay Independent, which I will talk about in further detail on the next slide, or these three clinical questions that were part of the algorithm. The three questions were: feels unsteady when standing or walking, worries about falling, or has fallen in the past year. If a participant that you are screening says "Yes" to any of these three questions, they are categorized as high-risk for falls.
- Stay Independent: 12 question tool
- I have fallen in the past year.
- I use or have been advised to use a cane or walker to get around safely.
- Sometimes I feel unsteady when I am walking.
- I steady myself by holding onto furniture when walking at home.
- I am worried about falling.
- I need to push with my hands to stand up from a chair.
- I have some trouble stepping up onto a curb.
- I often have to rush to the toilet.
- I have lost some feeling in my feet.
- I take medicine that sometimes makes me feel light-headed or more tired than usual.
- I take medicine to help me sleep or improve my mood.
- I often feel sad or depressed.
This is the 12 question tool, Stay Independent. If a participant says "Yes" to any of these questions, they are going to be receiving a score of either a one or two. And if they answered, "No," then there will be a score of zero. After the conclusion of all these questions, you would add up the score. If the score is over four, the person will be labeled as a fall risk.
For our study, we asked those three clinical questions (feels unsteady when standing or walking, worries about falls, and fallen in the past year). And if they said, "Yes," they were eligible for our study. And if not, we used the 12 question tool again because although those three clinical questions are incorporated in this 12 question tool, some questions are not. There might be some people that have not fallen yet, and they might not necessarily be worried about falling. However, they might say "Yes" to some of the other questions. I think it is helpful to identify people that might be at risk for falls that have not fallen yet, and this might be one of the best ways that we can intervene.
Pre-intervention Assessments
- Canadian Occupational Performance Measure (COPM)
- Gather info
- Vision
- Resources
- Medication
- Motor Function
- Short Physical Performance Battery
- Grip Strength
- Frailty
This is one of the first areas that was affected by COVID-19 as we were designing this study. As mentioned in my quantitative analysis, participants were recruited from primary care clinics and community health centers serving the homeless. And with many of those places running at lower capacity, in a temporary shutdown, or people living with HIV not wanting to engage in research during this pandemic, we had to narrow our focus. Instead of just having a broad recruitment setting, we used our existing participants from past studies and from our cohort, and we ran an analysis to see if they answered yes to any of those three clinical questions by proxy from any of the assessments. From this, we identified a pretty solid sample from using that method. Due to the pandemic, we had to think of some alternative ways to recruit.
Some of the measures for the intervention include a pre and a post-test, and these are both completed virtually and in-person. One of the limitations that was identified by one of the papers when we were developing this intervention was that sometimes if exercises are not tailored to the participant or are not recommended from a community health center, then participants might be less likely to adhere.
The first one is the Canadian Occupational Performance Measure. This is a client-centered outcome measure that helps provide the basis for setting intervention goals. The Canadian Occupational Therapy Measure allows us to know what motivates our client, and this will allow customization of the intervention itself. We wanted to gather similar information similar to what the cohort study looked over like a history of falls and falls efficacy. In addition to that, we know that vision is a major component to fall risk. So, we will be gathering vision information, as well as, additional data regarding resources, like the food insecurity piece that was highlighted in the qualitative analysis that Christine did.
For the motor function piece, this will be kept consistent. We will do the Short Physical Performance Battery and capture grip strength using the handheld dynamometer as these are two things that are directly related to the Fried Frailty Phenotype that I talked about a little bit earlier.
The pre-intervention assessments will be done virtually and also in-person. The COPM, questions regarding resources, and a current medication/substance use will be done virtually. For things that need to be done in-person, such as the Short Physical Performance Battery and grip strength, that will be done in person. And, the intervention (exercise) is entirely virtual. We also have 10 video and phone group sessions and weekly phone check-ins with an occupational therapist to provide problem-solving and support.
The home exercises will be done three times a week for 10 weeks, and these exercises will be taught in person during the pre-intervention assessment. Participants will be provided video clips as reminders as we know that memory might be disrupted in this population. This was something that was highlighted as something that should be emphasized by the focus groups. This was also supported via the phone check-ins. The phone check-ins will also be used to help address any questions regarding the exercises and any challenges related to falls during the previous week.
From the qualitative piece, we found that participants really love the piece where they can meet as a community and talk amongst each other. This was something that happened during the focus groups. Everyone got really close, especially during the pandemic. That social piece is something that is missing thus was included in our intervention. We will also encourage participants to turn off their cameras if they want to. During the qualitative piece, we found that some participants did not want to broadcast their surroundings.
Interventions
- Areas addressed
- Motor Function
- Assistive Devices
- Reminders
- Strategies for adapting the environment
To summarize, our interventions will address motor function, strength, and endurance using the exercises, and they will be tailored to each participant's level of fitness. We will also look at assistive devices, which were indicated as areas of need in the qualitative analysis. The need for reminders will be addressed with these weekly phone calls and strategies for adapting the environment. This will be implemented during the weekly phone calls to help adapt each participant's environment to mitigate any fall risk. These can be simple things such as removing throw rugs, enhancing lighting, and other kinds of suggestions.
Post-intervention Assessment
- COPM
- Gather info
- Vision
- Resources
- Medication
- Motor Function
- Short Physical Performance Battery
- Grip Strength
- Frailty
Lastly, the post-intervention assessments will the same as the pre-intervention assessments. Now, I will turn over the mic to Simone, and she will talk a little bit about lessons learned and any takeaway points.
Take Away Points
- Recruitment
- Passive
- Recruit participants from previous studies
- Intervention
- Hybrid
- In-person
- Assessments
- Virtual
- Groups
- Home exercise
- Hybrid
- Assessments
- In-person
- Hybrid
Simone: There were some lessons that we learned from our studies with these participants, and some of them had to do with the special population that we were working with and others had to do with pivoting due to the COVID-19 climate that we are in right now. One area includes recruitment. We, and other studies, have certainly recruited by hanging flyers in particular areas, perhaps places where participants receive medical care, and those can be effective. However, especially with this population, passive recruitment is not as advantageous. Having someone who can, if possible, physically go and meet with groups of participants who might be interested in taking part in studies would be wonderful. As Danny said, we have access to a cohort of participants who are in another study who then could participate in ours. A part of that advantage includes being able to create a relationship with participants, particularly when they are part of a vulnerable population, and to create a relationship and trust with that client. This not only helps them to participate or, hopefully, decide to participate in your studies, but also gives them the level of comfort to really be able to feel comfortable enough to ask questions and make sure that they are treated in the way that they should be when they are engaging in studies with us.
Another aspect of altering our recruitment a bit for this population includes the importance not only of interactions but the environment in which you are talking to participants. This includes making sure that you are not in a distracting environment and in a space that makes the participant feel comfortable enough to share details, that might be very personal. This is very important for vulnerable populations.
I talked a little bit about recruitment materials. Flyers are more of a passive form of recruitment and might not be as advantageous. If you do decide to use flyers, you may want to create materials that are tailored specifically to the population, involving information that they care about. We always compensate participants who take part in studies. But for this population, in particular, there are barriers to access that might influence their ability to participate. We need to make sure to provide compensation for transportation, parking, and so on if they are able to come in person. That is quite important. And last, in terms of recruitment, I want to bring up the debriefing process. With all studies, we debrief to let participants know what they took part in, why the study is important, and how it relates to them and the population that they are a part of. If you create a relationship with them, they feel comfortable enough to really ask questions that they might have during that debriefing period.
Danny talked about the intervention which we originally intended to be in person. Due to COVID-19, we pivoted to create a hybrid format so that participants could take part in person for some of the assessments. They also were able to participate virtually. The advantage of participating virtually is that there are platforms, like this one that we are using today, that really help to increase the access to some participants who might not be able to make it in for the sessions due to the barriers mentioned earlier. Interventions can take quite a bit of time. Participants may have to go several days a week to a particular site. But with a virtual format, they can take part and not necessarily have to physically go visit a site. The other piece that is advantageous, in terms of a virtual format, is that during COVID-19, it facilitated the ability for us to also include a group portion. Participants talked about how important it was for them to have support from other people who are a part of their population and who really understood what they were going through. Thus, we really saw the richness that shifting to a virtual format.
In terms of home exercise, having a virtual format means that you are not necessarily going to include equipment that is traditional for physical activity interventions. For example, clients in other studies might be asked to go to a setting that has special equipment that you might find in a gym. This is obviously not something we are doing during COVID-19. Home exercises increase access to physical activity for clients who might not have the equipment, and then hopefully, this leads to their ability to continue to do that after the intervention. In contrast, clients who come in and use your specialized equipment for eight weeks and then do not have access to that kind of equipment later might find this hard to generalize that to their everyday lives, and hopefully, reducing fall risk. We also did a hybrid format for our assessments as some of them could be conducted over the phone. Lastly, l will say that in terms of confidentiality, people who are part of vulnerable populations might not necessarily want to be seen visually on a video chat but can still participate by turning their cameras off and talking to the group. We also saw that as a very huge advantage for this population so that there were multiple ways in which they could participate and hopefully still benefit from the intervention.
Christine: I can also talk a little bit more about our focus group as related to the pandemic and participating in the intervention. As you have heard multiple times in this presentation, people were very excited to be part of a group and have that interaction with other people. We saw this pre-pandemic with the interviews that I did, which is typical to see in a narrative interview, but it was really most striking in the focus groups. Because in the focus groups, we had a really hard time getting people to stop talking. The RAs were very concerned about how I was going to do a virtual focus group with people just on the phone as it is much harder than it would be in Zoom. There was more talking over each other because they all wanted to participate. I did not have to do any teeth pulling to get people to participate and they did not want to end. The more that they went on, the more they would get off-topic. Somebody would talk about needing adaptive equipment, like needing a medical bed, and someone else would say, "Oh, I have one. I know where you can get one." They wanted to start exchanging phone numbers and emails. When at the beginning, they did not even want their name shown. They also talked about the desire to get out of their homes during the pandemic, both to get away from their children and to get away from the other people in their house, They felt trapped. Again, the mobility impairments made it more difficult. People who were homeless, living in shelters, or "couch surfing" were able to participate in the focus groups just fine. Although, many times they were outside as you could hear cars, sirens, et cetera. Thus, I think there will be no problem with them participating in the intervention itself. Another time it was raining and I was afraid that no one would show up. However, they made it. My experience in working with people with homelessness is that their sense of resourcefulness is just really amazing.
Questions and Answers
What was the size of the focus group and did the size vary?
The focus groups were between three and five participants. They were pretty consistently around four. We kept them smaller than we would have done if we had been in person. We recruited up to seven to eight, knowing that we would probably get about half of that.
When do you expect to release the results from the intervention and where will we be able to find them?
We are hoping to conduct the intervention this winter and spring since we have pivoted to a format that can be done during COVID-19, and we would be happy to share those results once we have written that up.
Where was this study conducted?
We are located in Boston, Massachusetts, so that is where we conducted the study.
After the intervention, did the fall rate go down? Did substance abuse patterns change?
That is a great question because we know that our collaborators have told us that their substance abuse patterns have decreased over their time in that study. We are looking at their fall rate, but we do not yet know whether their fall rate has decreased. That is a part of what we will be examining.
Do the reported cognitive issues stem from medication, environmental factors, comorbidities, or a combination?
Danny, would you like to take that question? Sure, I think it would be an interaction of all those things. I do not think we will be able to definitively say it is one thing over another, but maybe one of them would exasperate it. However, I would say it is an interaction between all those factors listed.
What did they most want to talk about? Personal needs or general issues? Chris, if you would not mind taking that one.
It was a combination. They talked about their personal needs. What was really striking was how common those were across the group. I see another couple of questions here that are related to the focus group, so I will just answer those real quick too. The study did not provide internet access for the focus group piece but that is something that we have looked at doing for the actual intervention if there is anybody who does need internet access or does need to use an iPad or something like that. There are some resources that I think we will be able to provide for people. The version of Zoom that we used was a more protected version because this was research, and we were going through the Institutional Review Board. We had to be very careful about any identifications. This was another reason that we did not record the video part of it. We only recorded the audio part, and we had that transcribed by a service that signed a disclosure agreement. The clients that participated in the focus groups also signed a confidentiality agreement as part of their consent form, as you would do in any research study.
How would your client disclose their experiences with other treating professionals? Do they sign disclosures to share information? How did they improve their environment to do modifications to the environment? Did you allow any other family members to share in the groups?
The participants in the groups were just the clients themselves. There were no other family members in the groups, and they were free to address anything that they felt was important to them during that time. This could include information about other treating professionals. As the information is confidential, we would not talk about who those individuals were, but instead, we only gathered information about themes that emerged from the conversation.
Resources
Available in the handout.
Citation
Gill, S., Helfrich, C., & Shin, D. (2020). OT's mental health response to the COVID pandemic: The medically complex client with HIV. OccupationalTherapy.com, Article 5374. Retrieved from http://OccupationalTherapy.com


