Editor's note: This text-based course is a transcript of the webinar, Pelvic Muscle Dysfunction And Continence Improvement: A Primer For Occupational Therapy, presented by Kathleen Weissberg, OTD, OTR/L.
Learning Outcomes
- After this course, participants will be able to identify urinary incontinence (UI) treatment guidelines, the direct impact of UI on occupations of the elderly population, and describe normal bladder and pelvic muscle function.
- After this course, participants will be able to recognize the pathophysiology of transient (acute) and established (chronic) urinary incontinence.
- After this course, participants will be able to list occupation-based assessment and management strategies for various types of incontinence, including effective behavioral treatment strategies, and state how to set up and facilitate a Multi-disciplinary Team Continence Improvement Program.
Introduction
Thank you for joining us today. I'll begin with an overview of the topic, and then we'll address some important considerations and regulatory aspects. In this session, we will be discussing continence and incontinence from various perspectives.
Let's first consider the perspective of the patient or resident you may be working with, whether it's in a home care setting, outpatient situation, or skilled nursing facility. Imagine you are at home and experiencing urinary incontinence issues. Your family believes the problem is worsening and suggests you move into a skilled nursing facility for better care. Upon arrival, you face challenges, such as wetting or soiling yourself, leading to social isolation and a decline in your usual sociable behavior.
Next, let's explore the regulatory perspective. If you are involved in areas like estate surveying or Medicare, you may be looking for ways to reduce healthcare costs. It's important to understand the financial burden that urinary incontinence places on the healthcare system. This raises questions about why guidelines are not being strictly followed and why more proactive measures are not being taken.
As someone working in a skilled nursing facility for an extensive period, you may be concerned about the number of residents experiencing urinary incontinence and the associated costs. You wonder if there are ways to improve the situation and provide better care.
Finally, let's consider the perspective of us, the clinicians, such as occupational therapists. While specialized biofeedback training is not a requirement, it's essential to acknowledge that we can still make a difference in addressing urinary incontinence. This session aims to serve as a primer and help you realize that there are actionable steps we can take to improve the quality of life for those dealing with this condition.
Bowel incontinence is indeed a separate and important topic that we can address in the future, but for now, let's concentrate on urinary incontinence and the specific issues related to it. By narrowing our focus, we can delve deeper into understanding and managing this particular concern effectively. Let's proceed with our discussion on urinary incontinence and explore the various perspectives and solutions within this scope.
Scope of the Problem
Let's now delve into the scope of the problems related to urinary incontinence.
Statistics
- Over 25 million adult Americans experience temporary or chronic urinary incontinence.
- This condition can occur at any age, but it is more common in women over the age of 50.
- Prevalence
- Women – 61%
- Men – 3-10%
The current statistics reveal that more than 25 million American adults are affected by temporary or chronic urinary incontinence. While this condition can occur at any age, it is more prevalent in women, especially those over the age of 50 and those who have experienced pregnancy or vaginal delivery. In women, the prevalence of urinary incontinence is approximately 61%, while in men, it ranges from 3% to 10%. However, it's important to note that the actual rates for men might be higher, as they tend to be less open about discussing these issues, leading to potential underreporting.
Comparing these figures to past estimates, we can observe a significant increase in the reported numbers. Previous estimates ranged from 38% to 49%, suggesting that within the last five to ten years, there has been a dramatic rise in the prevalence of urinary incontinence.
This data underscores the importance of addressing this concern from multiple perspectives, considering the impact on individuals, the healthcare system, and skilled nursing facilities.
Risk Factors
- Population aging
- Greater than 70 years
- Obesity prevalence
- Body mass index >40
- Vaginal birth
- Smoking
Understanding the risk factors associated with urinary incontinence is crucial in developing effective interventions. One significant risk factor is population aging. While urinary incontinence is more commonly observed as people age, it is essential to emphasize that it is not a normal part of the aging process. However, the risk of urinary incontinence does increase with age, particularly after the age of 70.
Another risk factor is obesity, with individuals having a body mass index (BMI) greater than 40 being at a higher risk of developing urinary incontinence. Interestingly, overweight women are also more prone to incontinence compared to those with an ideal body weight. Research has shown that weight loss in significantly overweight women with incontinence can reduce episodes of unwanted urine loss.
Vaginal birth is another significant risk factor, having a strong association with urinary incontinence, particularly in women. Additionally, smoking is known to be a contributing factor as tobacco smoking can cause chronic coughing. For individuals, especially those with stress urinary incontinence, who also smoke, the recurrent downward pressure on the bladder during coughing can exacerbate leakage. Therefore, smoking cessation is recommended as a first-line approach to reduce or eliminate some of these stress urinary episodes.
Statistics, Cont.
- Urinary incontinence has been estimated to affect between 50% and 65% of nursing home residents.
- At least 11% report UI at admission to hospital, and 23% at discharge.
- At least 3 million are affected by fecal incontinence and/or defecation problems.
- Denial is common.
Additional statistics shed further light on the impact of urinary incontinence in various healthcare settings. In nursing homes, the prevalence of urinary incontinence is estimated to affect anywhere between 50% to 65% of residents, with some facilities reporting even higher rates depending on their approach to managing the issue.
Interestingly, 11% of individuals report experiencing urinary incontinence upon admission to the hospital, and this figure increases to 23% at the time of discharge. Additionally, studies have revealed that some individuals entering nursing homes without any chronic cognitive disorders, such as dementia or Parkinson's, and who are initially functional, independent, and continent may develop dependency and urinary incontinence within six months to a year, seemingly without any underlying disease process triggering these changes.
Several factors contribute to this phenomenon. In hospitals, catheter use, immobility, medication interactions, and poor staffing may play a role in the development of urinary incontinence. Urinary tract infections (UTIs) are also prevalent in hospitals and can contribute to or worsen incontinence.
Regrettably, some patients may refrain from speaking up about their incontinence issues due to various reasons, including fear of being placed into a nursing home by their families. This fear is not unfounded, as incontinence is indeed a key factor considered in determining the need for nursing home placement. Moreover, the issue may be magnified in skilled nursing facilities, leading some individuals to remain silent about their challenges with urinary incontinence.
Tag F690
- Providers are responsible for ensuring that a resident who is continent of bladder and bowel on admission receives services and assistance to maintain continence unless his/her clinical condition is/becomes such that it is no longer possible to maintain continence.
- Urinary incontinence is not a normal part of aging.
When discussing nursing homes, it's important to highlight Tag F690, a significant guideline in state surveys that industry professionals are well-acquainted with. This tag emphasizes the responsibility of providers to ensure that residents admitted with bladder and bowel incontinence receive the necessary services and assistance to maintain continence, except when their clinical condition makes it impossible. Conditions such as dementia or Alzheimer's may be relevant factors to consider in such cases. Despite the fact that the prevalence of urinary incontinence increases with age, it is crucial to acknowledge that it is not a normal part of the aging process. Unfortunately, there is often a lack of awareness and education surrounding this issue, something that occupational therapy practitioners can play a pivotal role in addressing.
- A resident who is admitted with an indwelling catheter or subsequently receives one is assessed for removal of the catheter as soon as possible unless the resident’s clinical condition necessitates continued catheterization.
- A resident who is incontinent of bladder receives appropriate care and services to prevent urinary tract infections (UTIs) and, to the extent possible, restore continence.
When a resident is affected by urinary incontinence, the facility is required to provide services based on a comprehensive assessment. This assessment involves various healthcare professionals, each playing a specific role in addressing the resident's needs.
According to guidelines, if a resident is admitted with an indwelling catheter or later receives one, the facility must assess its removal as soon as possible unless there is a valid medical justification for its continued use. The goal is to ensure appropriate care and services for residents with urinary incontinence, aiming to prevent urinary tract infections (UTIs) and, where possible, restore continence, which is a reasonable expectation following a UTI. The regulatory intent related to indwelling catheters is to ensure that they are not used unless medically justified and that they are discontinued as soon as clinically warranted.
Throughout my extensive experience in this industry, I have encountered instances where residents were equipped with catheters when they may not have needed them, possibly for reasons unrelated to medical necessity. This highlights the importance of a thorough and diligent assessment process involving nursing, physicians, occupational therapists, physical therapists, and other healthcare professionals. Together, they collaborate to develop individualized care plans to address the unique needs of residents with urinary incontinence, promoting optimal care and outcomes.
Incontinence
- “Urinary incontinence is not normal.”
- 80% of cases see improvement without surgery
- Of skilled nursing
- 80% of them could have been toileted
Urinary incontinence is not a normal condition, and research has demonstrated that approximately 80% of cases can be improved through behavioral interventions. In this discussion, we will explore various approaches to address urinary incontinence, including staff collaboration, medication management, behavioral strategies, and exercises like Kegel exercises.
A noteworthy statistic in skilled nursing facilities is that 80% of residents are assisted with toileting. This highlights areas where improvements can be made, such as staffing and staff attitudes. Creating a positive impact is crucial, as instances of residents being disregarded when requesting toileting assistance can lead to potential urinary tract infections (UTIs) and other complications. As occupational therapy practitioners, we have an opportunity to make a significant difference in changing mindsets and attitudes and ultimately enhancing the quality of care provided.
By advocating for individualized care plans, promoting timely responses to residents' needs, and implementing evidence-based interventions, we can play a vital role in improving continence outcomes and overall well-being for those affected by urinary incontinence. Our contributions align with the guidelines for treatment, reinforcing the importance of a comprehensive and proactive approach to address this common and manageable condition effectively.
- Continuous process of consistently providing individualized care
- Completes a comprehensive, accurate, appropriate, and adequate exam
- Provides resident and family education
- Absorbent products should not be used as the primary long-term approach until….other alternative approaches have been considered
Providing individualized care is a continuous and essential process, which we often hear and acknowledge, but it requires a genuine commitment to living it in practice. Cookie-cutter approaches, such as toileting every two hours, do not align with individualized care. Instead, a comprehensive and accurate examination is crucial to determine the most appropriate and adequate treatment plan. In this industry, nursing typically takes the lead in this aspect, but occupational therapy, along with physical therapy, speech therapy, and pharmacy, play significant roles in ensuring a collaborative and holistic approach to care.
While absorbent products like pads can be used, they should not be the primary or sole method of managing urinary incontinence. Effective documentation must showcase efforts to explore other interventions first. Individualized treatment plans are essential, especially considering factors like cognition and comprehension, which significantly influence program effectiveness. Restoration programs cater to individuals who can actively participate and comprehend, while adaptive programs require staff involvement in implementing the plan.
Ultimately, the key takeaway is the importance of the least invasive evaluation and treatment methods, ensuring that the care provided is uniquely tailored to each resident.
Cost of Urinary Incontinence
The costs associated with urinary incontinence are multi-faceted and can be examined from various perspectives.
Clinical, Psychological, and Social Impact
- UI is often underreported, generally not identified, and when it is, often inadequately treated.
- UI imposes a significant psychological impact on individuals, their families, and caregivers.
Let's begin by examining the clinical, psychological, and social aspects of urinary incontinence. As previously stated, denial can contribute to underreporting and difficulty in identifying the condition. Even when identified, urinary incontinence may not always receive adequate treatment. There is a need for healthcare professionals with the skillset and willingness to address this issue effectively.
Family/Caregiver Psychosocial Costs
- Guilt
- Frustration
- Care-Giver Burden/Burnout
- Depression
- Risk of Mistreatment/Neglect
- Financial burden
- Institutional placement
Urinary incontinence not only affects the individual but also places significant psychological stress on their families and caregivers. Often, it becomes the primary reason for admission to long-term care settings, leading to challenges in socialization and participation in daily activities. From an occupational perspective, individuals may lose their sense of role as social beings, hindering their active engagement in life.
Family members and caregivers also experience a range of emotions, including guilt, frustration, depression, and burnout. They may struggle to provide the necessary care and support, feeling helpless in resolving the incontinence issue. This emotional toll can impact both the affected individual and their caregivers, limiting their ability to enjoy activities and outings together. There is also a risk of mistreatment, as individuals with urinary incontinence may face mistreatment or neglect in both home and institutional settings.
Anecdotal evidence highlights the reality of such mistreatment. In a five-star community, my aunt who had dementia and a UTI requested to use the restroom, only to be refused and left sitting in her urine as a form of punishment. Such incidents underscore the importance of addressing the psychosocial costs of urinary incontinence and providing compassionate care that upholds the dignity and well-being of those affected and their caregivers.
Individual Psychosocial Costs
- Psychosocial:
- Embarrassment/shame
- Anger
- Frustration
- Fear
- Depression
- Social restrictions
- Social isolation
- Quality of life:
- Loss of self-esteem
- Altered body image
- Impaired sexual functioning
- Lower quality of life
- Limited work productivity
Psychosocial costs associated with urinary incontinence encompass a wide range of emotions, including embarrassment, shame, anger, frustration, and fear. These feelings can lead to social isolation, adversely impacting an individual's quality of life. Issues with self-esteem and body image may arise as a result of incontinence, affecting one's sense of self-worth and confidence. The impact on sexual life and intimate relationships can be significant, as the fear of incontinence during intimate moments may cause distress and hinder sexual activity.
Furthermore, individuals of working age or those engaged in volunteering activities may face challenges in their respective occupations due to urinary incontinence, further impacting their overall quality of life. It is crucial to recognize that the psychosocial costs are not limited to urinary incontinence alone but also extend to bowel incontinence, which can be equally, if not more, distressing from a psychosocial perspective. Addressing these psychosocial factors and providing comprehensive support is essential to help individuals affected by incontinence maintain their dignity, well-being, and engagement in daily activities.
Cost of Complications
- Increased Risk of Falls
- Persons aged 60-80 form 53% urine while asleep
- More frequent trips to the bathroom
- Urine leaks on the floor cause falls
- The majority of falls occur while returning from the bathroom
- Disrupted Sleep
- Fatigue
When considering the physical aspect of urinary incontinence, bladder function plays a crucial role, especially in individuals aged between 60 and 80. During this age range, around 53% of urine is formed while sleeping, leading to more frequent trips to the bathroom at night, known as nocturnal urination. This can present challenges for seniors, particularly during nighttime awakenings when they may feel disoriented, encounter poor lighting, or lack the assistance of staff or family members. The location of assistive devices and potential hazards, such as mats on the side of the bed, can further complicate matters.
As a result, individuals may experience urine leakage on their way to or from the bathroom, sometimes leading to slips and falls. In some cases, they may not even remember the urine was present due to visual or cognitive factors. Disrupted sleep and increased fatigue from multiple nighttime trips to the bathroom can also impact an individual's overall well-being and performance of daily activities. This, in turn, may affect their role performance and engagement in occupations, highlighting the need for comprehensive care and interventions to address the physical challenges associated with urinary incontinence in this age group.
- Direct
- Skin irritations and infections
- Pressure ulcers
- Falls
- Urinary sepsis
- Physical activity restrictions
- Dehydration
- Medication side effects
- Indirect
- Drug side-effects
- Adverse drug effects
- Allergic reactions to drugs and materials
- Increased nursing care
- Lost wages
- Patient
- Family member
The following day may bring further considerations, like skin irritations, falls, dehydration, and medication side effects.
A common misconception among seniors is that they may believe reducing their fluid intake would be a suitable approach to managing incontinence. However, this is counterintuitive and not the best course of action. Decreasing fluid intake leads to higher medication concentrations and an increase in medication side effects, perpetuating a harmful cycle. We often encounter drug side effects and potential changes in roles due to these circumstances.
Cost of Incontinence
- Over $20 billion per year
- Most of that cost is spent on incontinence supplies and management, including pads and laundry.
- Routine care costs vary from $50 to $1,000 per person per year.
- Combined direct and indirect costs of UI amount to over $60 billion per year.
The annual cost of these issues amounts to over $20 billion. The majority of this expenditure is allocated to incontinence supplies, such as management pads and laundry soap. Routine care costs can vary significantly depending on the individual, ranging from $50 to over $1,000 per person per year. When considering both direct and indirect costs, the impact on our seniors reaches an astounding $60 billion.
From the perspective of skilled nursing facilities, the expenses are substantial. For instance, a community with around 100 to 200 beds could easily spend $10,000 to $15,000 per month on supplies alone.
Urinary Incontinence Costs
- Typical SNF resident is incontinent 5-7 times daily.
- Cost per incident without labor is $5.46 and $15.26 with labor.
While it may not be feasible to completely eliminate the issue of urinary incontinence, there is significant potential to improve the situation. On average, a person may experience incontinence five to seven times daily, incurring a cost of $5 per incident without factoring in labor, and $15 per incident when considering labor costs.
By focusing on reducing the frequency of incontinence episodes, we could achieve substantial cost savings. For instance, a 25% reduction would lead to savings of $6,500, not including supply costs. Similarly, a 50% reduction would yield even greater savings. However, it's essential to emphasize that the impact goes beyond financial considerations; it directly affects the well-being and quality of life of individuals, enabling them to be more active and engaged members of their communities. The potential positive impact is evident from the data presented in the accompanying slide.
Clinical Benefits of Treatment
- The National Institute of Health reported that a simple program of pelvic muscle exercises can reduce incontinent episodes by up to 86%.
According to a recent study reported by the National Institute of Health, a simple behavioral program that includes pelvic muscle exercises (commonly known as Kegels) has shown promising results in reducing incontinence episodes. The program can lead to a minimum reduction of about 29% to 30%, with some participants experiencing a remarkable 86% decrease in episodes. It is important to highlight that these positive outcomes are achieved without the need for surgical interventions, as the program focuses on non-invasive approaches.
As occupational therapy practitioners, we have the opportunity to make a significant impact by implementing these effective behavioral programs, improving the quality of life for individuals dealing with incontinence issues. While there are invasive options available as well, the study's results demonstrate the potential of non-invasive methods to bring about substantial improvements.
Anatomy and Physiology of Voiding
What is Continence?
- A state in which a person possesses and exercises the ability to store urine and micturate at a socially acceptable place and time.
Continence is defined as the state in which a person has the ability to store urine and exercise control over its release at a socially acceptable place and time. Incontinence, on the other hand, refers to the involuntary loss of urine, which can present as a social or hygiene issue and can be objectively observed.
When considering the definition of continence, it becomes evident that there are various points in the process where breakdowns can occur. These breakdowns may result from a range of factors, including medical conditions, muscle weakness, neurological issues, or other underlying causes. Identifying and addressing the specific factors contributing to incontinence is essential in developing effective interventions to manage or alleviate the problem.
Breakdowns in the process of continence can occur at various stages within the urinary system and the associated control mechanisms. For instance, problems might arise with urine production due to kidney dysfunction, affecting the filtration process that forms urine. Additionally, storing urine efficiently depends on the coordination between the bladder, sphincters, and urethra. Dysfunction in any of these components can result in difficulties with urine storage and possibly lead to incontinence.
What is Micturition?
- Storage and emptying of urine from the bladder
- Spinal reflex influenced by higher centers of cortical control combined with the ability to voluntarily relax the pelvic musculature will lead to normal micturition.
Figure 1 shows an overview of the system.
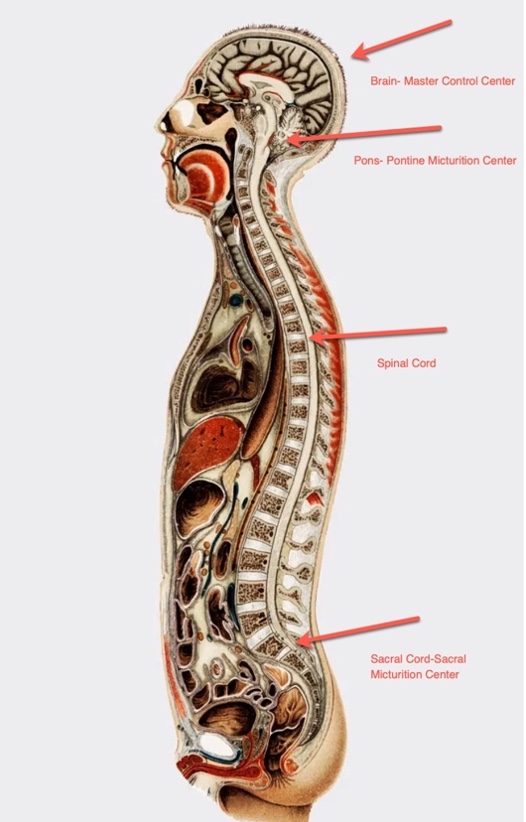
Figure 1. Lateral view of a person showing anatomical areas that control micturition.
The micturition reflex is another critical aspect to consider. Normally, the bladder fills, and stretch receptors within it signal the brain, initiating the micturition reflex when the appropriate time to void arrives. However, certain conditions like an upper motor neuron lesion or cognitive impairment can disrupt this reflex inhibition, leading to uncontrolled urination.
Nerve signals play a vital role in the entire urination process. Diseases, conditions, or injuries that damage the nerves involved can cause various urination problems. For example, conditions like diabetes, stroke, Parkinson's, multiple sclerosis, or spinal cord injuries can impact the nerves responsible for bladder function, leading to challenges in emptying the bladder.
The coordination between sensory and motor nerves is essential for the proper functioning of the urinary system. Sensory nerves, such as the parasympathetic nerves at S2-S4, provide feedback about the bladder filling sensation, while motor nerves control the detrusor muscle and the bladder neck for emptying. Understanding these interconnected processes helps us identify potential urinary issues and design appropriate behavioral interventions, such as Kegel exercises, to override the feedback loop and address certain urination problems effectively.
Figure 2 shows another graphic of the different areas of control.
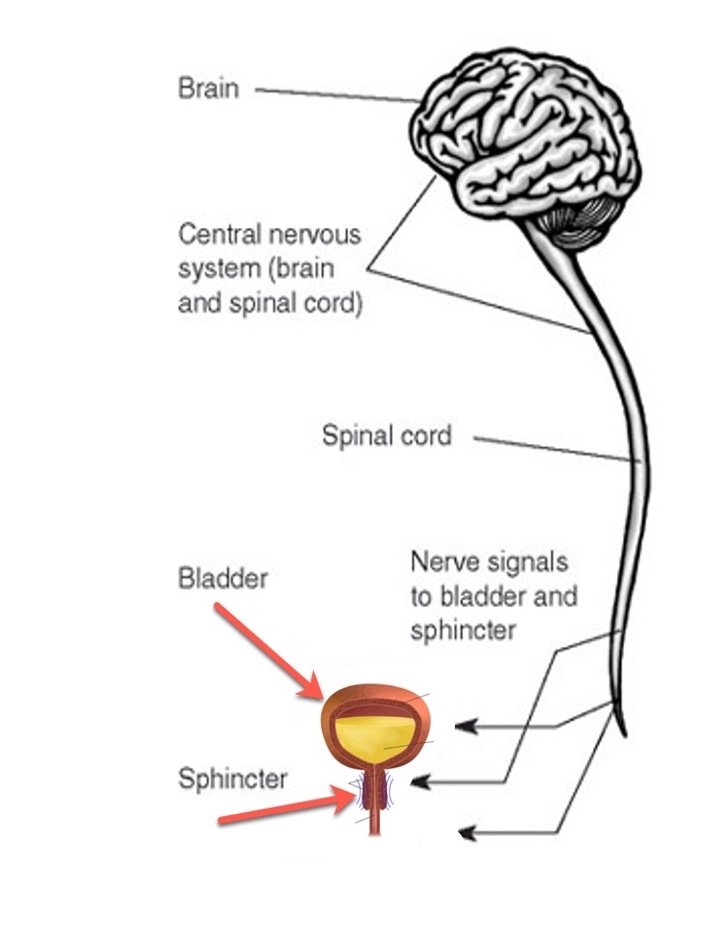
Figure 2. Another graphic shows anatomical areas that control micturition.
Urinary System Structures
- Kidneys
- Ureters
- Bladder
- Urethra
The urinary system comprises several essential structures that work together to maintain the body's fluid and waste balance. Let's take a closer look at each of these components. It is also shown in Figure 3.
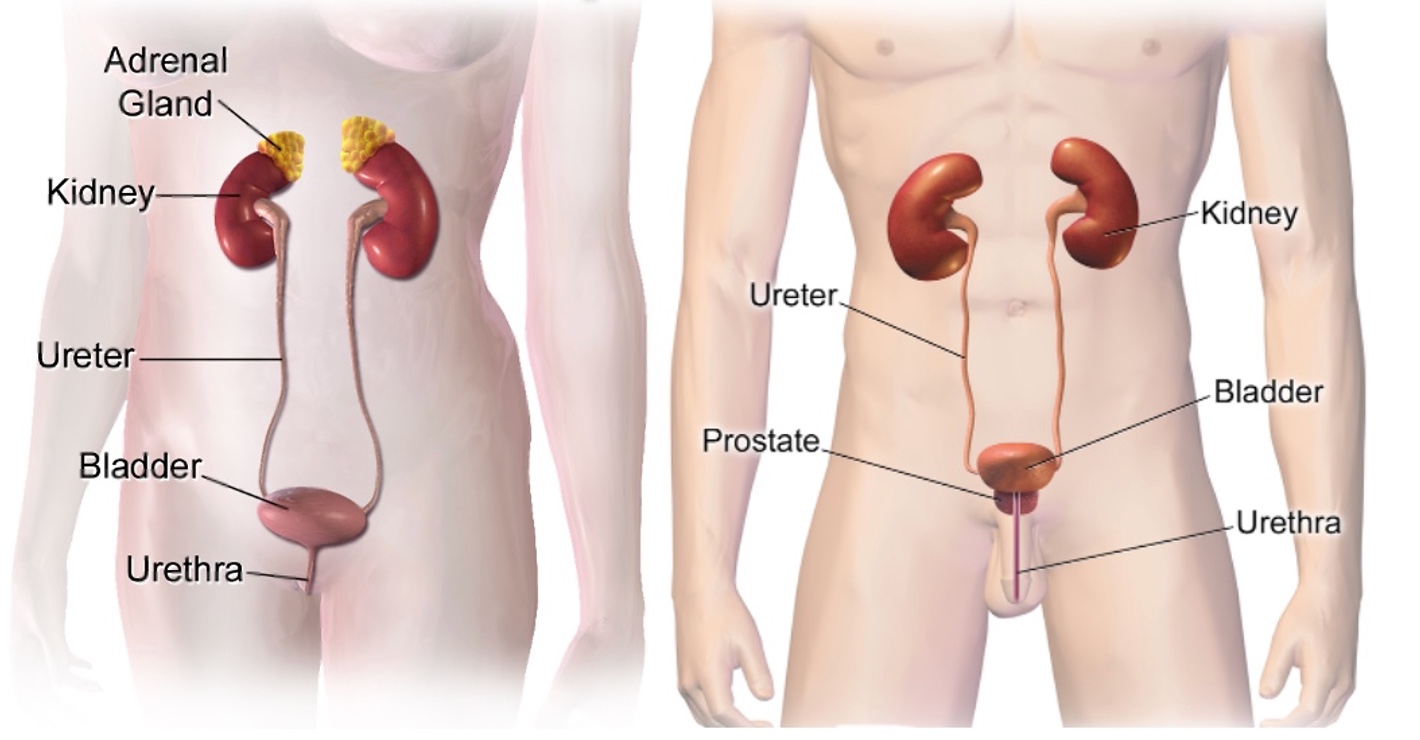
Figure 3. The anatomy of the urinary system for both a female and male
The kidneys, akin to two remarkable filters, are located on either side of the spine just below the ribcage. Their function is akin to that of a master chemist, responsible for filtering waste products, excess substances, and toxins from the blood to form urine. Just like a meticulous chef, the kidneys ensure that only the right elements are kept while the unwanted waste is discarded. For instance, they regulate the levels of substances like sodium, potassium, and calcium, ensuring our body stays in proper balance.
Picture the ureters as the reliable transport system connecting the kidneys to the bladder. These long, muscular tubes skillfully carry the produced urine from each kidney, like diligent couriers making sure the precious cargo reaches its destination promptly. Think of them as the conduits that facilitate communication between the kidneys and the bladder.
The bladder, also known as the detrusor, serves as a flexible reservoir for urine storage. It's akin to a well-designed expandable bag, capable of accommodating varying amounts of urine. The bladder can stretch to hold a substantial volume of fluid, and it remains relaxed while gradually filling up. When it's time for elimination, the detrusor contracts and exerts pressure on the stored urine, pushing it toward its final destination through the urethra.
Lastly, the urethra acts as the gateway for urine to exit the body. This narrow tube extends from the bladder to the outside world. Think of it as a security door, tightly closed to keep urine in the bladder until it's time to go. When that time comes, the urethra opens up, allowing the urine to flow out smoothly, like water through a controlled faucet.
Bladder/Detrusor
- Located behind the pubic symphysis
- Hollow muscular sack expands to hold + 1 pint of fluid
The bladder is also known as the detrusor. It is positioned behind the pubic symphysis and is described as a hollow muscular sac. The bladder has the capacity to expand and hold approximately one pint of fluid. Figure 4 includes cross-sections of both male and female anatomy.
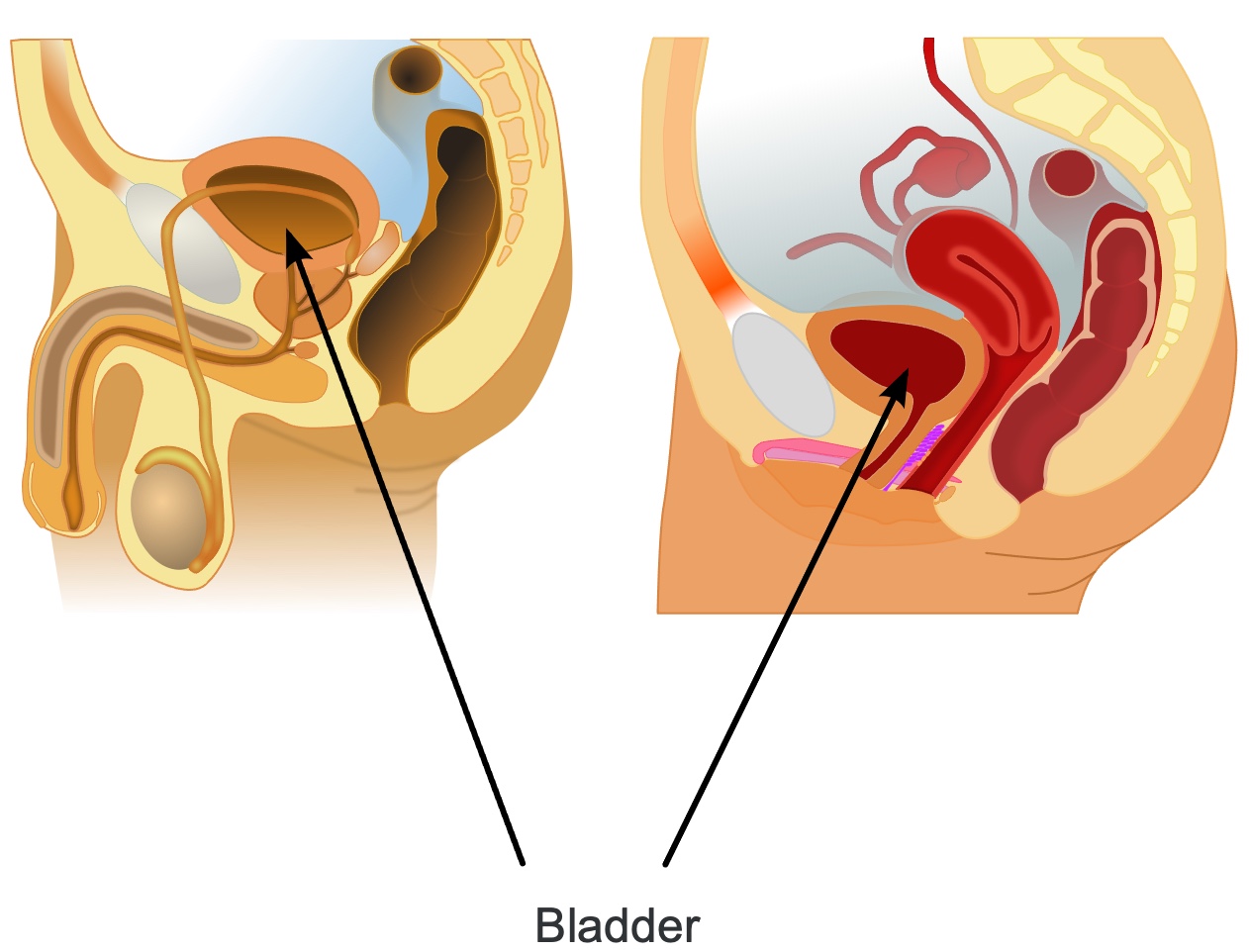
Figure 4. Graphics of the bladder or detrusor muscle in male and female anatomy.
In the female cross-section on the right, you can observe the bladder located just above the uterus. During pregnancy, as the uterus expands, it can exert pressure on the bladder, potentially leading to issues with urinary incontinence.
Likewise, in the male cross-section on the left, you can see the bladder positioned in front of the rectum. There is a close relationship between these two organs, and issues such as chronic constipation and incomplete emptying of the rectum could result in pressure on the bladder, leading to urinary incontinence as well.
Understanding the anatomical relationships and potential sources of pressure on the bladder is crucial for identifying the underlying causes of urinary incontinence in both male and female patients. Addressing these factors can help in developing effective management and treatment strategies for individuals experiencing urinary incontinence.
Urethra
- Hollow muscular tube
- Smooth muscle lining of the urethra contracts to keep urine from leaking or relaxes to let urine flow out
- Length of the urethra
- Males up to 20cm (length of the penis)
- Females 3-4 cm
The urethra is a smooth muscular tube that serves as the pathway for urine to exit the bladder and be voided from the body. In males, the urethra is considerably longer, approximately 20 centimeters, spanning the entire length of the penis. On the other hand, in females, it is much shorter, measuring around three to four centimeters (Figure 5).
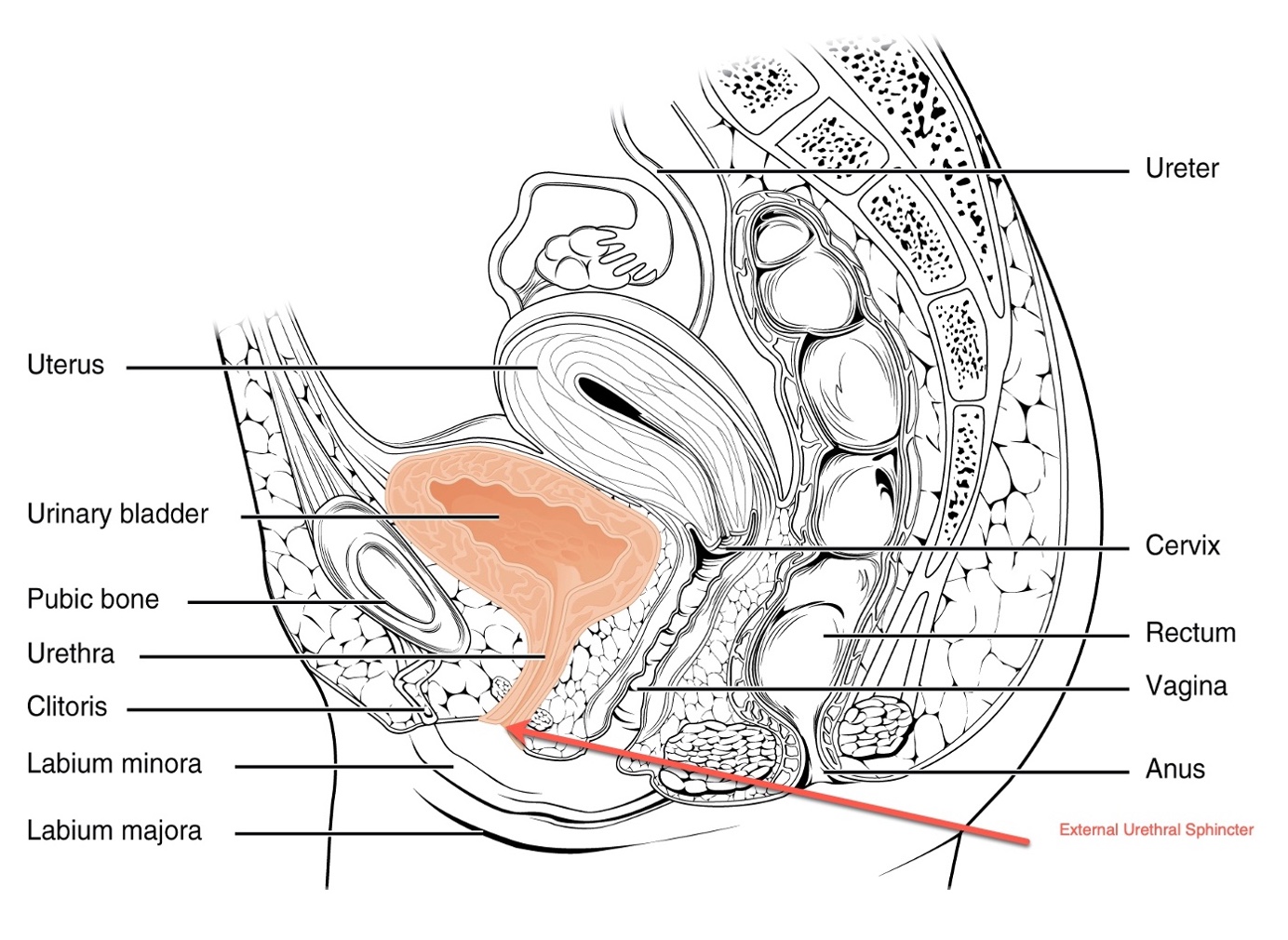
Figure 5. Example of the urethra on female anatomy.
The inner lining of the urethra contains smooth muscle, which contracts to maintain urinary continence, preventing urine from leaking out of the bladder when not desired. Conversely, when the person is ready to urinate, the smooth muscle relaxes, allowing the urine to flow out.
The urethra is equipped with sphincters—internal and external—which also play a crucial role in maintaining urinary control. These sphincters contract to keep urine in the bladder until it's time for elimination.
- Urethra gets support from the pelvic floor as it provides closure pressure on the urethra.
Additionally, the pelvic floor plays an essential role in supporting the bladder and the urethra. The pelvic floor is highlighted in yellow in Figure 6.
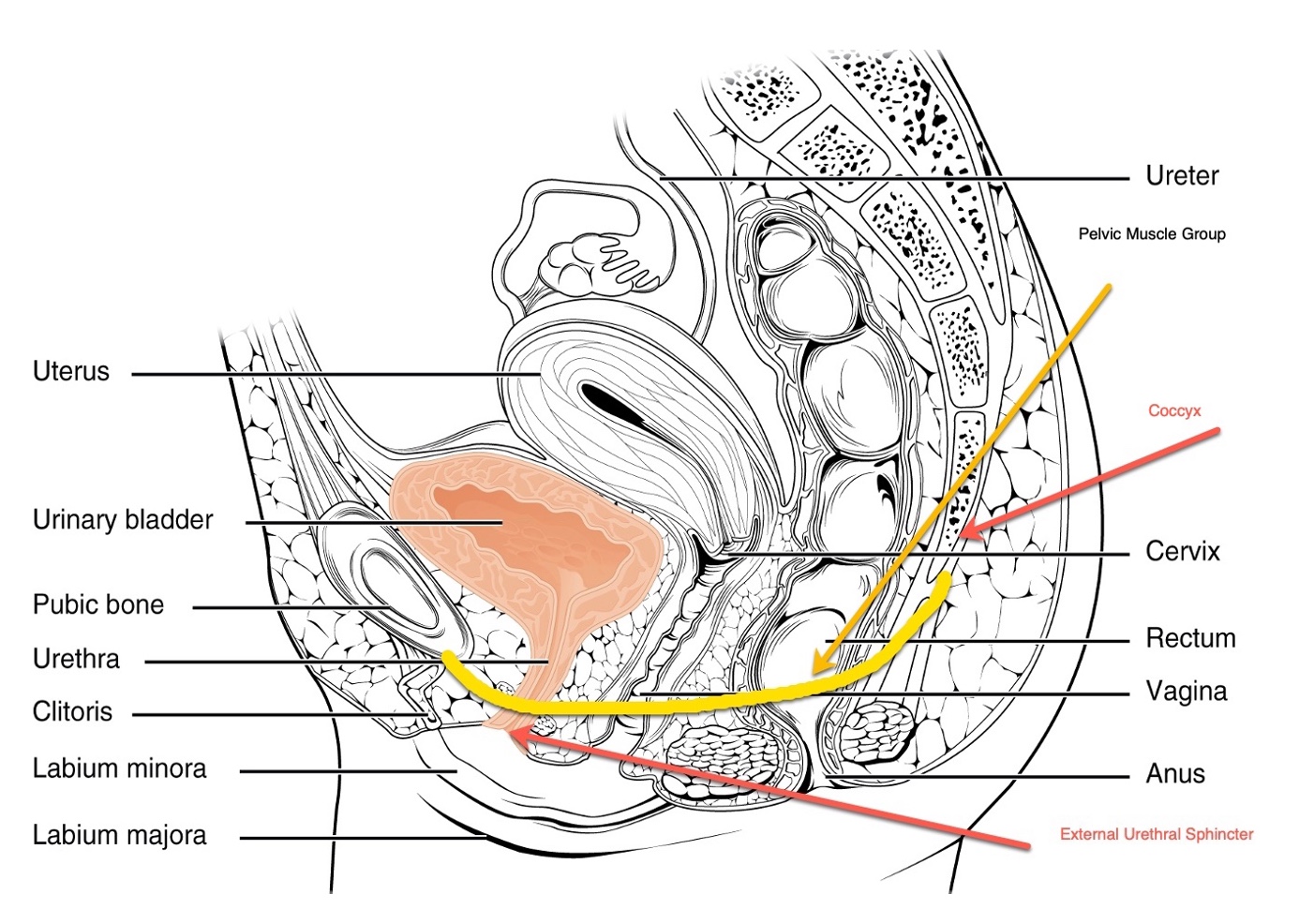
Figure 6. The pelvic floor highlighted on female anatomy.
The pelvic floor muscles, resembling a sling or hammock, contract to lift and support the bladder, particularly its neck. This positioning helps control the release of urine, allowing it to flow when needed and preventing leakage at inappropriate times.
In male cross-sections, you can observe the relationship between the urethra and other surrounding structures, providing further insights into the complex anatomy of the urinary system.
Understanding the interplay of the urethra, sphincters, and pelvic floor is essential in addressing issues related to urinary continence and developing effective strategies for managing urinary problems in both males and females.
Prostate
- Prostate is a gland which surrounds the neck of the bladder and the urethra in the male.
The prostate gland is situated just below the bladder, as shown in Figure 7, and it can be visualized in the cross-sections as the area right above the yellow pelvic floor line.
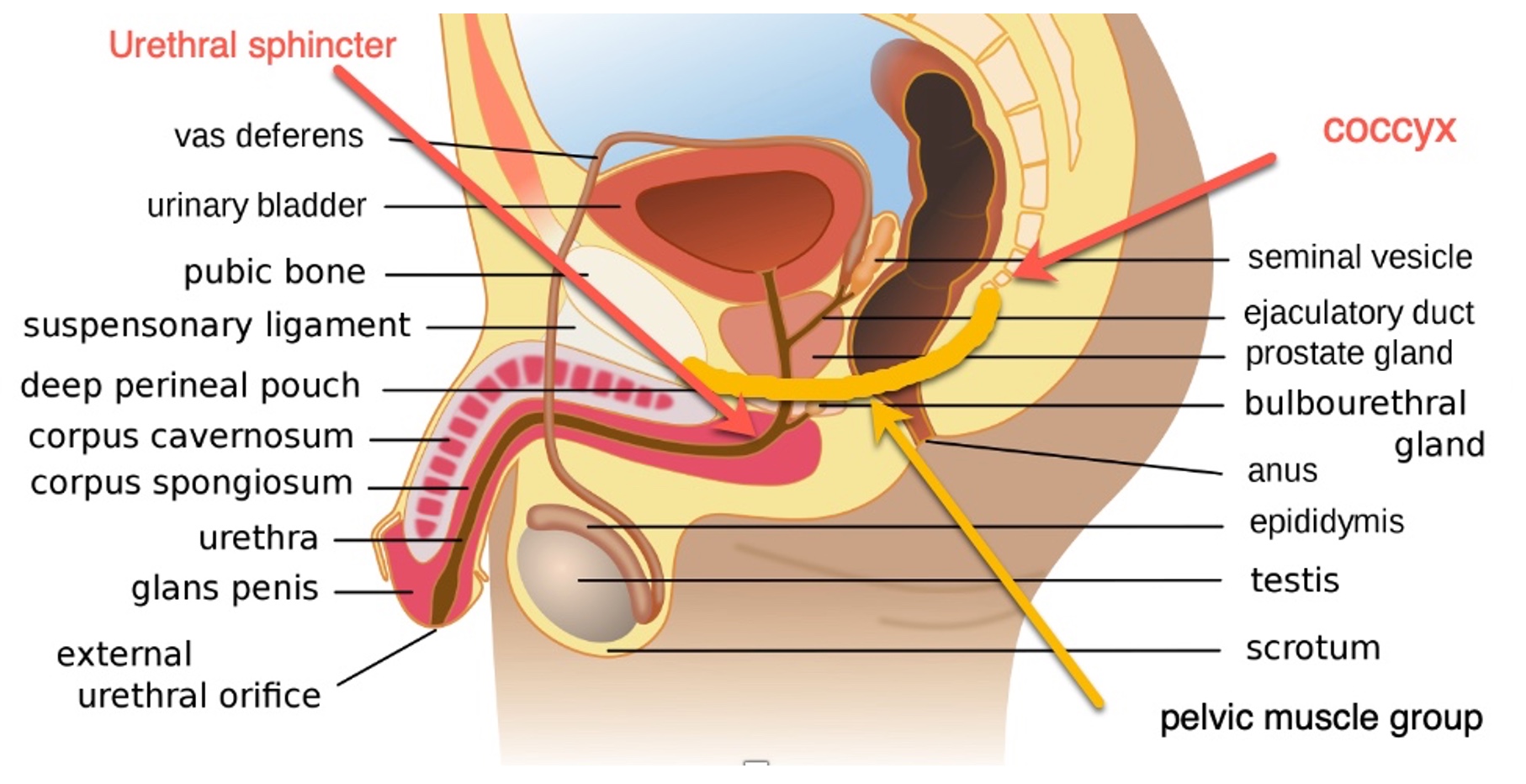
Figure 7. Graphic showing the prostate gland on male anatomy.
One important characteristic of the prostate gland is that it surrounds the urethra. As you can see, the urethra originates from the bladder, runs through the prostate, and continues its path until it exits the body.
The positioning of the prostate around the urethra can have significant implications for urinary flow. If the prostate becomes enlarged due to conditions like benign prostatic hyperplasia (BPH) or prostate cancer, it can obstruct the urethra, leading to difficulties in urination. In elderly men, BPH is a relatively common condition where the prostate gland gradually enlarges, potentially causing urinary problems by constricting or partially blocking the urethra.
This obstruction can significantly impact the flow of urine, causing hesitancy, a weak stream, incomplete emptying of the bladder, or even a complete stoppage. Depending on the severity of the enlargement or the presence of other prostate-related conditions, medical intervention may be necessary to address the urinary issues and ensure proper urinary function.
Understanding the relationship between the prostate gland and the urethra helps healthcare professionals identify potential urinary flow problems in male patients and implement appropriate treatment strategies to alleviate symptoms and improve overall urinary health.
Structures Involved in Micturition
- Bladder/Detrusor
- Smooth muscle under voluntary control
- Trigone
- Area where ureters empty into the bladder and looks like a triangle
- This area contracts first to help prevent the reflux of urine back up to the kidneys
Let's delve into the structures related to urinary control. The bladder contains the detrusor muscle, which is a smooth muscle under involuntary control. However, the feedback loop enables us to exert some voluntary control over its functions, such as retaining or releasing urine.
Another crucial structure is the trigone, an area in the bladder where the ureters empty. The trigone's significance lies in its automatic contraction when there is an issue, preventing the reflux of urine back into the kidneys and reducing the risk of kidney infections.
In the cross-section images of Figures 8 and 9, we can observe the bladder's location, surrounded by the levator ani muscle group, responsible for supporting the pelvic floor. The external urethral sphincter and internal urethral sphincter control the opening and closing of the urethra.
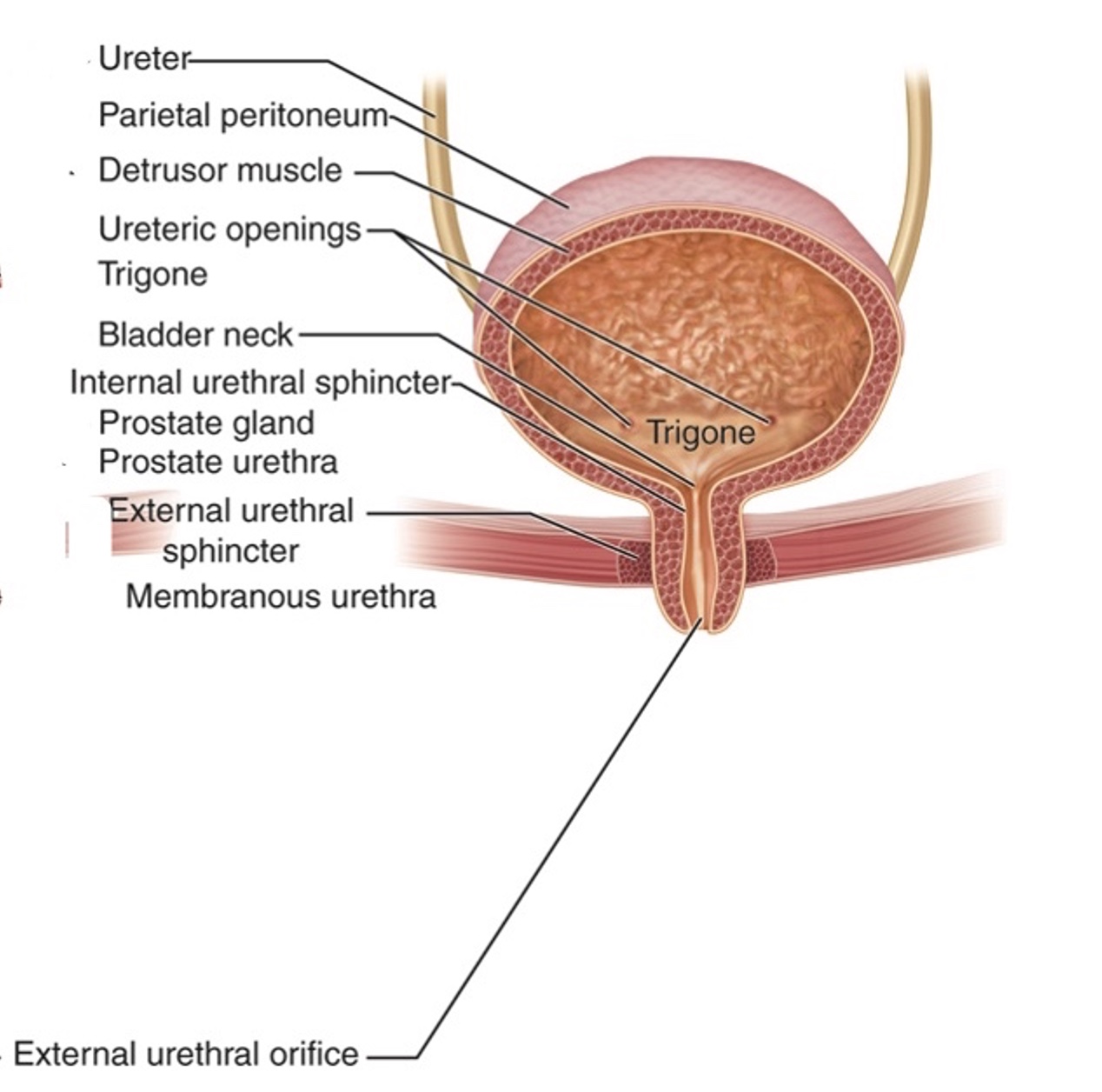
Figure 8. Female cross-section of urinary structures controlling micturition.
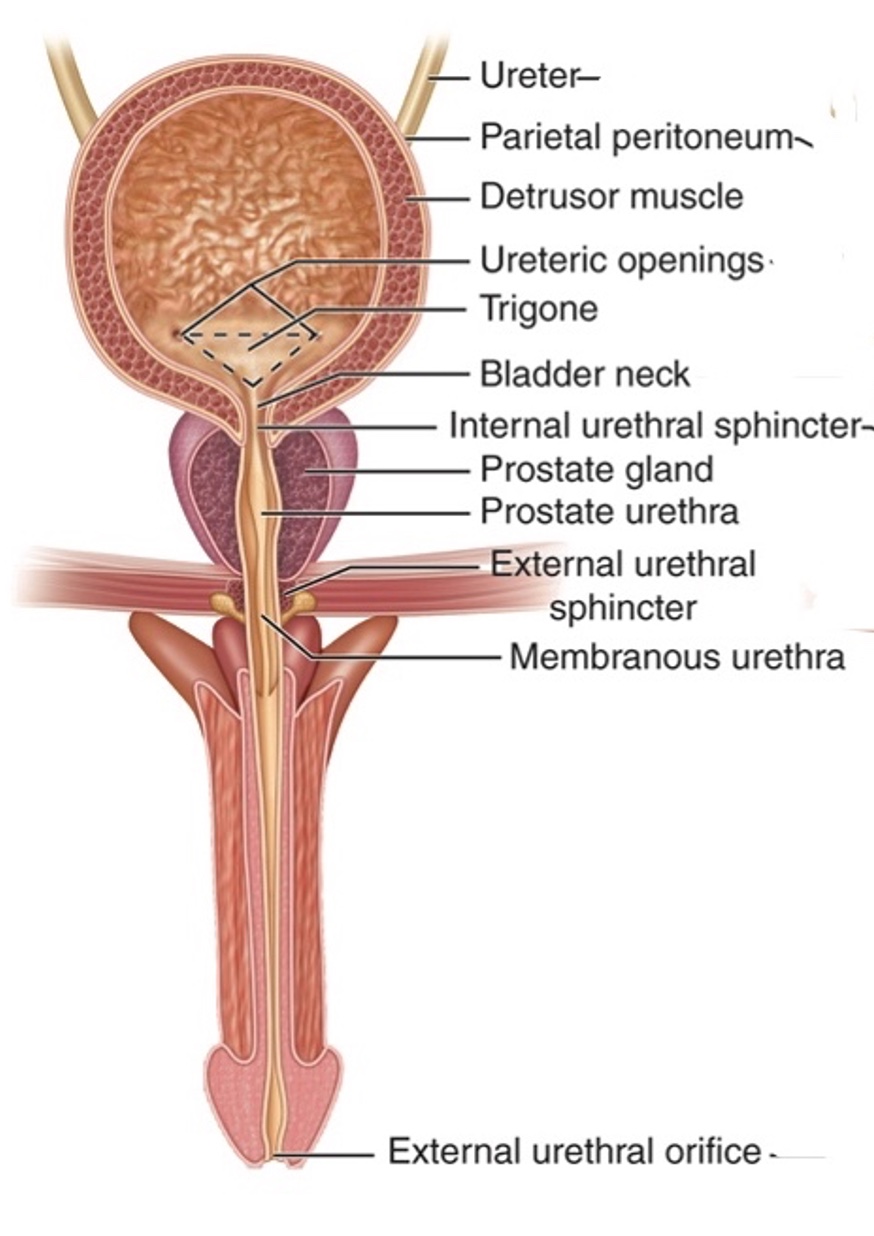
Figure 9. Male cross-section of urinary structures controlling micturition
In males, the prostate's relationship with the urethra can impact urinary output, particularly if there is an enlargement of the prostate. Understanding these structures and their interconnections is essential in comprehending the complexities of urinary control and potential issues related to urinary incontinence.
Normal Bladder Filling
- Kidneys produce urine which is transported through the ureters to the bladder.
- To prevent urine loss as the bladder fills, there is a gradual increase in urethral resistance – contraction of the urethra
- Pelvic floor muscles, stimulated by the autonomic and voluntary nervous systems, return to a low level of tonic contraction which helps maintain continence.
- The bladder fills from the bottom up and normally fills at a rate of about 1 ml/min by a series of squirts from the ureters (urine always being produced and dumped into the bladder)
Let's dive deeper into the process of normal bladder filling, as shown in Figure 10, as it is crucial to understand the feedback loop involved in continence.
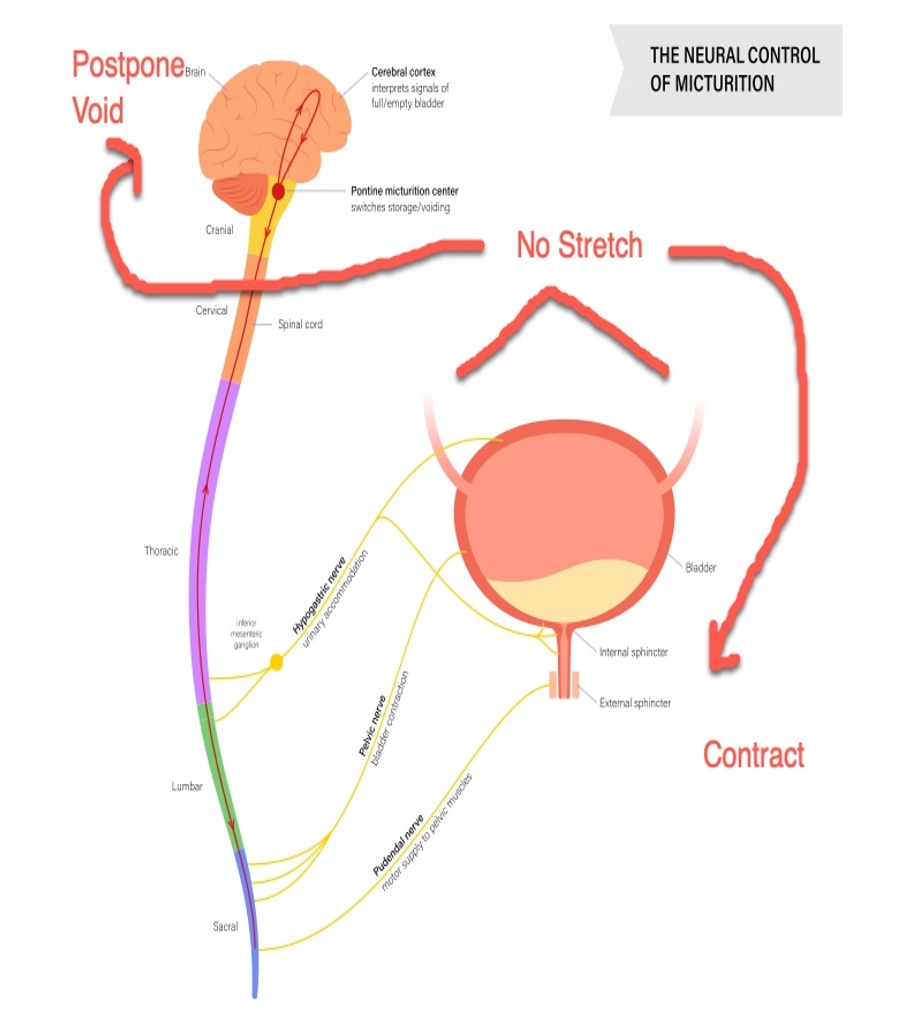
Figure 10. Illustration of normal bladder filling (Click here to enlarge the image.)
The kidneys produce urine, which then travels through the ureters and collects in the trigone area of the bladder. As the bladder fills, the urethra contracts to prevent urine loss. Additionally, the pelvic floor maintains a low-level tonic contraction to support and close off the sphincter. This sustained muscle activity is essential for continence, as it holds back the urine and gradually strengthens as the bladder fills.
- Initially, there is no sensation of filling (stretch receptors not firing)
- As it fills, a vague sensation deep in the perineum develops but is easily ignored
- With further filling, the sensation becomes harder to ignore; at this stage, voiding will need to occur
- Afferent or sensory nerves for this sensation originate from stretch receptors in the detrusor and run in the pelvic nerves and then in the lateral column of the spinal cord
- Bladder filling occurs via neural responses
- Sympathetic system via T10-L2 by stimulating the bladder, neck, and proximal urethra
- The parasympathetic system is activated.
- In the sacral spine (S2-S4) by stimulating the detrusor muscle (normally inhibited by the descending fibers from the pons so that the detrusor does not contract)
- Additional spinal-level inhibition
- Created by the somatic contraction of the pelvic floor and external urethral sphincter
- *EMG studies of the urethra and pelvic floor during bladder filling show increased muscle fiber recruitment of both these structures
The stress reflex ensures that the pelvic floor continues to contract and support, and the urethral resistance remains intact to prevent leakage. The external sphincter, surrounded by striated muscle, plays a critical role in keeping urine from leaking.
The mid-brain's pontine center is responsible for reflexive control, which can be overridden by the cortex. However, this conscious control generally develops around the age of two. When it's appropriate to void, the cortex sends a message allowing the reflex to occur. Alpha motor neuron activity drops to remove inhibition, resulting in sphincter relaxation, enabling voiding.
The shape and angle of the bladder and its neck play a significant role in proper voiding. The pelvic floor's contraction helps maintain the appropriate bladder shape, postponing or delaying the voiding. Proper voiding requires the muscles to relax, drop the bladder's angle, and allow urine to flow. However, if the pelvic floor muscles are weak, relaxation may lead to voiding when it's not intended. It's essential to strike a balance in strengthening these muscles to prevent urinary incontinence and ensure proper voiding when desired.
Normal Bladder Emptying
- When the bladder fills to a specific volume, stretch receptors in the bladder sense fullness (T10-L2)
- At the appropriate time and place, the brain releases inhibitory control, and a voluntary micturition reflex occurs, initiating detrusor (bladder) contraction and relaxation of the smooth and striated muscles of the sphincters (T10-L2 and S2-S4)
- Pons micturition center causes bladder emptying by relaxation of the pelvic floor, relaxation of urethral sphincters, sustained detrusor contraction forcing urine from the bladder
The reflexive control of the bladder's filling and emptying is largely coordinated by the brainstem's pontine center. While this reflex operates automatically, the cerebral cortex can exert conscious control over it when the appropriate time and place for voiding are recognized. When the cortex sends the signal to relax the pelvic floor and sphincter muscles, urination occurs. An overview of this can be seen in Figure 11.
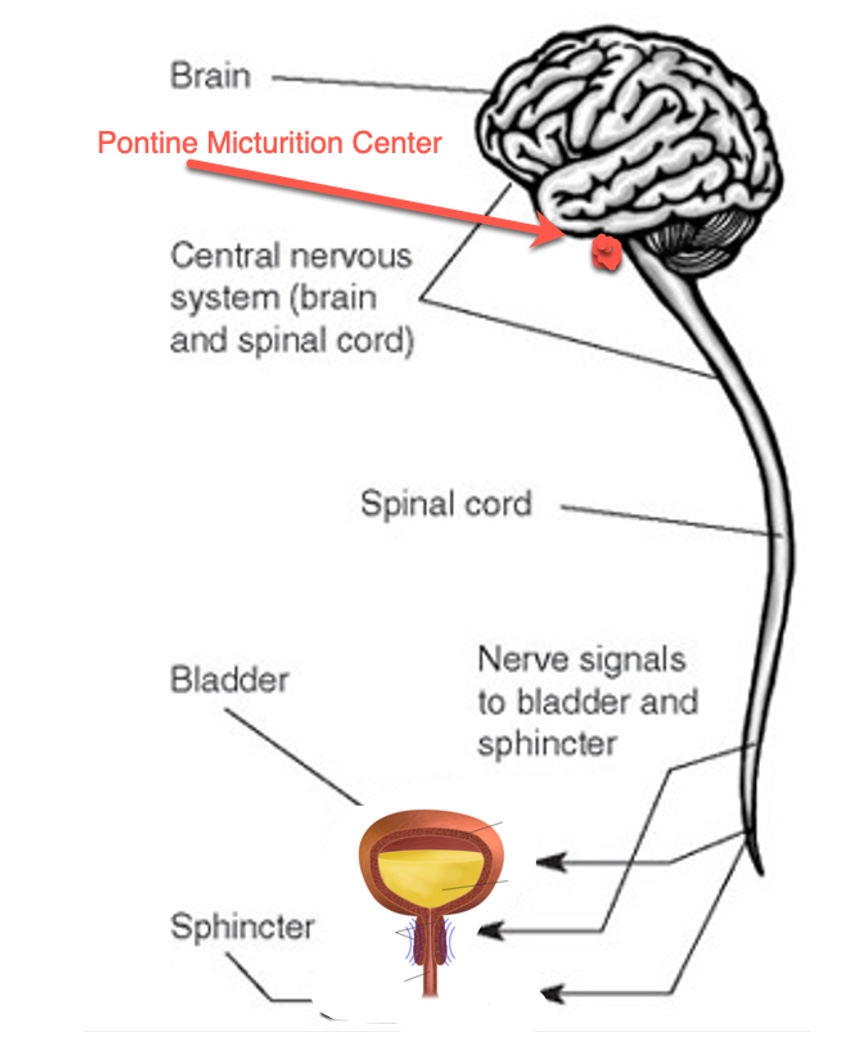
Figure 11. An illustration of bladder emptying.
The Pudendal Nerve
- Supplies:
- Most of the innervations to the perineum.
- Toward the distal end of the pudendal canal, the pudendal nerve splits to form the dorsal nerve of the penis or clitoris and the Perineal nerve.
- These nerves run anteriorly on each side of the Pudendal artery.
- The Perineal nerve gives off scrotal or labial branches and continues to supply the muscles of the urogenital diaphragm.
The pudendal nerve plays a crucial role in bladder control, originating from the S2-S4 nerve roots (Figures 12 and 13).
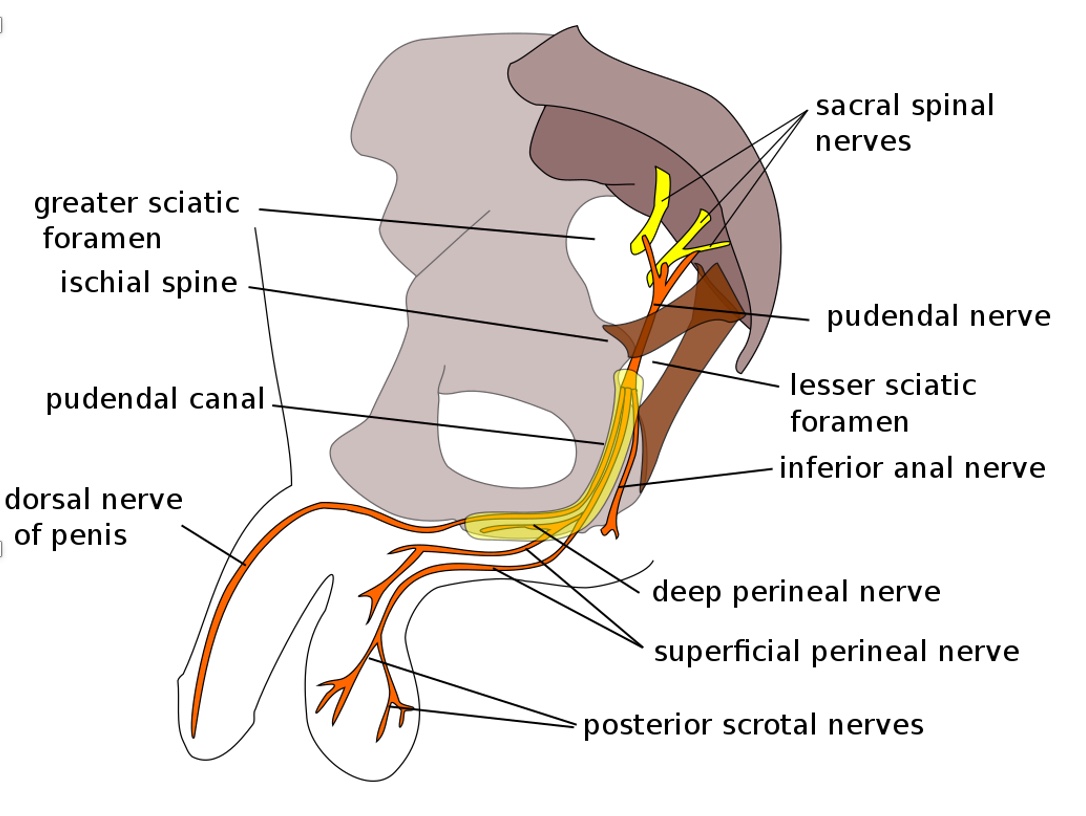
Figure 12. Illustration of the pudendal nerve in a male.
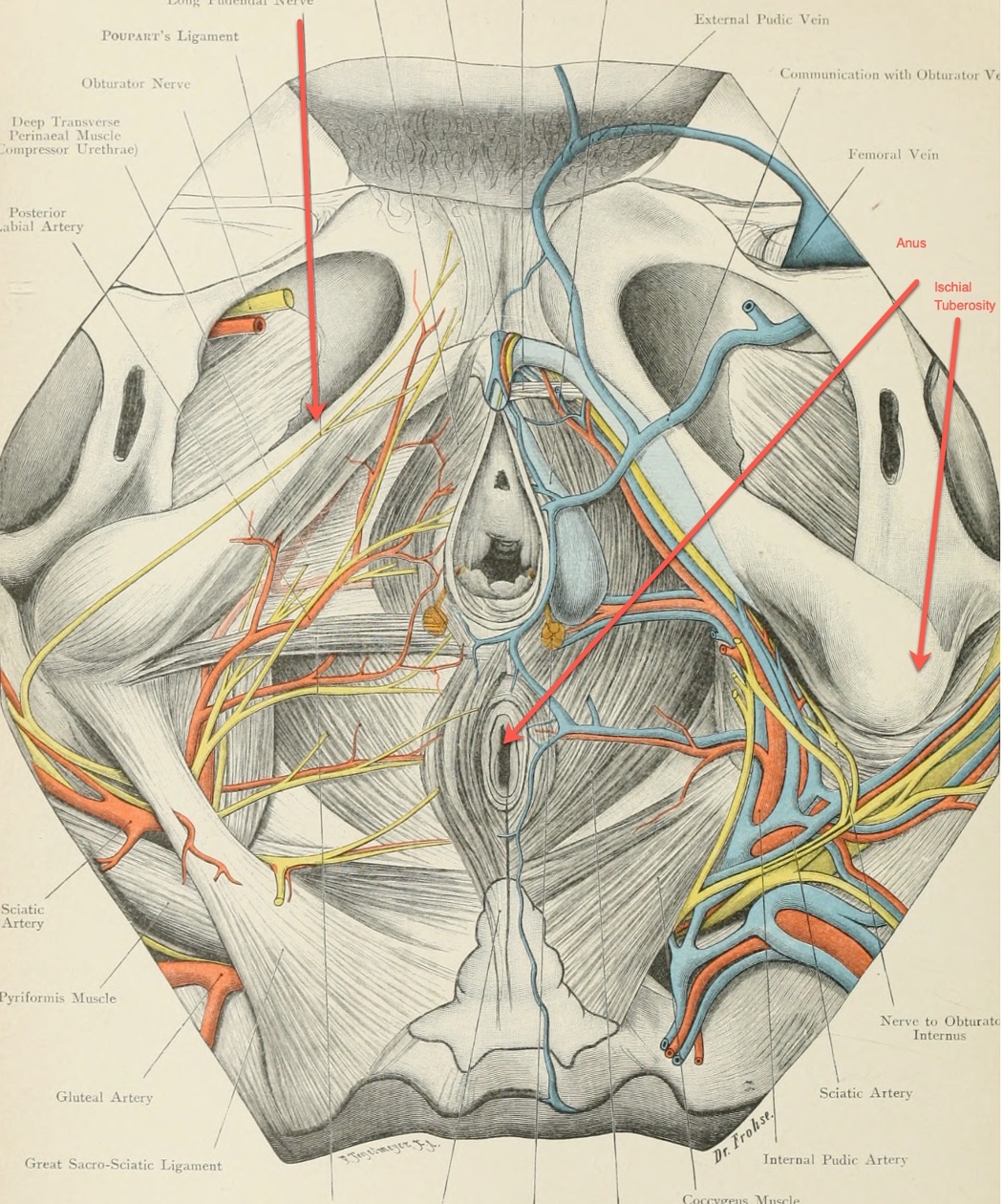
Figure 13. Illustration of the pudendal nerve in a female(Click here to enlarge the image.)
The pudendal nerve innervates the pelvic region, providing sensory and motor input to the striated muscle groups, including the pelvic floor and external sphincter.
Additionally, it has autonomic branches that communicate with the smooth muscle of the bladder and pelvic floor. The pudendal nerve also transmits information to the cerebral cortex, inhibiting the micturition reflex.
- Take Note:
- Elderly with compression fractures at S2-S4
- Osteoporosis etc., can lead to urinary retention since the peripheral parasympathetic nerves from S2-S4 facilitate the contraction of the detrusor
- Radical prostatectomy, as well as pregnancy and childbirth, can damage the pudendal nerve, also located at the S2-S4 level.
- Detrusor motor control area in the cerebral cortex arterial supply is from the middle and anterior arteries.
- The same arteries are affected by CVA, leading to an unstable bladder.
- Elderly with compression fractures at S2-S4
This complex nerve network is significant as it influences bladder function and can be impacted by various factors, such as posture, compression fractures, or labor and delivery-related issues.
Muscle Contractions
Urinary Sphincters
- Sphincters used to stop sudden urine flow
- Fast twitch fibers(35%) act quickly and intensely when coughing, sneezing, or doing something unexpected that increases the pressure on the bladder and urethra
- External sphincter under voluntary control
- (i.e. open and close these circular muscles at will through the Pudendal nerve)
- Internal sphincter NOT under voluntary control
- (in females, the internal sphincter is not effective as the bladder angle changes)
- Internal sphincter
- For males is above the prostate and externally below the prostate
- For females is located toward the neck of the bladder
The urinary sphincters, both external (voluntary control) and internal (involuntary control), are crucial in maintaining continence. These are shown in Figure 14.
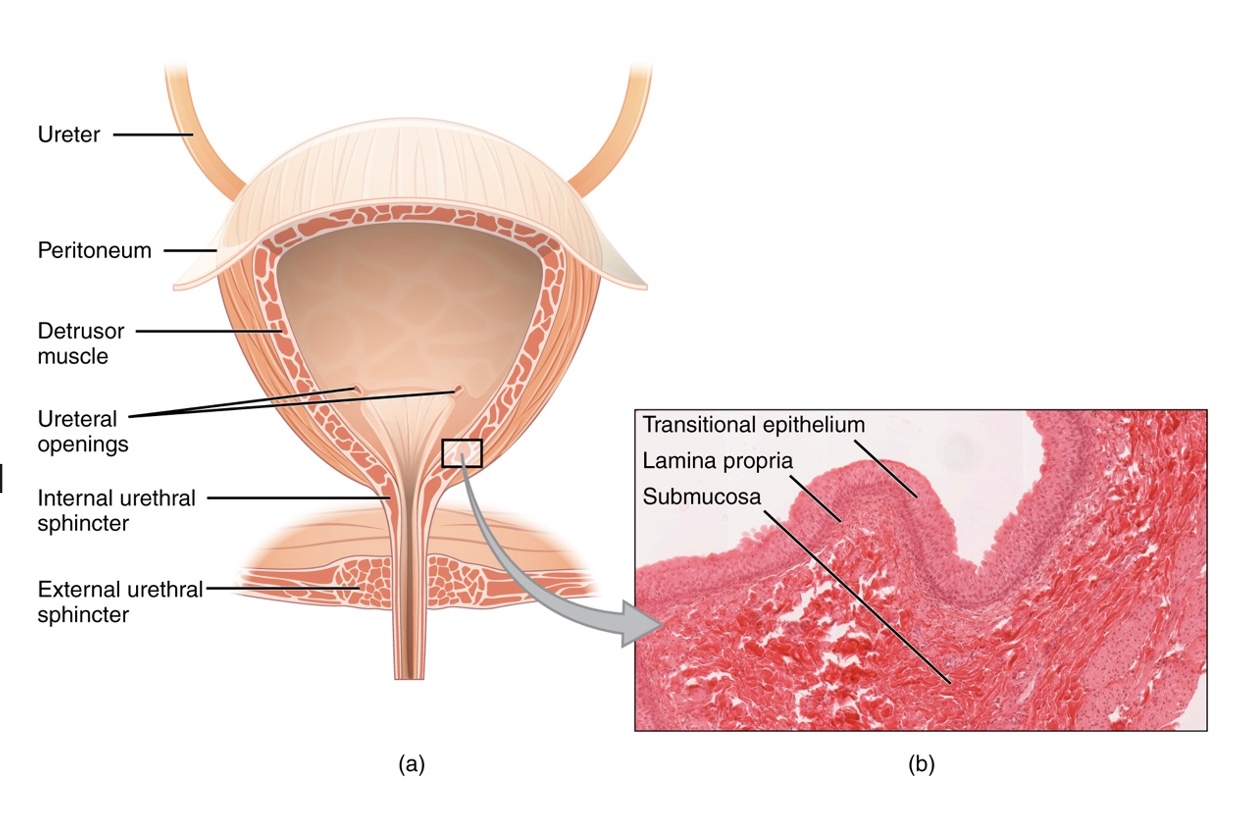
Figure 14. Illustration of sphincters.
- Sensory through T10-L2
- Motor contraction of the pelvic floor and the urethra through S2-S4
The pelvic floor's sustained low-level contraction and the fast twitch fibers in the sphincters work together to prevent urine leakage during everyday activities like sneezing or coughing. Understanding these intricate systems can help in addressing urinary incontinence and improving overall bladder health.
The relationship between the urinary sphincters and the pelvic floor muscles is closely interconnected in terms of anatomy and function. While the sphincters themselves are not part of the pelvic floor muscles, they work in tandem to maintain continence.
Pelvic Floor Muscles
- Levator Ani Muscles form the pelvic floor
- Pubococcygeal
- Iliococcygeal
- Ischiococcygeal
- Function in a sling-like fashion/hammock, maintaining constant low-level contraction for postural support of the internal organs
- Also called the pelvic diaphragm
- Deep muscle group of the perineum
The pelvic floor muscles, also known as the Levator Ani, consist of three main muscles: the pubococcygeal, iliococcygeal, and ishiococcygeal muscles. These deep muscles function like a sling or hammock, providing support to the internal organs and maintaining a constant low-level contraction.
- Support the bladder and urethra for an optimum position for continence
- Primarily slow twitch or type I muscle fibers
- Attach to the obturator tendon, the pubis, the sacrum, and the inner surface of the pelvis
- Also involved in providing improved closure of the urethral and anal sphincters
- The pubococcygeal muscle assists the urinary sphincter
- The iliococcygeal muscle assists in support of the vagina
- Ishiococcygeal muscle assists the anal sphincter
When they relax, the visceral contents drop down, allowing for the proper relaxation and emptying of the bladder. The pelvic floor muscles primarily consist of slow twitch or type one muscle fibers, which enable them to sustain contractions for extended periods, supporting bladder control.
These muscles are closely related to the hip and pelvic musculature, and any issues with hip fractures, hip replacements, or poor positioning can potentially impact the levator ani muscles and contribute to problems with urinary continence. The three components of the Levator Ani have specific functions: the pubococcygeal supports the urethra for storage, the iliococcygeus supports the vagina, and the ishiococcygeal assists the anal sphincter. Together, they have four main purposes: providing support to the viscera, facilitating storage by exerting passive and dynamic force on the urethra, inhibiting the detrusor to further support storage, and elongating to allow strain-free evacuation during voiding.
In Figures 15, 16, and 17, the illustrations depict the pelvic floor muscles from different angles, providing a clear visual of the hammock-like structure they form to support the internal organs and contribute to continence.
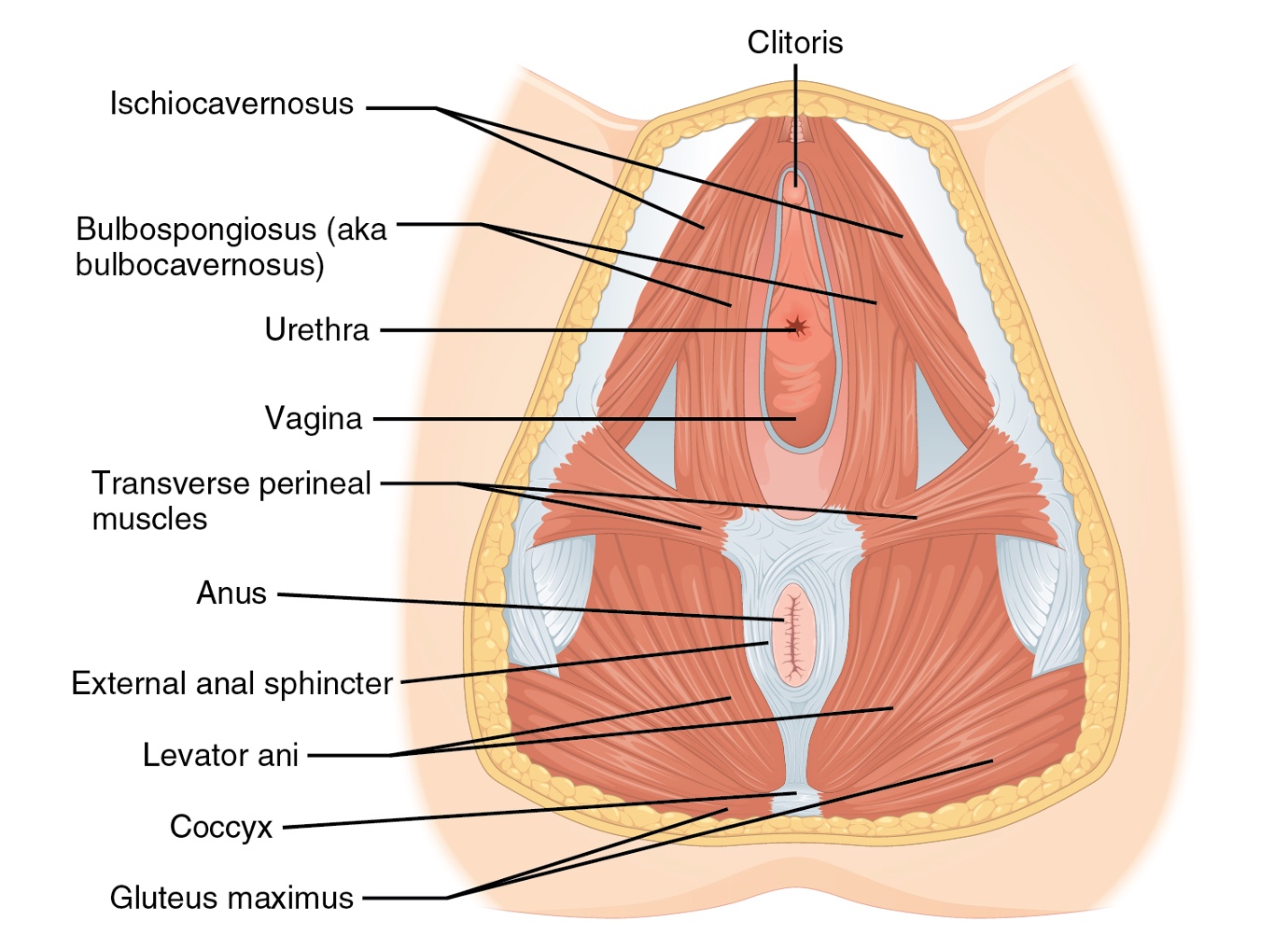
Figure 15. Pelvic floor muscles in a female.
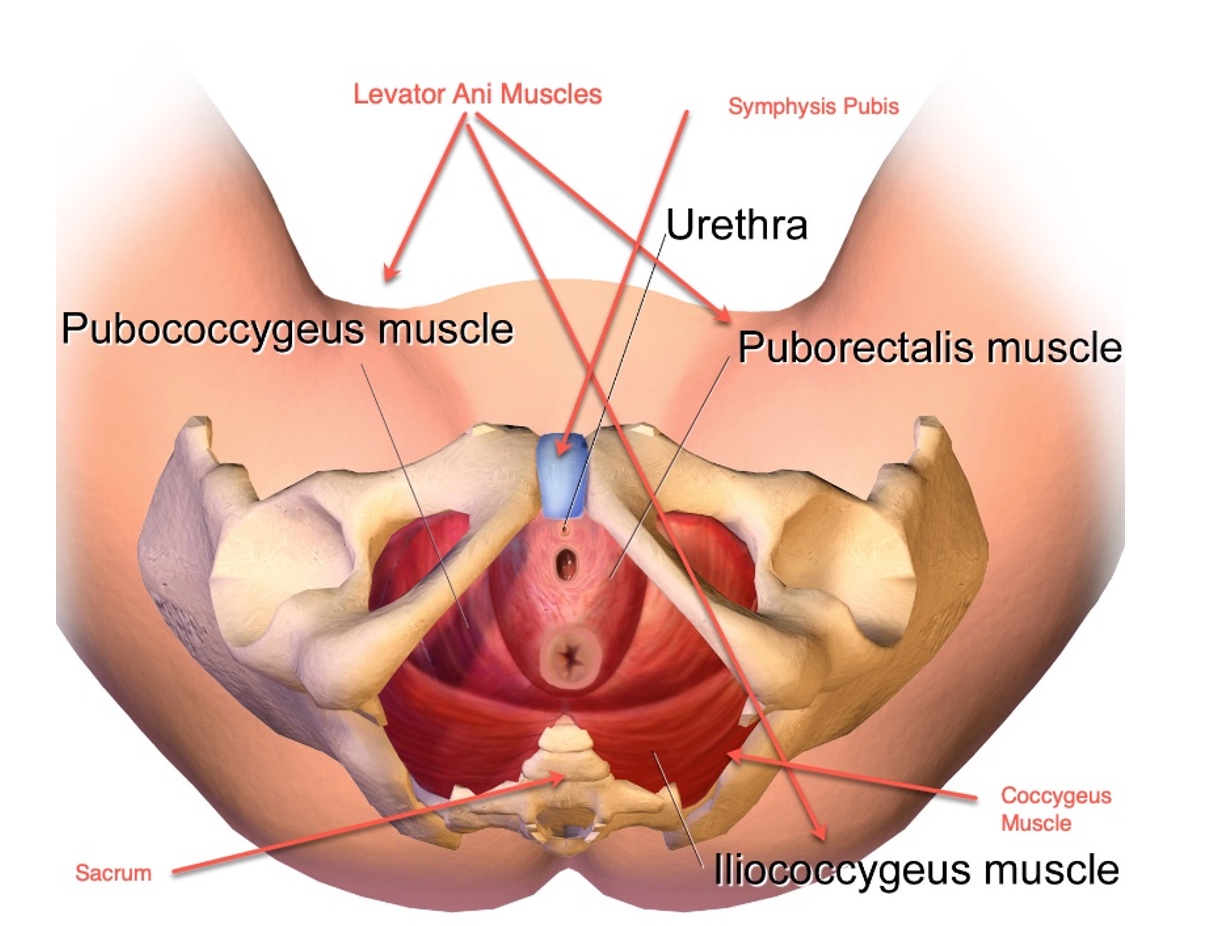
Figure 16. Another illustration of the female pelvic floor muscles.
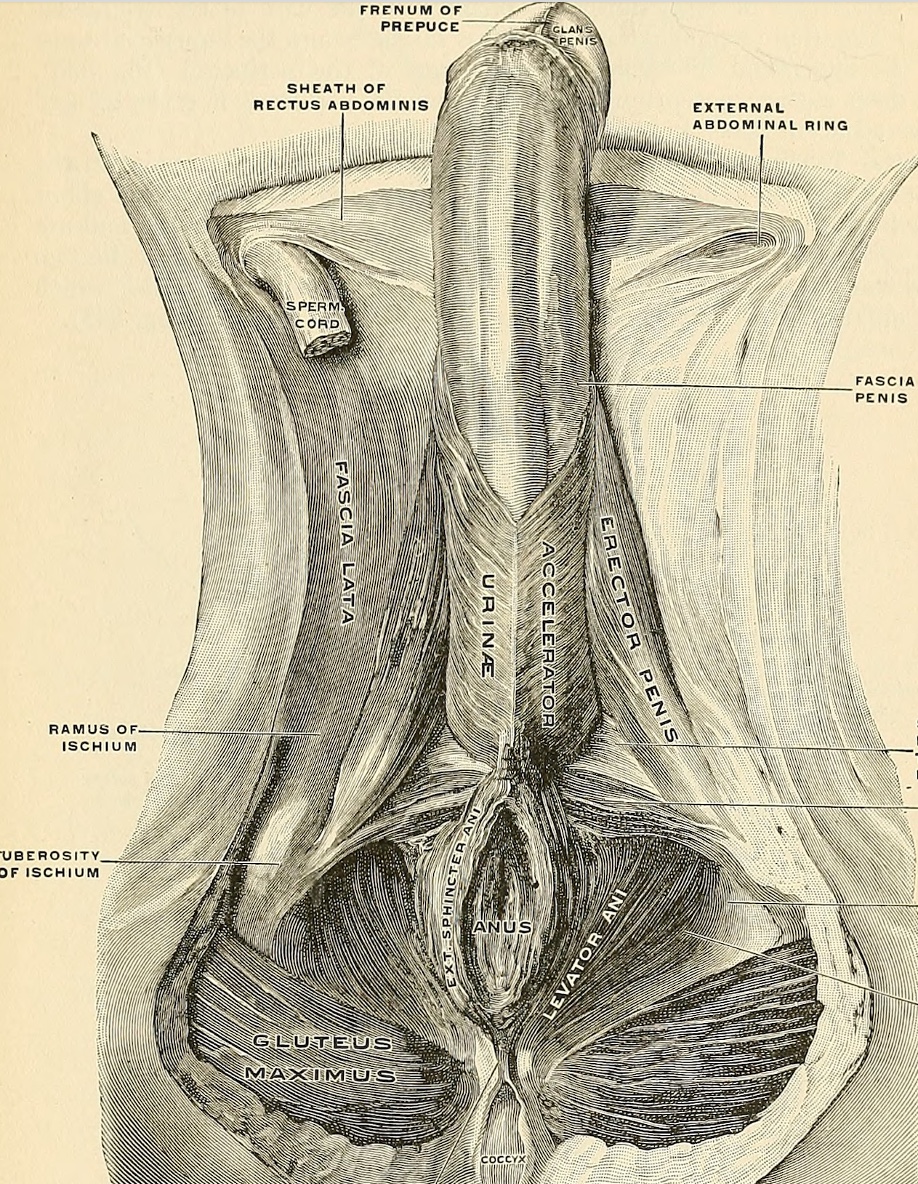
Figure 17. Illustration of the male pelvic floor muscles.
Lower Quadrant Cylinder
- Muscles forming the lower cylinder
- Diaphragm superiorly
- Multifidus posteriorly
- Transverse abdominus anteriorly
- Levator ani inferiorly
- When we move, these core muscle groups are active in all movements.
This cylinder concept involves a rectangular structure consisting of the diaphragm at the top (superiorly), the multifidus at the back (posteriorly), the transverse abdominis at the front (anteriorly), and the pelvic floor muscles (levator ani) at the bottom (inferiorly), and it is shown in Figure 18.
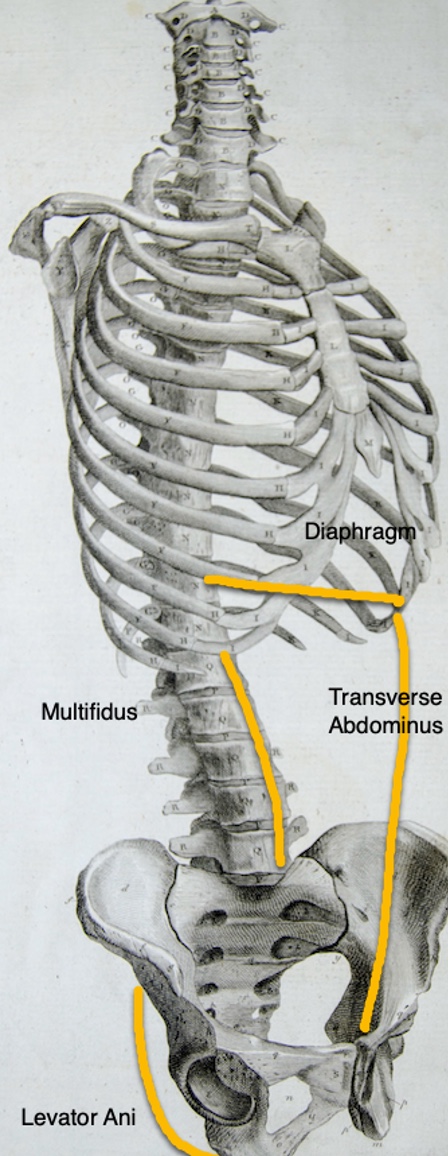
Figure 18. Illustration of the lower quadrant cylinder.
Understanding the cylinder concept is crucial because it highlights the interconnectedness of these muscles and their role in various activities. The levator ani, being part of the pelvic floor, plays a significant role in supporting the viscera and maintaining continence. It is activated during numerous daily activities, such as transfers, rolling, sit-to-stand movements, bending, reaching, and gait.
The cylinder concept also emphasizes the indirect interactivity between the different muscles. For example, activating the transverse abdominis can indirectly impact the levator ani. Similarly, the diaphragm's proper function is essential, especially during exercises, as it affects the entire cylinder and can influence the feedback loop associated with continence.
Types of Incontinence
- Stress
- Urge
- Mixed
- Overflow
- Functional
- Iatrogenic
Stress Urinary Incontinence (SUI)
- Involuntary loss of urine, occurring when, in the absence of a detrusor contraction, the intravesical pressure exceeds the maximum urethral pressure
- Leakage of small amounts of urine during physical movement (laughing, coughing, sneezing, exercising)
Stress urinary incontinence (SUI) is characterized by the involuntary loss of urine when the pressure inside the bladder exceeds the maximum urethral pressure, resulting in leakage during activities that increase intra-abdominal pressure. This type of incontinence is more commonly seen in women, often following pregnancy or childbirth, and can also occur in men after prostate surgery (TURP).
- Storage problem
- Deficient urethral closure mechanism
- Associated with intra-abdominal pressure
- Pressure gradient does not work
- Women > Men (due to pregnancy/childbirth)
- High levels of physical activity (e.g., running)
It is a failure to store urine properly, and the leakage usually occurs in small amounts.
- Causes of Stress UI
- Incompetent urethra/stretching from childbirth
- Weak pelvic floor musculature
- Prostate surgery
- Neurologic dysfunction and atrophy – reaction time from abdominal pressure increase to sphincter activation too slow
- Denervation injury of pelvic floor musculature due to pregnancy
Causes of SUI can include an incompetent urethra due to stretching from childbirth or weak pelvic floor muscles. Neurologic dysfunction, such as delayed sphincter response, can also contribute to SUI.
- Age-related hormonal deficiencies and atrophy of tissues
- Lower estrogen levels
- Changes in urethral mucosa
- Changes in cell structure/connective tissue
Other factors like estrogen deficiency, obesity, urethral sphincter weakness, and changes in urethral mucosa or connective tissue can play a role in this type of incontinence.
- Treatment for Stress UI
- No approved pharmacological agents
- First-line therapies (pelvic floor rehab)
- Urethral bulking with injectable agents
- Surgery (urethral support by sling)
When it comes to treatment, first-line therapies involve pelvic floor rehabilitation and exercises. Electrical stimulation, such as medium-frequency Russian stim or interferential stimulation, may be used as a form of pelvic floor rehab. Injectable agents into the urethra can also provide some relief by strengthening the area. In some cases, surgery may be considered, but most cases of SUI can be effectively managed with conservative approaches like pelvic floor rehab.
Urge/Overactive Bladder (OAB) Incontinence
- Involuntary loss of urine associated with a strong desire to void (urgency)
- Leakage of large amounts of urine at unexpected times, including during sleep
- Urge incontinence results when an overactive bladder contracts without us wanting it to do so.
- Feel as if they can't wait to reach a toilet
- May leak urine without any warning at all
- Infection can cause irritation to the bladder lining
- Can be a nervous system problem
Urge incontinence is another type of failure to store urine, where the person experiences an involuntary contraction of the detrusor muscle in the bladder, leading to a sudden and strong urge to urinate, often resulting in leakage before reaching the toilet. This condition is characterized by increased pressure in the bladder during filling, and individuals may have a decreased sensation of bladder fullness, leading to a sense of urgency and an inability to hold urine.
- OAB Causes
- Uncertain predisposing factors
- Voiding against urethral obstruction
- A habit of low-volume voiding
- Lower sensory threshold
- Sensory urgency
- Diet – bladder irritants and fluid restriction
Overactive bladder (OAB) is a specific form of urge incontinence, where individuals experience urinary urgency, and increased daytime and/or nighttime frequency of urination without any detectable underlying disease or infection. It is prevalent in about 12% of both men and women and becomes more common with advancing age.
- Causes of Urge Incontinence
- Urinary tract infections, cystitis, bladder tumor, stones, irritation (fluids & diet)
- Decreased sensation of fullness
- Neurologic sensitization and dysfunction
- CVA
- Immobility
- Dementia
- Multiple Sclerosis
- Parkinson’s
- Spinal cord tumor or lesions
The exact cause of urge incontinence and OAB is not always clear, but it could be related to voiding against urethral obstruction or low-volume voiding patterns, leading to a lower sensory threshold for bladder fullness. Other factors like dementia, Parkinson's, UTIs, tumors, stones, detrusor hyperactivity, or bladder contractility impairment could also contribute to this condition.
Mixed Incontinence
- Combination of urge and stress urinary incontinence, often associated with the elderly patient
- Most common type of incontinence in SNF
There is also a mixed type of incontinence, which is quite common, especially among women. Mixed incontinence is a combination of both stress and urge urinary incontinence, presenting a challenge for those affected. It's important to note that urge incontinence, similar to stress incontinence, can also be effectively addressed with electrical stimulation if necessary. Both types of incontinence involve failures to store urine properly and may involve some level of sensory impairment. These issues are frequently encountered in skilled nursing settings.
Overflow Incontinence
- Any involuntary loss of urine associated with the overdistention of the bladder (automatic response by the body to protect the kidneys)
- Overflow incontinence occurs when the bladder is allowed to become so full that it simply overflows.
Overflow incontinence is, as it sounds, a failure to empty the bladder properly. In this type, individuals don't feel the need to urinate, and the bladder ends up overflowing, resulting in small amounts of leakage.
- Causes of Overflow Incontinence
- Outlet obstruction
- Enlarged prostate
- Fecal impaction
- Diabetes
- Heavy alcohol use
- Decreased nerve function
- Weak detrusor
- Peripheral neuropathy
- Outlet obstruction
This can be caused by bladder weakness or a blocked urethra that hinders normal emptying. It is more commonly observed in men, especially if there's an enlarged prostate causing the blockage. Women can also experience this condition due to bladder weakness or certain medical conditions like diabetes or decreased nerve function.
A post-void residual (PVR) test would reveal a full bladder in these individuals, but they lack the sensation of needing to empty it, leading to involuntary leakage. An appropriate intervention for them would be the double void approach.
Various factors can cause overflow incontinence, including medications, diabetic neuropathy, low spinal cord injury, fecal impaction, constipation, and peripheral neuropathy.
Functional Incontinence
- Urinary leakage associated with inability to toilet because of impairments of cognitive and/or physical functioning, psychological unwillingness, or environmental barriers
- Functional incontinence occurs when one cannot get to the toilet or get a bedpan when needed
- The urinary system may work well, but physical or mental disabilities or other circumstances prevent normal toilet usage
Functional incontinence occurs when individuals have a normal urinary system, but face barriers that prevent them from accessing the toilet or appropriate facilities for voiding. This type of incontinence is often related to cognitive, communication, or physical impairments that hinder the person's ability to communicate their needs or physically reach the toilet.
- Causes of Functional Incontinence
- Most common = STAFF
- Impaired mobility
- Severe dementia
- Communication difficulties
- Depression
- Hostility
- Caregiver, toilet and/or toilet substitutes unavailable
Various factors can contribute to functional incontinence, such as impaired mobility, dementia, communication difficulties, the use of physical restraints, musculoskeletal dysfunction, visual impairment, fear of falling, poor lighting, clothing management difficulties, and environmental barriers like narrow doorways or inaccessible facilities.
Addressing functional incontinence requires a comprehensive approach involving occupational therapy, physical therapy, speech therapy, and nursing to identify and address the underlying barriers and provide appropriate interventions and support to help individuals achieve continence and improve their quality of life.
Iatrogenic Incontinence
- Diuretics
- Sleeping pills/sedatives
- Decongestants
- Anti-depressants
- Cold remedies
- Parkinson’s meds
- Pain meds
- Blood pressure
Iatrogenic urinary incontinence is related to medications, and it's an important consideration, especially for seniors who often take multiple medications. Certain drugs can contribute to urinary incontinence by affecting the urinary system in various ways.
For instance, diuretics increase urine production, leading to a fuller bladder and potential leakage. Sleeping pills and sedatives relax the muscles, including those involved in bladder control, which can reduce the awareness of the need to void. Decongestants, on the other hand, can tighten the pelvic floor muscles, making it difficult to void properly.
Antidepressants may cause overflow incontinence, as they can relax the bladder too much, resulting in urine overflow. Cold remedies, pain medications, and certain blood pressure medications can lead to urinary retention, making it challenging to empty the bladder fully.
Additionally, medications used to manage Parkinson's disease can increase the likelihood of overflowing incontinence due to their impact on the bladder and its control.
Neurogenic Incontinence
- Symptoms range depending on site of neurologic insult
- Detrusor underactivity/overactivity
- Sphincter underactivity/overactivity
- Loss of coordination with bladder function
The final type of urinary incontinence is neurogenic in nature, and its presentation varies depending on the location and extent of the neurologic insult. This type can manifest as detrusor underactivity or overactivity, as well as sphincter dysfunction and lack of coordination between these structures.
- Causes of Neurogenic Incontinence
- Spinal cord injury
- Multiple sclerosis
- Peripheral nerve lesions due to:
- Diabetes mellitus
- Tabes dorsalis
- Herpes zoster
- Herniated lumbar disk disease
- Radical pelvic surgery
Neurogenic urinary incontinence can be attributed to conditions such as spinal cord injuries, diabetes, herniated lumbar discs, among others.
- Other factors
- Delirium or confusional state or diet
- Atrophic vaginitis/urethritis
- Pharmaceuticals
- Psychological disorders, especially severe depression
- Endocrine disorders, hyperglycemia or hypercalcemia
- Restricted mobility
- Stool impaction
Additionally, various factors may contribute to this type of incontinence, including the use of pharmaceuticals, restricted mobility, stool impaction, and endocrine disorders, like thyroid conditions. Hormonal imbalances, such as a lack of estrogen, weakness, surgeries, and the effects of childbearing, are also among the potential causes. As healthcare professionals, it is essential to identify the specific type of neurogenic incontinence to develop targeted and effective treatment plans.
Other Causes of Urinary Incontinence
- Urinary tract or vaginal infections
- Postmenopausal – lack of estrogen
- Constipation or fecal impaction
- Weakness of certain muscles
- Blocked urethra d/t enlarged prostate
- Disorders involving nerves or muscles
- Some types of surgery
- Childbearing
- SCI
Determining Type of Incontinence
During our occupational therapy evaluation, it is crucial to determine the type of incontinence the individual is experiencing to tailor our interventions effectively. We can start by asking specific questions to identify the type of incontinence.
- Stress Incontinence
- Does the patient leak while laughing, coughing, sneezing, lifting, or doing physical activity?
- Has the patient had a prostatectomy?
- Does the patient urinate during sex?
- Did the patient have vaginal deliveries?
- Did the patient have a hysterectomy?
For stress incontinence, we may inquire if they experience leakage during activities like laughing, coughing, or sneezing and if they notice urine leakage during sexual intercourse.
- Urge Incontinence
- Does the patient have a strong urge to urinate but is unable to make it to the restroom?
- Does the patient strain to urinate?
- Does the patient have large accidents?
- Does the patient urinate a lot at night?
- Is the patient urinating frequently?
For urge incontinence, we can ask about the frequency of sudden, strong urges to void and if they have accidents, especially at night.
- Functional Incontinence
- Does the patient have arthritis? Fatigue? Weakness? Seem depressed?
- Does the patient have dementia?
- Does the patient have trouble removing clothes? Walking? Walk too slowly?
- Does the patient have accidents early in the morning?
Functional incontinence may be explored by assessing their ability to manage clothing, mobility issues like arthritis or trouble walking, and if they have difficulty reaching the restroom on time due to cognitive or physical limitations.
- Overflow Incontinence
- Has the patient injured the spinal cord? Or issue with nervous system?
- Does the patient have diabetes?
- Could he have an enlarged prostate?
- Had surgery that traumatized urethra?
- Could the patient be constipated?
- Tenderness over the pubic bone?
- Signs of an Enlarged Prostate
- Difficulty getting stream started
- Slow, weak, or interrupted stream
- Frequent voiding small amounts
- Pain or burning with voiding
- Voiding at night
- Urgency
- Incomplete emptying
- Incontinence
For overflow incontinence, we may look into their medical history, such as diabetes or prostate-related issues, and check for any tenderness or discomfort over the pubic bone, which could indicate an enlarged prostate.
By gathering this information and conducting a thorough assessment, we can better understand the underlying causes of their incontinence and develop appropriate interventions to improve their quality of life and functional independence. As occupational therapists, we play a vital role in addressing the multifaceted aspects of incontinence and its impact on daily activities, working in collaboration with other healthcare professionals to provide comprehensive care.
Average Bladder Function
Average Function
- Average Bladder Capacity:
- Younger Adult - 500-600 cc or 16.6-20 fluid oz. (2–2 ½ cups of fluid)
- Elderly – 200–400 cc or 6.6–13.3 fluid oz. (3/4–1 ¾ cups of fluid)
- Average # Voids/Day:
- Younger Adult 4-7 times / 24hrs
- Elderly 5–8 times / 24hrs
As we age, bladder function undergoes changes that can impact urinary continence. The elderly bladder may not distend as much as a younger one, leading to reduced holding capacity. While a healthy person can typically hold their urine throughout the day without issues, seniors may have a decreased ability to do so. When they feel the need to go, it may be urgent, and it's essential to recognize and respond to their needs promptly.
- Nocs:
- Younger Adult - Seldom or 1 times
- Elderly - 1 to 2 times
- 24 Hour urine output
- Younger Adult – 1000-5000 cc or 33.3
- 166.7 fluid oz. (4.16–20.8 Cups)
- Elderly – 1000–2000 cc or 33.3
- 66.7 fluid oz. (4.16–8.3 Cups)
- Younger Adult – 1000-5000 cc or 33.3
Frequent trips to the restroom, especially more than twice per night, known as nocturia, are not typical for healthy individuals. However, this can be a common occurrence among the elderly, affecting their sleep and daily routines. Additionally, as we age, urine output naturally decreases, and certain diseases or medications can further lower it. Seniors may be prone to reducing fluid intake to avoid incontinence, but this can lead to other health complications.
- A healthy person’s bladder can usually be emptied voluntarily prior to sensory awareness, defined as voluntary control.
- Time from initial urge until bladder reaches capacity is usually 1-2 hours.
A healthy person's bladder can be voluntarily emptied before sensory awareness, which means they can urinate on command for various situations, like lab tests. However, elderly individuals may not have the same level of voluntary control over their bladder, making managing continence more challenging for them. Furthermore, the time from feeling the initial urge to void until the bladder reaches its full capacity is typically around one to two hours, and this can vary among seniors.
Post-Void Residual
- PVR (Post Void Residual) or the urine left in the bladder after toileting can be assessed by a straight catheter or a bladder scan. WNL < 100cc or < 50cc; more = retention
It's crucial to recognize the significance of post-void residual (PVR), which is the amount of urine remaining in the bladder after toileting. PVR can be measured using a bladder scan or a straight catheter. In a healthy individual, the normal PVR should be zero, indicating that the bladder has emptied completely.
However, concerns arise when the PVR is higher, typically starting to become concerning when it exceeds around 100 CCs. It's essential to consider factors such as age, actual bladder capacity, and any underlying disease processes when evaluating the significance of the PVR measurement. For instance, if someone has a large bladder capacity, a small amount of PVR might not be alarming. But if the bladder capacity is low, even a relatively small PVR can become a matter of concern.
Ultimately, the goal is to have as close to zero PVR as possible. Ensuring that the bladder fully empties during each voiding helps to minimize the risk of urinary retention and associated complications.
Fluid Intake Requirements
- Fluids come from food and liquid intake
- Thirst sensation may be decreased in older adults - offer fluids throughout the day
- Dehydration is serious and prevalent with LTC
Fluid intake and hydration are critical considerations in the care of older adults. As people age, the sensation of thirst tends to decrease, making it essential to proactively offer fluids to seniors, both food and beverages. Dehydration is a prevalent and serious concern among the elderly, so encouraging and facilitating adequate fluid intake is crucial.
As occupational therapy practitioners, we may play a role in helping seniors with diet modifications that support their hydration needs. It's important to identify and offer alternative food and drink options that are not irritating to their bladder or overall health. Restricting fluid intake is not an effective strategy to manage urinary incontinence or other health conditions; instead, promoting a balanced and appropriate fluid intake is the key.
Dietary Irritants and Fluids
- Many foods can irritate the lining of the bladder
- Eliminating dietary caffeine can help this
- However, limiting overall fluid intake is not effective for managing UI.
- Substituting bladder irritants:
- Water
- ½ and ½ water to juice
- Decreasing the amount of times coffee is served
Bladder irritants can play a role in exacerbating urinary incontinence in some individuals. While there is no specific diet that can cure incontinence, certain foods and beverages, such as citrus, artificial sweeteners, caffeine, and alcohol, have the potential to irritate the bladder lining and contribute to the condition. Managing and avoiding these irritants can be beneficial for some individuals.
As we age, there are changes in bladder function that can lead to an increase in frequency and nighttime bathroom visits despite a decrease in overall urine output. The ability to store urine diminishes with age, resulting in a reduced bladder capacity and a greater sense of urgency to urinate. Younger individuals may have stronger musculature and a greater bladder capacity, allowing them to hold urine longer. In contrast, seniors may experience more frequent urges to urinate due to reduced storage capabilities.
Constipation can also be a contributing factor to bladder control issues. Addressing constipation through dietary adjustments, such as increasing fiber intake to add bulk to the stool, may help alleviate related bladder problems.
Bladder Irritants
- Artificial sweeteners/colors
- Alcoholic beverages
- Apples
- Apple juice
- Artificial sweetener
- Beer
- Caffeine
- Carbonation
- Chilies/spicy foods
- Citrus fruits/juices
- Coffee (including decaf)
- Colas
- Corn syrup
- Cranberries
- Honey
- Grapes/grape juice
- Guava
- Milk/dairy
- Peaches
- Pineapple
- Plums
- Strawberries
- Sugar
- Tea
- Tomatoes
- Vinegar
- Vitamins B and C
- Wine
The above list is some examples of bladder irritants.
Substitutions
- Low-acid fruits
- Tea substitutions
- Vitamin substitute
- Juice substitutes
- Coffee substitutions
- WATER!! Water does not irritate
When considering urinary health and preventing irritation, the best substitution is indeed water. Water does not irritate the bladder and is a safe and gentle option for maintaining hydration. It is crucial to avoid adding artificial sweeteners or other irritants to water, as this can negate its beneficial effects on bladder health. Staying hydrated with water remains a key strategy for supporting overall urinary function and preventing potential irritation.
Vitamin C- These Do Not Irritate the Bladder
- Asparagus
- Avocado
- Broccoli
- Brussels sprouts
- Cabbage, raw
- Cantaloupe
- Cauliflower
- Green pepper
- Greens (collards, kale)
- Lima beans
- Mango
- Papaya
- Peas
- Raspberries
- Spinach
- Squash
- Strawberries
- Turnips
- Vitamin C fortified cereal
Vitamin C is essential for our health, but for individuals who find citrus irritating to their bladder, there are alternative sources for obtaining vitamin C without causing bladder irritation.
Calcium- These Do Not Irritate the Bladder
- Broccoli
- Clams
- Collards, cooked
- Farina
- Oysters
- Salmon
- Sardines
- Self-rising flour
- Soybeans, cooked
- Turnip greens, cooked
- Ice milk
Likewise, calcium is essential, but for those who experience bladder irritation from dairy products, there are other dietary sources available to meet calcium needs.
Prescribed Medications
- Oxybutynin (Ditropan) and Tolterodine (Detrol) -- urge incontinence
- Pseudoephedrine (Sudafed) -- stress incontinence
- Imipramine (Tofranil) -- urge or stress incontinence
- Tamsulosin (Flomax) or Terazosin (Hytrin) -- overflow incontinence
As for prescribed medications, they can be helpful in managing different types of urinary incontinence. For instance, Ditropan or Detrol can assist individuals with urgent incontinence or hyperactive bladder by reducing muscle spasms and improving control. Sudafed, although it may cause urine retention, could potentially be beneficial in treating stress urinary incontinence when there is a failure to store urine properly. Tofranil, an antidepressant, can increase bladder volume and improve control of urine flow. Flomax or Hytrin can improve urinary flow, especially for those with an enlarged prostate. However, it is essential to remember that these medications should be prescribed and managed by a physician.
Evaluation
Nursing and MD Evaluation
- History
- Detail of Symptoms and Associated Factors
- Physical Exam
- Urinary Analysis and PVR
The evaluation of urinary incontinence involves an interdisciplinary approach with contributions from nursing, physicians, and occupational therapists, among others. Various assessments are performed to gather comprehensive information. These include medical and neurological evaluations, genital urinary assessments, and physical examinations. Estrogen levels may be considered for women experiencing incontinence related to hormonal changes.
Detailed symptom analysis, including timing, precipitants, and bladder diary data, helps understand the nature of the condition.
Urinalysis and blood tests are conducted to identify any signs of infection or underlying medical conditions that could be affecting bladder function. In some cases, specialized tests like cystograms may be used to examine the bladder more closely.
Additionally, post-void residual (PVR) measurements are taken to determine if the bladder is emptying properly.
Patient Questionnaire
- Gender
- Do you ever leak urine when you don’t want to?
- When did you notice the onset of urinary leakage?
- Did the urine leakage begin after trauma?
- Did you leak urine as a child? Until what age?
- How does UI affect you?
- How often do you leak urine?
- When does leakage occur?
- Do you wake up at night to urinate?
- Do you awaken as you are losing urine?
- When you leak urine, how much leaks?
- Do specific activities cause you to leak urine?
- Do you ever have trouble getting to the toilet on time or have accidents while removing your clothes prior to urination?
- Do you realize that you are losing urine as it runs out?
- How often do you normally urinate?
- Once your bladder feels full, how long can you hold it?
- Can you stop the flow of urine at will?
- Do you know when you have to go?
- Do you have any of the following?
- Difficulty starting a stream
- Straining
- Very slow stream or dribbling
- Discomfort or pain
- Burning
- Blood in the urine
- Do you feel that you completely empty?
- Do you leak urine while having sex?
- Current method of managing urinary leakage?
- How much fluid do you take in within a 24-hour period?
- Do you ever have uncontrolled loss of stool?
- Current medications
These next slides provide a comprehensive set of questions to ask during the evaluation of urinary incontinence. Understanding the specific details of the individual's condition is essential for developing an effective treatment plan. Some of the questions include when and how often the leakage occurs, the amount of leakage, the triggers for leakage during certain activities, and the individual's ability to hold urine. Assessing their awareness of the need to urinate and their ability to stop the flow of urine is crucial.
Additional inquiries cover any discomfort or abnormalities experienced during urination, the presence of blood or burning sensations, and any issues related to sexual activity. The current management methods used by the individual, such as medications or assistive devices like bedside commodes or urinals, are also important to consider. Understanding the person's medication regimen is critical as it may reveal potential interactions or side effects contributing to their incontinence.
As occupational therapists, this detailed assessment helps us gain insight into the individual's specific challenges and needs, allowing us to create personalized interventions that address the underlying causes and improve their overall bladder function and continence.
Medical History
- Congestive heart failure
- Stroke
- Depression
- Glaucoma
- Cancer
- Dementia
- Diabetes
- Heart arrhythmia
- Parkinson’s disease
- Fainting
- Prior CNS trauma/surgery
- Dizziness
- Other neurological disorders
Understanding the individual's medical history is crucial for a comprehensive evaluation. While we may not conduct a full medical history ourselves as occupational therapists, collaborating with other healthcare professionals, such as nurses or physicians, can provide us with essential information about the person's overall health and any conditions that may be contributing to their urinary incontinence.
For example, medical conditions like glaucoma could impact the person's ability to see and navigate their environment, potentially leading to difficulties in finding the bathroom or detecting urine on the floor. Neurological conditions like Parkinson's disease can affect bladder control due to nerve impairments.
Prior Genitourinary History
- Rheumatic heart disease
- Bladder tumor
- Multiple vaginal deliveries
- Recurrent UTI
- C-sections
- Pelvic irradiation
- Bladder suspension
- Urethral stricture/dilation
- Vaginal hysterectomy
- Prostate surgery
- Abdominal hysterectomy
Tumors or prior genital and urinary history, such as vaginal deliveries in women, may provide insights into the type of urinary incontinence the individual is experiencing.
24-Hour Voiding Diary
- Purpose: To obtain accurate, baseline bladder health information of the resident receiving skilled therapy for UI
- Standard of care is 3 days – 7 for outpatients
- Administered three times (preferably throughout)
- At Initial Evaluation for – baseline
- After 4 weeks of therapeutic intervention to determine progress to date
- At D/C from program to determine the status at D/C
A 24-hour voiding diary is a valuable tool for assessing and understanding an individual's bladder health. While the standard of care is typically three days in outpatient or home settings, it may be extended to seven days for a more comprehensive assessment. As occupational therapy practitioners, we can utilize the voiding diary to establish a baseline of urinary frequency, type of incontinence (mild, medium, severe), and fluid intake from both food and liquids.
- Voiding diary can provide information about:
- Urinary frequency
- Incontinence type
- Fluid intake
- Time of occurrence
The diary helps us track when incontinent episodes occur, how much urine is leaked, and whether the individual remains dry or not. It also aids in identifying patterns and triggers for incontinence, such as certain foods or fluids, medication timings, or specific activities. Collaborating with the person and the healthcare team to define what constitutes an episode of incontinence ensures that we are addressing the individual's goals accurately.
Analyzing the voiding diary data allows us to tailor interventions based on the individual's patterns. For example, if someone is consistently experiencing incontinence at a certain time of day, we can plan toileting or provide a bedpan or urinal preemptively to promote continence during that period. This may be especially useful for individuals with cognitive impairments who may not be able to actively participate in bladder retraining or other interventions.
- The most important thing to document is an accurate count of incontinent episodes
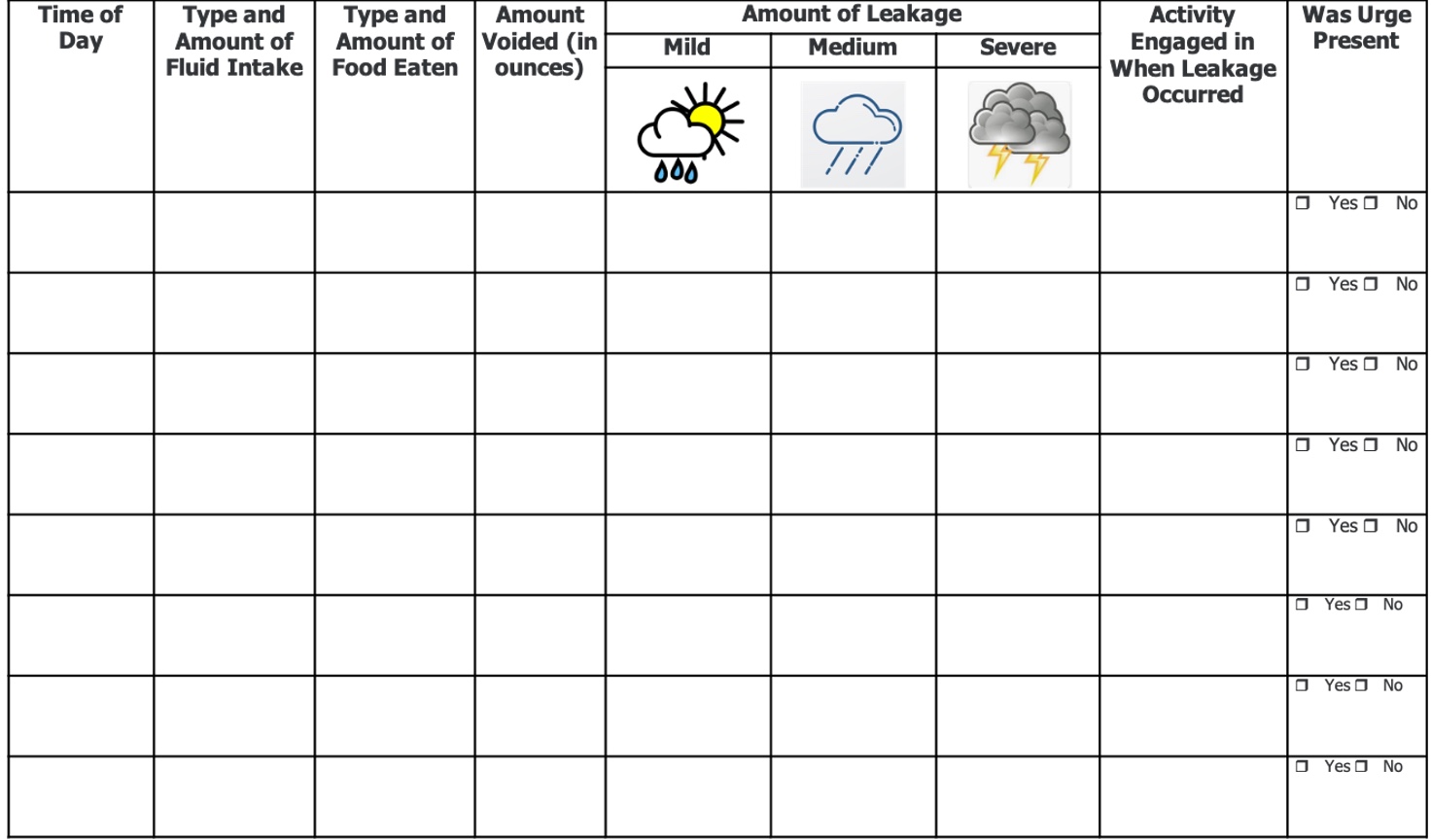
Figure 19. Example of a voiding diary.
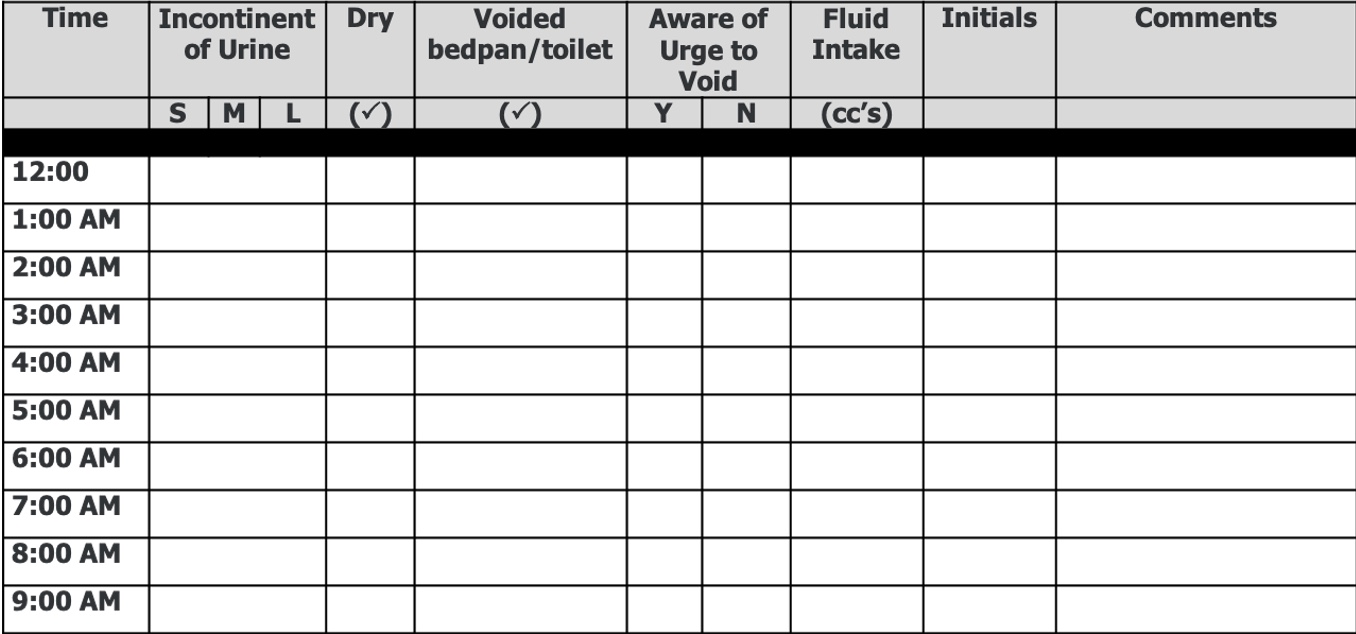
Figure 20. Another example of a voiding diary.
By using the voiding diary, we can make more informed decisions about behavioral and lifestyle modifications, such as scheduled toileting, fluid management, and dietary adjustments. The goal is to optimize bladder function and minimize incontinent episodes, thus improving the person's overall quality of life.
Nursing Interventions
- Teach pelvic muscle exercises
- Assess voiding patterns and maintain bladder records
- Assess for bladder irritating substances
- Assess for chronic constipation
- Encourage drinking 6-8 glasses of fluid
- Instruct on habitual voiding
- Implement a bladder-retraining program
Interdisciplinary collaboration is essential in addressing urinary incontinence effectively. Nursing interventions play a crucial role in managing and supporting individuals with incontinence. They can teach pelvic muscle exercises, assess voiding patterns, and identify irritating substances that may exacerbate the condition. Encouraging adequate fluid intake is also important to prevent dehydration, a common concern among seniors.
The concept of voiding habitually can be useful in certain cases where a person may benefit from adhering to a scheduled toileting routine to minimize accidents and embarrassment. Bladder retraining programs, gradually increasing voiding intervals, can be implemented to achieve a more regular voiding pattern.
- Teach relaxation techniques (e.g., deep breathing, imagery)
- Client education and instruction
- Encourage client to express concerns
- Review bowel patterns
- Respond promptly to requests for assistance
- Place bedside commode/nightlight
- Suggest assistive devices
- Advise against restrictive clothing
- External urine collection device
- Consult with physician
- Teach signs and symptoms of UTI
- Assess perineum, apply moisture barrier cream
- Change saturated pads promptly
- Inspect skin frequently
Nursing and occupational therapy practitioners contribute significantly to incontinence management. Relaxation techniques, such as deep breathing exercises and imagery, can be taught to help reduce anxiety and control the urge to void. Additionally, we can address environmental factors, such as providing bedside commodes and assisting with the selection of appropriate assistive devices or clothing modifications to enhance continence.
Evaluation and Documentation
Initiation of Skilled Therapy
- Medical diagnosis
- Treatment diagnosis should be:
- The reason skilled therapy is indicated
- What is causing the UI
The evaluation process for urinary incontinence involves a comprehensive assessment of the individual's medical and treatment history. Identifying the underlying cause of incontinence is crucial for effective treatment. As occupational therapy practitioners, we should also consider the impact of incontinence on the individual's quality of life, their ability to engage in meaningful occupations, and any maladaptive behaviors that may hinder their management of the condition.
Setting patient-centered and objective goals is essential in the treatment plan. These goals could include increasing pelvic floor strength to reduce leakage during specific activities or improving self-toileting abilities. The documentation should be detailed, outlining the strategies and interventions used for different types of incontinence, such as Kegel exercises for urge incontinence, adaptive clothing for functional continence, or temporary use of pads for overflow incontinence.
In some cases, we may be able to fully restore continence, while in others, our focus might shift toward compensation or adaptation. Training caregivers and patients in techniques to manage incontinence effectively can significantly enhance their ability to cope with the condition.
Therapy Evaluation
- Reason for Referral
- Prior Level of Function
- Chief Complaint
- Previous Treatments
- History - Past Medical, Surgical, OB/GYN, Medications
- Aggravating and Alleviating Factors - UI Symptoms
- Precipitating Events
- Skills and Functional Assessment
- Maladaptive Behavior
- Effect of UI on Quality of Life
- PVR
- Goals
- Treatment Plan
- Strengthening
- Environmental Modification
- Functional Maintenance Program
In the evaluation process for urinary incontinence, it's important to swiftly identify both the medical diagnosis and the treatment diagnosis. The focus of our treatment plan revolves around addressing the root cause of the incontinence. As we delve into the evaluation, the comprehensive assessment encompasses all necessary aspects, so I won't reiterate that here.
However, it's crucial to consider the impact on an individual's quality of life, including their chosen occupations and activities of daily living. Furthermore, we should be attuned to maladaptive behaviors. These can manifest in various ways, such as individuals crossing their legs or adopting certain postures in an attempt to manage incontinence. These behaviors can restrict their engagement in life activities and limit their overall well-being.
Our role as occupational therapy practitioners lies in identifying these maladaptive behaviors and collaboratively working with clients to develop strategies to overcome them.
Goals
- Goals related to the problem of UI episodes
- Increase strength of pelvic floor muscles as evidenced by no leakage during sit-to-stand transfers
- Patient to enjoy meals in dining room without need to toilet 4/7 days
- General goals
- Patient will increase UE strength from __ to __ to increase ability to self toilet / mobilize self in chair/bed
- Patient will be able to ambulate __ feet within __ seconds to increase ability to self toilet
When crafting goals for managing urinary incontinence, it's crucial to ensure that they are both objective and patient-centered. These goals need to reflect specific and measurable outcomes that directly relate to the individual's needs and preferences. For instance, one goal could be centered around enhancing pelvic floor strength, which can be measured by the absence of leakage during activities like sit-to-stand walking for a certain distance.
Another goal might focus on bolstering the person's ability to independently use the toilet. This goal could involve working toward specific milestones, such as achieving a consistent toilet schedule or mastering toilet transfers safely and effectively.
Functional Documentation/Types of Incontinence
Functional documentation is a crucial aspect of managing urinary incontinence, and it should be tailored to the specific type of incontinence a person is experiencing.
- Urge Incontinence
- Independent Kegel exercises/pelvic floor exercises
- Habit training/caregiver training
- Functional Maintenance Program
- Regular toileting every 2-4 hours
- Train caregiver to assist with exercises
- Behavior modification/relaxation techniques
For urge incontinence, you may discuss Kegel exercises, regular toileting strategies, caregiver training, and behavior modification techniques.
- Stress Incontinence
- Pelvic floor exercises
- Increase continence/controlled voiding
- Follow the established bladder program
- Functional maintenance program
- Manage clothing/briefs and pads
- Ability to use communication system
For stress urinary incontinence, interventions may involve using adaptive equipment, managing clothing, briefs, or pads, implementing a controlled voiding program, and establishing a functional maintenance program.
- Functional Incontinence
- Transfers and ambulation
- Toilet and bedside commode transfers
- Manipulate clothing/adaptive clothing
- Use communication system
- Maintain personal hygiene
- Negotiate around furniture
- Functional maintenance program
For functional continence, effective strategies can include utilizing adaptive clothing and implementing a communication system to signal the need for bathroom use, especially in skilled care environments.
- Overflow Incontinence
- Use pads/briefs for incontinence
- Manipulate equipment for self-catheterization
- Safely use the Valsalva maneuver and external abdominal pressure to facilitate emptying of the bladder
For overflow continence, interventions might involve the temporary use of pads or briefs while teaching the individual proper utilization. Additionally, techniques like the Valsalva maneuver could be taught to facilitate complete bladder emptying.
Functional Documentation/Model of Care
- Restoration
- Compensation
- Adaptation
As previously mentioned, these are the models of care we can consider.
- Restoration
- Increase active shoulder motion/strength for independence in personal hygiene
- Improve extremity/trunk strength for toilet transfers
- Improve fine motor coordination to manage clothing
- Follow a toilet schedule
In some cases, we can fully restore a person's continence ability. This could involve addressing personal hygiene, such as improving wiping techniques to prevent UTIs or focusing on toilet transfers and enabling individuals to independently follow their own toilet schedule.
- Compensation level
- Compensatory strategies for navigation/orientation
- Independent use of bedpan
- Environmental modification for safe toilet transfers
- Adding brake extenders for transfer safety
In situations where full restoration isn't possible, compensation strategies come into play. This might include enabling someone to independently use a bedside commode or providing orientation and navigation support to help them access the bathroom, especially in cases related to functional incontinence.
- Adaptation level
- Training caregivers to take the patient to the bathroom on a set schedule
- Training caregivers in the proper transfer techniques to promote safe transfers and limit episodes of stress incontinence due to the transfer method used
Adaptation becomes crucial in scenarios where full restoration is challenging. Teaching caregivers, whether they're nursing staff or the individual themselves, essential techniques to manage the situation is paramount.
This collaborative approach ensures that the person's needs are met effectively, even if complete restoration of continence is not achievable.
Role of Occupational Therapy
Why Should OTs Treat Incontinence?
- Incontinence and pelvic floor disorders have a profound impact on occupation, the daily activities that give life meaning
The field of urinary incontinence management offers a range of specialized training options. From electrical stimulation to biofeedback and beyond, these approaches can complement traditional methods. If you're truly dedicated to mastering these techniques, I encourage you to explore specialty certifications that can provide you with advanced knowledge and skills in urinary incontinence management. These certifications can enhance your ability to provide comprehensive care and support to individuals dealing with this condition.
Incontinence and Occupation
- UI is recognized as one of the leading causes of institutionalization of the elderly
- Impairments in bowel, bladder, and urogenital function result in loss of self-esteem, difficulty maintaining a healthy and independent lifestyle, and fulfilling relationships
- Activities outside the home, social interactions with friends and family, and sexual activity may be restricted or avoided entirely
The impact of urinary incontinence disorders on patients cannot be understated. These conditions significantly affect their capacity to participate in meaningful occupations and activities. As we've discussed, the implications extend beyond physical discomfort to encompass emotional well-being, self-esteem, and social interactions. Recognizing the profound consequences of these disorders emphasizes the importance of our role in providing effective care and support to enhance their overall quality of life.
Role of OT
- All occupational therapy practitioners have the education and training to provide the following skills defined as basic UI interventions.
It's essential to acknowledge your existing skills and capabilities in addressing urinary incontinence issues. As healthcare professionals, you possess a diverse range of expertise that can be harnessed to provide comprehensive care and meaningful interventions for individuals dealing with these challenges.
Basic OT Interventions
- Assessment and training of self-care skills
- Clothing management
- Toilet transfers
- Hygiene
- Recognition of toileting needs
- Environmental modifications
- Prompted or scheduled toileting programs
Your ability to assess various aspects of daily life, such as clothing management, transfers, hygiene, and toileting needs, allows you to comprehensively address the impact of urinary incontinence on an individual's functional abilities. Additionally, the programs we'll discuss shortly provide effective frameworks for addressing these challenges.
- Identification of the need for adaptive equipment or adapted techniques
- Raised toilet seat or bedside commode
- Adapted handles or methods of suppository insertion, toileting, etc.
- Use of adapted clothing fasteners
- Training in adapted techniques for intermittent self-catheterization and use of urine collection devices
Your expertise enables you to identify the necessity for adaptive equipment and interventions that can significantly enhance an individual's quality of life. These solutions can range from basic adjustments like using a raised toilet seat or adding handles and extenders, to more specialized interventions such as teaching intermittent self-catheterization or applying condom catheters.
Therapeutic Exercises
- Purpose:
- To improve function of the UE or LE, back and trunk and associated muscles that provide improved mobility, transfers and toileting – DO YOU REMEMBER THE LOWER QUADRANT FUNCTION????
You possess the foundational capability to provide exercises as part of your interventions. Remember the importance of lower quadrant function, which encompasses various aspects related to pelvic health and urinary continence.
- Exercises
- LE
- Sit to stand or stand to sit, Quad/Hamstring
- Squats
- UE
- Biceps/Triceps, armchair handles, pulleys
- LE
The exercises you provide for basic mobility can indirectly affect the Levator Ani muscles, which can be particularly beneficial for addressing issues related to failure to store urine.
- Exercises
- Standing performance
- Gait
- Hand dexterity
- Postural correction
- Strong pelvic floor, trunk, and proximal lower extremities will help maintain the position of the internal organs of the urinary system and thus impacts UI.
Exercises that target the core muscle group can have a positive impact on urinary continence. Let's now delve into some specific exercises to further illustrate this concept.
- Adductor Ther Ex
- Have patient sit or recline comfortably with a small rolled towel (6-inch diameter) placed between knees and ask patient to gently squeeze the roll for the count of 3-10 (based upon patient tolerance) and then relax for a count of 10. Repeat 10 times.
The first exercise, which is adductor ther ex, involves the patient placing a towel or a ball between their knees (shown in Figure 21- the left image).
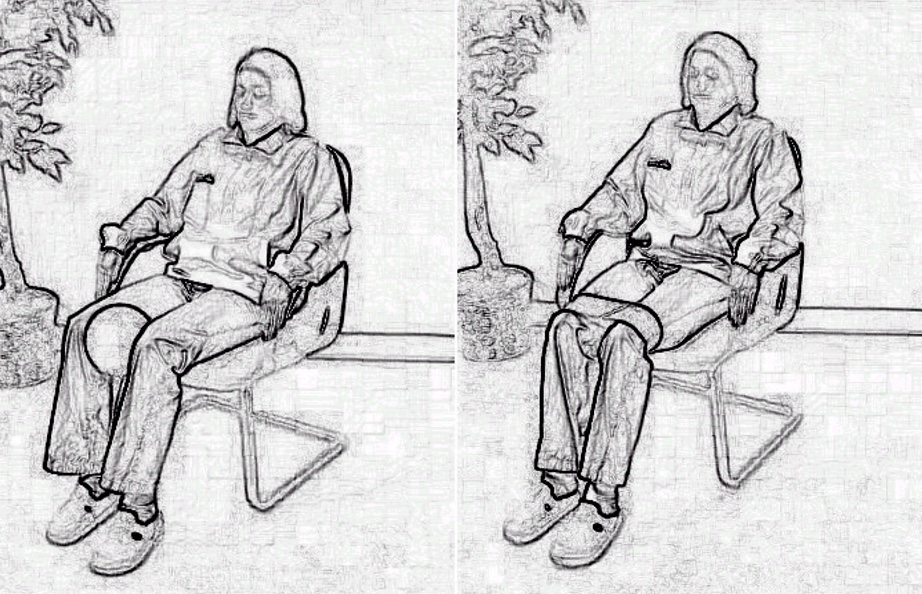
Figure 21. Adductor and abductor therapeutic exercise examples.
They are instructed to squeeze the object, hold the squeeze for a specific count based on their tolerance, and then relax it out for another count while maintaining continuous breathing. It's crucial to avoid breath-holding during the exercise, as that doesn't contribute to the desired impact on the diaphragm and the lower quadrant function. This exercise targets the adductor muscles and contributes to the holistic approach to addressing urinary incontinence issues.
- Abductor (Obturator Internus) Ther Ex
- Use a rolled towel as in adducter exercises. Gently secure theraband around thighs, just above the knee. Instruct the patient to gently roll knees out for a count of 3-10 (based upon patient tolerance); relax for count of 10
The next exercise is the abductor therapeutic exercise. In this exercise, the patient uses a TheraBand or a similar resistance band around their knees (also shown in Figure 21. They are instructed to roll their knees outward, holding the position for a specified duration, and then roll their knees back in. These exercises, like the previous one, contribute to targeting the core muscles and promoting the overall function of the lower quadrant, which plays a role in addressing urinary incontinence issues.
- Pelvic Floor Activation
- With patient standing with feet shoulder width apart, and toes laterally rotated 10 degrees, ask patient to do a 1-inch knee bend, count 3-10 (based upon patient tolerance) and rest for count of 10
- Gluteal sets
- With patient supine, ask patient to squeeze buttocks for a 3-5 count. Repeat 10 times
The next exercise is pelvic floor activation. For this exercise, the patient stands with their feet shoulder-width apart and toes laterally rotated. They perform a slight one-inch knee bend and hold the position, then return to the starting position. This exercise can be done with a few quick bends followed by a slower sustained hold. This exercise targets both fast-twitch and slow-sustained contractions of the pelvic floor muscles, which are vital for addressing urinary incontinence issues.
The last exercise mentioned is glute sets. This involves squeezing the buttock muscles. This exercise is relevant because the gluteal muscles are interconnected with the pelvic floor and anal sphincter muscles. Strengthening the gluteal muscles can have a positive impact on the overall support and function of the pelvic region, contributing to urinary continence.
- Transverse Abdominus Ther Ex
- With patient supine, knees flexed using a bolster, and upper extremities crossed resting on trunk/chest. Ask patient to lift head and shoulder off mat or bed using a smooth and consistent movement. Lower slowly. Repeat per patient tolerance. May use elevated patient bed initially, lowering as patient improves.
The next exercise is targeting the transverse abdominis, which involves a crunch-like movement. By engaging the transverse abdominis, you're further focusing on the lower body quadrant and the interconnected muscles. An example is shown in Figure 22.
Figure 22. An example of an exercise is standing.
If possible, encourage the patient to do four quick knee bends followed by a slower, sustained hold. Remember that the sphincters and pelvic floor muscles consist of both fast twitch fibers, which quickly prevent urine flow during moments of increased intra-abdominal pressure like sneezing or coughing, and slow twitch fibers that maintain a continuous low-level contraction to support the visceral contents.
- Treatment plan
- First 30 days
- PME Therapeutic exercises – mandatory per CMS for the first four weeks prior to e-stim application
- Functional treatment – transfers, gait, self-care management, toileting, adaptive equipment training, clothing management, safety environmental management
- Postural correction
It's important to note that electrical stimulation is subject to regulations, especially in skilled nursing facilities. The initial 30 days are crucial as this is the period when you will focus on exercises, functional interventions, correcting posture, and potentially implementing compensation or adaptation strategies. This early phase is essential for establishing a strong foundation for treatment and making significant progress.
- After 30 days, if skilled, continue with:
- UE/LE Exercises if skilled
- Postural correction
- ADL training
- Balance, gait, transfers, etc.
- Add e-stim(either MFAC or IFC) for pelvic floor muscle strengthening for urge, stress, or mixed UI
After the initial 30 days, if the skilled treatment phase continues and exercises like Kegel and pelvic floor exercises haven't effectively reduced incontinence episodes, you can consider incorporating additional interventions. This might involve adding medium-frequency alternating current Russian stimulation or an inferential stimulation. However, it's important to clarify that when we refer to a "failed" episode of pelvic floor exercises, it means that the exercises were correctly performed but didn't yield the expected results. This definition aligns with Medicare regulations and should not be mistaken for non-compliance or incomplete attempts. Other insurance providers might have varying criteria, but this insight pertains to Medicare standards.
Behavioral Training
Habit Training
- Toileting scheduled to match the patient’s voiding habits based on the voiding diary; to the toilet in advance of need
- Upon rising
- After meals
- After naps
- Before bed
- Goal is not every 2 hours
- Timed schedule: every 3-4, etc. hours
- Caregiver dependent
Scheduled toileting involves a fixed time schedule for voiding, often at regular intervals, like every three to four hours. However, this approach may not be person-centered or individualized, as people have different natural voiding patterns. Some individuals may find success with scheduled toileting, but it might not work for everyone and can lack flexibility. It's important to consider the preferences and needs of the individual when determining whether to implement scheduled toileting as part of their care plan.
Voiding Options
- Prompted voiding
- Recommended in patients who can learn to recognize some degree of bladder fullness or the need to void or who can ask for assistance or respond when prompted to toilet
- Double voiding
- Recommended for those individuals who do not completely empty the bladder
Prompted voiding is a strategy where caregivers prompt individuals to use the bathroom at specific times or when they show signs of bladder fullness. Instead of asking if the person needs to use the bathroom, the approach involves checking if they are wet or dry and then guiding them to the bathroom if needed. Positive reinforcement or recognition is often used when the individual successfully follows through with the prompt. This approach can be helpful in assisting individuals with recognizing their own bodily cues and maintaining continence.
Double voiding is a technique used to help individuals fully empty their bladder, especially if they have difficulty completely emptying it in one attempt. The process involves initially urinating, then standing up or shifting weight, followed by sitting down again and taking a few deep relaxation breaths. This aims to encourage the bladder to release any remaining urine that may not have been expelled during the initial voiding. This technique can be particularly useful for those with incomplete bladder emptying issues.
Bladder Training
- To postpone voiding
Bladder training involves techniques aimed at helping individuals gradually increase the time between voiding episodes. The goal is to strengthen the pelvic floor muscles and develop better control over the urge to urinate. Bladder training may include postponing voiding until the bladder feels fuller, inhibiting the urge to void, and gradually extending the time between voids. This can be challenging but can lead to improved bladder control over time.
Urge Inhibition Training
- Techniques for resisting or inhibiting the sensation of urgency
- Bladder training and urge inhibition training are strongly recommended for urge and mixed incontinence and also recommended for the management of SUI.
Urge inhibition training focuses on resisting the urge to void and postponing it for longer periods. The approach may involve starting with short intervals and gradually working up to longer periods between voiding. Adjusting fluid intake can also play a role in this training. Education, positive reinforcement, and scheduled mandatory voiding are components of these programs, particularly suitable for individuals who are cognitively capable of participating.
Bladder training and urge inhibition training have strong evidence supporting their effectiveness and are rated at an A level of recommendation for addressing urinary incontinence.
ADL Training
- Environmental - bedside commode, urinal, room closer to the toilet
- Clothing modifications – zippers, Velcro
- Toileting independence strategies
- Self performance in locomotion and transfer
- Self performance in toilet use/hygiene
- Memory/cognition strategies
Regarding ADL training, we've briefly touched upon this topic, and I believe there's no need to reiterate it extensively. However, ADL training involves various approaches, such as memory or cognition strategies, as well as reminders. Environmental adjustments can also play a role in this context, along with clothing management strategies and potential adaptations. These strategies aim to address the impact of urinary incontinence on daily life activities and promote effective management within individuals' routines.
Pelvic Muscle Rehabilitation
- Pelvic Muscle Group Exercise (Kegels)
- Electrotherapy Assisted
- Biofeedback Assisted
- Related Therapeutic Exercise
- Adductor Ther Ex
- Abductor (Obturator Internus) Ther Ex
- Pelvic Floor Activation
- Gluteal Sets
- Transverse Abdominus Ther Ex
- Increase urethral and anal closure pressure
- Increase muscular support of the pelvic viscera
- Improves cerebral control of micturition
- Reduces urgency
- Enhances voluntary inhibition of urgency
- Improves functional angles at the bladder neck and in the rectum
In the context of pelvic muscle rehabilitation, it's important to recognize that these exercises can be integrated with biofeedback or electrotherapy if applicable. The goal of this approach is to enhance closure and control of micturition, ultimately reducing the frequency of voids and urine loss. Isolating the correct muscle group can be achieved through various methods, such as tightening muscles to prevent gas passage or voluntarily stopping the urine stream during voiding. Feedback mechanisms, like resting a hand on the stomach or observing movements, can help ensure correct execution.
When discussing exercise regimens, it's essential to address how to find and perform these exercises effectively. Traditionally, quick contractions followed by rapid relaxation, as well as sustained contractions for about five seconds, are suggested. Variations in positions – sitting, lying, standing – are important as voiding control should be achieved across different situations. Promoting relaxation through controlled breathing is also an integral part of the exercise.
For a more comprehensive approach, a home exercise program can be tailored to specific types of urinary incontinence. A structured regimen for stress urinary incontinence or urge urinary incontinence can be developed over several weeks to address individual needs and gradually enhance pelvic floor muscle control. This approach is not only limited to skilled settings but also encourages patients to continue the exercises independently, thus contributing to their overall improvement.
Rehabilitation Results
- Decreased number of incontinent episodes
- Decreased volume of urine loss
- Decreased number of voids per day
- Increased bladder capacity
- Increased strength/tone of pelvic muscles
- Increased QUALITY OF LIFE
The overarching objective of pelvic muscle rehabilitation is to enhance closure mechanisms, regain control over the process of micturition, and ultimately reduce the frequency of daily voids while minimizing urine loss.
Pelvic Floor Muscle Exercises
- How to isolate the muscle group
- How to know if you’re performing correctly
- Traditional Kegel exercises
- Quick twitch
- Slow twitch
- Impacting the cortical loop through relaxation and Kegel exercises
Isolating the pelvic muscle group can be achieved through various techniques. Patients can tighten their muscles to avoid passing gas or voluntarily interrupt the flow of urine while voiding. Different methods involve inserting a finger into the anus for both genders or the vagina for females. For males, moving the penis up and down can also help isolate these muscles.
- Clients are often given the exercises with little explanation from the healthcare professional
- Written and verbal instructions alone are often inadequate
- 30% perform incorrectly even with intensive instruction
Correct execution is crucial, which can be determined by checking for abdominal movement while resting a hand on the stomach or observing hip movement in front of a mirror.
- Find the muscles
- Tighten muscles to avoid passing gas
- Wink the rectum
- Voluntarily stop urine stream
- Squeeze muscles around finger inserted in anus or vagina
- Move penis up and down
- Squeeze and relax the muscle quickly 4-5 times
- Squeeze the muscle for 5 seconds, relax for 5 seconds
- Repeat 5-10 times
- Repeat exercises 3 times during day
- Perform exercises lying, sitting, standing
To perform traditional kegel exercises, individuals can rapidly contract and relax the muscles a few times to engage the fast-twitch fibers. Then, they can hold the contraction for about five seconds, followed by relaxation for the same duration.
- Perform exercises 3 times each day, 5-10 repetitions each session
- Perform the exercises in different positions each session
- Time of day is not critical
- Impacting the cortical loop through relaxation and Kegel exercises
This cycle can be repeated five to ten times several times a day in various positions such as sitting, lying, and standing. Adding variations to the exercises can impact the cortical loop, influencing both quick contractions and sustained relaxation. Practicing kegel exercises with controlled breathing can help maintain a balance between sustained contraction and relaxation, aiding in controlling the micturition reflex and improving bladder control.
Stress and Urge UI Exercise Programs
The following slides provide a detailed home exercise program for both stress urinary incontinence and urge urinary incontinence. This program spans several weeks and offers a structured approach to addressing these specific types of incontinence. It's important to note that this program serves as a guideline and can be adapted to meet individual patient needs. Since some of these exercises transition to non-skilled activities relatively quickly, they can be effectively taught to and continued by the patients themselves. This emphasizes the importance of patient education and empowerment in managing their urinary incontinence concerns.
- Stress UI
- Week 1
- Exercise – quick Kegels
- 2 sets of 15 repetitions in each position – sitting, standing, and lying
- Week 2
- Exercise – slow Kegels with 3 second hold
- 2 sets of 10 repetitions in each position – sitting, standing, and lying
- Week 3-4
- Exercise – slow Kegels with 5 second hold
- 2 sets of 10 repetitions in each position – sitting, standing, and lying
- Week 5-6
- Exercise – slow Kegels with 10 second hold
- 2 sets of 15 repetitions in each position – sitting, standing, and lying
- Week 1
- Urge UI
- Week 1
- Exercise – quick Kegels
- 2 sets of 15 repetitions in each position – sitting, standing, and lying
- Week 2
- Exercise – slow Kegels with 3-5 second hold
- 2 sets of 10 repetitions in each position – sitting, standing, and lying
- Week 3
- Exercise – slow Kegels w/ 5-7” hold
- 2 sets of 15 repetitions in each position – sitting, standing, and lying
- Week 4-5
- Exercise – slow Kegels w/7-10” hold
- 2 sets of 15 repetitions in each position – sitting, standing, and lying
- Week 6+
- Exercise – slow Kegels with 10+ second hold
- 2 sets of 15+ repetitions in each position – sitting, standing, and lying
- Week 1
Treatment Strategies
Behavioral Therapy
- Bowel and bladder retraining
- Prompted and scheduled toileting
- Habit training
- Pelvic muscle re-education
- Dietary and fluid modifications
Lifestyle Interventions
- Fluid and diet modification
- Prevention
- Weight loss
- Smoking cessation
- Relaxation
As mentioned, we've discussed certain approaches already, as above, in the two categories. Weight loss and smoking cessation are important factors, and we've delved into them. Relaxation techniques have also been covered briefly, so I won't revisit those in detail.
Let's now delve into continence management strategies. It's important to consider the type of incontinence a person is experiencing, and this is where the initial assessment becomes crucial. Understanding the specific type of incontinence helps tailor the management approach to address the underlying causes and issues.
Urge Continence Management Strategies
- Urge Incontinence: Sudden need to urinate
- Treatment
- Behavioral strategies
- Habit and bladder training
- Relaxation
- E-stim
- Treatment
When dealing with urge incontinence, behavioral strategies are key. Implementing techniques like habit training, bladder retraining, and relaxation exercises can help individuals regain control over their urgency to void. Electrical stimulation and biofeedback are also useful tools to consider.
Stress Continence Management Strategies
- Stress Incontinence: Leakage of Urine
- Treatment
- Pelvic floor exercises
- E-stim
- Treatment
For stress urinary incontinence, focusing on the pelvic floor is indeed essential. Pelvic floor exercises play a central role in strengthening the muscles that support continence. Electrical stimulation and biofeedback can also aid in improving pelvic floor function.
Functional Continence Management Strategies
- Functional Incontinence: Socially unacceptable urine outflow
- Treatment
- Habit training
- Scheduling
- Behavior modification
- Strength, ROM, gait, transfers, ADL training
- Treatment
In cases of functional incontinence, establishing a routine schedule for toileting can be beneficial. Behavior modification techniques can be used to encourage regular bathroom visits and overcome any obstacles that might hinder the person's ability to reach the restroom in time. This is particularly important when dealing with individuals who may have cognitive or mobility challenges.
Overflow Continence Management Strategies
- Overflow Incontinence: Leakage of Urine
- Treatment
- Medications
- Adaptive equipment
- Habit training
- Treatment
When addressing overflow incontinence, a comprehensive approach is important. This could involve considering medications, though this aspect may fall outside the scope of occupational therapy. Adaptive equipment might be helpful in managing this condition, and habit training can play a role in optimizing bladder emptying. Additionally, the use of pads or other continence products can provide practical support to manage episodes of overflow.
Treatment Parameters: Bladder Retraining
- Bladder Retraining
- Request patient to delay void until scheduled time
- Begin with patient’s natural frequency
- Vary schedule when patient feels urge to void, have patient take 2 deep breaths, use relaxation and distraction, contract pelvic floor muscles, wait 10 minutes, rise slowly and walk to bathroom to void.
Bladder retraining can be a very effective strategy. Varying the voiding schedule and utilizing relaxation techniques are key components. Guiding patients to contract, wait, and then void slowly can help them gain better control over their bladder and reduce episodes of incontinence. The combination of physiological and behavioral approaches can contribute to successful outcomes in managing urinary incontinence.
Desired Outcome: Bladder Retraining
- Increased control over urge sensation and training of bladder to accept greater volumes of urine
- Eliminate episodes of urge and stress incontinence
- Increase independence and involvement in ADLs and social activities
The ultimate goal of these strategies is to help individuals gain control over their urge sensations and eliminate episodes of urge incontinence. By employing techniques such as bladder retraining, relaxation, and distraction, patients can learn to better manage their bladder function and regain control over their urinary patterns.
Treatment Parameters: Timed or Habit Voiding
- Request that patient void each hour
- As patient demonstrates longer dry periods, increase time by 15-minute increments as patient is able
Timed or habit voiding involves gradually increasing the intervals between voids based on the patient's ability to maintain longer dry periods. This approach aims to improve bladder control by gradually extending the time between trips to the bathroom. During these extended intervals, patients can engage in various strategies, such as exercises or dietary adjustments, to help manage their urinary patterns effectively.
Desired Outcome: Establishment of Timed Voiding Plan
- Reduce leakage
- Increased independence in activities of daily living
The primary goal of timed or habit voiding is to reduce instances of leakage and establish a more controlled and predictable voiding pattern. By gradually extending the time between voids and implementing strategies to manage urinary function, individuals can regain bladder control and minimize the impact of incontinence on their daily lives.
Treatment Parameters: Prompted Voiding
- Monitor patient – caregiver asks patient if he/she is wet or dry
- Prompt patient – caregiver verbally asks patient to attempt to void
- Praise patient – caregiver praises patient for a successful void
Prompted voiding involves assisting the individual in recognizing their need to void and guiding them to the bathroom to avoid accidents. By providing verbal cues or reminders, caregivers or healthcare professionals can prompt the person to attempt to void at appropriate intervals.
Desired Outcomes: Prompted Voiding
- Reduced episodes of incontinence
- Increased independence and involvement in activities of daily living
- Improved patient morale and participation in social activities
The key objective is to enhance the individual's sense of independence and accomplishment while also reducing the occurrence of incontinent episodes. Through positive reinforcement and support, prompted voiding helps individuals regain a sense of control over their bladder function and maintain their dignity.
Treatment Parameters: Double Voiding
- After patient has voided once, request patient to stand up for a few seconds, sit back down, and try to void a second time
Double voiding involves encouraging the individual to void twice within a short span of time to ensure that the bladder is more fully emptied. By sitting on the toilet, then standing up and shifting positions, and finally sitting down again to void a second time, individuals can prevent residual urine from remaining in the bladder.
Desired Outcomes: Double Voiding
- No leakage between voiding
- Decreased burden of care
This approach aims to alleviate the need for frequent voiding, reducing the burden of care and improving the overall efficiency of the bladder. Ensuring that the bladder is adequately emptied can help minimize the frequency of incontinent episodes and promote a more consistent and manageable voiding pattern.
Treatment Parameters: Pelvic Floor Exercises
- Pelvic Floor Exercises
- Patient to perform the exercises in side-lying, supine, sitting, and standing
- Five to ten repetitions of each exercises
- Performed 3-5 times each day
We previously covered the importance of pelvic floor exercises for addressing both stress and urge incontinence.
Desired Outcomes: Pelvic Floor Exercises
- Reduce leakage
- Increased independence with stress incontinence
Our focus remains on addressing stress and urge incontinence to reduce instances of leakage.
Treatment Parameters: Relaxation
- Ability to relax abdominal muscles and intra-abdominal pressure while maintaining pelvic floor contraction
We've previously delved into the significance of relaxation in conjunction with pelvic floor exercises.
Desired Outcomes: Relaxation
- Muscle and bladder control facilitated
- Minimize urge incontinence
The balance between strengthening and relaxing those muscles is crucial for addressing both stress and urge incontinence. I'll refrain from revisiting these points, as our previous discussions have covered them comprehensively. This recap serves as a quick reference for your understanding.
Treatment Parameters: Electrical Stimulation
- Requires specialized training
- Duration 2-4 weeks
- Only after a failed attempt at Kegel exercises
- Increased strength of pelvic floor musculature to reduce leakage and improve storage capacity.
It's important to be aware of your state's practice regulations and certifications when it comes to utilizing electrical stimulation. This intervention becomes relevant when traditional methods, including Kegel exercises, have been exhausted and your aim is to strengthen the pelvic floor muscles. It is important to adhere to professional guidelines and exhaust traditional options before considering advanced techniques.
Case Studies
- Determine type of incontinence
- How do you know this?
- Other contributing factors?
- Program/treatment goals
- Treatment interventions
- Behavioral, physical, interdisciplinary
Case studies can be a great way to tie together the concepts we've discussed. Analyzing specific scenarios will help illustrate the application of various strategies for different types of incontinence and contributing factors.
Case Study A
- 87 y/o female with R hip fracture
- Hx CVA with right hemiparesis, MI
- Leakage with transfers
- Drinks tea and OJ
- Has not started pelvic floor exercises
This case study illustrates how a comprehensive approach is crucial in managing urinary incontinence in older adults. The patient, an 87-year-old female with a history of right hip fracture, CVA, hemiparesis, and MI, presents with leakage during sit-to-stand and transfers. Her daily intake includes three cups of tea and one glass of orange juice. Notably, she hasn't yet started pelvic floor exercises.
- Type of incontinence
- Stress UI
- Other contributing factors
- Clothing management?
- Dietary considerations?
- Will exercises be helpful?
Analysis reveals stress urinary incontinence due to her leakage during movements. Contributing factors involve impaired clothing management due to her hemiparesis, which can hinder toileting. The potential impact of dietary irritants like tea and OJ is considered. The uninitiated pelvic floor exercises suggest the need for strength training.
- Program/treatment goals
- Education re: appropriate water intake and effect of bladder irritants.
- Increase strength and tone of pelvic musculature
- Increase coordination, balance, and UE function to independently manage clothing with toileting
Proposed interventions encompass improving water intake, modifying bladder irritants, enhancing strength and tone, addressing relaxation, coordination, and balance, and fostering independence in toileting.
- Treatment interventions
- Training in Self Care
- Therapeutic Exercise
- Therapeutic Activity
Strategies encompass self-care, exercise, bladder and bowel training, potential adaptive equipment, and clothing management. This case exemplifies how individualized and multifaceted strategies address the complex nature of urinary incontinence management.
Case Study B
- 65 y/o male hx prostate cancer, diabetes
- Never knows he needs the bathroom until too late
- Assist for transfers due to weakness and LOB
- Cluttered room
In this second case, a 65-year-old male with a history of prostate cancer and diabetes presents a different set of challenges.
- Type of incontinence
- Overflow UI
- Other contributing factors
- Cannot make it to bathroom in time
- Weakness, loss of balance
- Cluttered room
- Unsafe ambulation
- Decreased transfer ability
He complains of not realizing he needs to use the bathroom until it's too late, indicating overflow urinary incontinence. His minimal transfer assistance is due to weakness and occasional balance issues. His room's clutter and his maladaptive behavior of grabbing onto furniture while walking to the bathroom present additional factors.
- Program/treatment goals
- Strength/balance for transfers and decrease time it takes to get to bathroom
- Environmental modification; bedside toilet
- Functional mobility with assistive device
- Medical and nursing intervention
- Scheduled toileting based on void diary
It's evident that addressing his incontinence requires a holistic approach. First, decluttering his room would enhance safety and mobility. Second, targeting his balance and strength deficits is essential to facilitate timely bathroom visits. The option of using a bedside toilet or urinal might also be considered.
- Treatment interventions
- Training in Self Care
- Therapeutic Exercise
- Neuromuscular Reeducation
- Therapeutic Activity
Goals encompass improving strength, balance, and reducing the time required to reach the bathroom. Functional mobility training with an assistive device, such as a walker, can aid his transfers. Collaborative efforts may involve medications, protective undergarments, and possibly scheduled toileting based on a voiding diary. These interventions, involving various disciplines, contribute to a comprehensive approach to managing his urinary incontinence.
Case Study C
- 87 y/o female w/CVA, speech deficits, unilateral neglect, spasticity
- Hx UTI
- Leakage worse at night, large amounts
- Assist for toileting, transfers, mobility, and hygiene
Lastly, let's consider the case of an 87-year-old female with a CVA history, residual speech deficits, unilateral neglect, and spasticity affecting her upper and lower body. She's also experienced recurrent bladder infections, with leakage throughout the day, worsening at night, especially with larger amounts of leakage. Her cessation of enjoyable baking activities might be a result of psychosocial factors.
- Type of incontinence
- Urge UI
- Other contributing factors
- Symptoms worse at night, large volumes
- Bladder infection/UTI
- Not attending activities
- Assistance for transfers, hygiene, mobility
- Baking activities?
This complex scenario suggests urge urinary incontinence as a likely culprit. Given her recurrent UTIs, teaching proper hygiene techniques becomes crucial. Additionally, her cognitive and communication challenges necessitate tailored strategies for conveying her needs.
- Program/treatment goals
- Increase strength and balance for transfers
- One-handed techniques
- Adaptive equipment instruction
- Compensatory techniques for communication
- Clothing protection
- Staff training in activities dept
- Nutritional assessment
- Functional mobility training with assistive device
- Scheduled toileting
- Environmental modification
The overarching goal involves enhancing her strength and balance for transfers.
- Treatment interventions
- Training in Self Care
- Therapeutic Exercise
- Neuromuscular Reeducation
- Therapeutic Activity
- Treatment of Speech Language
Specialized techniques for one-handed toileting may be essential due to her CVA history. Collaborating with speech-language pathology can help devise effective communication approaches. For her physical limitations, addressing spasticity, unilateral neglect, and visual adaptation becomes integral. Educating staff, especially in the activities department, on her needs and preferences is vital to her participation in meaningful activities. Dietary considerations, such as identifying bladder irritants, may contribute to reducing her symptoms. The integration of scheduled toileting while engaging in her chosen activities aligns with her preferences.
Wrap Up
Continence Management Outcomes
- Significant cost reduction
- Prevention of complications requiring more extensive treatment and cost
- Psychological lift to patients and families
- Re-entry into the community or a lesser required level of care
- Facility-level commitment to care
To conclude, the evidence presented by studies cited by the Agency for Healthcare Research and Quality (AHRQ) demonstrates the potential for substantial improvements in urinary incontinence rates, possibly reaching up to 90%, by employing a combination of traditional pelvic muscle exercises, along with supplementary methods like electrical stimulation or biofeedback. Achieving this outcome entails more than just financial considerations; it involves addressing psychological and emotional well-being, as well as the ability to reintegrate individuals into the community and reduce the intensity of care needed. However, the success of these strategies hinges on the commitment and collaboration of the entire healthcare team, including occupational and physical therapists, nursing staff, patients, families, and dietary specialists. Ultimately, the patient's needs and preferences must remain at the forefront of our efforts for these interventions to truly make a meaningful impact.
Questions and Answers
Is cranberry juice or lemon juice helpful for UTIs?
Cranberry juice may act as a lower-level irritant, but it does not significantly irritate the bladder in most cases. Regarding lemon juice, I have not come across specific recommendations for using it in relation to UTIs. However, it is essential to recognize that not everyone will experience the same level of irritation from various foods and beverages. Individual responses can vary widely.
Are intravaginal and intrarectal exams important to ensure proper pelvic floor activation?
That's a great question, and thank you for asking. In my opinion, often we can determine adequate activation without resorting to these methods. However, if we're having trouble assessing activation accurately, then using probes could be beneficial. I have no objections to patients using probes to assist in identifying and perfecting their pelvic floor activation. If it helps them visualize their efforts and receive real-time feedback, it can be a valuable tool.
Can occupational therapy address behavioral issues related to incontinence?
Occupational therapy can play a significant role in addressing behavioral aspects of incontinence. For example, in cases involving dementia, behavioral interventions can be employed to understand the underlying causes of atypical urinary behaviors. By addressing the root of such behaviors, we can contribute to managing and improving incontinence issues that may be linked to behavioral triggers.
References
Cunningham, R., & Valasek, S. (2019). Occupational therapy interventions for urinary dysfunction in primary care: A case series. American Journal of Occupational Therapy, 73(5), 7305185040p1–7305185040p8.
Due, U, Klarskov, N, Gräs, S, & Lose, G. (2019). Pelvic floor muscle training with and without supplementary KAATSU for women with stress urinary incontinence - a randomized controlled pilot study. Neurourology and Urodynamics, 38: 379– 386.
Jose, P. & Kumar, V. (2020). Effect of combined pall of press and Kegels training for urinary incontinence in multigravida women and quality of life. Indian Journal of Physiotherapy & Occupational Therapy, 14(1), 167-171.
Molitor, W. L., & Nadeau, M. (2020). Occupational therapy for older women with urinary incontinence. SIS Quarterly Practice Connections, 5(3), 24–26.
Singh, N., Arya, K.N., & Pervin, A. (2017). Synergistic action of deep abdominals and pelvic floor muscles: Implication for incontinence management in women. Indian Journal of Physiotherapy and Occupational Therapy, 11(3), 66-69.
Citation
Weissberg, K. (2023). Pelvic muscle dysfunction and continence improvement: A primer for occupational therapy. OccupationalTherapy.com, Article 5629. Available at www.occupationaltherapy.com
