Editor's note: This text-based course is a transcript of the webinar, Polyvagal Theory And Chronic Pain: Exploring Treatment Options, presented by Zara Dureno, MOT.
Learning Outcomes
- After this course, participants will be able to evaluate the different trauma responses in the body and how they relate to pain.
- After this course, participants will be able to compare and contrast 4 different techniques for managing trauma responses.
- After this course, participants will be able to define chronic pain and describe how it is produced in the body.
Who I Am!
I am excited to be here. The polyvagal theory is one of my favorite things to talk about. When I first learned about it, I thought it just made everything make sense, so I hope this is the same for you today.
When we learn about polyvagal theory, it is beneficial for anyone with a nervous system. This content will be helpful for everyone, especially in the context of trauma, chronic pain, and longstanding conditions.
The image on the left is from when I was 12 (Figure 1). I was in a serious horseback riding accident that left me in pain for about ten years.

Figure 1. The left image is of the author after a horseback riding accident, and the right image is of the author hiking.
Learning about chronic pain science and polyvagal theory helped me to manage my pain. This is me on the right after climbing a wonderful mountain in Coquitlam, BC. I was able to get over my pain to do this. My passion for explaining this is because I think it is incredible what we can do with our brains and our nervous systems, and I want to give that knowledge to everyone because it is so beneficial.
What is Chronic Pain?
- "Chronic pain was defined as persistent or recurrent pain lasting longer than 3 months.” (Treede et al., 2015)
- No pain receptors in the body, but there are nociceptors. These are interpreted through the RAS, limbic system, and frontal cortex.
- How we think about pain and our emotions, affect how much pain we are in.
- The more amygdala activation, the more pain.
What is chronic pain? I did another presentation for OccupationalTherapy.com about chronic pain and concussions. In that one, I go a lot more in-depth into chronic pain. In this one, I will go a lot more in-depth into polyvagal theory. You can go to that presentation if you are craving more about chronic pain after this.
Chronic pain is persistent or reoccurring pain lasting longer than three months. After that three-month mark, we would expect that most things would be healed, like our muscles, bones, and ligaments. Usually, these structures do not take longer than three months to heal, and there is typically some level of nervous system involvement.
The second point is that there are no pain receptors in the body. We have receptors that detect heat, chemical changes, and pressure called nociceptors. However, they do not see pain per se. If there is enough heat, pressure, or chemical change, the information gets sent up through the spine into the brain, where the brain interprets it.
The different areas in our brain that interpret that information are the reticular activating system, the RAS, the limbic system, and the frontal cortex. We will mainly be talking about the limbic system component today, but the reticular activating system and frontal cortex are also important in pain.
The reticular activating system alerts us and keeps us awake, so getting enough sleep is essential for pain. This is where occupational therapists can come in with our sleep hygiene interventions.
Our frontal cortex involves our thoughts about pain. If you are trained in things like cognitive behavioral therapy or CBT, this can help people challenge their thoughts around pain. And as you can imagine, if these parts of our brain are needed to produce pain, they can also do the opposite. They can tell our bodies that we are safe and do not need pain.
When we have chronic pain lasting longer than three months, our body is sensitized, and there is more limbic system activation. The small almond-shaped part of our brain, called the amygdala, is responsible for sympathetic activation and fear. This part of our brain becomes very active. When that part of our brain is active, it will create more pain because the limbic system is involved with pain. Amygdala activation gets louder, especially if chronic pain happens from a traumatic event. The more amygdala activation, the more pain.
We want to think about how our clients are thinking about their pain and what their emotions are. We can also notice if our clients have these survival responses that pertain to this amygdala activation, which we are going to learn about.
Why Do Some People Have Persistent Pain?
- Mentally: Stress, depression, anxiety, trauma
- Personality: Self-critical perfectionism, Type “A” (Kempke et al., 2014)
- Physically: Bones, muscles, nerves, and ligaments typically take 6-8 weeks to heal from an injury
- Cancer, arthritis, and nerve damage can sometimes cause chronic pain, but these things are generally noticeable on imaging and have a component of sensitization
- Weaker supporting muscles, stretched ligaments, compensatory movements, and tension in muscles can cause physical pain.
Why do some people have persistent pain? We know there are mental factors. If somebody is under a lot of stress, there is amygdala and limbic system activation. If someone has depression, anxiety, and a history of trauma, they are more likely to have persistent pain
Another thing is personality. If somebody is self-critical, a perfectionist, or has a type A personality, they are more apt to have chronic pain.
Physically, a person's bones, muscles, nerves, and ligaments take six to eight weeks to heal. Still, we might see weaker supporting muscles, stretched ligaments, or compensatory movements. This is something we may notice as OTs when they are doing different activities of daily living. We may see compensatory movements or bracing.
Bracing also tells us there might be some of that amygdala sympathetic nervous system activation. Bracing is involved with our survival responses.
Another thing to be concerned about is clients with cancer, arthritis, or nerve damage. We want to ensure that they are getting the proper assessments. Many things are noticeable on imaging and will have a component of sensitization. Sensitization of the nervous system will be a component in almost all chronic pain.
For those whose original injury has healed, we may take them from a 10 out of 10 pain rating to a 4 out of 10 pain rating. Or, somebody who has chronic pain from arthritis might reduce their pain to a 7 instead of a 10. There may be an underlying physical thing continuously happening, but we can still mitigate some of that pain because we can work on the sensitization component.
What is Polyvagal Theory?
- “Polyvagal Theory describes an autonomic nervous system that is influenced by the central nervous system and responds to signals from both the environment and bodily organs. The theory emphasizes that the human autonomic nervous system has a predictable pattern of reactivity, which is dependent on neuroanatomical and neurophysiological changes that occurred during evolution”. (Porges, 2018)
- A THEORY that is a valuable framework for helping our clients.
You probably learned about the sympathetic and parasympathetic nervous systems in your anatomy classes. The sympathetic nervous system is activated, and the parasympathetic nervous system is slowed down, traditionally called "rest and digest."
The polyvagal theory was introduced to divide the parasympathetic nervous system into two parts. Parasympathetic is the freeze response, slowing down in response to a threat, and rest and digest.
The vagus nerve runs from the base of our spine into our pelvis. It is called vagus because "vagus" means wandering in Latin. The vagus nerve wanders all through our body. We will discuss different ways to interact with this nerve later in this presentation. Figure 2 is an overview of the parasympathetic and sympathetic nervous systems.
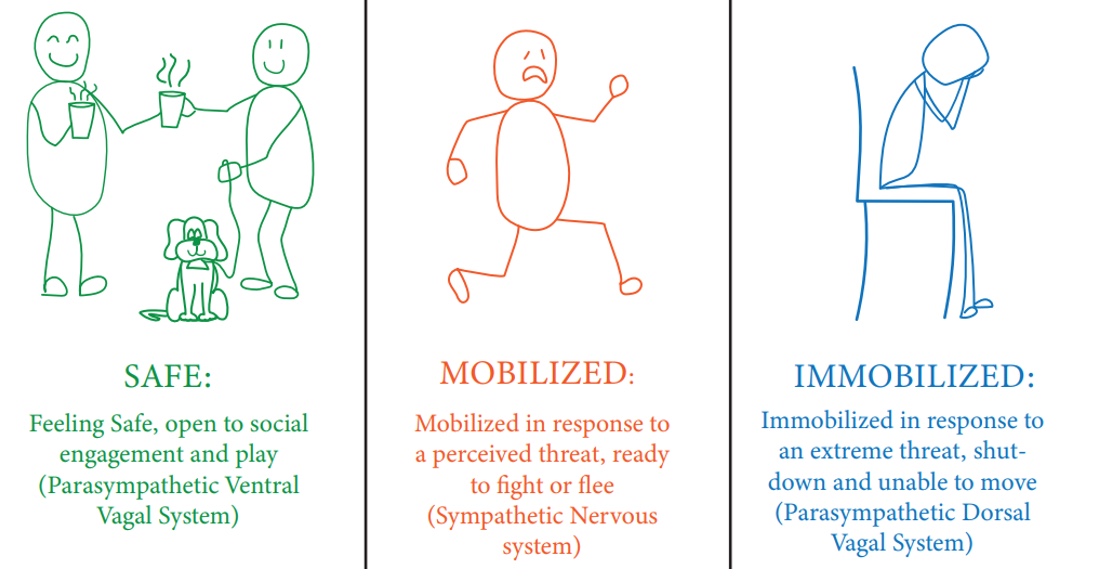
Figure 2. Overview of the parasympathetic and sympathetic nervous systems.
The ventral vagus nerve runs from the bottom of the spine into the stomach, and it is responsible for our rest and digest. The base is the dorsal vagus nerve and is the immobilized/freeze response.
This is a theory and a practical framework in the context of chronic pain for our clients. In people with pain, we often see a survival response and amygdala activation with either the sympathetic activation or freeze response when we see people with pain. As I said, this can be very helpful for our day-to-day lives because things can be stressful. We can always use more nervous system regulation.
Autonomic States (Fight/Flight/Freeze/Fawn)
The autonomic states are flight, fight, freeze, and fawn. You might have heard of the first three. The last one was more recently added so it might be new to you.
Before we get into this, I want you to do a little mental experiment. I want you to close your eyes and imagine yourself walking in the woods. The sun is going down, and it is starting to get dark. You spent too much time in the woods, and now you are trying to get out. You are almost near the trail's end, but you hear a couple of twigs snapping and a loud noise. Our nervous system will respond because it is trying to help us survive. Immediately, we will have some activation in that limbic system, our emotional brain, and we will probably fight, flight, freeze, or fawn. The first thing we will probably do is swing our heads in that direction. We might start to brace our bodies and sweat. Our breathing is also going to change. All of these things are part of the autonomic nervous system, meaning that we do not have much control over them unless we have a feedback loop or an idea of how to work with our nervous systems, which are tools I will give you.
As we turn our heads, bracing, sweating, and breathing fast, we notice, "Oh, it's just a squirrel." Hopefully, what would happen is that we go back into a regulated state. However, people who have consistently dysregulated states or have had something that causes a shock to their system, like a car accident, might be dysregulated for a full day. We may see that a lot in our clients.
Let's now get into these states.
- Sympathetic:
- High level of threat: preparing the body for action
- Fight-irritability, frustration, anger, rage, aggression, defending, actually fighting
- Flight-wariness, nervousness, avoiding, anxiety, panic, ignoring, running away, muscle tension
- Fawn-appeasing, placating, codependency, people pleasing
- High level of threat: preparing the body for action
- Sensations when you are in fight or flight
- Heart rate increase
- Tunnel vision
- Increase of sweat
- Shallow or fast breathing
- Temperature changes
- Muscle tension
- Dry mouth
- Loss of appetite
- Bladder urgency
- Temporary hearing loss
- Shaking
- Increase in headache or pain
- Dizziness/spinning
- Flushed face
Our sympathetic states activate with a high threat level as we prepare the body for action. As I said, we have options from the one that is going to hurt us the least to the one that is potentially going to hurt us the most. Let's say there was a lion in front of me. The first best option is to fawn. This means that I am appeasing and placating it. I am throwing a piece of meat in the other direction or using a tone in my voice that will convince this lion not to hurt me. The second choice is to run away, which is dangerous as I could be chased. The last option is that I could fight. We will talk about freeze later.
Somebody can have a traumatic event or several cases of small traumas or stressors throughout their life. If somebody is in chronic pain, that in itself is traumatic. We know as occupational therapists when somebody has chronic pain, it takes away most of their meaningful occupations and maybe even causes role changes.
In addition, the limbic system gets activated, and that part of the brain is pinged all day long. The amygdala is constantly activated by that pain and nociceptors sending information saying, "Hey, here's some heat, pressure, or chemical changes." The amygdala wants to be left alone. Over time, the person might gravitate towards more fight reactions where they are irritable, frustrated, angry, raging, or picking fights with people. They can be defensive as they feel more wary, nervous, avoiding, and anxious. They may have increased muscle tension. Or they might be appeasing and placating, with a lot of codependency in their relationships. They want to please people. These are all examples of our bodies trying to survive.
Unfortunately, chronic pain becomes a feedback loop where the pain pings the amygdala to be more active, the amygdala makes the pain worse, and then this becomes a cycle. I had most of these symptoms before coming to this presentation today. We can see signs like dry mouth, bladder urgency, and shakiness. I am a musician, and the first time I went on stage, I shook so hard that my whole leg bounced.
Another critical point is that our amygdala does not know the difference between a stressful email and a lion in front of us. It will activate the sympathetic nervous system, but maybe not to the same degree, and cause all these symptoms.
While looking at this list, I want you to think about which might be in your nervous system pattern. Are you a person who is in a fight, flight, or fawn pattern? I take clients through this, and I let them tell me about which symptoms they are having and how they know they are in one of these states. When we are more familiar with our state, we can start to take control of it.
The first step in nervous system regulation is knowing what is going on in your nervous system, which will also help a lot with pain.
Parasympathetic-Dorsal/Freeze
- Parasympathetic-Dorsal
- High level of threat: Preparing the body for energy conservation
- Freeze: Defeat, learned helplessness, shame, shutdown, depression, immobilization, depersonalization, numbness
- Freeze
- Held or restricted breathing
- A sensation of heaviness/fatigue
- Difficulty moving
- Speaking slower
- Feeling cold or numb
- Stiffness
- Decreased heart rate
- Muscle tension
- Stomach upset
- Blurred vision/unfocused
This causes us to freeze. As I said, we have the dorsal vagus nerve that runs from the stomach to the pelvis. This is activated when there is a high threat level, and we are preparing the body for energy conservation. Over time, if somebody is experiencing this a lot and not just at the moment, this can look like defeat, learned helplessness, shame, shutdown, depression, immobilization, and depersonalization, which is where you are looking at your life like it is on a film. There can also be a sense of numbness.
If we think our client is in freeze mode, we can explain this process gently to our clients. We may be able to help motivate them to do some of their occupations. They may be stuck in a depressed, anti-motivational state and have difficulty engaging in an occupation. Acknowledging the freeze response and using some nervous system regulation tools can help them to be motivated to participate in an occupation more.
As this is part of the autonomic nervous system, there are going to be all of these nervous system things that are happening, like a decreased heart rate, muscle tension, stomach upset, nausea, blurred vision, et cetera. All of these states are going to cause more pain. You may notice somebody zoning out or feeling heavy and tired. It is good to take note of this to help your clients regulate to get more out of your sessions.
You can check in to see where the client is and assess if you can get them into a parasympathetic ventral vagus state. They will get much more out of the session when they are in this state. They are going to be focused and attentive when there is no threat.
Sympathetic and parasympathetic vagus dorsal systems are activated when there is a high threat level. And when a person has chronic pain, there can be a heightened threat all the time, and not always on a conscious level. A high threat can be from trauma or a lot of things, but the bodily subconscious assumption is they are not safe.
We want to do is help our clients feel safe. Ways to do that are by building a rapport with them and teaching them techniques.
Parasympathetic-Ventral-Rest/Digest
- Parasympathetic-Ventral
- No threat: Preparing the body to rest and connect
- Rest and Digest: Calm, restoration, eating, digestion, meditation, relaxation
- Social engagement: Connection, play, focused work, creativity, safety
- Ventral Vagal (Rest/digest)
- Warm, soothing vocal tone
- Sighs and easy breaths
- Expanded vision (aware of the periphery)
- Relaxed muscles
- Smiling
- Open and confident posture
- Easy eye contact
- Gentle movements
When there is no threat, we are in a ventral vagus state. Again, this is a helpful theory for thinking about these different states. This state is also called rest and digest or social engagement. We feel calm, are eating and digesting correctly, can meditate, and are relaxed.
I want to comment on eating and digestion. For many of our clients with irritable bowel syndrome or other things going on with their stomach, part of that can be from this nervous system dysregulation. Remember, our bodies do not care about digesting food if we are in survival mode. We are concerned about getting away or fighting the lion. Our body shunts blood to our extremities to fight or flee. In contrast, when we are regulated and feel safe, we can digest properly. Thus, many of our clients with chronic conditions have tummy issues.
We are helping clients to socially engage. Is also a big part of occupational therapy. Dysregulation can be a roadblock to being engaged and focused on work. This can be an essential thing when considering return-to-work strategies and creativity. If they are more creative types, regulation will also help with that creativity.
One sign that can tell us that either our clients or we are regulated is using a warm, soothing vocal tone. A faster or louder voice may signal sympathetic activation. It is normal to be a little bit nervous when you are presenting (like I am), and that shows up in your voice. Talking to your client in a soothing, warm tone will signal their nervous system that they are safe.
Sighs and easy breaths are other signs of a rest and digest state. I want everyone to sigh right now to see how good that feels. This is an excellent quick and easy way to regulate the nervous system. It is a sign that your nervous system is excellent and regulated.
If there is a lion in front of me, I would be focused on that lion, and my vision would be tunnel vision and nothing else. If I am aware of my periphery, this is a signal that I am safe.
Other positive signs include relaxed muscles, smiling, and an open and confident posture. Additionally, subconscious postures can contribute to chronic pain when trying to protect our internal organs. For example, we may be tense if we are in a fight state or caved in with forward and elevated shoulders in a freeze state. We are subconsciously protecting the base of our brain and internal organs, which are essential for survival. Much tension in the traps comes from that unconscious protection of our brainstem to keep that area nice and tight for protection. If our posture is open, our shoulders are down, and we are smiling, making easy eye contact, using gentle movements, et cetera. We are showing that we are regulated.
The goal is not to stay in a ventral vagal state all the time, as noted in the infographics in Figure 3.
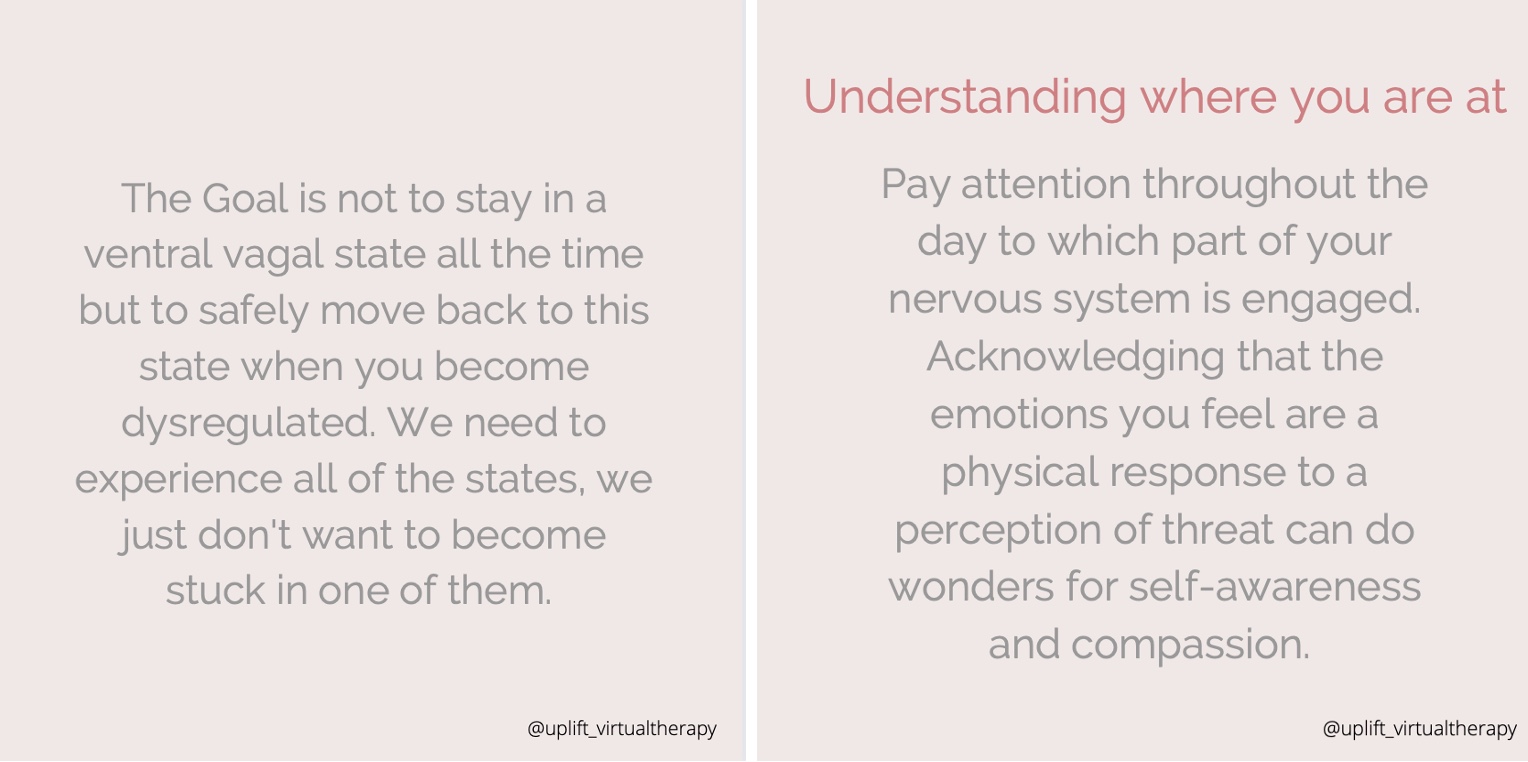
Figure 3. Infographic from the author's social media platform.
The goal is to safely move back to the state when you become dysregulated because we need these states to survive. That is why they are called survival responses. If we are walking in the woods, like in the earlier example, and we realize it is a squirrel, we should be able to move from the fight, flight, freeze, or fawn states back to a regulated state.
If we are dysregulated all day, our nervous system is not regulated. Sometimes we even see people with dysautonomia, with so much dysregulation in their nervous system that their heart rates and other autonomic symptoms are all over the place. With chronic pain, we know that some level of that is happening.
We need to experience all the states, but we do not want to be stuck in them. I usually tell my clients to pay attention throughout the day to which part of their nervous system is engaged. Even while taking this course, you might want to check in with yourself. We just reviewed the emotions and physical sensations representing different nervous system states. By looking at those two things, think about what state you might be in. You may have had an excellent or stressful day. You may have gotten a massage an hour ago and feel great. I wish that for all of you.
Another important thing is to acknowledge that the emotions/sensations you feel are a physical response to a perceived threat. This does not mean we are anxious or bad. Many clients carry horrible shame about not being able to do the things that they once loved to do or acting out stress on others. It makes sense you would feel activated because of what has happened to you and your nervous system. There has been global mass trauma for many people these past couple of years.
While there are various reasons why people may be activated, it is never somebody's fault, per se. It is their nervous system doing its job. I often liken it to a dog that has been abused. If you adopt this dog, you cannot yell at it and expect it to change. We cannot say, "You're a bad dog." Instead, we have to say, "Yeah, it makes sense that you are acting like this because of what happened to you. I will treat you with compassion and love and work through this." I highly stress to my clients that when we are doing this work, I want them to take the shame and judgment out of it and bring that self-compassion and self-awareness.
Strategies
- Regulating the Nervous System
- Creating a sense of calm
- Soften muscles around eyes: Look around the room and acknowledge you are safe, open up peripheral vision, and cup warm hands over eyes
- Yawn, belly breathing, or “horse breath”: A quick way to stimulate the ventral vagus nerve and instantly calm down
- "Vuu-ing”: Inhaling and then exhaling the sound "vuuu"
- Co-regulation: Regulating with another human, pet, or nature
- Creating a sense of calm
Now, we get to get into the juicy bits about how to regulate the nervous system. I have listened to thousands of podcasts and done a ton of research, including reading white papers, to compile the best research I had for regulating our nervous system.
Much of this has to do with stimulating the ventral vagus nerve. I do not want you to get the wrong idea about this because we are not always stimulating it but activating it to make that part of our body more engaged.
As you can see, there are different ways to regulate the nervous system. First, we can soften our eyes to decrease tunnel vision. We want to consciously become aware of our periphery to trick our nervous system into thinking that we are safe because we are. Right now, I am looking straight at the computer, but in my periphery, I can see my water glass, plants, and the wall. As we go through these ideas, you can do these exercises with me and notice how they feel. Another thing that we can do is look to the left as far as we can and hold it, then look to the other side. You might notice some regulation things start to happen. You might yawn or sigh, as those are signs that your nervous system is starting to regulate.
Another thing that I love and do every day is rub my hands together. You can try this with me if you want. You rub your hands together and make them nice and warm, and then you hold them over your eyes. You can even massage around the eyes and feel the nervous system start to regulate as you do that. Being in the dark and having your eyes closed indicates that you are safe. Our eyes should not be tightly closed, as that might mean something is coming at us. If our eyes are softly closed, we feel safe enough not to have to look in all directions. Some clients might be challenged with this if they have had severe trauma. They may not feel safe enough to close their eyes, so you can work with the other eye exercises.
Some breathing exercises include stimulating a yawn. I guarantee some of you just yawned after I said that. You can stimulate a yawn just by saying the word, or you can open your mouth like you are going to yawn. Yawns cool down our brain as sometimes our brain is slightly warmer with sympathetic activation. Cooling down the brain can actually help to regulate it.
Most of you probably know about belly breathing. You put your hand on your belly, take a nice deep breath into the belly, and exhale longer than the inhale. If we tell our clients to take deep breaths, sometimes that can make them more anxious as breathing in can activate the sympathetic system. In fact, if you want a lot of energy or need to wake up, you can do quick inhales. However, if you want to cue that ventral vagus system, you want to inhale and exhale slowly. I usually say to inhale for a count of four and exhale for a count of eight. We also want them to put a hand on their belly so they can feel it moving. For kids, I have them imagine that their belly is a balloon, and they are blowing it up. We then take a little pin and pop it. If you have a client that says they do not have the time to do this, they may be willing to do it with their kids. It is beneficial for the client and their kids.
Vuu-ing is a technique from Stephen Porges, who created the polyvagal theory. You inhale, exhale the sound, "Vuu," and hold that note for a while. I am not going to do that fully here.
Another thing is co-regulation. While it is very important for a client to learn how to regulate their nervous system, it is super important for a client to also regulate with other people. They can regulate with you because, as the awesome clinicians you guys are, I am sure you are providing a sense of rapport, a soothing vocal tone, soft eye contact, and an open body posture. The best way to help somebody else's nervous system to regulate is to be regulated yourself. Between sessions, you can use some of these techniques to regulate yourself. If you go into a session and are dysregulated or discombobulated, it is a cue to the nervous system that something is going on. Encouraging clients to be social in different ways is also important, even if they have chronic pain. As occupational therapists, we are good at finding ways to help people do things and be socially engaged. I introduce ideas to my clients, and I have them pick a few.
- Stimulating the Ventral Vagus Nerve
- The ventral vagus nerve helps us feel calm, connected, and content. It is the opposite of flight/fight/freeze mode.
- Physiological sigh: Take 2 quick inhales and sigh out a long exhale
- Diving reflex: Dunk head in a bowl of cold water, run ice over forehead, or take a cold shower, holding breath for 5-8 seconds
- Pressure and touch: Self hug or massage, massage ears, hand on chest, cuddling a pet or person, weighted blanket
- Creativity and expression: Sing, dance, paint, listen to music, laugh out loud
- The ventral vagus nerve helps us feel calm, connected, and content. It is the opposite of flight/fight/freeze mode.
We also have the physiological side. I am not sure if you are familiar with Dr. Huberman, a neuroscientist and ophthalmologist out of Stanford. He has so many amazing hacks, and I recommend listening to his podcast. He describes a lot of research that is helpful for regulating the nervous system.
The first is you take two quick inhales, and you sigh out a long exhale like you are fogging up a mirror. You can do that a couple of times to feel better. Again with pain, we want to release that tension and decrease amygdala activation. We are also doubly inflating the alveoli and offloading CO2. These things are going to help the client to regulate and feel better.
Clients either love or hate the diving reflex. I have started doing this every morning, and it is better than a cup of coffee. You dunk your head in a bowl of cold water and hold your breath for a few seconds. Every mammal has a thing called the diving reflex, which our body automatically helps us to feel alert, awake, and activated. We can also take a cold shower to stimulate our stress response in a controlled environment. You are creating a pathway in your brain from stressed to not stressed.
For pressure and touch, you can wrap your arms around and give yourself a nice hug. That pressure on the chest puts pressure on that ventral vagus nerve. We can also use self-massage and massage the ears, especially as the ventral vagus nerve comes closest to the body's surface inside the ear. I feel like yawning as soon as I do it because my body starts to regulate. Putting that pressure into the ear can be a good way to self-regulate. There are diagrams of where to massage ears that you can look up.
You can also buy ventral vagus nerve stimulators that put electricity into the nerve to stimulate it.
Weighted blankets are awesome, and cuddling is great if available to the person.
Lastly, we can look at creative activities and singing. If there was a lion in front of you, you would not stop to sing a show tune or paint a picture. These activities are good cues that the nervous system feels safe and it is ok to relieve the tension. Or, "I do not need this much pain because I do not need protection right now."
- Stimulating the Ventral Vagus Nerve
- Gargling for 10-20 seconds a few times a day
- The Valsalva Maneuver
- Engaging in play
- Shaking the whole body
- Opening posture
Here are a few more suggestions. You can gargle for 10 to 20 seconds a few times a day. This is an easy one to do, as you can do it right before you brush your teeth. By gargling, we stimulate where the ventral vagus nerve comes down at the back of the throat.
The Valsalva maneuver is where you plug your nose and breathe out with your mouth closed like you will pop your ears, but you do not fully pop them. It puts pressure on the nasal cavity, abdomen, and heart. This procedure is not recommended for people with heart issues. Some emergency response teams use this to reset someone's heart if they have heart issues or arrhythmias. It is pretty effective on the heart, but we want to make sure someone does not have heart issues before they do this. I am not going to do it right now as I have low blood pressure, and as this lowers my blood pressure even more, it makes me feel a little dizzy. This maneuver can help if somebody is panicking. For example, if someone is panicking due to pain, this may help them to settle down so they can move in a more fluid way.
Engaging in play is another way to stimulate the ventral vagus nerve. You can do this with kids or pets. Board games can also be helpful because you engage parts of the brain that are important for regulation. Laughter yoga is great too. I lead laughter yoga classes, and I can give you more information about that at the end if anyone is interested.
You may notice that if you get anxious, you can give your body a quick shake, making you feel more prepared to do an activity. We are moving that energy through our body and opening our posture, as we discussed.
Sensory Modulation: Regulate Yourself With Your Senses
- Energize
- Smell citrus
- Taste peppermint
- See bright patterns
- Hear an energizing song
- Feel a splash of cold water
- Move quickly, spin, or balance
- Calm
- Smell lavender
- Taste chamomile
- See a cool color
- Hear nature sounds
- Feel a weighted blanket
- Move or rock slowly
Sensory modulation is also super beneficial. By giving you these ideas, I am hoping you can build your toolkit and decide which ones will be best for you and your clients. Sensory modulation is something we already do as occupational therapists, often for kiddos with autism or ADHD. There is also similar activation in the amygdala in the ADHD brain, which works well for nervous system regulation. We are doing this to regulate and energize our senses. Ideas include using citrus, peppermint, bright patterns, energizing songs, cold water, et cetera.
I have a little vial of lavender next to my computer for when I am having particularly difficult sessions with my clients. I do most of my work virtually. I can open it up without them even seeing it. I instantly feel calmer. You can create a list with your clients of the things that energize or calm them, and these are going to be different for each person.
Identifying Triggers and Glimmers
- A glimmer is the opposite of a trigger, they are the things that cue our nervous system to feel safe
- Make a list of triggers and glimmers with your clients, the more glimmers and sense of safety, the less pain
- Think like an OT! What meaningful activities help them feel safe? How can they do those activities even with their limitations?
Another thing that I do with clients is to identify their triggers and glimmers. A trigger is something that forces us into a dysregulated state of fight, flight, freeze, or fawn. It also makes the pain worse. A glimmer is a thing that is going to trigger our nervous system into a sense of safety, so a cue that helps us to feel safe. The more glimmers somebody participates in, the more sense of safety and the less pain.
As an OT, what meaningful activities help them feel safe? There is a wonderful woman named Deb Dana, and she has a book on polyvagal theory. She has worksheets on triggers and glimmers. We need to help the client find glimmers and meaningful activities. We may need to break down activities, so they can do them, even with their limitations.
A glimmer of mine is dogs. If I see a dog, I instantly feel happy and calm. I love the smell of lavender, as I stated earlier. I love hot cocoa, the sensation of a weighted blanket, dancing, and being around certain people I love.
Homework I Give Clients
- A few times over the next week, notice when you are triggered. Write down:
- What triggered you?
- What state were you in? How do you know? How intense (0-100)
- Which strategy/strategies did you use?
- How did you feel after? (0-100)
I give clients homework. I first ask them what state they are in. Secondly, I have them identify a few times over the next week when they are triggered and how they knew. "I was in fight mode because I was angry. My muscles were tense, and I was grinding my teeth." This is perfect because they are talking about their emotions and physical state. I can then ask, "How intense was it?" They may answer, "It was a 70 out of 100." We can then ask if they used any strategies and if they worked. We can then ask if the intensity of their feelings diminished.
Other Options
- Vagal stimulators
- Meditation/hypnosis
- Curable app
- Greg Lehman’s free pain book
I talked about the vagal stimulator that goes onto the ear. I think there are ones that you can get implanted into your brain for more serious dysautonomia. I have not looked into that too much because that is not my scope of practice, but I think it is on the market.
Meditation and hypnosis are awesome. The Curable app is a good app for pain and has a workbook. Greg Lehman's free pain book is another resource.
You might have noticed on a few slides that it says Uplift Virtual Therapy. This is my business, and I can be found on TikTok and Instagram. My site has a whole bunch of the strategies that we just went over, and it has me demonstrating all the strategies.
How Does This Connect to OT?
- Large portion of clients with mental health and chronic pain concerns can benefit from these strategies.
- The role of engaging in meaningful activity to help the nervous system feel safe cannot be underestimated.
- If a client is regulated, they may participate in sessions more.
- Understanding these responses helps us to understand our clients holistically.
- Sensory modulation, pacing, and finding activities which help a person regulate are what we are amazing at!
Occupational therapy has many clients with mental health and chronic pain concerns. Pretty much anyone can benefit from these strategies, but definitely people with these concerns. Engaging in meaningful activity to help the nervous system feel safe cannot be underestimated. We, as occupational therapists, have this unique role where we get to peer into someone's values, interests, and passions. If there is anything in this world that helps us to feel safe, it is engaging in the things that we love. Engaging in our passions and being in the moment of flow is powerful.
Give yourself a little pat right now for being part of such an awesome profession. If a client is regulated, they will participate more in sessions. We talked about that already. Understanding these responses can help us understand our clients more holistically. We may say, "Oh, now I totally recognize that the client is in flight. Maybe we should do some exercises before we continue with the session." Or, "This subject brings up that for my client, so let's talk about that more and find some ways to regulate around it." The cool thing is, unlike a psychotherapist or a counselor, we do not have to dive into the past and talk about their childhood or what happened to them to help them regulate. Instead, we can deal with how those things manifest in what is happening now. Our scope is to do things now, give people strategies, and educate them. We use sensory modulation, pacing, and finding activities that help a person regulate.
Questions and Answers
Do your clients ever describe having tooth pain? For example, I can feel my pain all the way from the base of my spine right up to my two front teeth, increased jaw tension, teeth clenching to the point of cracking a tooth, and dental damage.
This is a good question. When there is tooth pain, I always refer to a dentist, and I am sure you already have. The thing with those nerves is that if they are being stimulated, there can be a component of sensitization. Nerves in the mouth can be some of the most sensitive nerves in our body.
If someone is clenching their jaw a lot, that means that there is amygdala activation. Clenching is a fight-or-flight response; for many, this shows up in their jaw. Other areas can be in the traps or hips. There are areas in our body where we tend to store that tension more. Using some of the mentioned techniques can help relieve some of that clenching. A dentist should help to ensure that nothing is going on with the nerve.
Do any of your clients present with changes to their blood pressure? For example, their BP goes higher when pain spikes.
Yes, this happens all the time. I have many clients in my practice, especially those with dysautonomia, demonstrating this. They may also have a resting heart rate of anywhere from 110 to 120, which is high and a good indication that their sympathetic nervous system is activated.
I have never heard of the phrase cooling down your brain before. Is this merely a descriptive term, or are there studies that show actual temperature rise?
I have some pain management patients who take their temperature during pain exacerbation, and they typically report temp elevation up to 100 degrees Fahrenheit. The brain and the body with temperature regulation are going to be a little bit different. When I was talking about cooling your brain, I meant that when we yawn, it is cooling our brain down, according to some studies. It is a slight amount, but it is enough to cool the brain.
If we notice temperature increases when people are in pain or talking about pain, this is a sign of sympathetic activation. Again, if I was in front of a lion, I would probably be sweating profusely due to vast temperature changes. Sometimes we get cold or hot, which is a sign of dysregulation.
What is horse breath?
It is taking a deep inhale and then exhaling with a fluttering of the lips like a horse. Kids love this. It vibrated the ventral vagus nerve to help us to calm down. Many people do this unconsciously when they are stressed.
What podcasts do you recommend?
I recommend the Huberman Lab. That is the scientist that I was talking about earlier. There are some other podcasts on chronic pain if you search.
What yoga did you mention?
It was laughter yoga. Laughter yoga is a set of exercises where people laugh for no reason. I have done this in hospitals, retirement homes, and with groups of people with disabilities or chronic pain. I have even hosted laughter yoga sessions on Eventbrite. There are also a ton of videos on YouTube for laughter yoga if you wanted to introduce your clients to them.
What was the worksheet you mentioned?
Deb Dana has a worksheet called Triggers and Glimmers. We identify our client's triggers and then identify their glimmers so that they can avoid their triggers or anticipate their triggers. The goal is to add more glimmers to their lives.
I feel the acupressure seeds in the ear work great to calm people.
Yes, any pressure in that part of the ear stimulates the ventral vagus nerve, which is very close to the skin.
How do you explain the neurological basis of this theory to clients in an easy-to-understand manner?
I usually talk about the autonomic nervous system and how there are automatic responses that happen. I also like to use the lion example. We can then run through the four options of fawn, flight, fight, and freeze, going from least dangerous to most dangerous. On any given day, a person may go all the way from fawning to freezing. I allow them to ask a lot of questions.
There are also a lot of videos on YouTube about polyvagal theory. Stephen Porges does an excellent job of explaining it because he is the one who invented it.
When you talked about clients with IBS, were you referring to their digestion as not working?
Less blood flow to the digestive organs in fight, flight, or freeze equals slower digestion and stomach upset. You have probably noticed that you feel like you are going to throw up or feel nauseated when anxious. Many of these symptoms have a biological basis, but some of the symptoms can be relieved by nervous system regulation.
What are some of the ways you have implemented essential oils into your treatment sessions? Any recommendations for therapeutic activities with essential oils?
I usually have the client create a list of senses that are energizing and those that are calming. Then I have them choose from this sensory kit (either mine or something they create) to use when they are dysregulated. Examples are weighted blankets, essential oils, et cetera.
How I am doing OT in telehealth?
I see clients for concussions, chronic pain, and mental health trauma disorders. I do a lot of treatment online because many clients have difficulty leaving their houses. Sometimes we set up the camera, and they do their ADLs in front of me on camera. Much of my treatment is education, coaching, and return-to-work strategies. This seems to work well online, and my clients have responded well.
What techniques would you recommend for a student that has catatonia and autism?
Any techniques you can get the client to do. You want to choose activities that are interesting to the client. I may say, "Which one of these do you think you would actually do?" For example, one may say, "I would never get into a cold shower," while others may say, "That sounds cool." You can take the sensory lists with you to see what works for each client. For individual clients, you are going to have to use your creative, awesome OT brain and figure out what will work for them and their limitations.
Would these techniques also work with a client with a panic disorder?
Absolutely. You want to find things that are not going to be triggering for them. Sometimes breathing techniques are triggering for people with panic disorders, but there are a whole bunch of other techniques you can rely on.
Do you typically document the practice of these strategies during treatment for reimbursement?
I always document whatever we did in the session. I do not work in the States, so I think the reimbursement rules are different in the States.
References
Dana, D. (2018). The Polyvagal theory in therapy: Engaging the rhythm of regulation (Norton series on interpersonal neurobiology). WW Norton & Company.
Kempke, S., Luyten, P., Van Wambeke, P., Coppens, E., & Morlion, B. (2014). Self‐critical perfectionism predicts outcome in multidisciplinary treatment for chronic pain. Pain Practice, 14(4), 309-314.
Lagueux, É., Dépelteau, A., & Masse, J. (2018). Occupational therapy's unique contribution to chronic pain management: A scoping review. Pain research & management, 5378451. https://doi.org/10.1155/2018/5378451
Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. (2020). Am J Occup Ther, 74(Supplement_2):7412410010. https://doi.org/10.5014/ajot.2020.74S2001
Porges, S. W. (2018). Polyvagal theory: A primer. Clinical applications of the polyvagal theory: The emergence of polyvagal-informed therapies, 50, 69.
Treede, R. D., Rief, W., Barke, A., Aziz, Q., Bennett, M. I., Benoliel, R., ... & Wang, S. J. (2015). A classification of chronic pain for ICD-11. Pain, 156(6), 1003.
Citation
Dureno, Z. (2023). Polyvagal theory and chronic pain: Exploring treatment options. OccupationalTherapy.com, Article 5575. Available at www.occupationaltherapy.com
