Editor's note: This text-based course is a transcript of the webinar, Postpartum Path To Well-Being And Longevity: Postnatal Pelvic Health Virtual Conference, presented by Laura Rowan, OT/L.
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
- After this course, participants will be able to identify three important areas of care that can help with recovery after childbirth to support daily activities.
- After this course, participants will be able to identify two hormonal connections between the pre and postnatal period and the transitions into perimenopause and menopause.
- After this course, participants will be able to recognize how techniques for calming the nervous system can help break the cycle of intergenerational trauma and how this relates to self-healing and parenting.
Introduction
It is truly an honor to wrap up this Postnatal Pelvic Health Virtual Conference, thoughtfully organized by occupationaltherapy.com. This week has been filled with brilliant insights from pelvic health therapists who shared invaluable pearls of wisdom, helping us better support this much-deserving population. I chose today’s topic to build on these golden nuggets of knowledge, connecting them to a pathway that moves from the perinatal period toward future health and wellness.
In this presentation, we’ll explore hormonal rhythms as predictors of health and wellness, address common roadblocks to recovery, and outline protocols to overcome these challenges. We’ll establish a broader appreciation for pregnancy and postpartum as a window of opportunity that allows individuals to take agency over their future health outcomes. Doing so can break intergenerational cycles of dysregulation, ease challenging menopause transitions, and mitigate the risk of other illnesses.
It’s important to recognize that not all birthing persons identify as women or moms. For this presentation, I will use these terms interchangeably, with deep respect for all gender identities and preferences. Let’s embrace this opportunity to expand our understanding and create meaningful change for the individuals and communities we serve.
Invitation for Self-Awareness
I like to view pregnancy and postpartum as an invitation for self-awareness. For many of our clients, this is the first time they are truly learning about their bodies, and it permits women to educate themselves in ways they may not have before. Typically, we don’t give much thought to automatic functions like peeing and pooping—they just happen until they don’t. It’s often at that point that we are forced to tune in. Pregnancy and postpartum provide an opportunity to reconnect with the body and rebuild from a more informed and intentional foundation.
Because of this, I believe we can strive for better than before. Personally, as a female athlete in my late 40s, I feel stronger now—both physically and mentally—than I did in my 20s and 30s, even after having two pregnancies and two vaginal deliveries. With the knowledge and tools I’ve gained, I’ve rebuilt in ways I never imagined possible. This is the message I want to share: it is possible.
For our clients, areas where we can help bring awareness include hormone rhythms, breath, core and pelvic floor function, posture and alignment, lifestyle and habits, nutrition, and mood. These concepts, discussed throughout this week, are foundational and relevant across all practice settings. Importantly, we don’t need to be pelvic health specialists to integrate these insights into our work. Pelvic health transcends all ADLs, practice settings, and populations, and we have a role to play in helping our clients—and society—view pregnancy and postpartum as a window of opportunity rather than a negative problem area.
By embracing the wisdom and insights offered through hormonal rhythms and life transitions, we can empower our clients to make informed lifestyle choices. These choices can enhance vitality, quality of life, and long-term well-being, creating a path toward stronger, healthier futures.
Hormonal System Overlap
Hormonal symptom overlap exists across the menstrual, maternal, and menopausal transitions, with many symptoms appearing in these phases. These include nausea and vomiting, mood changes, anxiety and depression, cognitive changes like brain fog and short-term memory issues, executive functioning difficulties, hot flashes, night sweats (vasomotor symptoms), sleep disturbances, fatigue, breast tenderness, menstrual cycle changes, headaches, hair loss, weight changes, low libido, urinary incontinence, gastrointestinal symptoms, vaginal dryness, and other genitourinary symptoms.
By recognizing these potential symptoms and their overlap, we can foster earlier awareness in our clients, leading to earlier detection and intervention. This proactive approach empowers individuals to take agency over their future health rather than succumbing to illness and disease.
However, these symptoms are often easy to dismiss as part of typical day-to-day overwhelm, making early warning signs easy to miss. Encouraging clients to tune into their bodies and recognize when symptoms persist or escalate allows us to support them in addressing underlying issues and optimizing their health for the long term. Building this awareness and addressing concerns early can transform these life transitions into enhanced health and well-being opportunities.
Hormonal Wisdom
Hormonal wisdom provides us with a wealth of early warning signs and red flags—if we know how to interpret them. This wisdom allows us to take a proactive rather than reactive approach to health management.
For instance, the menstrual cycle is an essential vital sign. It provides critical insight into our health markers monthly, weekly, and even year-over-year. Understanding patterns and changes in the menstrual cycle can give us valuable clues about overall health and help detect potential concerns early.
Similarly, pregnancy acts as a natural stress test for the body. Changes in cardiovascular health, blood sugar levels, mood, and cognition during pregnancy and postpartum provide vital insight into health markers. These changes can serve as potential predictors for future conditions, including hypertension, stroke, diabetes, dementia, depression, and even suicide.
It’s important to educate our clients that their health journey doesn’t end when the baby is born. This is the beginning—a critical window to make lifestyle changes that can positively influence their future health outcomes. Prevention, rather than intervention, is the key. And that’s a message worth repeating: this is a time for prevention, not just intervention. By embracing hormonal wisdom, we can help our clients view this period as an opportunity to build a foundation for long-term health and well-being.
Cardiovascular
There are critical implications for cardiovascular health during the perinatal period. Hypertension during pregnancy is a significant "check engine light" that shouldn’t be ignored, as it can lead to increased vasomotor symptoms—hot flashes and night sweats—later in menopause. Both hypertension and these symptoms are indicators of underlying vascular dysfunction, which is a leading cause of mortality in women. Addressing this isn’t just about improving quality of life but saving lives.
We can take clear action steps to mitigate these risks. First, identify those at higher risk, particularly individuals who experienced hypertension during pregnancy. Implement risk prediction and reduction strategies, starting with routine blood pressure monitoring. Blood pressure should be checked at every prenatal and postnatal visit—it’s a simple yet powerful step.
Beyond that, we can empower clients to self-monitor their blood pressure at home. Setting them up with a blood pressure cuff and teaching them how to use it effectively fosters health literacy. It’s not just about tracking health markers but understanding what those markers mean and how to respond to them. Education is key to empowering clients to take ownership of their health.
This is personal for me. I experienced hypertension at the end of both of my pregnancies and was induced early as a result. While my blood pressure normalized after delivery, I’ve since made significant lifestyle changes to prioritize my heart health. With a family history of heart disease—my father died of a heart attack at age 65—I’m committed to breaking that genetic predisposition. Pregnancy was my stress test, and I’m heeding the wisdom it shared. This knowledge isn’t just about me; it’s about equipping clients with the tools to listen to their bodies, make informed choices, and take charge of their health for the long term.
Gestational Diabetes
The statistics are clear: individuals who had gestational diabetes during pregnancy are 10 times more likely to develop diabetes or prediabetes later in life. Because of this heightened risk, it’s recommended that they be screened for diabetes 4 to 12 weeks postpartum and every three years thereafter. However, current practices reveal a gap—while significant progress has been made in screening during pregnancy, there’s limited follow-up postpartum.
This is an area where we, as practitioners, can make a difference. Educating our clients about the importance of ongoing screening is key. Encourage them to advocate for themselves by requesting follow-up screenings if their healthcare provider hasn’t already offered them.
The message remains consistent: health management doesn’t end once the baby is delivered. Postpartum is not a closing chapter—it’s the beginning of an opportunity to bolster future wellness. We can help clients navigate this critical window for long-term health and prevention by empowering them with knowledge and encouraging proactive measures.
Longevity
When we talk about longevity, we’re not just discussing living longer—we’re emphasizing living better. This means prioritizing quality of life, positive health markers, and overall well-being. Dr. Peter Attia’s book "Outlive" introduces the concept of Medicine 3.0, which shifts the focus from treatment to prevention. This proactive approach addresses health risks before they become problems, fundamentally altering how we view and manage long-term health.
Attia also discusses the “it’s too late” theory, highlighting that once markers like high blood pressure or insulin resistance appear, the window of opportunity for easy intervention has often passed. At that stage, reversing the cumulative effects of these markers becomes far more challenging. This underscores the importance of prevention and early action.
Hormonal awareness plays a key role in this preventive approach, providing insights throughout the different phases of hormonal transitions. By understanding and responding to the patterns and shifts in our hormonal seasons, we can act more efficiently to optimize health and well-being. This awareness empowers individuals to take charge of their health early, enhancing longevity and quality of life throughout those years.
What Brings Us In?
Let’s talk about what motivates individuals to seek pelvic rehab. We’ve made significant progress in raising awareness about pelvic health, and as a result, more moms are seeking support. Some common drivers or motivators include worry and fear about long-term effects. Clients might share concerns like, “My mom was never the same,” or “My grandmother’s uterus was falling out.” These generational narratives often create anxiety about their own outcomes.
Word of mouth is another powerful motivator. Clients may have heard about pelvic rehab from a friend, someone at yoga, or even a casual conversation. For all its flaws, social media has also played a big role in spreading awareness. Platforms like Instagram and Facebook have become spaces where people learn about pelvic health and recognize its importance. Sometimes, clients arrive saying, “I don’t know why I’m here, but my doctor or therapist told me to make an appointment.” Regardless of how they come to us, the opportunity to provide education, guide their healing journey, and support their recovery is invaluable.
Whatever brings them through the door, it’s our role to create a space where they can begin to understand their pelvic health, build awareness, and transition toward healing and recovery with confidence and knowledge. This initial step is pivotal, and the right support can set the stage for long-term wellness.
Common Areas of Intervention
These broad areas of intervention provide a general overview of the physical symptoms that often bring clients into pelvic rehab. What’s important to highlight here is how these physical symptoms are significant life disruptors. They are the issues that women notice most—the ones that interfere with their ability to engage in meaningful occupations and purposeful activities.
These symptoms often motivate action because they directly impact daily life, whether it’s their ability to work, care for their families, exercise, or enjoy leisure activities. By recognizing the profound effect these physical challenges have on their overall participation, we can approach intervention in a way that addresses the symptoms and empowers women to reclaim their roles and routines. This connection between physical health and functional participation is at the core of pelvic health intervention's impact.
Common Therapeutic Modalities
Kirsten Spurrier highlighted key interventions in her talk about the driver of function (Day 2 of this virtual conference), emphasizing some of the most empowering foundational concepts for recovery. She spoke about the profound outcomes of focusing on the basics, such as posture and breathing, and reminded us not to underestimate their transformative healing power.
One of the most striking points Kirsten made was the importance of not assuming clients already know this information. Time and again, I hear clients express amazement at learning to breathe effectively for the first time, regardless of age. They are often surprised by the immediate impact of proper breathing and posture on their physical recovery, daily lives, and overall sense of well-being.
This foundational work is deeply tied to occupational impact. When clients learn to harness the basics, they often experience renewed confidence and capability to engage with meaningful activities and routines. It’s a reminder that even seemingly simple interventions can have a profound ripple effect on function and quality of life.
Occupational Impact
Pelvic health has a profound impact on all areas of occupation, and it’s important to highlight the role of what I like to call the intrinsic ADLs—those internal, essential activities and functions that must happen daily for us to live. These include fundamental bodily functions like elimination, digestion, and other internal regulatory processes.
These intrinsic ADLs form the foundation for our ability to engage in external ADLs, such as bathing, dressing, toileting, and everything else on the list. Without proper internal function and regulation, participating in external daily activities can become significantly more challenging. Recognizing and addressing these intrinsic needs is crucial to supporting our client's wellness and independence.
New ADLs
Parenting often brings us into a world of tasks and challenges we’ve never encountered before. Activities like breastfeeding, babywearing, diaper changing, transporting a baby while carrying out other ADLs, stroller pushing, and navigating entirely new routines and schedules are suddenly part of daily life. These shifts also come with new roles and relationships as we transition into parenthood.
The truth is that parenting doesn’t come with a guidebook, and most of us are figuring it out as we go. It reminds me of the movie "The Wild Robot," where a robot AI assistant—designed to support busy humans—finds itself in the wild, surrounded by nature and no humans. In one scene, the robot is told by a mother possum, who has her babies climbing all over her, that it needs to care for a baby gosling that has lost its family. The robot replies, “I’m not programmed to be a mother. I don’t know how to do that.” And the mom possum says something so profound: “Yeah, none of us do. We just make it up.”
This moment resonates deeply because it captures the essence of parenting. It’s not about knowing exactly what to do but about adapting, learning, and doing the best we can in the moment. For clients, recognizing this can be freeing—knowing they’re not alone in figuring it all out and that it’s okay to “just make it up” as they go. Our role as practitioners is to support them in this journey, helping them navigate these new functional tasks and roles with confidence and compassion.
Roles and Relationships
Parenting introduces a whole new role, and it’s not just about caring for the baby—it’s also about navigating the broader changes it brings to every aspect of life. One of the most significant areas of adjustment is partnership. Many new parents fear losing closeness with their partner or their relationship shifting. They may wonder if they’ll lose what they had before and how to nurture their bond amidst all the changes.
Professionally, there’s often a reevaluation of direction, priorities, and capacity. Questions like What direction do I want to go in? When and if should I return to work? become central. Balancing these decisions with new parenting responsibilities can feel overwhelming, requiring reflection on personal and family goals.
Then there’s the aspect of identity—who they are as individuals. Becoming a parent can lead to existential questions like, Who am I now? Does everything about me have to change? Is it okay to embrace a new version of myself? What does that look like? This sense of self-evolution can feel both liberating and disorienting.
Caregiving also takes on new dimensions. It’s no longer just about the baby—many parents care for others, such as aging parents, while still trying to carve out time to care for themselves. Balancing these caregiving roles while maintaining self-care often feels like an impossible juggling act.
Acknowledging these layers of change and complexity is crucial. Parenting is not just about learning new skills—it’s about embracing the emotional, relational, and identity shifts that come with this transformative time. As practitioners, we can help parents process these changes, find clarity, and prioritize their well-being while adapting to this multifaceted new chapter.
Multi-system/Mindbody Approach
Let’s look at the less traditional ADLs and therapeutic interventions. These go beyond the external ADLs and delve into the intrinsic, internal functions—what I like to call the bodily systems. These include the musculoskeletal, respiratory, urinary, gastrointestinal, sexual, reproductive, cardiovascular, and lymphatic systems. On top of this, we must consider the social-emotional aspects: the nervous system, emotional roles and relationships, hormones and rhythms, and broader influences like culture, race, and socioeconomic status. This multi-system approach allows us to address the complex interplay of these systems, moving beyond just the pelvic floor to truly understand and support our clients holistically.
I often refer to myself as a pelvic health therapist because focusing solely on the pelvic floor can feel limiting. A multi-system approach broadens the scope of care and provides numerous avenues to make progress. However, it’s important to note that this wealth of information can feel overwhelming for clinicians and clients. The key is approaching this complexity with curiosity and using it as an opportunity to empower rather than overwhelm.
One client’s experience highlights the importance of this approach. She is a postmenopausal woman in her 50s who recently shared a profound reflection while waiting for a mammogram. Sitting in the waiting room with other middle-aged women facing fears about their health, she contrasted this moment with memories of being in a waiting room filled with glowing, excited pregnant women years earlier. She expressed an intense need to feel cared for in her current phase of life. Her case demonstrates how education and a multi-system perspective can create space for healing.
Initially, this client sought care for urethral pain during voiding (with UTI-like symptoms), dyspareunia (painful intercourse), and incontinence. As a wellness coach trained in trauma-informed care, she strongly believed these issues were linked solely to trauma. When I introduced the possibility of hormonal changes influencing her symptoms, she resisted. However, as we explored further, I explained how hormonal changes can impact tissue sensations, muscle and tendon integrity, and their interplay with the nervous system, resulting in tension and pain like the protective response from trauma. This opened the door for her to consider new perspectives.
During our work, we identified more tension and discomfort in her left pelvic floor muscles and urethra, prompting her to mention a longstanding left hip issue. She admitted she’d been "hammering" that hip due to its weakness and pain. This connection allowed us to explore biomechanical contributors to her symptoms. We discussed balancing her intentions and energy—recognizing that while tension and strength are essential, too much can lead to dysfunction.
She also shared that during Bikram yoga, she experienced significant leaking and dizziness, signaling that her body was pushing past its limits. These moments became opportunities to reframe her approach, integrating restorative yoga and self-care practices to complement her strengthening efforts.
As we discussed further, I introduced the idea that balance changes as we transition through hormonal seasons—monthly, yearly, and across the lifespan. What works in our 20s and 30s often doesn’t serve us the same way in our 40s, 50s, and beyond. This opened up a conversation about her microbiome and estrobolome—the gut bacteria that process estrogen. These systems influence weight, libido, mood, and overall health, connecting back to her bladder and sexual symptoms.
This case exemplifies how addressing multiple systems—biomechanical, hormonal, emotional, and more—can lead to deeper insights and meaningful improvements. By guiding clients to listen to their bodies, balance their efforts, and adapt to their changing needs, we can help them achieve greater health and well-being.
OTPF-4: Client Factors
Let’s take a moment to connect our discussion to the professional framework provided by the OTPF-4, specifically within the client factors table. These slides (refer to the handout) highlight how our work aligns with and is supported by the framework, emphasizing the comprehensive scope of occupational therapy.
I circled values, beliefs, and spirituality because they connect to the foundational work we do with clients, addressing their core motivations and perspectives. I also circled bodily functions and mental functions, including thought, emotional regulation, and consciousness, all of which tie into nervous system regulation—a concept we’ll explore further later.
The OTPF-4 notes that occupational therapy practitioners have a broad knowledge of body functions and understand how interactions among these systems support health, well-being, and participation in life through meaningful occupation. This includes areas such as nervous system regulation, voice and speech (highlighting the connection between the glottis and pelvic floor), and broader systems like cardiovascular, immunological, respiratory, digestive, metabolic, endocrine, genitourinary, and reproductive. These are where hormones, sensory energy, drive, and sleep intersect—key areas we address with clients.
I also starred vestibular and proprioceptive functions, which are integral to nervous system regulation, which we’ll explore further. The neuromusculoskeletal and movement functions highlighted in the OTPF-4 reinforce the essential interplay between physical and functional health in supporting occupational performance.
Thank you, OTPF-4, for providing a robust framework that validates and strengthens our work. This framework ensures that we address the full scope of human function and its interaction with occupation. This comprehensive perspective helps guide us in supporting our clients’ health and participation across all areas of life.
What Blocks Us?
Let’s examine what prevents moms from successfully implementing the effective interventions we’ve discussed. Despite the many tools available, significant barriers make navigating postpartum life particularly challenging.
Time management is a real struggle. Moms often juggle dysregulation, fear, worry, stress, pressure, anxiety, depression, resentment, anger, sadness, and overwhelm. These emotions sound all too familiar to many, and they are compounded by poor boundaries, inadequate sleep, insufficient nutrition and hydration, and a lack of support—or difficulty receiving support. Limiting beliefs, unresolved stories, and coping mechanisms that no longer serve them further complicate the picture, alongside a decreased self-awareness of triggers, tipping points, and strategies to manage them.
Dr. Jessica McHugh Conlin opened this conference by highlighting the critical importance of maternal mental health and its far-reaching implications. Moms face an extraordinary cognitive load—balancing multiple roles and responsibilities while navigating hormonal chaos. The shame and guilt they feel when they can’t seamlessly keep all the balls in the air only add to the burden.
The images in Figure 1 illustrate this reality.

Figure 1. Examples of roles of new moms.
The mom is multitasking with baby care, home management, and returning to work while battling frustration and sleep deprivation. The image on the bottom right captures the culmination of it all—shutdown mode. A mom lays on a pile of laundry, aware of what she needs to do but unable to act. Her child is nearby, but she’s disengaged, watching a tablet. This moment reflects poor modeling for her child, and it’s likely the beginning of nervous system dysregulation in that child.
Children notice these moments deeply. They may wonder, Why doesn’t mom want to play with me? Am I not enough? Do I need to take on the role of making her feel better? These experiences contribute to the formation of their own stories and coping mechanisms. When a mom is unkempt or hasn’t been able to shower or use the bathroom in peace, it highlights how basic self-care can fall by the wayside, further exacerbating dysregulation.
Nervous system dysregulation leads to increased allostatic load, the cumulative wear and tear on the body from chronic stress. This can result in poor health markers, disease, maladaptive coping strategies, and ineffective parenting models. Over time, it reinforces intergenerational trauma by fostering dysregulated children with limited social-emotional intelligence and poor coping skills.
Breaking this cycle starts with recognizing and addressing these blocks. By helping moms develop strategies to regulate their nervous systems, prioritize self-care, and reframe their stories, we can support them in creating healthier dynamics for themselves and their families. This work isn’t just about the mom’s well-being—it’s about shaping a positive foundation for the next generation.
What Transforms Us?
So, what transforms us? How do we truly set moms up for success? It begins by understanding their communication and learning styles early on. Identify their specific blocks and determine what they need to thrive. Ask them how they feel about exercises—do they find structure helpful, or does it stress them out? The key is to work with what works for them.
Tools like motivational interviewing, active listening, and reflective listening help uncover what drives and motivates them. Habit stacking can make these strategies more accessible by integrating small, manageable habits into their daily routines. Work with their calendars to schedule and create bite-sized, tangible, and easy-to-achieve goals. These small successes build confidence and create momentum.
To bulletproof recovery, go beyond identifying blocks—break them down. Address the underlying nervous system and social-emotional contributors to their challenges. This comprehensive approach often reduces the physical symptoms that initially brought them in.
I used to say, “It all comes back to the breath,” but I’ve now revised that to, “It all comes back to the nervous system,” which naturally incorporates the breath. It’s a broader, more integrated perspective. And it’s critical to reframe postpartum not as something to “get past” but as a way of moving forward into life’s next transitions with agency and self-awareness.
As occupational therapy practitioners, occupational-based programming is where we shine. Instead of adding to the overwhelming to-do list and contributing to feelings of shame, inadequacy, or failure, we can help moms integrate therapeutic work into their daily activities. This image shows how much therapeutic movement occurs in a single day as a new mom.
Teach moms to be mindful and intentional in these moments. When they say, “I didn’t get to do anything—I’m a bad student—I didn’t do my homework,” shame and guilt often pile up. Help them reframe. Highlight all they did accomplish, even if they didn’t recognize it as therapy. Reinforce their progress and successes by creating easy, achievable tasks that fit naturally into their day.
For example:
- Work on posture and alignment while feeding the baby.
- Incorporate core, pelvic floor, and intra-abdominal pressure strategies during floor play or while lifting the baby.
- Use functional mobility and transportation activities as opportunities to reinforce alignment strategies.
Helping moms integrate these practices seamlessly into their lives empowers them to feel accomplished, reduce stress, and create sustainable habits that enhance recovery and well-being. This approach isn’t just about recovery—it’s about equipping them to move forward confidently into the next stages of life.
Well-Being Study
The psychological well-being of women in the perinatal period remains poorly understood, yet it is clear that subjective well-being and health are deeply interconnected. Diener and Chan’s review of well-being, health, and longevity highlights that well-being is as impactful on health as many other behaviors—underscoring that poor well-being during this period can be a precursor to future illness if not addressed. The Department of Health England reinforces this connection, emphasizing that promoting emotional well-being is just as vital as supporting physical health. The two go hand in hand.
A recent study surveyed 19 women aged 18 to 40 years who had given birth within the last six months. The findings revealed that many aspects of well-being were compromised postpartum, particularly vitality and positive functioning. The women described challenges in feeling good about themselves and a lack of trust in their parenting abilities. Social isolation was a recurring theme, and relationships—both with partners and communities—played a significant role in their sense of well-being. Many reported stress and conflict related to relationship changes, including pressures to return to intimacy, often self-imposed.
Interestingly, while these women recognized shifts in their subjective well-being, they were hesitant to frame their experiences as depression or dissatisfaction with their baby or situation. This highlights a key point: many women do not seek support because they do not perceive their challenges as significant enough or fear stigma. This insight presents an opportunity to educate, advocate, and break down the stigma around decreased postpartum well-being. Without acknowledgment, it becomes nearly impossible to seek support or make improvements.
The study utilized the European Social Survey well-being model, examining seven focus areas:
- Emotional well-being: Balancing positive and negative emotions.
- Satisfying life: Positively evaluating life overall.
- Vitality: Having energy, feeling rested, and being physically active.
- Resilience and self-esteem: Feeling good about oneself, optimistic for the future, and able to handle difficulties.
- Positive functioning: Autonomy, competence, engagement, meaning, and purpose—an area occupational therapy practitioners excel in supporting.
- Supportive relationships: Close, trusting relationships with family and friends.
- Trust and belonging: Feeling respected and supported within one’s community.
A powerful quote from the study captures the essence of postpartum challenges:
"Women reported that the time after birth was often challenging in terms of feeling good about themselves. This was attributed to new learning skills, getting to know a new baby, and experiencing changes to family dynamics, all of which were challenges to their sense of who they were and their ability to cope."
This encapsulates the cycle of new learning, identity shifts, self-doubt, and limiting beliefs—all of which feed into nervous system dysregulation. These insights further reinforce the importance of occupational-based programming as a best practice. By addressing these challenges through purposeful activities, nervous system regulation, and targeted support, we can empower women to navigate postpartum transitions with resilience and confidence. This work is not just about addressing immediate needs but fostering long-term well-being and vitality.
Journaling and Tracking
Journaling and tracking can be powerful tools for building awareness and establishing a mindful practice for mothers and babies. A mother and baby journal acknowledges that mom counts, too. It's not just about logging the baby’s poops, diapers, and feeds—it’s also about tracking the mom’s trends, symptoms, and experiences. This dual approach helps identify red flags early and provides insight into overlapping symptoms that may go unnoticed.
This is particularly relevant for new moms in their late 30s and early 40s who may already be experiencing early perimenopausal changes. The overlap between postpartum and perimenopausal symptoms can lead to delays in intervention. Journaling offers a way to tease apart these symptoms, creating clarity and reducing the risk of mismanagement.
Beyond its diagnostic and organizational benefits, journaling is inherently therapeutic. Many clients have shared that they feel better simply by writing things down. Journaling can bring awareness, facilitate emotional processing, and help “move things through” mentally and emotionally. Tracking is a form of data collection—empowering moms with knowledge about their bodies, routines, and emotional states.
This systematic and organized approach allows moms and practitioners to receive and process information effectively, forming the foundation for informed care plans. With this awareness, care becomes proactive, personalized, and focused on achieving optimal outcomes, ensuring both mother and baby thrive.
What to Track
Tracking can be a transformative tool for understanding connections that might otherwise go unnoticed, especially in the counterintuitive world of pelvic health. What might seem like a helpful approach can sometimes lead to unintended consequences, so detailed tracking allows us to uncover patterns and connections that support more effective interventions.
Some general pelvic health indicators that can be helpful for clients to track include:
- Urinary and gastrointestinal symptoms: bladder and bowel habits.
- Sleep patterns.
- Menstrual cycle details.
- Headaches, migraines, nausea, dizziness, and vertigo.
- Emotions, stressors, and thoughts.
- Daily events, activity routines, and medication changes.
For clients with overlapping symptoms related to pregnancy and perimenopause—such as mood changes, anxiety, breast tenderness, irregular cycles, fatigue, sleep difficulties, cognition challenges, vaginal dryness, and genitourinary symptoms—tracking these can reveal critical insights. Not all clients need to track everything, but during your interview, you can work with them to identify the most relevant aspects based on their stories and concerns.
Tracking can help uncover surprising connections. For example:
- How constipation and mood might influence bladder leakage.
- How anxiety and interpersonal stressors might exacerbate bladder pain or vulvodynia.
- How sensitivities to sugar or gluten might impact mood or pelvic organ prolapse symptoms.
One client illustrates the importance of tracking. She came to me initially during the summer but stopped therapy after feeling overwhelmed, particularly with the stress of hosting her in-laws for several months. She admitted to trying to fast-track her recovery, experimenting with a birth control hack by skipping the placebo week to eliminate menstruation, hoping to reduce inflammation and bladder pain. However, this approach backfired, and she experienced continuous bleeding for months.
Compounding this, she stopped taking her thyroid medication due to challenges finding a new provider after relocating. This led to significant bladder symptoms—urgency every 30 minutes during the day, nocturia up to six times per night, and poor sleep—which affected her emotional wellness. Although she identified as “always anxious,” she struggled to connect her worsening symptoms to her anxiety. Through education and connecting the dots, we began to build her buy-in for a more strategic, holistic approach.
We also uncovered a C-section scar that was referring pain to her bladder, further contributing to her symptoms. Given her challenges, I recommended tracking several aspects of her health:
- Bowel movements and gastrointestinal symptoms.
- Bladder symptoms, including urgency and frequency.
- Hydration and nutrition intake.
- Stressors and anxieties, noting connections with bladder symptoms.
- BASE signals: breathing, actions, senses, and emotions—observing how these factors interact with her symptoms.
- Sleep patterns, fatigue levels, and cognitive changes.
This comprehensive tracking plan allows us to create a customized bladder retraining program. For example, with urgency every 30 minutes, we’ll work to gradually extend this to 40 minutes, then 45 minutes, and so on. Tracking will also provide data to develop an individualized nervous system regulation profile tailored to her needs.
By focusing on these details, tracking empowers clients with knowledge and helps establish actionable steps toward recovery. This approach fosters deeper engagement, allowing clients to see and embrace the connections between their habits, symptoms, and well-being.
Postpartum Journal & Tracker
Figure 2 shows two Images from the full mother and baby postpartum journal and tracking.
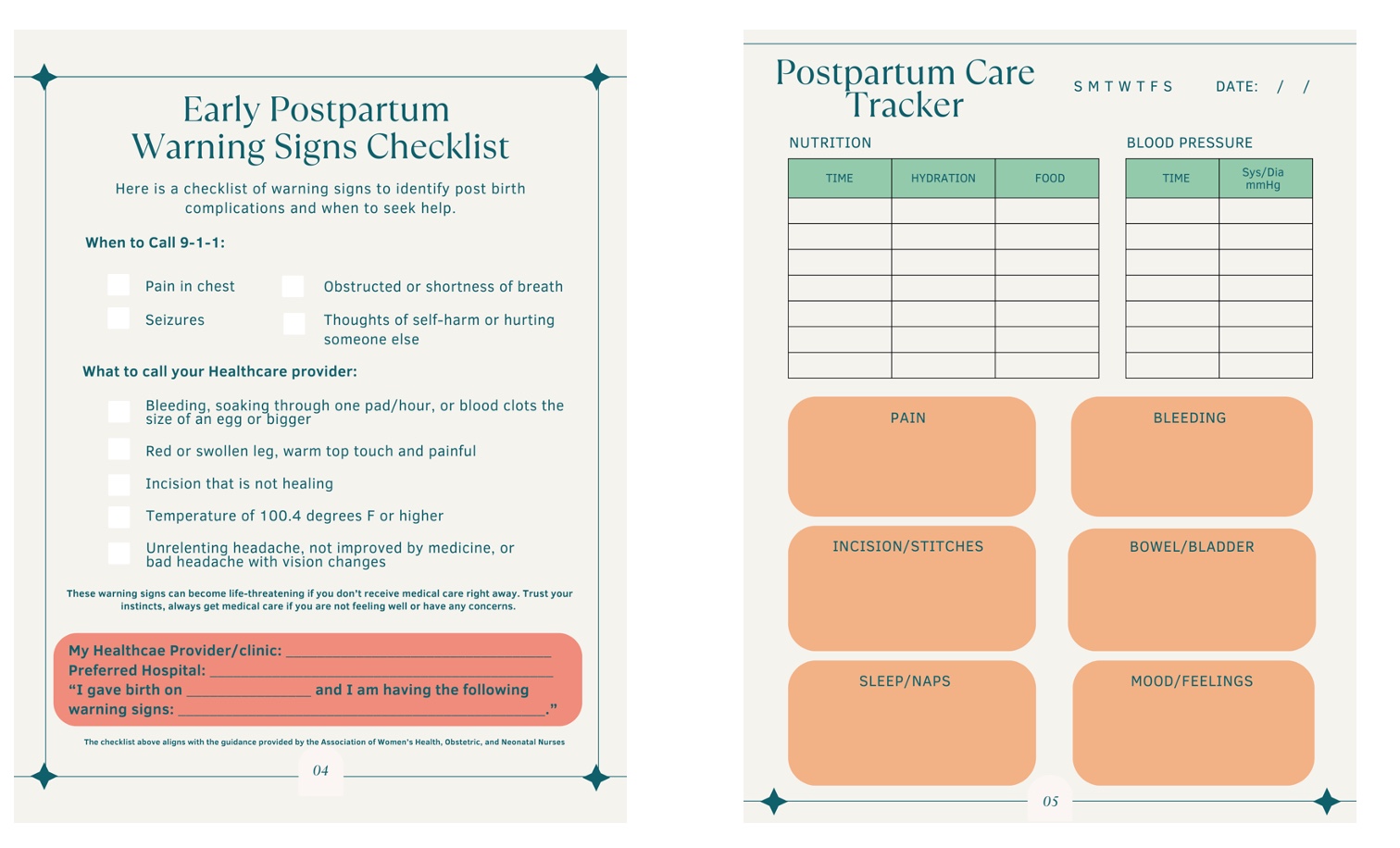
Figure 2. Postpartum Journal and Tracker. (Click here to enlarge this image.)
Dr. Ali Kochi, a pelvic health doctor of physical therapy, worked with me earlier this year during the Birth Healing Summit hosted by Lynn Schulte to help create the Mom and Baby Journal. Dr. Kochi recently had her third baby this past August, and her insights into the process are invaluable. Here’s a quote from her about the impact of the journal:
"By researching and creating the Mom and Baby Journal, I uncovered not only the resilience of my body but also the importance of self-reflection and monitoring my mental and physical well-being. It became my lifeline, helping me identify the subtle signs of preeclampsia that might have gone unnoticed. Trust your instincts about your body—your journey is the key to your health."
Dr. Kochi’s pregnancy was considered geriatric, though it was otherwise uneventful. She had no blood pressure issues, diabetes, weight concerns, or mood challenges. However, the postpartum tracker proved to be lifesaving for her. She emphasizes that monitoring the mother’s health, not just the baby’s, is critical and that we can’t rely solely on brief interactions during doctor’s visits.
One week postpartum, Dr. Kochi began feeling unusually exhausted and unwell. Trusting her instincts and knowledge from creating the journal, she checked her blood pressure. Initially, in the 130s to 140s, it continued to climb. She also noticed that her swollen ankles weren’t improving with elevation, compression, or ankle pumps. By the next day, her blood pressure was in the 160s. Even as she doubted herself—what she refers to as “self-gaslighting”—she kept monitoring. When it reached 171/110, along with redness in her face and her ankles feeling “like Tempur-Pedic mattresses,” she knew it was serious.
She went to the ER, where the nurses were astonished she had caught it early. They asked what made her check, and she credited her research and inner awareness. Her experience highlights the importance of taking vitals for clients, recommending that every postpartum individual have a blood pressure cuff, and encouraging them to track and trend their symptoms.
This process ties into critical postpartum care. Dr. Rebecca and Jenna Seagrave’s discussion (Day 3 of the Virtual Conference) during their session on acute postpartum rehab stressed that the timeframe before the six-week checkup is critical and should not be overlooked. Dr. Kochi’s story exemplifies why early monitoring is essential.
The Postpartum Care Tracker includes:
- A checklist of early postpartum warning signs (when to call 911, when to reach out to a provider, and what information to provide).
- There are sections for tracking vital aspects such as nutrition, blood pressure, pain, bleeding, incision healing, emotions, and mood.
This resource is available as a PDF in the handout section, and I encourage you to use it for yourself, your clients, your family, and your friends. Please share it widely—it’s a valuable tool for empowering postpartum individuals to take charge of their health and well-being.
Below the Surface
To truly address the drivers and root causes of issues, we must look below the surface at the subconscious factors that often influence our experiences without full awareness. I use the analogy of an iceberg to illustrate this concept. The part of the iceberg above the water represents our conscious awareness—the things we readily see and recognize. However, the larger mass below the surface represents our subconscious awareness—the hidden influences that operate behind the scenes and often hold the key to resolving deeper issues.
These subconscious drivers are critical to uncover because they frequently contribute to the root cause of a problem. Without addressing them, we risk creating a "revolving door" scenario where clients improve temporarily but return later with the same issue—a month, two months, or even a year down the road. By working with clients to delve beneath the surface and identify these hidden influences, we can create lasting change, breaking cycles of recurrence and promoting sustainable well-being.
This approach is not just about symptom management but about true resolution. It requires curiosity, patience, and the willingness to go beyond what is immediately visible. It enables clients to gain awareness of subconscious patterns and connections that may be driving their challenges. Together, we can foster deeper healing and resilience, ensuring their temporary and transformative progress.
Nervous System (NS) Regulation & Redesign
Starting with Permission to Feel by Dr. Mark Brackett, I’ll be upfront—this book was a game changer for me. It came into my life after I had begun exploring nervous system regulation, and it illuminated how emotionally illiterate I was. It pushed me to expand my emotional vocabulary, a journey that has significantly influenced both my personal growth and my approach to working with clients.
A critical question to ask clients is, How are you feeling? But it’s not just about getting a surface-level answer like “good” or “bad.” It’s about holding space for them to explore their emotions more deeply. What are they really feeling? How has their mental health been affected? Do they know when they are dysregulated? What are the signs they recognize in themselves, and what strategies do they use to cope? We can establish a baseline for understanding their emotional and mental state by asking these questions.
Some clients may have already developed a deep understanding of these concepts, perhaps even more so than us. That’s why it’s crucial to begin by understanding where they are, socially, emotionally, and hormonally, before determining how to move forward.
One of the questions I often pose is, How can we help our kids manage their emotions and behaviors if we don’t know how to manage our own or model it for them? It starts with us. I firmly believe in learning through lived experience—it’s how I teach. Live it, learn it, apply it. By diving into these practices ourselves, we can better support our clients and, ultimately, model healthy behaviors for the next generation.
Nervous system regulation is a foundation we can build upon to redesign how we approach therapy. By addressing the nervous system, we can:
- Break cycles of dysregulation.
- Decrease the allostatic load (the wear and tear of chronic stress on the body).
- Heal at the ground level, supporting physical rehabilitation efforts.
The nervous system drives many of the more visible symptoms that bring clients into therapy. If we can integrate nervous system awareness and regulation into our programming, the potential for profound and lasting effects is immense. This approach helps us address the symptoms and underlying drivers, creating opportunities for true transformation and long-term resilience.
AIR Model
The book The Secret Language of the Body by Jennifer Mann and Cardin Rabin emphasizes a profound idea: our nervous system always communicates with us, yet most of us haven’t been taught how to interpret its signals. The authors liken this disconnect to visiting a foreign country and trying to order food in your native language—you may not get what you want, or perhaps nothing at all.
This concept is particularly relevant when addressing symptoms like bladder pain. If we misunderstand the body's "alarm signals," we may apply interventions that are not only ineffective but could worsen the issue. For example, treating bladder pain with Kegels can exacerbate the problem if the pain stems from overactivity or tension in the pelvic floor. Instead of providing relief, such mismatched interventions lead to frustration, discouragement, and even greater discomfort.
The key lies in understanding the language of the body: learning to listen to the nervous system's signals, understanding their meaning, and responding appropriately. This alignment allows us to unlock more effective and compassionate approaches to healing. Progress often requires curiosity and a willingness to learn the "foreign language" of our bodies.
The AIR model—Awareness, Interruption, and Redesign—provides a structured nervous system regulation and healing method. This approach allows us to move beyond patterns of dysfunction and create new pathways for resilience and balance. Here's a breakdown of the AIR model:
- Awareness: Recognizing and understanding what’s happening within our bodies and minds.
- Interruption: Implementing strategies to disrupt unhelpful or automatic responses.
- Redesign: Creating new, healthier patterns for the brain, body, and nervous system to adopt.
We apply the AIR model to three domains: mind, body, and human experience. Let’s explore a few examples:
Mind:
- Switching: This interruption strategy uses exercises that engage vestibular and proprioceptive systems. Examples include wall push-ups combined with head turns, bringing a knee to the chest while breathing or visual tracking paired with arm circles while balancing on one leg. These practices help reset the nervous system by integrating movement and sensory input.
- Distancing: As part of the redesign process, this practice involves cultivating an observational self. By viewing oneself and the situation from a detached, scenic perspective—without judgment—it becomes easier to gather information and make sense of what’s happening.
Body:
- Translating: This awareness tool helps identify nervous system states and understand the underlying triggers. It brings clarity to why we’re experiencing certain physical or emotional sensations.
Human Experience:
- Attuning, Tending, and Bonding: These practices focus on fostering connection and care, both for oneself and with others. They provide a foundation for emotional safety and regulation, which is critical for healing.
I’ll dive deeper into these domains when I share my personal experience, illustrating how these principles have been applied in practice to foster growth and transformation. The AIR model equips us to interpret the nervous system’s signals and guide our clients (and ourselves) toward a more balanced and empowered state of being.
BASE
BASE is a framework I use during interruption exercises to help clients become aware of what their body is communicating before applying strategies and assessing shifts. BASE stands for Breathing, Action, Sensations, and Emotions. It’s a tool to drop into the body, bring awareness to the present state, apply an intervention, and revisit BASE to see if there's a noticeable change.
This method is particularly useful for clients who may not naturally connect with their body’s signals, like the client I mentioned earlier with bladder pain who attempted to "hack" her hormones and fast-track her healing. I’ve encouraged her to integrate BASE into her tracking system to help her tune in more effectively.
B: Breathing
- What am I feeling in my breath?
- Locations: Is it centered in the belly, chest, lungs, or nose?
- Speed and depth: Is it slow, fast, shallow, or deep?
- Qualities: Is the breath comfortable and easy, or does it feel uncomfortable and restricted?
A: Action
- What does my body want to do, and how does it want to do it?
- Posture and shape: Is it slouched, tense, upright, relaxed, or rigid?
- Potential movements: Am I fidgety, jumpy, distracted, yelling, stuck, still, or hiding?
- Energy: What is the energy level—high, low, sleepy, hyper, placid, or buzzing?
S: Sensations
- What am I feeling in my body and where?
- Descriptors: Tingling, tension, gripping, burning, relaxing.
- Location: Is it in my belly, head, chest, or elsewhere?
- Movement: Is it fixed, still, spreading, or moving?
- Qualities: What’s the intensity? Is it stuck, flowing, constant, or intermittent?
E: Emotions
- How am I feeling, and where in my body am I feeling it?
- Labels: Anger, sadness, fear, or others.
- Location: Jaw, chest, lower back, shoulders?
- Intensity: Is it mild irritation or full-blown rage? Nervousness or terror?
- Qualities: Is it stuck, spreading, wanting to move, or blended with other feelings?
We help clients build awareness and attunement to their internal experiences by walking them through these elements. Once strategies are applied, BASE provides a structure to reassess whether any changes have occurred, creating a clearer understanding of how the body responds to interventions. This process fosters a deeper connection to the body, promotes meaningful progress, and enhances the overall effectiveness of their healing journey.
Mind, Body, Human
The mind, body, human concept ties directly into awareness, interruption, and redesign. It provides a lens to examine how we experience and process stress, emotions, and behaviors and how we can move toward healing and breaking generational cycles of dysregulation.
The mind represents our thinking brain—the part that wants to make sense of everything. It’s where clients often get stuck, asking questions like, Why is this happening? What’s it about? They want answers, but sometimes those answers aren’t immediately accessible. I gently redirect them to their present experience: What are you feeling? What are you noticing? Does this feel good, bad, or indifferent? This shift from thinking to experiencing helps them connect more deeply to their body’s signals.
The body encompasses our survival states and nervous system regulation. We are familiar with states like ventral vagal (calm and connected), fight or flight (high energy and mobilization), and freeze (immobilization, either with high or low energy). The goal isn’t to avoid stress or remain calm—that’s unrealistic. Instead, we work on expanding the window of tolerance so clients can move through stressors more efficiently and with less overwhelm. I emphasize that stressors will still arise, but building resilience helps shift through these states more smoothly.
The human aspect delves into attachment wounds and the inner child, exploring what we needed but didn’t receive in our formative years. It’s often not about what was done to us but what was missing—validation, love, or support. This process allows us to uncover how early experiences shaped our nervous system responses and behaviors. For example, when we consider the overwhelmed mom on the laundry pile, we can ask: What didn’t she get that she needed to feel regulated? What does her child now need to avoid perpetuating the same cycle?
I’ve personally experienced the impact of this process. For instance, when my kids were younger, I struggled with the transitional moments of getting them out the door. I’d end up yelling despite trying to approach the situation logically with strategies like giving them choices or creating routines. I now understand that I was relying solely on my thinking brain, never interrupting the behavioral response or recognizing subconscious coping mechanisms at play.
By using switching and translating practices, I’ve learned to shift my nervous system state and employ observational distancing. This allows me to step back without judgment and see the situation from a calm, regulated perspective, considering everyone’s emotions and needs.
The redesign process required deeper inner child work to address the roots of my dysregulation. For me, this involved revisiting my 5-year-old self. When dysregulated, I pictured myself as a small child curled up in a corner, unable to make eye contact or speak. My throat felt tight, my fists clenched, and my body burned with anger and frustration. Through this process, I asked my younger self what she needed, and the answer was clear: attention, love, and to be believed.
I held space for my inner child, parenting her with compassion and validation. This work allowed me to parent my children from a place of calm and connection rather than reactive patterns modeled for me. When I speak to my children, I imagine my younger self across the kitchen island. I can say things like, I don’t like how you’re talking to me; that doesn’t feel good, with emotional clarity and empathy. I can better see through their struggles to the fear, vulnerability, and need for love and validation.
This transformation has broken old patterns and created healthier models for my children. It’s an ongoing process of awareness, interruption, and redesign that fosters not only personal healing but also intergenerational growth and resilience.
Celebrate the Wins
Celebrating wins is a vital part of the healing and growth journey, both for ourselves and our clients. It’s easy to keep pushing toward the next milestone or goal and forget to acknowledge the progress we've made. Encouraging a positive mindset can make a profound difference.
One resource I often draw on is The Gap and the Gain by Dan Sullivan and Dr. Benjamin Hardy. This book introduces a concept I love sharing with clients: focusing on "the gain" rather than "the gap." The "gap" is the space between where we are and where we want to be, often leading to feelings of inadequacy or negativity. The "gain" is the recognition of how far we've come, creating a sense of accomplishment and optimism. Measuring backward—looking at the progress made rather than only forward at the goals yet to achieve—fosters positivity.
Incorporating sensory experiences is also crucial. Lindsay Vestal talks about the power of sensory anchoring, encouraging us to really savor our wins and embody them, so they don't just pass us by. It’s a simple but powerful practice that transforms fleeting moments into something more meaningful.
Pendulation is another important concept, reminding us that ups and downs are natural. We won’t always feel steady or "good," and accepting this helps us avoid catastrophizing when things swing downward. Knowing that the pendulum will swing back up provides reassurance and resilience.
Some strategies I recommend for celebrating wins include journaling. Writing down three successes for the day and three goals for tomorrow is a simple but transformative exercise. I've incorporated this into my nightly routine with my kids. On Sunday nights, when they experience the "Sunday scaries," we reflect on the great things they did over the weekend and set positive intentions for the week ahead. It’s a small practice, but it makes a big impact.
Another technique I encourage is asking the subconscious to "sleep on it." Before bed, I reflect on something I want clarity on, allowing my deep and REM sleep to process it. Upon waking, I take a moment to tune in and note my thoughts and feelings. This practice taps into the unconscious for creative problem-solving and self-reflection.
With clients, I make it a point to ask about what they did for fun, rather than just focusing on their pain or symptoms. This not only gets them thinking about positive experiences but also highlights whether they’re neglecting joyful activities in their routine. Sometimes, realizing they haven't prioritized fun can inspire them to intentionally create space for it.
Another resource I find valuable is Tammy Lynn Kent's books Wild Creative and Wild Feminine. These works emphasize prioritizing joys and “big rocks”—the foundational elements that create space and capacity for everything else. By anchoring clients in their passions and positive experiences, we can help them stay grounded and balanced.
When working through heavy or traumatic experiences with clients, I also like to balance the session by talking about something that makes them happy. This dual focus not only helps process trauma but also reduces protective tension and allows for a release through a positive lens.
As we wrap up, it’s crucial to recognize pregnancy and postpartum as windows of opportunity, not obstacles. By embracing this period as a time for self-discovery and connection with our bodies, we can change the narrative. Hormonal wisdom can help identify predictors of illness or menopause challenges, emphasizing prevention over intervention. Nervous system regulation can further reduce the allostatic load and foster well-being, helping to break cycles of intergenerational trauma.
Finally, I encourage you to support broader access to care through advocacy. The Pregnancy and Postpartum Act (HR 2480) is a federal bill aiming to provide pelvic health services to all pregnant and postpartum individuals. While this is a huge step forward, the bill currently defines pelvic health services as physical therapy alone. Occupational therapy must also be included to maximize the impact and capacity to serve this population. Let’s work together to advocate for a more inclusive definition.
AOTA
And AOTA helped us set up on our legislative action center ways to do that. You just, you go here, you click in your information, it pulls up your local reps for you and then we have a letter already written and you can edit it as you see fit or submit it as is and then you're done.
Summary/For More Information...
So if you want more essential pelvic health education, we have courses. Can you Education courses, workshops, membership and please email reach out. You can hit me up directly@infoessentialpelvichealth.com I have the website and the Instagram and the Facebook page as well as an essential pelvic health education Facebook group where I invite all clinicians, wellness professionals, medical providers and clients to ask questions, share information and connect.
Exam Poll
1)Which of the following is an example of how hormonal changes impact postpartum women, often continuing into perimenopause?
The answer is B cognitive changes such as brain fog and short-term memory loss.
2)Hypertensive disorders during pregnancy are primarily associated with which long-term health risk?
The answer is C cardiovascular disease.
3)What is a recommended practice for postpartum individuals to support nervous system regulation?
The answer is C, meditation and paced breathing.
4)In addressing well-being and longevity postpartum, why is journaling suggested as a beneficial practice?
Journaling is beneficial for identifying early signs of overlapping symptoms between postpartum and perimenopause.
5)What is an overlapping condition in both pregnancy and perimenopause?
The correct answer is all of the above.
Questions and Answers
How do you monitor Estrobo?
Monitoring Estrobo is not something I actively do, although there may be potential tests available. Instead, I focus on its broader effects, such as its impact on libido, weight gain, nutrition, and hormone metabolism. These factors help guide how I take Estrobo into consideration.
What interventions would you implement for vaginal dryness and vulvodynia?
I would start by assessing the individual’s hormone health and timeline to understand their hormonal balance. I would also evaluate their emotional status, nervous system, pelvic floor muscular tension, and coordination. Examining the vaginal tissues for dehydration, irritation, or signs of low estrogen is another key step. Based on this assessment, interventions could include vaginal estrogen, non-hormonal vaginal moisturizers, or specific lubricants, depending on the timing and nature of the vulvodynia, such as if it occurs during intercourse. If pelvic floor tension is a factor, I might recommend breathwork to help reduce tension and give the client tools to manage it consciously. This approach emphasizes creating mind-body connections and empowering clients to address their symptoms.
References
Please refer to the additional handout.
Citation
Rowan, L. (2024). Postpartum path to well-being and longevity: Postnatal pelvic health virtual conference. OccupationalTherapy.com, Article 5764. Available at www.occupationaltherapy.com
