Editor's note: This text-based course is a transcript of the webinar, The Reinvention Of Occupational Identity: A Decision-Making Approach, presented by Andy Pitts, DrOT, OTR/L.
Learning Outcomes
- After this course, participants will be able to identify possible clients to implement the elements of the framework.
- After this course, participants will be able to recognize opportunities to modify treatment approaches to incorporate occupational identity.
- After this course, participants will be able to list strategies and documents needed to fully execute the framework with older adult clients.
Introduction
- Why a decision-making framework?
- Worked in Skilled-Nursing
- Observed trends in the older adult clients
- Decreased Engagement
- Decreased Quality of Life
- Compromised Sense of Occupational Identity
Hello, everyone. I'm thrilled to be here to share insights about this topic. I'm an occupational therapist in North Florida with over five and a half years of diverse experience, ranging from school-based practice to skilled nursing. This varied background has exposed me to numerous opportunities and perspectives within the field.
Before we delve into the framework, let me provide some context about its inception. While working in a skilled nursing facility, I noticed a common theme among my clients – a significant portion either had sedentary lifestyles or, even more disheartening, lacked any primary occupation beyond watching TV. As occupational therapists, we understand the importance of engaging in meaningful activities for overall well-being, akin to our daily intake of vegetables. It became apparent that the occupational identity of these clients was compromised due to their limited engagement in activities.
Drawing on Gary Kielhofner's concept of occupational identity in the Model of Human Occupation (MOHO), which emphasizes identity formation through meaningful and personally relevant occupations, I explored this issue further. This led to the development of a framework that I will discuss throughout this session.
I want this talk to serve as a catalyst for your own reflections and spark thought-provoking conversations. It's crucial to note that the framework I'll present is a product of my doctoral capstone, currently in a phase of continuous improvement. While promising, the data collected is not foolproof, and there's ongoing work regarding future research and opportunities for refinement.
I appreciate your understanding that the aim of this course is to introduce you to a new perspective rather than make you an instant expert on the framework. I encourage you to approach this as a starting point; your thoughts and suggestions are welcome. Please feel free to share them in the Q&A session.
To complete my story, during my time in the skilled nursing facility, I frequently encountered older adults with low arousal, limited physical abilities, and minimal interest in occupations. Their responses to my introduction as an occupational therapist were often disheartening – expressions of not working, not caring, or lacking interest. This prompted me to ponder, "I see and hear you, but how exactly do you see yourself? What is your identity?"
I look forward to further exploring these questions and sharing the framework from these reflections. Thank you all for being here, and I appreciate your engagement as we navigate this session.
Operationalized Definitions
- Occupational Identity: The sense of self derived from the occupations clients engage in daily.
- How do OTs address it?
- What is the purpose of the framework?
- Occupation-Based Approach: Refers to a practice methodology where the occupational therapy practitioner utilizes occupation throughout the client’s continuum of care.
- Hybrid Approach: Refers to a practice methodology where the occupational therapy practitioner utilizes both biomechanical/rehabilitative frames in addition to occupation-based approaches.
Reflecting on my own experiences, I began questioning whether I had a clear occupational identity and how my decisions as an occupational therapist impacted the development of my clients' occupational identities. Operationalizing identity proved challenging due to its subjective nature. Identity, a fluid concept, evolves over time and is influenced by contextual factors like aging, physical and mental health, and life events such as retirement or marriage. Many clients could articulate their previous occupations but struggled to isolate those that formed their identity.
In response, I developed a framework that addresses occupational identity within the occupational therapy process, encompassing evaluation, assessment measures, and interventions. Before delving into the details, establishing ground rules and providing operationalized definitions became crucial.
Occupational identity remained a central theme, prompting questions for reflection. How do OTPs address occupational identity? As OTPs, we understand the significance of occupation-based practice, considering it the gold standard. This practice methodology seamlessly weaves occupation throughout a client's therapeutic journey, employing occupation-based assessment tools like COPM or the Barthel index, focusing on the quality of performance rather than specific skills.
I introduced a hybrid approach in my framework, recognizing the importance of preparatory approaches like biomechanical or rehabilitative methods. However, I emphasized bridging these approaches with actual occupation engagement. Acknowledging the appropriateness of this hybrid model for specific clients is crucial. For instance, those recovering from surgical procedures, like flexor tendon or rotator cuff repairs, may have constraints due to precautions or acuity. In such cases, interventions must align with these parameters while teaching clients occupation-based strategies to foster independence in desired activities. This balance ensures a holistic approach to rehabilitation, addressing both preparatory and occupation-focused aspects.
Methods and Theoretical Guidance
- Needs Assessment
- What is vs. Should be
- Phase I- Survey
- Phase II- Interviews
- Phase III- Beta Testing
- What is vs. Should be
- Dynamic Model of Occupation-Based Practice (Psillas & Stav, 2021)
- Places therapist at the center
- Views OBP as a continuum from Discrete to OBP.
- Kawa (Iwama, 2006)
- Contextual Analysis
The genesis of the framework emerged from my observations as a solitary clinician grappling with a prevalent issue in my practice. Wondering how other occupational therapists approached similar challenges led me to compare their methods with my envisioned ideal. To structure this exploration, I adopted a needs assessment methodology.
The needs assessment unfolded in three phases, beginning with pre-assessment (Phase One). Here, the investigator, in this case, me, identified the purpose for the needs assessment, determining what issues were at play and why they mattered. Stakeholders of occupational therapy services, essentially us as OTPs, played a pivotal role in this phase. To gauge the current practices among therapists, I designed a survey focusing on assessment tools, interventions, the balance between exercise and occupation-based approaches, and the utilization of theories and frames of reference.
Moving to Phase Two, the data collection phase, we delved into a comparative analysis, identifying gaps between observed practices and the desired standards. This phase served as the foundation for Phase Three, the implementation of the framework.
The Dynamic Model of Occupation-Based Practice guided this entire process, an innovative model that places the therapist at the center rather than the client. Developed by Dr. Wendy Staub and Dr. Seraph Sills, this model assesses the level of occupation-based practice therapists employ, treating it as a continuum. It scrutinizes elements like therapeutic intent and authentic occupations.
In conjunction with this, I incorporated the Kawa Model, not in a conventional sense for intervention or evaluation, but as a contextual analysis for Phase Two participants. Clients created Kawa diagrams based on their responses, and later, we coded these using Kawa principles. This multi-faceted approach aimed to provide a comprehensive understanding of the current state of occupational therapy practices and lay the groundwork for a more effective and client-centric framework.
- The Model of Human Occupation (Kielhofner, 1980)
- Volition- the act of choosing
- Habituation- repetitive doing
- Performance Patterns- increased performance and proficiency
- Theory of Identity Development (Marcia, 1961)
- Identity achievement, in which commitment is high and the person has gone through a period of exploring many options.
- Identity moratorium is when a person is trying out roles or activities to find the most suitable one.
- Identity foreclosure is when a decision has been made without looking into alternatives.
- Identity diffusion is when a person has no strong opinions or convictions and has made no effort to learn about or experience various options.
I also incorporated the Model of Human Occupation (MOHO), one of my favorites, especially its emphasis on volition. Given my focus on changing clinicians' decision-making, I found MOHO aligned well with the concept of volition. As clinicians become more acquainted with the framework, their daily practice habits will evolve and become more proficient.
Lastly, I drew on the theory of identity development, focusing on the stages of identity foreclosure and identity diffusion. These stages are pivotal, as they address common issues observed in the skilled nursing facility setting that prompted this journey. Identity foreclosure occurs when clients give up without exploring alternatives, while identity diffusion reflects a state of indifference. The framework aims to guide clients toward identity achievement, where commitment is high and they have actively explored and engaged in meaningful occupations.
I appreciate your patience as we navigate through this background information. Now, let's delve deeper into the practical aspects and application of the framework.
Occupational Deprivation Continuum
Whenever we talk about occupational identity, it's important that we talk about occupational deprivation. Occupational deprivation is when someone is being deprived of occupational opportunities. Figure 1 shows two systematic flows.
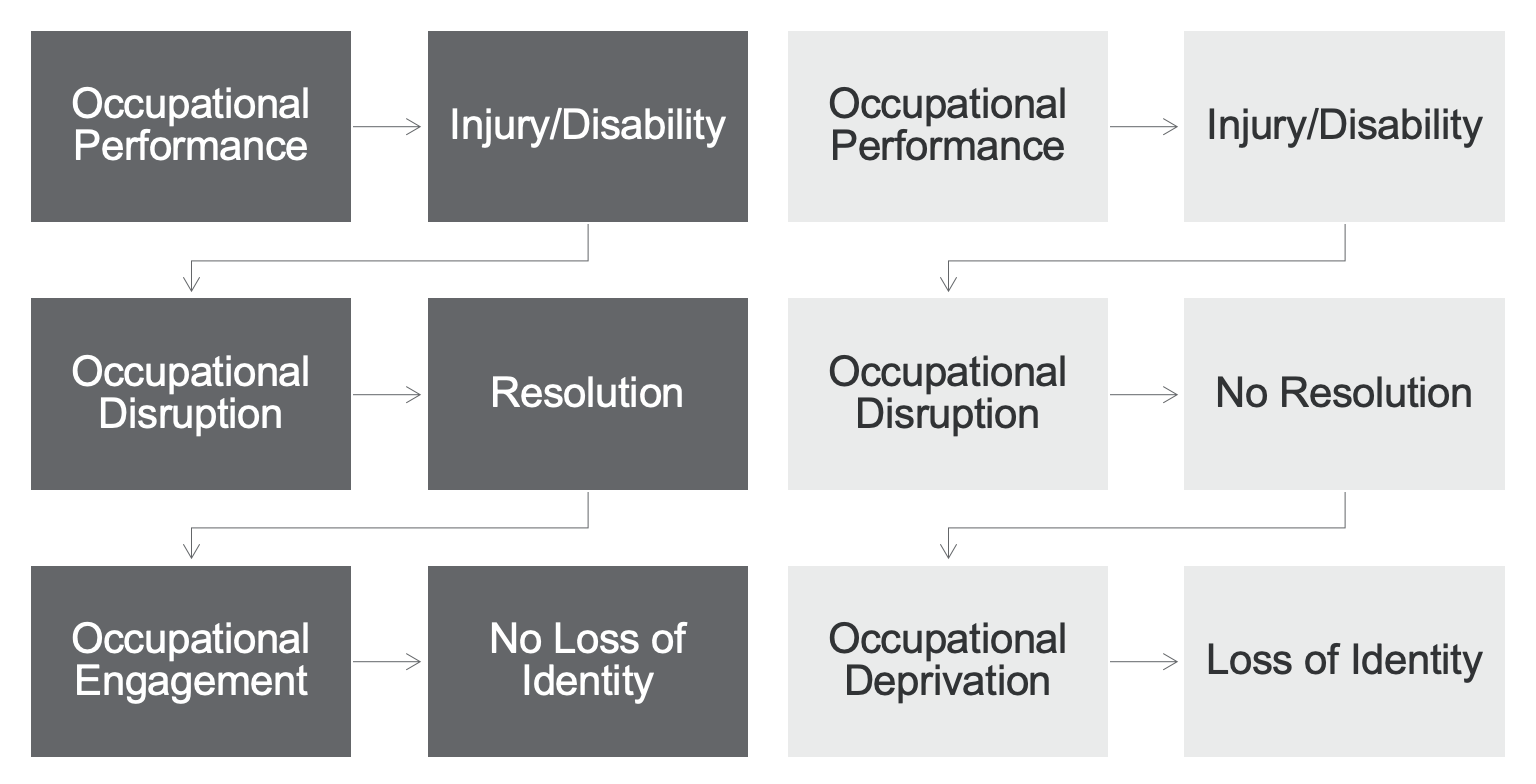
Figure 1. Systematic flows for occupational identity.
When occupational performance faces disruption, there are two potential outcomes to consider.
In the first scenario, resolution occurs. This might happen when a client experiences an improvement in health, allowing them to either replace lost occupations or continue engaging in them, albeit possibly at a different performance level. It's a positive turn of events that indicates adaptation and an enhanced ability to participate in meaningful activities.
On the flip side, if there is no resolution in the second scenario, the disruption persists, leading to occupational deprivation. This prolonged denial of meaningful occupational opportunities is significant, considering that occupational identity is closely tied to engaging in meaningful activities. The absence of these engagements can result in changes to a person's identity, often in a negative direction.
As occupational therapy practitioners, understanding these systematic flows is crucial for addressing disruptions and working towards positive resolutions. By preventing or mitigating the effects of occupational deprivation, we aim to foster a more positive impact on individuals' occupational identities. I look forward to delving further into the practical applications of these concepts within the framework.
Survey
Phases 1 and II
- Phase I Results
- Survey of 13 Occupational Therapists
- Consisted of 11 Questions
- Results showed a heavy reliance on preparatory approaches.
- Survey of 13 Occupational Therapists
Again, in phase one, I thought interviewing or surveying some therapists would be important. I had ideas of what was happening in the real world and wondered what everyone else was doing. I surveyed OTPs in various practice settings. These OTPs ranged in settings from home health to inpatient and skilled nursing. I even had a couple of outpatient and one acute.
Based on their responses (Figure 2), we can see that they're not using occupation-based practice very much.
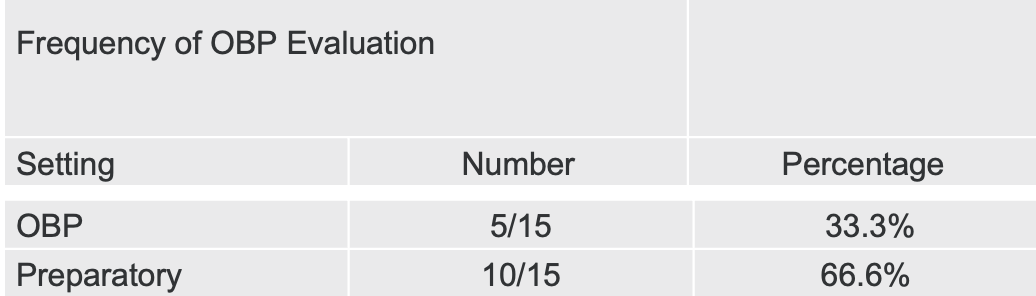
Figure 2. Chart showing survey results of OBP evaluation.
A notable trend emerged in examining the evaluation and assessment practices of OTPs through the survey. Approximately a third of the time, they were relying on occupation-based approaches. However, there was a significant reliance on biomechanics, the rehabilitative frame of reference, and other preparatory approaches. Furthermore, an alarming revelation surfaced – over 80% of treatments were predominantly exercise-based.
Equally concerning was the observation that OTPs were not consistently using models or frames of reference to guide their practice or make decisions regarding client care. This highlighted a potential gap in integrating theoretical frameworks within occupational therapy practices.
With this piece of the puzzle, attention naturally shifted to the other stakeholders – consumers or clients. Understanding their perspectives and experiences is pivotal to developing a more comprehensive and client-centered framework. As we continue, I'll delve into how these findings influenced the subsequent phases of the framework, aiming to bridge the gap between therapy practices and client needs.
- Phase II Results
- Semi-structured interviews of occupational therapy clients
- Open Ended Questions
- Interviewees expressed their experience with occupational therapy was not client-centered or encompassing of their occupational identity.
- Confirmed the results of the survey.
- Semi-structured interviews of occupational therapy clients
In phase two, I looked closer at the other crucial side of the equation: the clients themselves. Through semi-structured interviews, I engaged with clients who had experienced occupational therapy interventions. The findings from these interviews echoed and corroborated the patterns identified in the initial therapist survey.
Clients shared that occupational therapy practitioners primarily relied on exercise, often utilizing machines like bicycles or restorators. Importantly, clients felt that their goals were not consistently centered around their needs. Many expressed dissatisfaction, feeling that occupational therapists could not adequately address their unique concerns. This was often attributed to external factors such as stress and demands on the therapist's end, hindering the development of a strong therapist-client rapport. Consequently, this compromised the therapeutic use of self, reflecting a tendency to go through the motions rather than truly engaging with the clients on a personal level.
The interviews revealed a prevailing sentiment among clients—they were not satisfied with being treated as mere numbers, desiring a more personalized and meaningful approach. These insights strongly validated the initial hypothesis that occupational therapists were not effectively addressing the occupational identity of their clients. Armed with these findings, the framework evolved to bridge the gap and create a more client-centered and identity-focused approach within occupational therapy practices. As we progress, I'll delve deeper into how these revelations influenced the framework's subsequent phases and practical applications.
What's Next?
- Analyzed gaps in practice.
- Determined a logical flow for decision-making.
In the interim, I delved into analyzing practice gaps. Utilizing the collected information, I crafted a decision-making chart's flow and developed forms for streamlined data collection and service documentation. The framework's design was consciously modeled after the OTPF, aiming to ensure ease of adoption by therapists in their daily practice.
The primary focus remains on practicality, understanding the time constraints and workload we all navigate. A tool's effectiveness hinges on its simplicity and seamless integration into therapists' routines, acknowledging the reluctance to adopt anything overly complex or time-consuming.
Phase III
- Implementation Fidelity: Process to ensure a standardized procedure is utilized throughout a program.
- Drift: occurs when outside interpretations influence the consistency of how a program is delivered.
- Best-Testing: process to determine flaws or shortcomings to improve quality.
In phase three, our primary focus was on establishing implementation fidelity. This involves ensuring a standardized procedure is consistently applied throughout a program. It's about maintaining consistency in the program delivery from one client to another. The ultimate goal is to prevent drift, a common occurrence in standardized assessments where deviations may arise due to human factors or lack of manual access.
To minimize the risk of drift, I dedicated significant efforts to create and enforce implementation fidelity, a topic we'll delve into later. Additionally, phase three involved intensive data collection to assess the overall effectiveness of the program. Beta testing played a crucial role in this phase, serving as a process to identify flaws and shortcomings for quality improvement.
Like in software and other industries, beta testing was employed to work out bugs before the public release. This meticulous testing ensures that whatever is introduced functions appropriately, is user-friendly, and meets the expectations of those involved. The overarching goal is to deliver a product that works effectively and is well-received by its users.
Required Forms
- Decision-Making Framework
- Decision-Making Chart
- OBP
- Hybrid
- Occupational Identity Questionnaire
- Documentation Checklist
- Interest Checklist
- Daily Note Sheets
The core of understanding how to effectively utilize the framework lies in the required forms, anchoring back to the crucial concept of implementation fidelity. These forms serve as the embodiment of implementation fidelity, crafted to guide and meticulously document the client's progress and the therapist's perceptions. Specific details about these forms will be explored in the next section.
It's essential to note that the framework stands as a standalone entity, but I introduced the decision-making chart for seamless navigation. Two versions were created – one tailored for occupation-based practice and another for a hybrid approach. An integral component, the occupational identity questionnaire, though not my creation, is mandatory for correct framework utilization.
The documentation checklist holds significant weight, serving as a practical tool, a cheat sheet for monitoring client progress and documenting goals. The Interest Checklist, another mandatory form, acts as a springboard. Lastly, daily note sheets were incorporated for beta testing participants. These sheets served a dual purpose – facilitating real-time data collection and providing material for subsequent coding and analysis, details of which will be explored further in the upcoming discussion.
Decision-Making Framework
Figure 3 shows the framework. I had to revise it for it to translate to PowerPoint, but overall, the content is still present. The framework starts with the therapist.
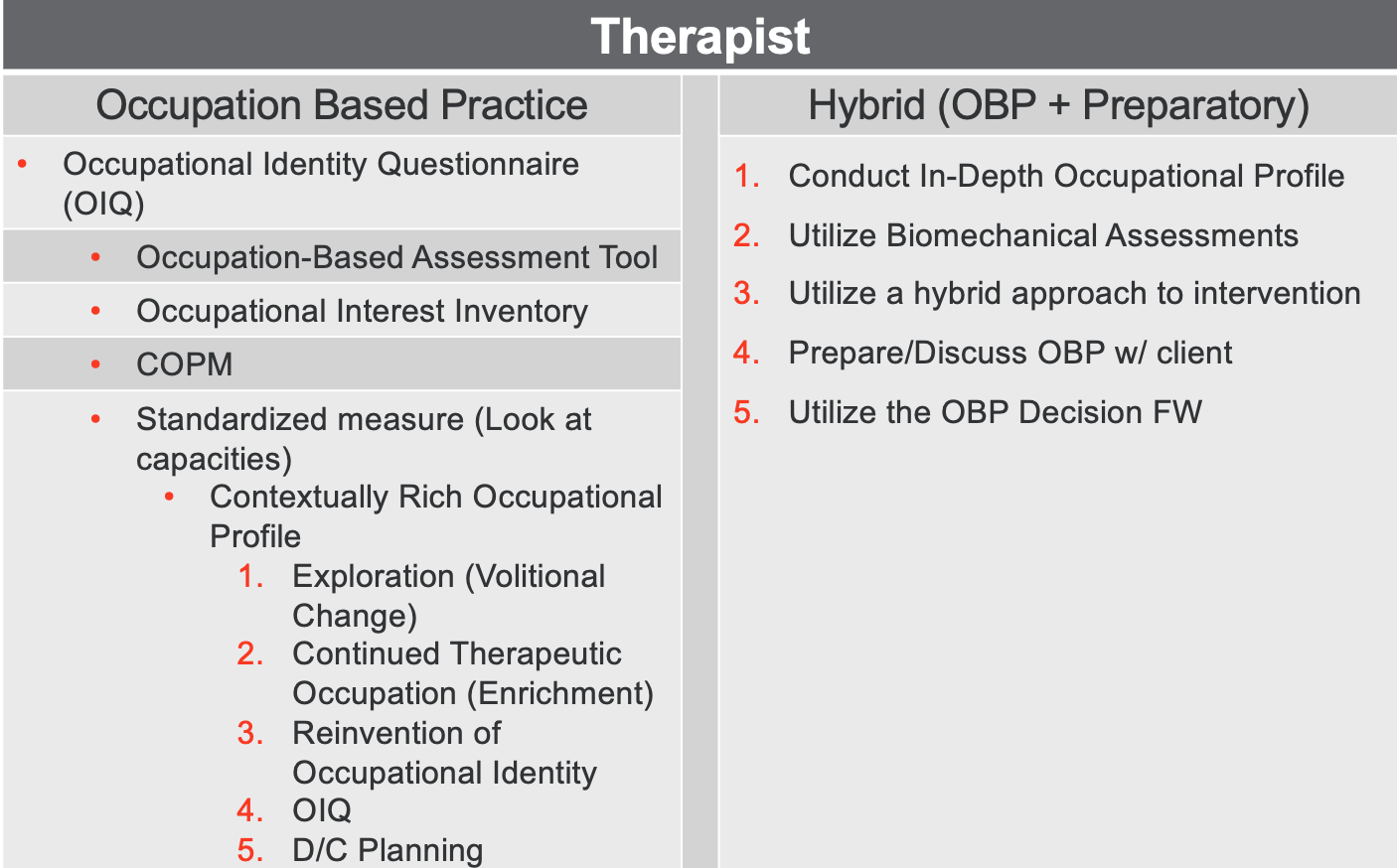
Figure 3. Decision-making framework (Click here to enlarge this image).
The initiation of the therapeutic process typically begins with the receipt of a referral, followed by a strategic decision-making process to determine the most suitable approach. This selection involves a comprehensive evaluation, considering various factors such as the client's history, medical information, and the acuity of their injury or illness. The decision between an occupation-based approach and a hybrid approach hinges on these considerations.
Upon opting for the occupation-based approach, the therapist undertakes a thorough chart review to ensure the client's appropriateness for therapy. Subsequently, the administration of the Occupational Identity Questionnaire becomes a pivotal step. Once completed, the therapist selects occupation-based assessment tools that align with the client's specific condition. The assessments are then carried out with precision and care. This meticulous approach ensures that the therapy chosen is tailored to the client's individual needs, setting the stage for a targeted and effective intervention. An overview of this process is in Figure 4.
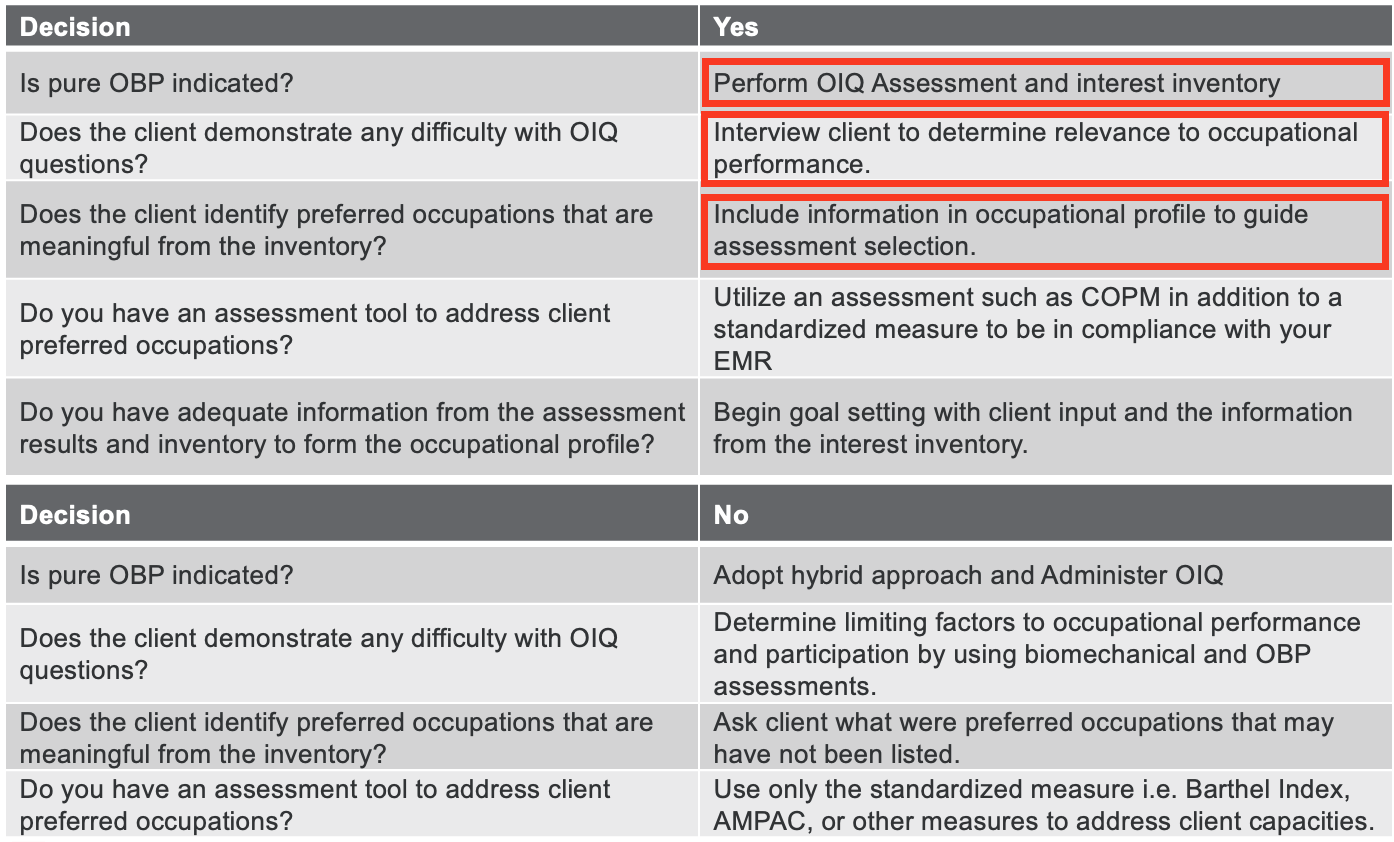
Figure 4. Chart showing the occupation-based process (Click here to enlarge this image)
The Interest Checklist takes center stage within the framework, though its detailed contents will be elaborated in the subsequent slide. This crucial tool compiles various hobbies and activities, prompting clients to rate their interests and experiences. Through this process, meaningful occupations can be identified, whether they are already significant to the client or have the potential to become so. The client's interest ratings become the basis for generating occupation-based goals, ensuring client-centered relevance within the scope of their current abilities.
For instance, if a client expresses interest in kayaking, a simulated occupation like using a Bosu ball might be implemented, aligning with the occupation-based focus while acknowledging the inherent constraints of a clinical setting.
Standardized measures required for electronic medical records are collected, typically encompassing active range of motion, pain, manual muscle testing, and GG codes. From this, a comprehensive occupational profile is crafted. This profile and The Interest Checklist become the launchpad for promoting occupational exploration. The aim is to instigate a volitional change process, influencing the client's attitudes and perceptions toward engaging in new or adapted occupations.
Throughout the framework, reassessment points are strategically embedded, allowing for goal adjustments based on the client's responses. If a particular activity fails to capture the client's interest, it may be discontinued in favor of alternatives that facilitate exploration.
Before discharge, the Occupational Identity Questionnaire (OIQ) is readministered to assess any changes or adjustments needed. Discharge planning then ensues, directing the client to the next appropriate site of care, whether home, a skilled nursing facility, inpatient rehab, or another setting.
The hybrid approach shares similarities with the occupation-based approach in its initial phases, incorporating the OIQ and occupational profile creation. However, it takes a step back from a full occupation-based focus, integrating preparatory approaches more prominently. This approach suits clients with surgical acuity, precautions, and restrictions.
Occupation-based principles are infused into the hybrid approach where feasible, resembling front-loading information to ease transitions. Therapists gradually shift towards occupation-based approaches once clients are beyond surgical precautions and can tolerate the change.
The Interest Checklist remains pivotal in this approach, serving as a springboard for the volitional change process. It facilitates conversations about meaningful occupations, past interests, and potential new pursuits. The decision-making charts act as guides and tools for implementation fidelity, ensuring therapists progress clients through indicated phases.
The Occupational Identity Questionnaire is administered for both approaches, serving as the ultimate determinant of success. It uniquely measures the client's perceived quality and sense of identity, making it a crucial metric in assessing the effectiveness of therapy. As a fluid concept, identity evolves over time, and the OIQ is specifically designed to capture this aspect.
As the framework progresses, therapists face a crucial decision— between occupation-based practice and the hybrid approach.
Occupational Identity Questionnaire
- Non-Standardized
- Likert Scale
- Completed by client
- Administered at pre and post
Here are two of the forms that are found in the framework (Figures 5 and 6).
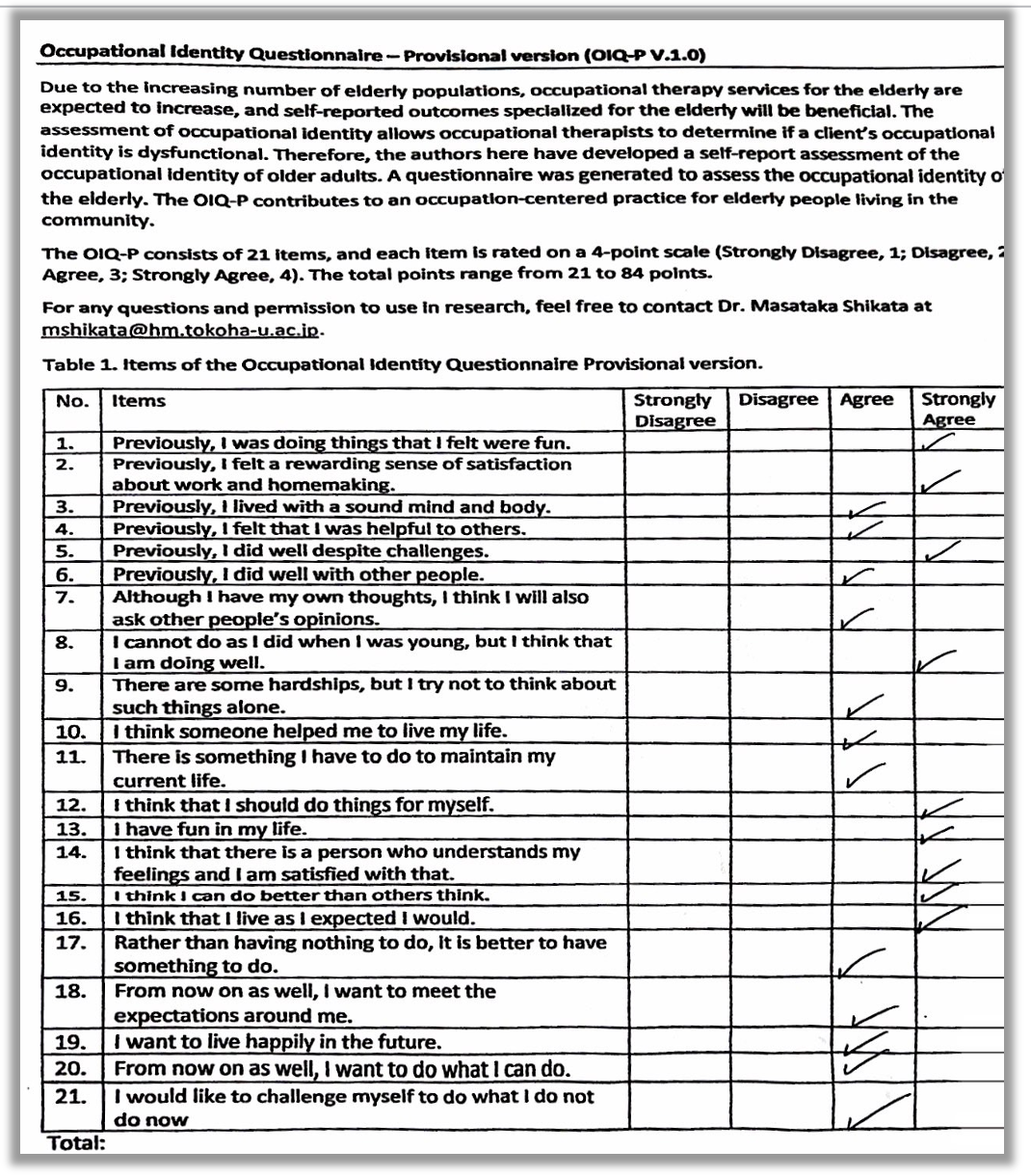
Figure 5. The Occupational Identity Questionnaire(Click here to enlarge this image).
The Occupational Identity Questionnaire (OIQ) is a non-standardized assessment within the framework. Employing a Likert scale, this client-completed questionnaire consists of 21 items, each requiring thoughtful reflection rather than immediate, instinctive responses. Given its nature, clients may need extra time to complete the questionnaire, particularly when navigating a new injury or condition.
The Likert scale ranges from one to four, with a maximum score of 84. While the OIQ isn't inherently standardized, it provides a tangible and somewhat objective measure for the purpose of the framework. For example, if a client marks eight ones, six twos, and five threes, they might receive a score of 35 out of 84. This score becomes a baseline for interventions tailored to the client's needs, focusing on specific occupations to aid in reconstructing identity. The anticipated outcome is an observable increase in the client's score by the end of the intervention.
Notably, the OIQ's creators are actively engaged in a standardization process to enhance its validity and other psychometric properties. Given its potentially time-consuming nature, administering the OIQ can be strategically integrated into the intake paperwork upon the client's arrival, ensuring minimal impact on therapists' limited evaluation time.
Despite its structured format, the OIQ offers opportunities for therapeutic engagement. If a client's responses raise concerns or require clarification, therapists can utilize the interaction to delve deeper, employing therapeutic use of self to build rapport, trust, and a sense of investment in the client's well-being. This dynamic interaction can positively influence goal development, client participation, and overall treatment consistency.
The Interest Inventory
Here is an example of The Interest Checklist, in Figure 6.
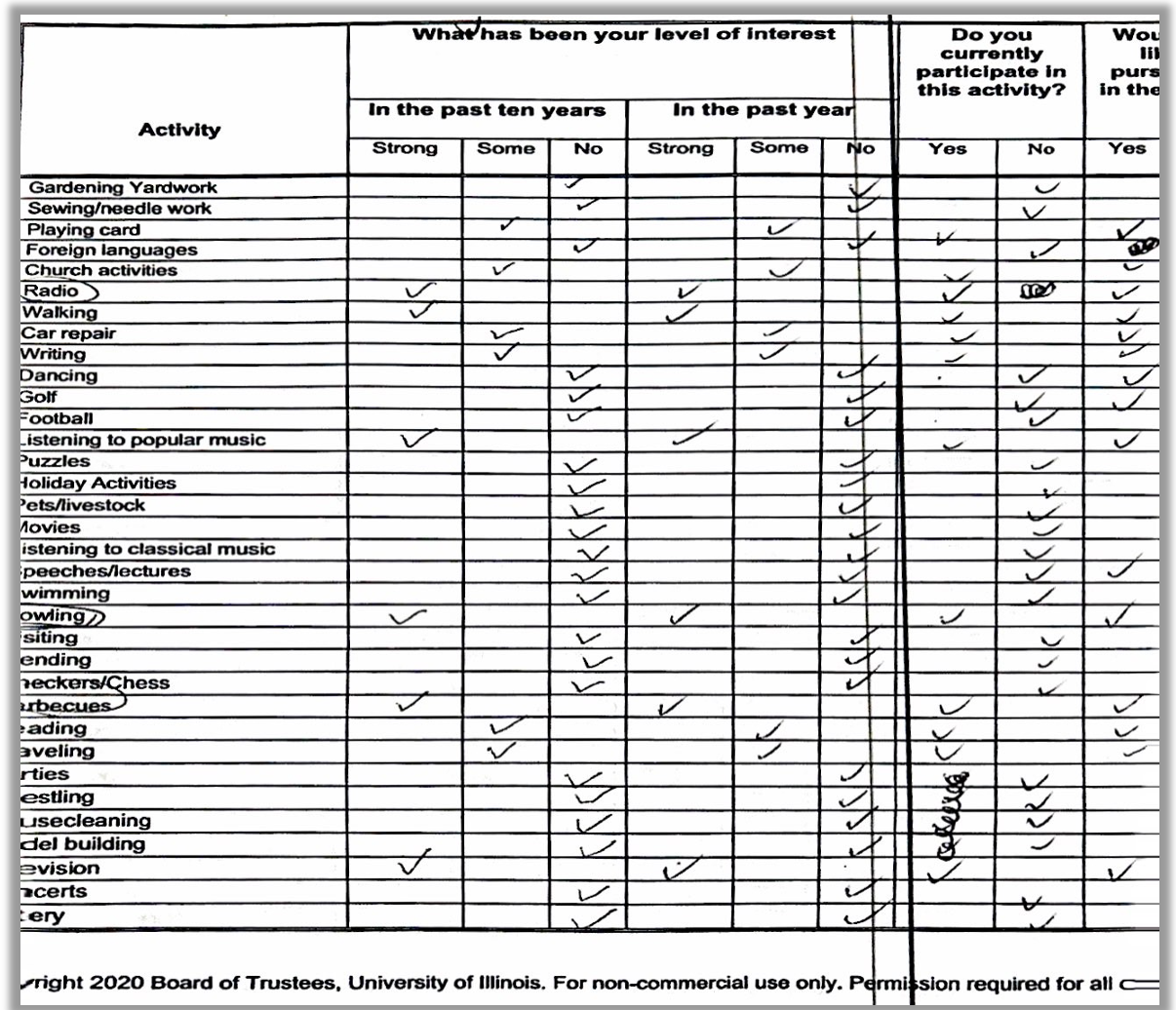
Figure 6. Screenshot of a partially completed Interest Checklist. (Click here to enlarge the image).
The Interest Checklist, about eight pages, offers clients a diverse array of options to select from. It is an invaluable tool for launching the exploration phase, providing therapists with rich insights into clients' specific activities of interest. When clients express enthusiasm or interest in a particular activity, it opens a gateway for therapists to explore potential interventions and set relevant goals, enhancing the appropriateness of the therapeutic process.
However, it's essential to acknowledge that the Interest Checklist has drawbacks, particularly its time-consuming nature. Feedback from beta-testing therapists highlighted the time-intensive aspect of this tool. This considers potential modifications, such as simplification or administration before the client arrives, enabling therapists to review it quickly rather than completing it during the evaluation.
For your reference, I've provided an example of the first half of the documentation checklist (Figure 7).
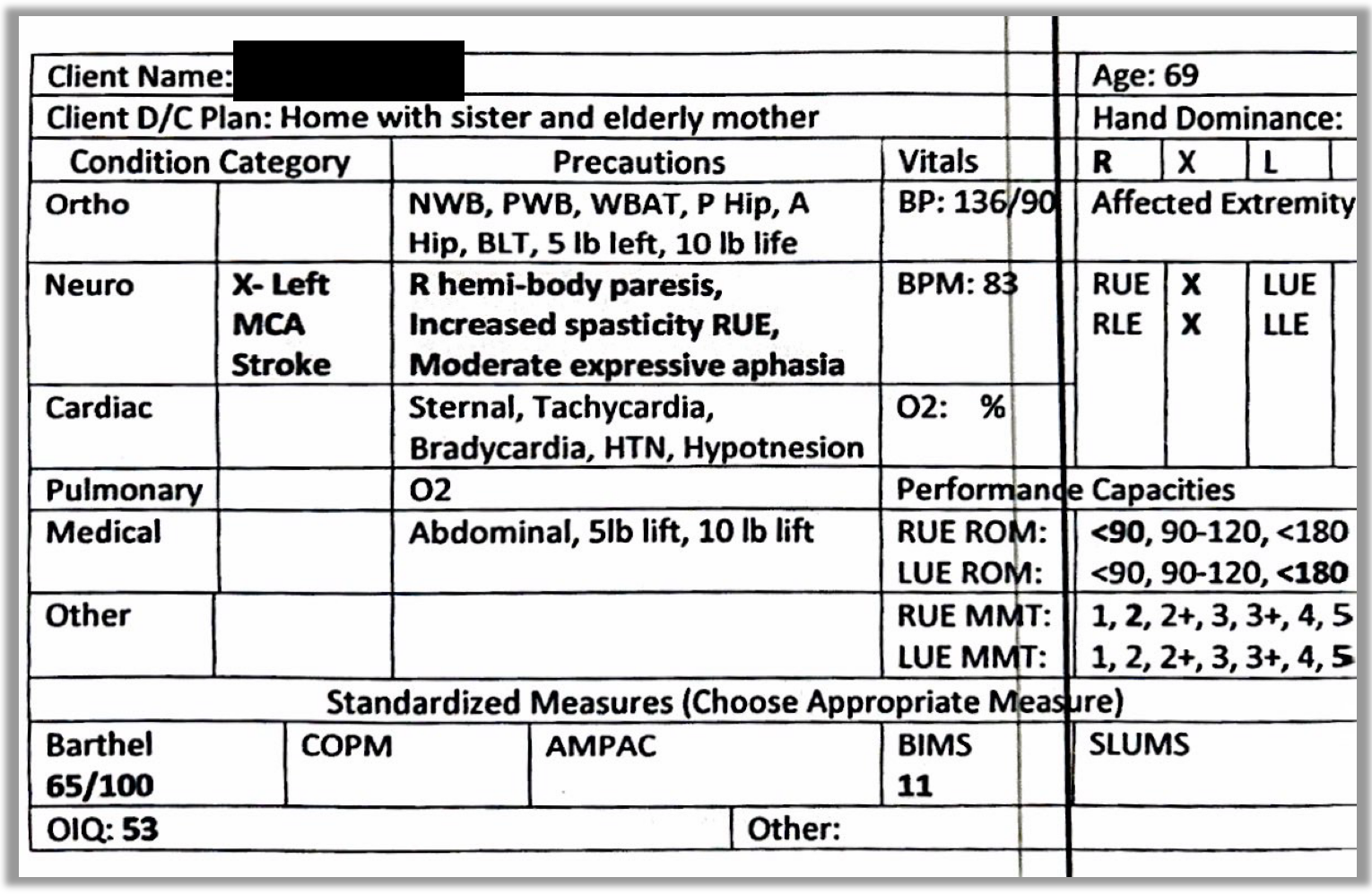
Figure 7. Part of a documentation checklist (Click here to enlarge the image).
The documentation checklist is a practical tool for therapists to record client concerns and functional abilities systematically. It incorporates examples of assessments to effectively monitor progress and track the client's therapeutic journey. Therapists can designate a desired assessment under "other" and assign a corresponding score if a desired assessment is not listed. For instance, including the BIMS as a cognitive screener helps identify potential cognitive issues, as illustrated by a client scoring 11, indicating a need for further attention or intervention.
This checklist is valuable in streamlining record-keeping, ensuring a comprehensive and organized approach to monitoring client progress and achieving therapeutic goals.
Taking a closer look at the client's condition, identified as a left MCA stroke, and considering the listed precautions—hemiparesis, increased spasticity, and moderate expressive aphasia—provides a contextual understanding. The top right corner highlights hand dominance (right-handed in this case) and the affected extremity (right upper extremity). Monitoring vitals, especially in a neuro patient with a history of stroke, is considered a prudent practice.
Performance capacities, including range of motion, offer valuable insights. While some EMRs may present range of motion in broad categories, this documentation provides specific details. For example, the therapist bolded 90, indicating that the client's right upper extremity has a range of motion under 90 degrees, contrasting with the left side, which falls within functional norms. This observation is further confirmed by bolding a score of 2 for manual muscle testing in the right upper extremity, indicating weakness. In contrast, the left upper extremity scores a 5, representing strength within norms. These nuanced details contribute to a more precise and tailored approach to client care.
This is the second half of that documentation checklist in Figure 8.
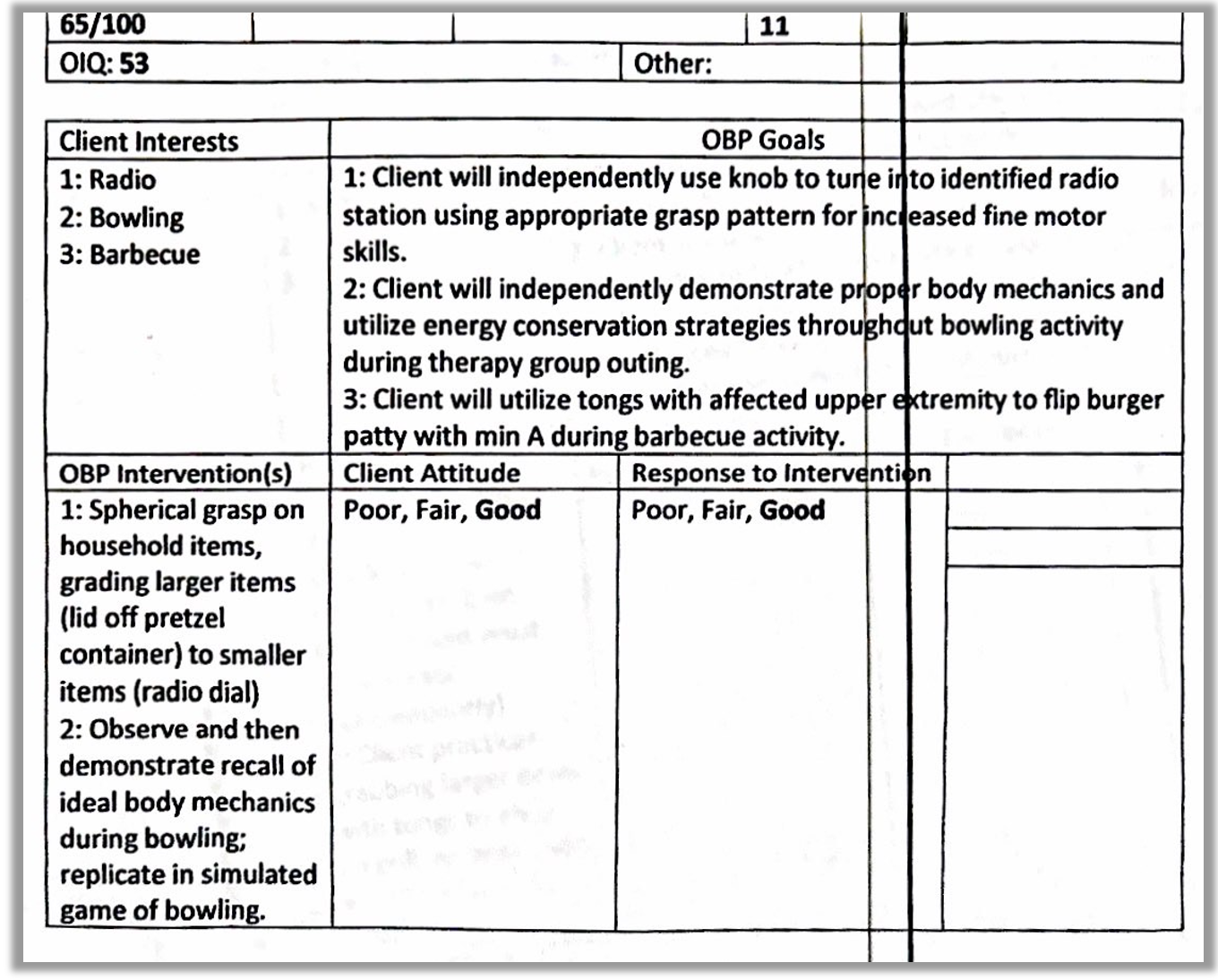
Figure 8. Second part of the documentation checklist (Click here to enlarge the image).
In this section, a comprehensive overview of the client's interests, derived from the Interest Inventory, lays the foundation for goal development. The therapist crafted three distinct goals based on the client's preferences and identified areas for improvement. These goals are intricately linked to interventions designed to address specific needs and enhance functional abilities.
The therapist formulated the following goals:
- The client will independently use a knob to tune in to the identified radio station using an appropriate grasp pattern for increased fine motor skills.
- The client will independently demonstrate proper body mechanics and utilize energy conservation strategies during a bowling activity in a therapy group outing.
- The client will utilize tongs with the affected upper extremity to flip burger patties with finesse during a barbecue.
The corresponding interventions are strategically aligned with the goals, providing a clear roadmap for implementation. For instance, to achieve the first goal, the therapist plans to work on a spherical grasp with household items, progressively grading the difficulty from larger to smaller items. This approach reflects a thoughtful progression tailored to the client's needs and abilities.
The second goal involves observing and demonstrating the recall of ideal body mechanics during bowling, followed by replication in a simulated bowling activity. While not fully authentic, this simulation falls within the middle ground of occupation-based practice, offering practicality and relevance.
This documentation serves as a reminder for therapists to align interventions with goals and provides a justification for the chosen interventions. It reinforces the importance of tailoring interventions to the client's specific goals, interests, and functional needs, enhancing the overall effectiveness of the therapeutic process.
Beta Testing
- Three therapists
- Two entry-level
- One post-professional
- Four clients
- All showed improvements in OIQ and standardized measures
- Average age: 67 years
- Race: not disclosed to PI
The beta testing phase involved three therapists, two classified as entry-level, holding master's degrees, and one with a post-professional status holding a doctorate. The testing included four clients, and across the board, all clients exhibited improvements in their Occupational Identity Questionnaire scores and standardized testing results.
The graph (Figure 9) provided illustrates the change in OIQ scores, indicated by the darker dots. An analysis of the data shows a positive correlation between increased Barthel scores and OIQ scores, suggesting a notable improvement in functional abilities and perceived occupational identity. Additionally, the percentage of occupation-based practice delivered was factored into the evaluation, highlighting the commitment to incorporating occupation-based approaches into the intervention strategies.
The positive outcomes observed in the beta testing phase underscore the potential effectiveness and impact of the framework on client progress and outcomes. It also provides valuable insights into the feasibility and applicability of the framework across various therapists and clients, spanning different levels of professional experience and education.
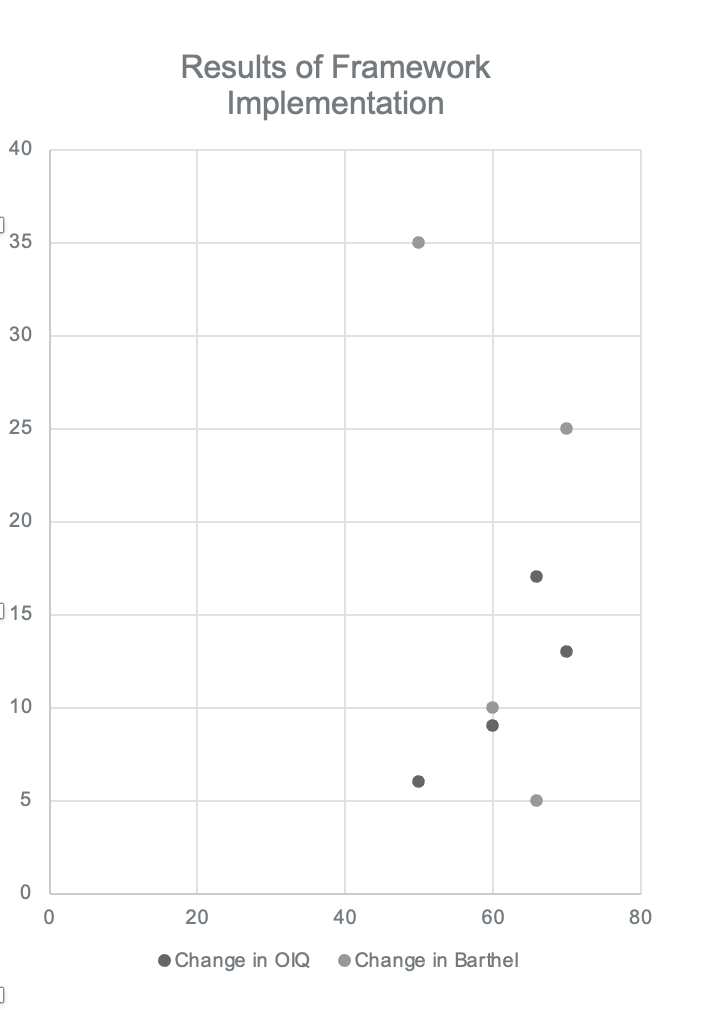
Figure 9. Scatterplot of the results of the framework implementation.
The graph depicting the relationship between the percentage of occupation-based practice and OIQ scores reveals a noteworthy trend. Generally, clients who experienced a higher percentage of occupation-based practice tended to achieve higher OIQ scores. While there is one outlier, most clients fall within a pattern suggesting a positive correlation between the extent of occupation-based interventions and improved OIQ scores. This trend aligns with expectations and reinforces the significance of incorporating occupation-based approaches into therapeutic interventions.
The beta testing involved clients with an average age of approximately 67 years old. The racial demographic was not disclosed as it was deemed irrelevant to the study. The favorable results observed in the beta testing phase, particularly the enhanced OIQ post-test scores, reinforce the positive impact of the framework on clients' perceived occupational identity.
It's worth noting that the higher the percentage of occupation-based interventions, the more substantial the increase in OIQ and Barthel Index scores. The consistent use of the Barthel Index by all participating therapists further adds to the reliability and consistency of the results, providing a comprehensive understanding of the positive outcomes associated with the framework.
- Favorable based on improved OIQ post-test scores.
- The higher percentage of OBP interventions showed increased OIQ scores.
- Therapists felt it was time-consuming.
- Needs to be more streamlined for documentation.
The beta testing phase provided valuable insights into the framework, highlighting certain areas that require refinement. One notable challenge identified by therapists was the perceived time-consuming nature of the framework, primarily attributed to the detailed documentation forms. Therapists expressed concerns about investing additional time and effort due to the need for specific forms dedicated to data collection.
Another noteworthy drawback mentioned by therapists was the duplication of documentation efforts. They reported needing to document information twice, which was seen as a potential inefficiency within the overall process. This duplication was attributed to using additional forms designed for data collection.
Additionally, the framework's reliance on specific forms was acknowledged as a practical necessity due to limitations in integrating with existing Electronic Medical Records (EMR) systems. Printing EMR records for data collection was often unfeasible due to company policies, necessitating dedicated forms. While these limitations were recognized, they also contributed to the perceived challenges faced by therapists during the beta-testing phase.
In response to this feedback, ongoing efforts are underway to streamline the documentation process within the framework. The aim is to address the identified challenges and reduce the time-consuming components, making the documentation more manageable for therapists. This reflects a commitment to continuous improvement, acknowledging that the framework is a dynamic tool subject to refinement based on practical experiences and user feedback. The goal is to enhance the framework's usability and efficiency while maintaining its effectiveness in guiding occupational therapy practices.
Case Study #1
Overview
- 76 yo F presented to SNF for skilled OT. Per EMR, Pt incurred a R Hip Fx and underwent an anterior THA. Pt presents with deficits in strength, balance, activity tolerance, and increased pain which limits her ability to perform preferred occupations and ADLs. Pt reports she was I at baseline but struggled to perform leisure occupations.
- UB Dressing: CGA
- LB Dressing: Mod A
- Bathing: Mod A
- Toileting: Min A
- OIQ: 46
- Barthel Index: 65/100
- Interest Inventory: Cooking, knitting, tennis, and water aerobics.
In this case study, a 76-year-old female has presented at a skilled nursing facility seeking skilled occupational therapy following a right hip fracture and subsequent anterior total hip arthroplasty. The patient exhibits notable deficits in strength, balance, and activity tolerance, accompanied by increased pain, which significantly hinders her ability to partake in preferred occupations and activities of daily living. Although the patient recalls being independent at baseline, the current struggle to engage in leisure occupations due to pain underscores the impact of her hip-related challenges.
Assessment of present levels reveals that the patient requires contact guard assistance for upper body dressing, moderate assistance for bathing, and minimal assistance for toileting. Baseline evaluations using the OIQ and Barthel Index provide a foundation for understanding the patient's functional status.
The patient's Interest Checklist highlights her active and diverse lifestyle, indicating a passion for cooking, knitting, tennis, and water aerobics.
Given this comprehensive profile, potential interventions could include targeted strength training, balance exercises, and pain management strategies. ADL training would focus on upper body dressing, bathing, and toileting with a gradual reduction in assistance. Leisure occupation interventions would aim to reintroduce and adapt activities such as cooking, knitting, and water aerobics to align with the patient's current capabilities.
Establishing goals for independence in ADLs, pain reduction, leisure occupation participation, and functional mobility would guide the therapeutic process. The collaboration between the therapist and patient is crucial in setting realistic goals tailored to the patient's interests, fostering a patient-centered approach to rehabilitation. The overarching objective is to address specific deficits and enhance the patient's overall independence and engagement in meaningful occupations.
OBP or Hybrid?
- OBP: Few Sx precautions, highly motivated, and active prior to injury
- OBP goals
- Pt will improve dynamic balance to good + in order to reduce risk of falls during dynamic movement tasks.
- Pt will independently complete a cooking activity in standing.
Considering the patient's profile—a 76-year-old woman recovering from a right hip fracture and anterior total hip arthroplasty—I lean towards adopting an occupation-based approach for her rehabilitation. The presence of only a few surgical precautions, coupled with her high motivation and active pre-injury lifestyle, aligns well with the principles of occupation-based practice.
An occupation-based approach seems suitable, allowing for a more direct, personalized intervention emphasizing meaningful and purposeful activities. This approach resonates with the patient's prior routines and interests, contributing to a more engaging therapeutic process.
Goals centered on improving dynamic balance and achieving independence in standing activities are in harmony with the occupation-based approach. By tailoring interventions to the patient's specific interests and prior activities, we can create a rehabilitation plan that not only addresses her physical deficits but also promotes a sense of purpose and engagement in her recovery journey.
OBP Interventions
- Tennis Game
- Dynamic balance, activity tolerance, coordination, and functional reaching
- Cooking Task
- Energy conservation, adaptive strategies, task simplification
In crafting interventions for this client, we can consider her specific interests highlighted in the inventory. One potential intervention involves introducing a simplified tennis game to address dynamic balance, activity tolerance, standing balance, coordination, and functional reaching. By incorporating elements of her favorite sport, we create a familiar and engaging context for rehabilitation, gradually adapting the game to her current capabilities while progressively challenging her balance and coordination.
Another targeted intervention revolves around a cooking activity, emphasizing energy conservation, adaptive strategies, and task simplification to promote independence. Recognizing the client's keen interest in cooking, this intervention seamlessly integrates functional tasks into her rehabilitation. Techniques such as task simplification and adaptive strategies will be employed to ensure success and build confidence in daily activities.
Case Study/D/C Planning
- Repeat all standardized measures.
- OIQ improved by 10 pts.
- Barthel Index increased 25 pts.
- All goals met.
- Pt D/C home.
In the subsequent phase, following the tailored interventions based on the client's interests, we reassess standardized measures. Combining standardized measures with occupation-based interventions, this holistic approach reveals positive outcomes for our clients.
The Occupational Identity Questionnaire (OIQ) demonstrates significant improvement, reflecting a ten-point increase. This positively impacts the client's perceived quality and sense of identity, highlighting the effectiveness of the occupation-based approach in addressing her specific needs and interests.
Moreover, the Barthel Index, another valuable standardized measure, shows remarkable progress with a 25-point increase. This improvement signifies enhanced independence in various activities of daily living, reinforcing the positive outcomes achieved through the comprehensive rehabilitation plan.
A noteworthy achievement in this case is the successful discharge of the patient to her home. The attainment of all set goals speaks to the efficacy of the tailored interventions and the client-centered approach employed throughout the rehabilitation process. This outcome not only signifies physical progress but also underscores the restoration of independence and functionality for the client in her home environment.
In summary, the combination of standardized measures and occupation-based interventions has proven instrumental in achieving positive outcomes, as evidenced by improvements in both the OIQ and Barthel Index. The ultimate goal of supporting the client's return to her home environment has been realized through the collaborative efforts of the therapeutic team.
Case Study #2
Overview
- 67 yo M presents to OP with flexor tendon repair in dorsal blocking splint. Pt is three weeks post op and is still limited with ROM and has stringent splinting schedule.
- UB Dress: Min A-T-shirt/Max A buttons
- LB Dress: Min A
- Shoes: Max A
- Decreased sensation
- Edema
- Pain
Case study number two is a 67-year-old male with a flexor tendon repair and a dorsal blocking splint. The therapeutic approach would need to be strategic and cautious due to the ongoing limitations in range of motion and the stringent splinting schedule.
Considering the limitations in range of motion and the need for careful management of the splinting schedule, a hybrid approach provides the flexibility to incorporate preparatory exercises that focus on maintaining joint mobility, managing pain, and addressing sensory changes. These preparatory activities can lay the foundation for future occupation-based interventions as the client progresses in his recovery.
OBP or Hybrid?
- OIQ Score: 37
- Barthel: 40/100
- Interest Inventory
- Poker
- Kayaking
- Mechanics
- Crochet
Hybrid Approach
- Edema Management
- Operating ROM within protocol
- Pain Management
- Single hand shoe tying
- Adaptive equipment for dressing
Adopting a hybrid approach aligns well with the client's needs and the postoperative considerations. The initial Occupational Identity Questionnaire score of 37 and a Barthel Index of 40 indicate a significant impairment, reinforcing the need for a careful and multifaceted therapeutic approach.
Considering the client's interests in poker, kayaking, mechanics, and crochet, we can integrate occupation-based alternatives within the hybrid approach. While prioritizing edema management, range of motion within protocol constraints, and pain management, the therapeutic plan can include tailored activities that resonate with the client's hobbies and preferences.
Occupation-based interventions such as single-handed shoe tying and adaptive equipment for dressing align with the client's specific needs and contribute to a holistic rehabilitation plan. These activities not only address functional goals but also resonate with the client's personal interests, fostering engagement and motivation throughout the recovery process.
As the client progresses in his rehabilitation, the therapeutic focus can gradually shift towards more occupation-based activities related to his interests, ensuring a balanced and patient-centered approach.
Goals
The goals encompass a holistic approach to the client's rehabilitation:
1. Implement a progressive upper body strengthening program.
2. Facilitate an increase in active range of motion.
3. Achieve dressing independence for lower body dressing with appropriate equipment.
4. Foster one-handed crochet as an occupation-based goal.
5. Enhance independence in buttoning activities.
6. Incorporate scar management techniques, such as scar massage.
7. Work on improving overall coordination.
8. Integrate assistive technology, like a card shuffler.
9. Ensure adherence to the splinting protocol.
These goals collectively address the client's physical and functional needs, incorporating meaningful activities and prioritizing engagement throughout rehabilitation.
Next Phase
- The client is no longer in the splint.
- OT is still indicated.
- Adopt the OBP approach moving forward.
In this phase of the framework, let's consider a hypothetical scenario where the client has successfully achieved the initial goals or is no longer constrained by the splint. While some residual issues persist, they may not be significant enough to warrant continued adherence to precautionary measures. This marks a crucial juncture where a full occupation-based approach becomes feasible.
Now, with the removal of the splint and diminished concerns over precautions, the occupational therapist has the freedom to delve into the client's previously identified interests—poker, kayaking, mechanics, and crochet. The occupation-based practice can be fully embraced, allowing for a more personalized and client-centered therapeutic approach. This transition signifies a shift towards holistic interventions that directly align with the client's meaningful activities and preferences, fostering a deeper engagement in rehabilitation.
D/C Planning
- Increased OIQ to 50
- Barthel Index 100/100
- Pain 1/10
- Edema WFL
- AROM WFL
As we progress, let's revisit the Occupational Identity Questionnaire with our hypothetical client. By reassessing the OIQ, we aim to gauge the impact on his identity and perception of self throughout the intervention. In this follow-up, his OIQ has improved to 50, reflecting positive changes in his perceived quality and sense of identity. Notably, he has achieved complete independence in activities of daily living and functional transfers. He reports minimal pain (one out of ten), edema, and active range of motion have returned to normal.
These outcomes suggest a successful occupational therapy intervention that not only restored functional abilities but also addressed the intrinsic aspects of identity. By incorporating his interests and preferences into the rehabilitation process, we fostered a more holistic and client-centered approach, as evidenced by the positive changes in the OIQ scores. This measurement tool is a valuable guide, enabling us to assess and enhance the client's sense of self throughout the therapeutic journey.
Summary
As we conclude, I want to express my gratitude for your participation in this session. Let's revisit the learning outcomes to reinforce what we've covered. Following this course, participants should be adept at identifying potential clients suitable for applying the framework. By recognizing opportunities to adapt treatment approaches, incorporating occupational identity becomes a seamless and integral part of client-centered care. Finally, you should now be equipped to list the strategies and required documents essential for successfully executing the framework when working with older adult clients. Thank you once again for your engagement.
Exam Poll
Question 1: What is occupational identity?
a. It's a practice methodology where the occupational therapist utilizes occupation
b. It is where the occupational therapy practitioner utilizes biomechanical, rehabilitative approaches
c. It is a sense of self derived from the occupation clients engage in daily
d. None of the above
Correct Answer: c. It is a sense of self derived from the occupation clients engage in daily.
Explanation: Occupational identity is the client's sense of self from engaging in daily occupations. It's not a practice methodology (a), nor is it focused on biomechanical approaches (b).
Question 2: What does the Model of Human Occupation (MOHO) address?
a. Volition
b. Habituation
c. Performance patterns
d. All of the above
Correct Answer: d. All of the above
Explanation: MOHO addresses volition (a), habituation (b), and performance patterns (c). It encompasses all these aspects.
Question 3: What is a true statement about the results of the author's studies?
a. Interviewees expressed their experience with occupational therapy was client-centered.
b. It showed a heavy reliance on preparatory approaches.
c. Interviewees expressed their experience with occupational therapy did encompass their occupational identity.
d. It only asks multiple-choice questions.
Correct Answer: b. It showed a heavy reliance on preparatory approaches.
Explanation: The study found that occupational therapists heavily relied on preparatory approaches (b), and clients felt their needs were not entirely client-centered.
Question 4: The Occupational Identity Questionnaire is...
a. Non-standardized
b. A Likert scale
c. Completed by the client
d. All of the above
Correct Answer: d. All of the above
Explanation: The OIQ is non-standardized (a), uses a Likert scale (b), and is completed by the client (c).
Question 5: In the case study, the client utilized a tennis game to work on all of the following except:
a. Dynamic balance
b. Coordination
c. Task simplification
d. Functional reaching
Correct Answer: c. Task simplification
Explanation: The client utilized a tennis game to address dynamic balance (a), coordination (b), and functional reaching (d), but not specifically task simplification (c).
Questions and Answers
I find that the majority of my clients are so low functioning that all OT goals are very basic like dressing, bathing, and toileting. I do not believe these goals that clients identify with regarding enjoyable part of life. How do you recommend enhancing client engagement in such mundane daily tasks?
I would recommend using that Interest Checklist to find meaningful or fun things. Do they have things that they enjoyed at some point in time? Something else that you may want to consider is interdisciplinary collaboration. For example, you might want to utilize the nursing staff to help you get them up so that you don't spend all your time with them and can explore other things.
I am finding the therapeutic exercise code being phased out by my management company. Is this common to multiple areas or just local to me? I believe it may be due to lower reimbursement. I relate exercise to strengthening, which is necessary for many clients. Am I correct?
Yes, therapeutic exercise is a lower reimbursement code in most places, and many companies are phasing it out. Keep in mind that we need to be using occupation as our intervention. I'm going to give the example of carrying a laundry basket. You can put ankle weights in the basket. You can do many different things to incorporate that strengthening piece, but it is still a functional activity. Then adding functional mobility adds another layer of complexity.
When do you use the OIQ?
It depends on when that disruption started. It's never a bad idea to start asking. "Based on your OIQ score, when did you start feeling this way? Can you give me some backstory on how that process started?" This may be your best jumping-off point because occupational disruption is unnecessary. There's no finite definition of how long a disruption occurs until it's a full-blown deprivation. The identity piece is very fluid and flexible from person to person.
References
See additional handout.
Citation
Pitts, A. (2024). The reinvention of occupational identity: A decision-making approach. OccupationalTherapy.com, Article 5690. Available at www.occupationaltherapy.com
