Anjali: Thank you, everyone, for showing up for this talk. I am currently a mommy of a newborn, and I am very excited about this topic.
Being an OT and a new mother, I found it a very interesting experience. I was able to use my OT mind when I was struggling with self-diagnosed stress. I have also seen it in my female colleagues, friends, and family members, and I really think that we need to advocate for what we can do for these mothers. How many of you are a mom or know of a mom who has been diagnosed with postpartum depression, or if not diagnosed, you definitely think there is some symptomatology going on? Thanks for taking that poll (live course)- the majority of you have answered "yes."
PPD and the DSM
Postpartum depression (PPD) is now listed as perinatal depression in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), but postpartum anxiety is not included. My sister is a psychiatrist, and she said postpartum anxiety is still not in the DSM. We know that this is a condition, but medically, it is not defined in the DSM. We all have heard about postpartum depression, but less is known or talked about postpartum anxiety.
I can admit that I have probably been dealing with anxiety. As mothers, we try to do it all, and this creates a lot of pressure. I think this is important to know that a client could be dealing with either depression or anxiety, or both. Back in 2012 when I had my first child, the seed was planted about this topic, and I started really trying to figure this out.
The Difference in Depression Types
From my research, I found a comparison of the postpartum brain versus the brain of someone that has a major depressive disorder or general anxiety disorder (Figure 1).
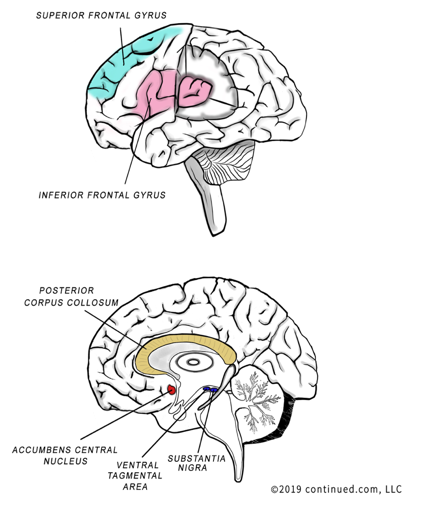
Figure 1. Brain areas affected by depression.
I am no neuroanatomist, but I did find in my research five unique areas that are affected in the postpartum brain and not in general depression. This information tells us that this is really something going on neurologically, and it is not just hormones, behavior, or attention-seeking. I am going to talk a little bit about those areas in a minute. But, I want to give you a quick neuro lesson first.
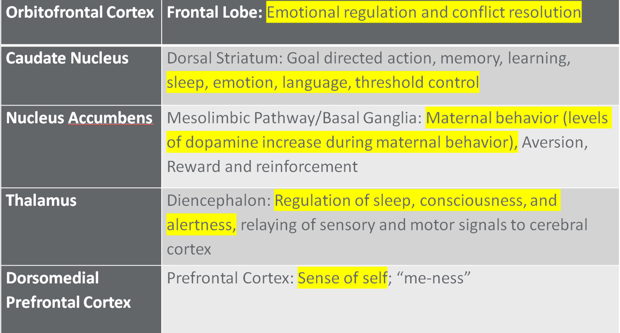
Figure 2. Brain areas defined.
The caudate nucleus manages sleep emotion, language, threshold control. The nucleus accumbens regulates maternal behavior. The levels of dopamine increase during maternal behavior so that is also being affected. The thalamus regulates sleep, consciousness, and alertness. I think everyone knows that a new mother does not sleep like she once used to. The dorsomedial prefrontal cortex is your sense of self or the sense of "me-ness." This is how many of us feel after we have had a baby. All of our attention is going toward that child and not to ourselves so we lose our sense of self a little bit.
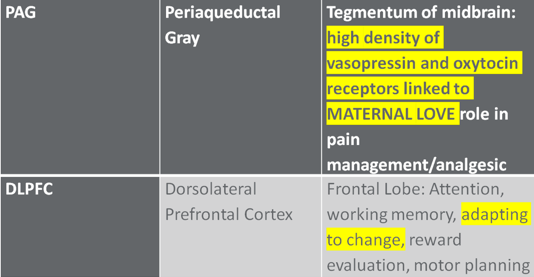
Figure 3. More brain areas defined.
The periaqueductal gray has a high density of vasopressin and oxytocin receptors that are actually linked to maternal love, and I found that very interesting. I am interested to continue to research and see if the same is for the father. We also hear about the poor outcomes from postpartum depression which sometimes can result in something happening to the child. The dorsal lateral prefrontal cortex helps a person adapt to change, and that is also affected.
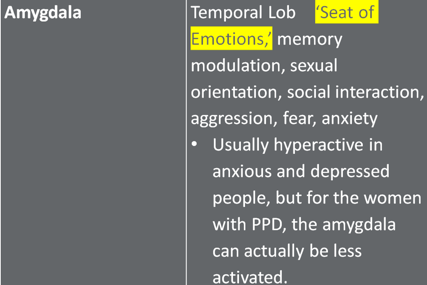
Figure 5. The amygdala.
The amygdala is the seat of our emotions.
Deciphering the Differences
Now, let's decipher the unique differences. I am going to show the brain again so that we can look at a few things.
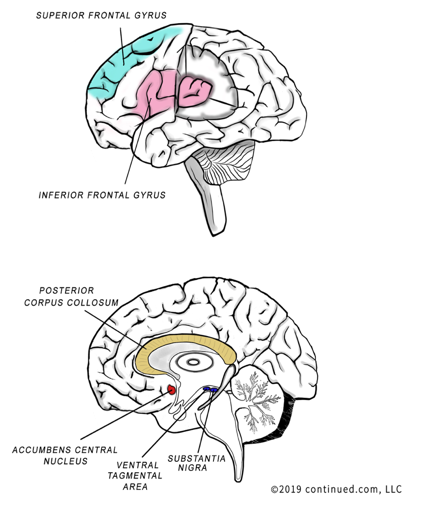
Figure 6. Brain areas affected by depression.
The superior frontal gyrus is in blue, and the inferior frontal gyrus is in pink. In the bottom image, the posterior corpus callosum is yellow, and the ventral tegmental area is dark purple.
In the following charts, here is a key:
- Blue highlighted areas indicate unique activity occurring during PDD as compared to major depression (MDD) and generalized anxiety disorder (GAD)
- Yellow highlighted areas indicate functional neurological responses hindered by PPD and ultimately hindering a mother’s occupational and role satisfaction during the post-partum period
Figure 7 shows an overview of the superior and inferior frontal gyruses.
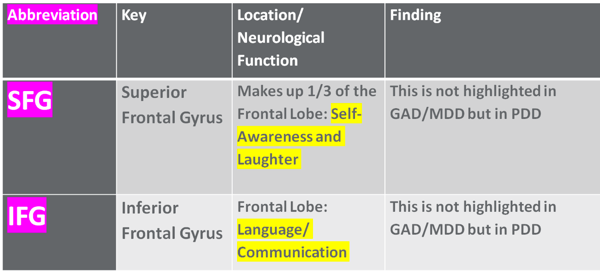
Figure 7. Findings for the superior frontal gyrus and inferior frontal gyrus.
The superior frontal gyrus is in charge of self-awareness and laughter. As an example, I ran into a friend in the Target parking lot. She had just had a baby, and she had a flat affect. She did not look the same at all. I told her husband, "You need to find out what makes her laugh." He replied, "Well, it's a good thing that I'm funny." It is the little things like that. We need to help our clients to find what they enjoyed and laughed about. This can be an intervention.
The next area is the inferior frontal gyrus that controls language and communication. If a mother becomes withdrawn and does not want to talk much, this area can be affected in the postpartum brain. Figure 8 shows an overview of the accumbens central nucleus (ACC).
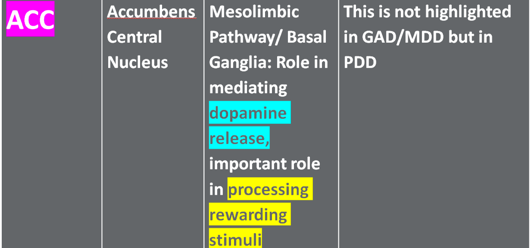
Figure 8. Findings for the accumbens central nucleus.
We all know that dopamine is important for processing rewarding stimuli. That is already being affected, so neurologically, postpartum women are really not that happy. Dopamine release is being affected. If we are assessing behavior, we should also be sensitive to the fact that the neurotransmitters are also altered.
The posterior corpus callosum is shown in Figure 9.
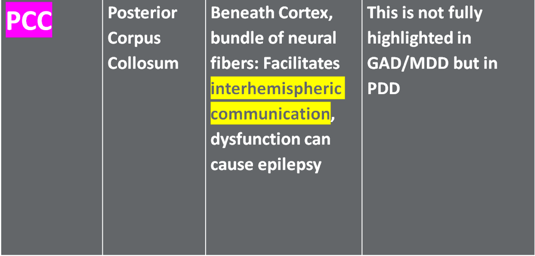
Figure 9. Findings for the posterior corpus collosum.
I think we all know that the corpus callosum controls interhemispheric communication. If that is affected, communication or processing may be impaired. You also have to consider that the client is not sleeping very well.
Finally, the VTA or the ventral tegmental area is seen in Figure 10.
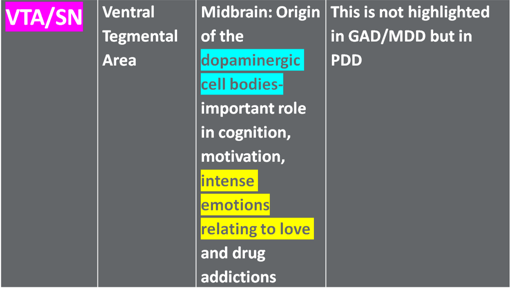
Figure 10. Findings for the ventral tegmental area.
This area is where the dopaminergic cell bodies originate, and this plays a role in intense emotions related to love. It is all connected to drug addiction. These are changes in the neurotransmitters.
Weaker Connectivity: "Mom Brain"
We have all heard about "mommy's brain." There is some weaker brain connectivity in women with PPD versus those who are not depressed postpartum. Weaker connections have been found between the anterior cingulate cortex, the dorsal lateral prefrontal cortex, and the hippocampus in depressed postpartum women. The hippocampus is what controls memory, so if that is affected, I guess "mom brain" could be a thing.
Behavioral Neuroscience
As I was looking through this, neuroscientists have researched this area quite a bit. I hate to read off the slide, but I think this is an important quote.
“When we talk about the neurobiology of postpartum depression and anxiety, our information from the studies done on humans is only comprised of about 20 papers. If you think that 10%-20% of women during pregnancy and the postpartum period will suffer from depression and/or anxiety, and then you realize there are only 20 publications looking at the neurobiology of these illnesses, it’s quite shocking.”- Pawluski, 2017
When I looked at the neurobiology of postpartum depression and anxiety, the studies done on humans only comprised about 20 papers. When you think that only 10 to 20% of women during pregnancy and the postpartum period suffer from depression and/or anxiety, and then you realize there are only 20 publications looking at the neurobiology, it is quite shocking. There needs to be a little bit more done on this topic.
Why OT?
Now that we know a little bit about the neuroanatomy and the implications neurologically of what is going on, what does this have to do with occupational therapy? We have psychiatrists diagnosing it. Others on the team include nurses and psychologists. There are also medications available. However, what if the mom does not want to take medications. For example, if she is nursing or prefers not to take meds, an OT might be able to help. PPD plays a key role in a new mother’s satisfaction/dissatisfaction of her occupational performance due to many variables, i.e. pressures to breastfeed, family dynamics, change in hormone levels in the woman, difficulty with ADL/IADL, difficulty with relationships, and difficulty with maintaining a sleep and rest schedule.
From the beginning, there is a lot of pressure, even in the hospital. How many wet diapers? Are they hydrated? Do they have jaundice? The only way to cure jaundice is for them to be hydrated. Now, if the mom is not producing milk right away, she may need to give the child formula. I have seen so many mothers freak out about this because "a good mother" provides for the child. That is huge stress the first day they are in the hospital. The lactation consultants are pro-breastfeeding, and as educated and knowledgeable as they are on the importance of that, it does create some stress and pressure on the mom who is just trying to heal and bond with her child. As if delivering the child was not enough work, now they have to make sure that they are eating well and are hydrated so they can provide for their child.
As OTs, we are skilled in OTs in feeding, coping strategies, pacing, routine adaptation, and all sorts of caregiver education techniques. The list is endless. A new mother or a potential client is integral to the growth of the child both physically and emotionally. As stated, there are lots of demands and processing involved. We need to make sure that our client is able to handle all of the demands. For example, feeding every two to three hours is a huge demand. It supports bonding and emotional attachment and meets the ADL needs of both the baby and the mother, but it causes a lack of sleep.
Another thing to consider is the support system. Does the mom have a lot of support? Are there family members around who can provide meals, who can make sure that the mother is hydrated, and who can care for the baby and help out? Babies that have medical issues or are premature add to this already stressful situation. Even when there is discharge to home, a nurse or a doctor may still be overseeing the case of the baby. The baby might be all taken care of medically, but what about the mom who now has this child in her home? Has anyone checked in on the mom? What was the normal routine before all of this? How can OT help her to get adjusted? What is the client's support system? I think all of this is very important. I know in other countries there is a lot of postpartum maternal care. In Europe, for example, they send a midwife to the home and to assess the mother. I feel like in this country, that is something we can certainly mirror if at all possible.
Now that we better understand the symptoms of postpartum, know that it is neurologically-based, and is not a simple perceived hormonal behavior, are we more likely to understand the value of our intervention? Many of you are saying, "Yes!" It is taking this knowledge and putting it into practice. Some of the other comments coming in are:
- We can look at the individual needs and interest of the mom to spur laughter and engagement.
- We are certainly important as long as the person, the mother, knows that there is some sort of an issue. That is a really good point, and I am glad you mentioned that. We, as OTs, are very self-aware and we study behavior all the time. But if you have no idea that you are depressed or anxious, how can anyone help you? We may need to approach them in a very sensitive way or speak to caregivers.
OT-Strategies
We need to start with an OT evaluation. Two good ones are the Canadian Occupational Performance Measure and the AOTA Occupational Profile Template, and that is on the AOTA website. If you have not used the COPM or the Occupational Profile in some time, I am going to refresh your memory by reading off a few areas that are very OT. First, we need to know the reason the client is seeking the service. Occupations where the client is successful, personal interest and values, an occupational history, and performance patterns are all important information. Routines, roles, habits, and rituals are other areas. We should also look at the physical and environmental sides of things like furniture, pets, spouse, friends, and caregivers. Looking at customs and beliefs are also crucial. If the mother is getting a lot of pressure from your family on why you are doing something a particular way, the therapist may need to help her navigate that. This can include questions such as:
- Why are you waking your child to feed them? We did not do it that way when we were parents.
- Why are you not nursing more? Or, why are you nursing? What about a bottle?
- Why do you believe in a pacifier?
Many people have opinions on how a woman should be raising their child, especially a newborn because they are helpless and everybody wants to help. However, this can be a huge stressor.
Other personal factors such as age, socioeconomic status, and education can be great information to gather. What stage of life are they in? You also need to look at your client's priorities and desired targeted outcomes. Much of this information is coming straight from the AOTA website. What were their life experiences? Who were they before this transition? Just like we would speak to our clients post-injury, motherhood is a transition. Together with the new mother or the spouse and caregiver, we can identify problem areas and include that as an assessment measure in your evaluation. Again, both the COPM and the Occupational Profile are great guides. The mother should score herself on key areas for both pre and post-partum. What was her occupation? Was she working? Does she plan to return to work? All of those things are really important to understand. Has she ever been a mother before? Does she plan to have more children? Is this a very unnatural experience for her? Is she having a hard time bonding? Are there any other marital stresses or frustrations going on that we need to be aware of that should would be willing to disclose?
We should gather information about the delivery and any post-trauma or healing issues. Many times, the delivery experience is not what the mother thought it would be. They can have a plan, but things might not go according to plan. There can also be some PTSD going on. Is she able to get in and out of bed? On and off the commode? In and out of the shower? Just like we would assess post-hip fracture or surgical intervention, we need to do the same with postpartum women. We can help her to establish an updated ADL and IADL routine so she feels successful and has that sense of "me-ness."
