Editor’s note: This text-based course is a transcript of the webinar, School-Based Occupational Therapy and Student Mental Health: Are We Helping?, by Moni Keen, OTD, OTR/L.
Learning Outcomes
- After this course, participants will be able to recognize the causes of mental health issues among our students.
- After this course, participants will be able to identify some mental health diagnoses of school-aged children and youth.
After this course, participants will be able to list facts regarding occupational therapy’s ability to address mental health needs among students.
Introduction
Hello everyone. I am very excited that you decided to give me some of your time today to learn about school-based OT and mental health. Mental health is a very important topic to me. I am very passionate about mental health, and it can play a much more significant role in our practice, whether we are school-based, inpatient, or outpatient. We have the opportunity and the privilege to address our clients' mental health needs in each therapy session.
Also, throughout this presentation, I am going to be using examples from my practice. I have been in school-based practice for over 25 years. I have learned to apply a lot of this knowledge. I can tell you that school today is certainly not what it was back when we went to school, whether you are working in special education or regular-ed. Today, our children have significant mental health concerns and are dealing with issues that even adults find very difficult to handle. We need to be that foundation of support for our clients, especially our little ones.
Concerns
- Significant increase in mental health issues among students (Blackman et al., 2016)
- Lacking the manpower to address mental health needs (Chan et al., 2017)
- Lack of resources for intervention (Capp, 2015; Chan et al., 2017; Moon et al., 2017)
- Occupational therapy is not viewed as a team member of mental health (Ball, 2018)
One of the concerns that we want to look at today is the significant increase in mental health issues among our students. Please remember that the statistics that I will be sharing with you today come from my capstone project, which I completed in 2019. We know that these values have probably increased rather significantly, simply because of COVID. Let's bear that in mind today.
There has been a significant increase in mental health issues among our students. Sadly, there is a lack of manpower available within our public and private education systems to handle these mental health issues and needs. There is a lack of resources in our schools to help these teachers, administrators, and children.
Lastly, occupational therapy is not viewed as a member of the interprofessional mental health team. I think we should be concerned about this. We know that our roots started in mental health practice. As we go through this presentation, let's think about what we can do to find that disconnect and correct it.
Facts
- School-aged children are dealing with significant mental health issues
- Impacting their occupation of the student
- Guidance counselors, school psychologists, and administration are addressing students’ mental health needs
- Are they prepared?
- Where is occupational therapy?
(Chan et al., 2017)
Here are some facts. School-aged children are dealing with significant mental health issues today. We know that our job as occupational therapists is to help our clients to engage in whatever their occupation is. And, a child's occupation in school is a student. A child may have a big test after witnessing domestic abuse or not sleeping well the night before. These are examples of the many issues that impact our students' ability to engage that role of student for that very day. The repercussions can last for some time.
Guidance counselors, school psychologists, and administrators currently address students' mental health needs. In my schools, the assistant principal's number one job is not to support teachers but to assess and take care of the behavior problems within the school. The majority of his day is writing up referrals for behavior within the school or on the bus. It is also suspending and expelling kids from school. This change in roles concerns me. A considerable part of their role should be to support teachers as well. School psychologists have the tools and resources to address these behavior needs, but they are also busy doing testing and holding meetings. Lastly, guidance counselors are meeting with classes and performing one-on-one counseling.
Where is occupational therapy? We should play a part with those other team members to help take some of the pressure off of them.
- Occupational therapists are qualified to work in mental health yet are underutilized in many cases.
- Where is the disconnect?
- How can occupational therapy become part of this interprofessional team?
- Social-Emotional Learning curriculum
(Chan et al., 2017)
Occupational therapists are qualified to work in mental health, yet we are underutilized. Where is that disconnect? In a few slides to come, I will show you the simple study that I did for my capstone project. I am also going to go over the results of the survey that I conducted. I hope that it opens your eyes as much as it did mine. I was hoping to get something a lot more positive, but it was very eye-opening.
What can we do as a profession and as a member of the team in school-based practice? What do we need to do to become part of the interprofessional team? One thing is that we can become familiar with and even certified in the social-emotional learning curriculum. We are going to go over two of those today. One is the Zones of Regulation, and the other, which is relatively new, is called Powerfully You.
A Few Statistics
- 20% of students have a diagnosable mental illness (Blackman et al., 2016)
- 21% increase between 6-18 years of age (Arensen et al., 2019)
- 50% of students are receiving intervention (Moon et al., 2017)
- 75% are receiving inadequate intervention or no intervention (Capp, 2015)
Here are some of the statistics that I found as I was doing my research in 2019. Again, let's remember COVID before looking at this. When we look at the different states and school districts, everyone handled COVID differently. Some of our schools went back face to face very quickly, while other schools and districts, like mine, did a hybrid model for a very long time. Our last day of school comes up next week, and some kids are still doing hybrid. Think about a child being taken away from their social unit during these long periods of shutdown. Imagine how we, as adults, are impacted. Now, try to apply that to our children who are in regular ed and the children who are in special education. They lose structure, peer groups, and a chance to be able to play and socialize. It impacts them in many different areas. Another piece of the puzzle that we need to look at is how this affects them academically. If they cannot keep up and understand the material from the vantage point of being online and start to fail their classes, this also impacts their mental health. Some of our kids shut down. We also see increases in behaviors, stomach issues, and mental health issues. COVID has thrown us a curveball in education. I think we are just seeing the tip of the iceberg for how it will impact our children throughout next year and possibly even more years to come.
Back in 2016, Blackman et al. (2016) found that 20% of students between six and 18 years old have a mental health diagnosis. There is a 21% increase between those ages for mental health issues (Arensen et al., 2019). Fifty percent of children diagnosed with mental health issues receive intervention, whether within the school setting or privately (Moon et al., 2017). But, 75% of them receive either inadequate intervention or no intervention at all (Capp, 2015). These kids are dealing with these emotions and traumas that they do not know how to handle. It impacts their ability to engage successfully in their occupation of being a student.
If you look at the pie chart in Figure 1, it gives you a brief breakdown of the different diagnoses that you may see within a school setting.
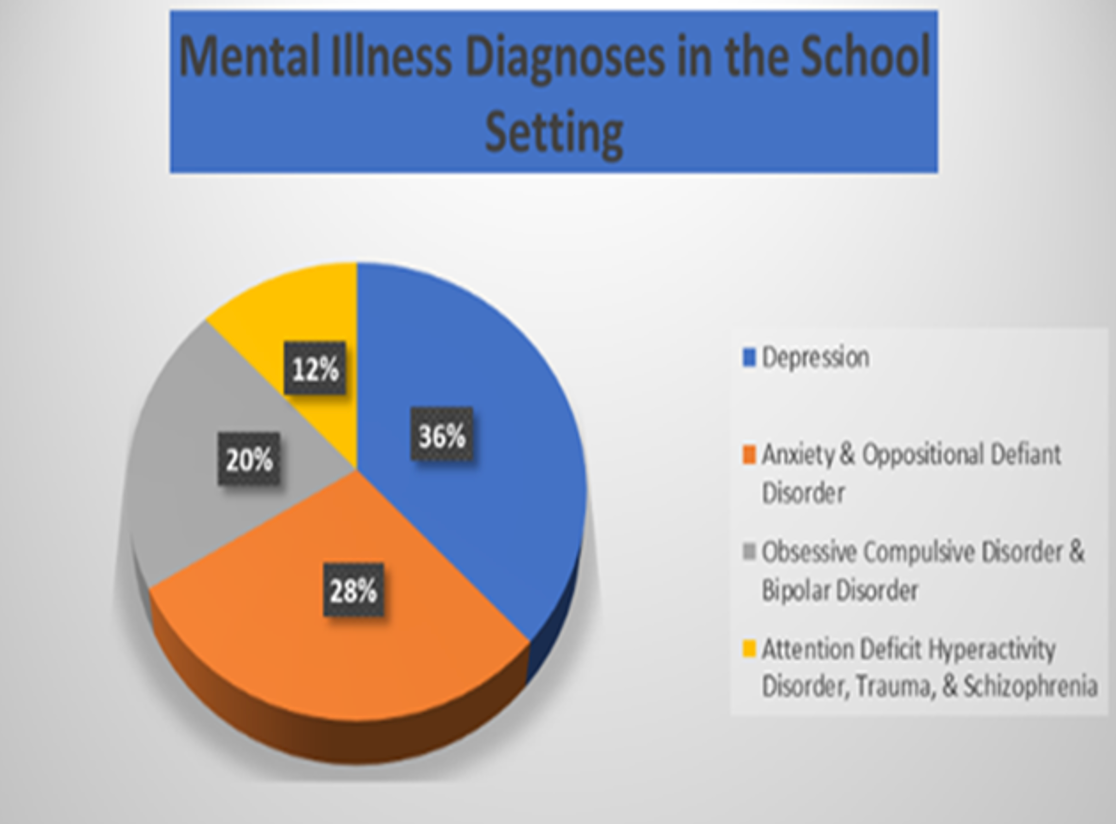
Figure 1. Mental illness diagnoses in a school setting. Click to enlarge the image.
The most significant mental illness diagnosis of children in a school setting is depression. I think that is very eye-opening, and it should cause us to be concerned. Many children are concerned for their safety and well-being. Then, 28% of kids have anxiety and oppositional defiant disorder. I see a lot of stress in kids. I work with a lot of children who are on the spectrum in my district. There is this one great kid that comes into therapy and constantly speaks words of affirmation to himself. "It's going to be okay." Sometimes he will shake, and I have to stop what we are doing, hold his hand, and guide him in a deep breathing exercise, slowly count to 10. I can see the anxiety coming out of him. Anxiety is typical for this child. During our therapy sessions, I constantly think of ways to help him relax a little bit more.
Twenty percent of students have been diagnosed with obsessive-compulsive disorder (OCD) and bipolar disorder. Many children on the spectrum deal with OCD. OCD impacts their ability to complete a task. Twelve percent have attention deficit hyperactive disorder (ADHD) or schizophrenia. We see schizophrenia more so in high school kids.
Childhood Trauma
Trauma-induced therapy is something you have to be trained in as it is handled differently. However, I still think that we, as OTs, can become certified in treating trauma. If a child is having difficulty during the school day, we have the tools to help them self-regulate and calm, if only for a moment, to help them reestablish a foundation to continue with their day.
Statistics
- 20-50% of students experience trauma within their families, school, or community
- 40% of 8-11-year-olds have reported having their lives threatened
- 68% of adolescents have experienced at least one traumatic life event
Here are some statistics. Twenty to 50% of our students experience trauma within their families, school, and community. There can be domestic violence, drug use, etc. Case in point, I worked with a little fella that would fall asleep in class. His grandmother was raising him, but when his mother was in the house, she smoked a lot of pot. We put two and two together and figured out that he was getting second-hand residue smoke. The second-hand smoke impacted his ability to remain awake at school and school performance due to no fault of his own.
A prevalent trauma in school is bullying. Bullying happens on the playground, classroom, school restroom, cafeteria, etc. Bullying is a huge component of trauma in our schools. I attended an IEP meeting today where a mom was concerned about her child getting transitioning to middle school and how bullying would be addressed in the school. Children are exposed to trauma in the community, like watching the news reports, car accidents, and violence in the home. Reports state that 40% of eight to 11-year-olds' feel threatened. That is almost incomprehensible to me. For example, they are molested and told not to tell anyone, or they will be harmed. Many children witness domestic abuse, and the parents threaten them not to tell. Sixty-eight percent of adolescents have experienced at least one traumatic event in their life. If you have experienced trauma in your life, you know how it has impacted you. I would challenge you to take that a step further and try and imagine how it affects our youth, whether they are regular ed neurologically typical or special ed, and have challenges. Trauma is going to impact them.
Types
- Physical abuse
- Sexual abuse
- Exposure to domestic or community violence
- PTSD, anxiety, depression
- Verbal/Emotional abuse
- Neglect
(Langley, Santiago, Rodriguez, & Zelaya, 2013)
What are some types of childhood trauma? There can be physical and sexual abuse that can happen anywhere. Children experience domestic or community violence, which can cause PTSD, anxiety, and depression. Verbal and emotional are other types of trauma. Neglect comes in many different shapes and forms, whether the child is not being fed, kept clean, etc.
What Can Occupational Therapy Do?
- RECOGNIZE, ASSESS, AND TREAT MENTAL ILLNESS (Arbesman et al., 2013)
- HAVE KNOWLEDGE IN PROGRAMMING (Arbesman et al., 2013)
- Environmental modification
- Sensorimotor regulation
- Life and social skills groups
- INCORPORATE THERAPEUTIC USE OF SELF (AOTA, 2016)
Occupational therapists are trained to recognize, assess, and treat mental illness. This goes across the board, and there is no age stipulation. Mental health treatment does not require us to sit down and complete a formal assessment. Every time that we work with a client, we should be actively addressing mental health needs. If they are having a down day, we should help them find ways to regulate themselves better. We need to celebrate with them when great things happen, and we need to process them in times of difficulty.
We also know programming. We are pros at environmental modification. I can go onto a classroom and see how busy it may be. What is on the walls? What is hanging from the ceiling? Is it overstimulating for the children? Can I put something over the lights to dim the room just a little bit? What is going on with air conditioning? Is that too loud? There are so many different factors that we can look at as practitioners to help modify a room to bring in more self-regulation.
I have recommended a quiet corner. Kids love teepees or tents that they can go into if they are overwhelmed. Removing themselves from the class to the quiet space for five to 10 minutes can help them decompress and regulate themselves. They can then come back out and ready to learn. You might even want to put a rocking chair in the room. Rocking is a calming thing to do. Fidgets can help kids when they feel nervous while they are talking, listening to lectures, and taking notes. You can also put Velcro underneath the desk or give them a Move 'n' Sit at their desk. TheraBand around the bottom of their chair can allow them to bounce their feet up and down. Physioballs are also options for kids to sit on, roll around, and jump up and down.
When looking at sensorimotor regulation, we can instruct teachers (and children) on some techniques to help calm the group or rev them up when they are having a very slow and tiring day. We have to remember that having low sensory input is just as crucial as being overstimulated. As OTs, we can come in and give recommendations to maintain a good level of arousal. For example, perhaps Johnny is overwhelmed and is starting to rev up. We can let him take a break, or one of the classroom assistants can walk around the school with him. He could take books back to the library for great resistive work. By removing him from the situation for just a brief period, I can assure you that he'll come back more ready to learn. Perhaps Sally has her head on her desk and not paying attention. You might want to put on some exercises on the smartboard and get the entire class up and do some jumping jacks or fun dances. There are plenty of programs like Oodles of Noodles. I cannot remember all of them, but there are plenty of options to get kids ready for class. It is vital that they take breaks throughout the school day because their sensory systems are in constant flux. They may just need some quiet.
We are pros at running life and social skills groups. What an excellent opportunity to sit down and talk to children about what it means to feel overstimulated or sluggish. This helps them to identify what their bodies need to regulate and get ready to learn. Lastly, as an OT, the most incredible tool in our toolkit is our therapeutic use of self. We can use this every time, any time, and all the time with our clients to help bolster emotional regulation.
Simple Study
Overview
- POPULATION
- Active school-based practitioner
- Must live in the state of South Carolina
- METHODS
- A self-designed survey using Survey Monkey
- 10 questions
- Demographics
- Likert scale
- Open-ended questions
Let's now talk about the study that I did. I live in the state of South Carolina. I surveyed school-based practitioners (OTRs and COTAs). They had to be actively practicing and in the state of South Carolina. It was a self-designed survey via Survey Monkey. I asked ten questions and asked them some demographics. I used a simple Likert scale to get some values and some open-ended questions to find some themes.
I was blessed to be able to get 35 participants. I have been in the school district for so long that I could reach out to many peers. This was crucial as I was not allowed to go through districts.
Survey Says
- 44% of practitioners felt moderately prepared to address mental health needs
- 28-40% of practitioners were not satisfied or slightly satisfied with how they address student mental health
- 28% of practitioners did not feel an interdisciplinary approach was being used
- 72% of practitioners did not feel administration had the skills to meet the mental health needs of students
The results made me sad. Only 44% of practitioners felt moderately prepared to address mental health needs. Some participants may have been a little confused by this. They may have thought that they needed to give formal assessments. Additionally, 28-40% of the practitioners were not satisfied or just a little bit satisfied with how they were addressing mental health. Twenty-eight percent also did not feel that an interdisciplinary approach was being used. I took this to mean that they thought only administrators, school psychologists, and guidance counselors addressed mental health. Lastly, 72% of practitioners did not feel that the administration, the principal, and the assistant principal had the skills to meet the needs of the students' mental health.
Graphs
I am a visual person, so I wanted to put the results in graph form, as shown in Figure 2.
Figure 2. Results of the author's study. Click to enlarge the image.
If we look at the first one, are OTs prepared? The final response of "feel extremely prepared" barely registered for participants. Moderately prepared did not register either on the graph. For the following question for satisfaction, the winner was "only slightly satisfied." I want all of us to be able to come home at the end of the day and think, "I did my part today to help anybody that I crossed paths with today. I helped make their day better." And, only 72% or 48% were slightly satisfied with what they did. Is administration prepared? Overwhelmingly they disagreed that administrators were ready to meet the mental health needs of the students. Some felt that there was an interprofessional approach, but the response "disagree" was a close second.
Things in Common
- Emotional Regulation
- Sensorimotor Regulation
- Zones of Regulation
- Classroom Modifications
- Therapeutic Use of Self
- Some therapists report they are not addressing mental health
- Some therapists state their abilities are not needed
- Lack of support from administration
With the open-ended questions, I was able to identify some common themes across the state. I thought these were pretty interesting. Many therapists felt that they used emotional regulation strategies with the children to help them to recognize how they were feeling. There was also a commonality with sensorimotor regulation. I am fortunate enough that at my schools, we have a sensorimotor room with some excellent equipment. These are some fantastic tools to use in the school system. A swing is one piece of equipment that most kids like. It provides calming, linear movement. I think the second favorite is the trampoline. A lot of kids want to come in and bounce out their wiggles. Many of the OTs across the state are trained in the Zones of Regulation and use that within their practice.
Many therapists are also using classroom modifications to provide a calm or a more alerting environment. We can use therapeutic use of self in the classroom, outside of the classroom, and anywhere we go within the school building. Some of the therapists reported that they did not feel that they were addressing mental health at all. Other therapists thought they had the skills to use within the schools, but they did not believe those abilities were needed. Finally, there was an overwhelming report of a lack of support from the administration.
Conclusions
- Indicates a lack of education regarding OT’s qualifications and roles
- Occupational therapy is not recognized as mental health provider (Cahill & Egan, 2017)
- Indicates a need for occupational therapy’s help (Ball, 2018)
- Current interventions are not enough
The conclusions showed a lack of education regarding occupational therapy in the school systems. With our qualifications and roles, we can address mental health. However, we are not currently being recognized as mental health providers. My very first job out of school in 1989 was at the Institute of Psychiatry at the Medical University of South Carolina. We did a lot of therapeutic media and cooking groups, and we could bill as such. We no longer can do that. Sadly, at the Institute of Psychiatry at the Medical University of South Carolina, they only have an OT there for consulting work. It is recreational therapy that is doing all of the intervention now. We need to wake up, lobby, and get our feet back in the door to be mental health providers.
- Indicates occupational therapy should be part of the interprofessional team (Arbesman, Bazyk, & Nochajski, 2013; Ball, 2018; Blackwell & Bilics, 2018)
- Qualified
- Holistic perspective
- Provide strategies and interventions others cannot offer
OT should be a part of the interprofessional team as we are qualified. Number two, we are a holistic practice that addresses mind, body, and spirit. We are concerned about the entire parts of the client. We provide strategies and interventions that other disciplines and other team members simply cannot offer.
Realizations
- Forgotten our holistic roots
- Body, MIND, spirit
- A generation of unaware practitioners
- Mental health IS addressed in all therapy sessions
- Loss of professional recognition (AOTA, 2017)
- Qualified Mental Health Practitioners
- Loss of billable service
- Decrease in types of service
Many realizations came to me because of my study. I feel that we have forgotten our holistic roots and how much we are influenced by the mind as we are by the body and spirit. We have to remember that if those things are not working together, we will not have a well-balanced person. I also feel like we have a generation of unaware practitioners. Again, mental health needs to be addressed in all of our therapy sessions. Due to the loss of professional recognition of occupational therapy as a mental health provider, we have a decrease in the types of services that we can render and the loss of billable services.
Facts
- Occupational therapists are qualified to work in mental health (Blackwell & Bilics, 2018)
- Occupational therapy is needed to address the mental health needs of students (Ball, 2018)
- Occupational therapy should be a part of the school-based interprofessional team (Chan et al., 2017)
- Education and collaboration with administration (Ball, 2018) is key to making this happen
Occupational therapies, again, are qualified to work in mental health. More OT is needed to address the needs of our children. We should be a part of the interprofessional team. Education and collaboration with the administration are the keys to getting us onto that interprofessional team.
Social Emotional Learning Curriculums
- ZONES OF REGULATION
- Created by Leah Kuypers
- Occupational therapist
- POWERFULLY YOU
- Created by Amy Herring and Heather Spann
- Occupational therapists
Let's now talk about some social-emotional learning curriculums. The two we are going to discuss are the Zones of Regulation and Powerfully You. Occupational therapists are the creators of these programs. This makes my heart sing because this is another indicator of how in tune we are with our clients in mental health and what we need to be doing to help them.
Zones of Regulation
What is self-regulation?
- The ability to adapt one’s
- neurological arousal
- emotional state
- motor activity
- attention
- behavior
- to match the demands of the situation.
(Zones of Regulation, 2021)
What is self-regulation? This is one of the definitions that made sense to me. We are "engagers" in a situation, and how do we respond to that. Is it equal to what the situation is? For example, if your house is on fire, the response will be that you need to get outside. How are we regulating our neurological arousal, emotional state, motor activity, attention, and behavior to match the situation.
Let's bring that down to a school-based level. I will give you a personal example. I have a child who comes in once a week to see me. Ms. Moni's rule is that we work first, then we play. After he finishes his work, he gets to go and do what he wants. He always finds a piece of Lego and says, "Ms. Moni, can I take this home?" For two weeks in a row, I said. "Go ahead." It was just a little Lego. Then, I started to see the pattern. Last week when he wanted to take a lego home, I said, "You know what, buddy, I've got other friends that want to come in here and might want to play with that particular piece of Lego. Let's leave that here, and it'll be here for you next week when you come." He did not like that answer and got very angry. I let him feel what he needed to feel. I validated that feeling. After that, I said, "I do have some Skittles in my pocket. I can give you some Skittles if you go put that back in the bucket." That is all it took. The power of a Skittle is incredible. You just never know what it can do. Again, I acknowledged the fact that he was upset. I then helped his response to match the level of what the situation was. He did not need to get angry and kick the desk and throw the Lego because he did not get to have it. He needed to take that answer of no, process it, and just go with it.
- Rooted in cognitive behavioral therapy (CBT)
- Strategies for emotional and sensory self-management
- Uses four colors to help students identify how they are feeling
- Provides strategies to support regulation
(Zones of Regulation, 2021)
In the Zones of Regulation, it is rooted in cognitive behavioral therapy, which we all know is changing how we think. Also, Zones of Regulation provide emotional and sensory self-management strategies. It is an excellent curriculum that uses colors to match moods.
Green Zone
- A calm state of alertness
- happy
- focused
- content
- ready to learn
- where optimal learning occurs
(Zones of Regulation, 2021)
The green zone is when the child is best ready to learn. They are happy, focused, content, and prepared to learn. For example, they are having a great morning, everything is going right, the school bus to their house was on time, and their breakfast was not too hot/too cold. This is where we want our kids to be.
Yellow Zone
- A heightened state of alertness and elevated emotions
- more control when they are in the Yellow Zone
- Stress
- Frustration
- Anxiety
- Excitement
- Silliness/wiggles
- Nervousness
(Zones of Regulation, 2021)
The child is a little bit more heightened and alert, but they are still in control. They may have stress about a big test to take or frustration from some results. They may have their lunch and feel anxious. They may be excited about earning a 100 on a test. They may keep going and get more and more with lots of silliness, wiggles, and then nervousness. They may be in the yellow zone because they cannot stop being nervous. "What do I need to do to calm down?"
Blue Zone
- Describes low states of alertness and down feelings
- Sad
- Tired
- Sick
- Bored
(Zones of Regulation, 2021)
In the blue zone, the child may be sluggish, and their alertness may be down. They may feel sad, tired, sick, or even bored.
Red Zone
- extremely heightened states of alertness and intense emotions
- Elated
- Euphoric
- Experiencing anger
- Rage
- Explosive behavior
- Devastation
- Terror
(Zones of Regulation, 2021)
The last state is the red zone. In the red zone, the child is teetering on edge. Their emotions and alertness are highly heightened and intense. They can have joy and euphoria, but they can also have anger, rage, and explosive behavior. They can also be scared or terrified. The cool thing about the Zones of Regulation and Powerfully You is that we are teaching our kids about their emotions and not to feel bad about them.
No Good or Bad Zone
- There truly is no “BEST” zone
- Our emotions are a range
- They are to be expected
- When dysregulated, pinpoint…
- how we feel internally
- determine the ZONE we are in
- regulate or manage it
- Tools and strategies
(Zones of Regulation, 2021)
There is no "best zone." We want them to understand that emotions are normal and expected. They need to pinpoint when they are dysregulated and what zone. "Am I feeling that heightened feeling? Am I feeling angry? Am I blue? Am I feeling sick? Am I not challenged? Or, am I in the yellow where I still can have a grasp on myself and bring myself back down to the green zone?" We teach them the tools and the strategies for how to handle their emotions. Our moods/emotions fluctuate daily and throughout the day.
Tools and Strategies
- Deep breathing
- Counting to 10
- Deep pressure
- Positive self-talk
- Removal from the situation
- Take a walk
- Talk to an adult
Deep breathing, counting to 10, deep pressure are some calming interventions. Sometimes, we can even have a child hug themselves or squeeze their hands together. Positive self-talk is another intervention. Other calming strategies include removing them from the situation, taking a walk, or talking to an adult.
Powerfully You
The next one is Powerfully You.
Words To Live By
“The more you can embody compassion, nonjudgement, and appreciation for individual differences while being present not only for your client but also for yourself, the more effective you will be in supporting your client’s journey.”
(Powerfully You, 2021)
In other words, when you can be in touch with your feelings and know what you need to do and how to handle them, the more powerful you will be for your client.
Social Emotional Learning (SEL) Curriculum
- Focuses on self-regulation
- Compassionate
- Non-judgemental
- Values individual differences
(Powerfully You, 2021)
Powerfully you is a social emotional learning curriculum. It focuses on self-regulation. It is compassionate, non-judgmental, and values differences in those emotions. It is essential to let the child know that it is okay to be angry or have a low battery.
Concepts of Powerfully You
- Safety
- Body sensing
- Body battery
- Activation/Arousal
- Self-Compassion
- Sensory and motor-based tools
- Mind and Body Awareness Tools
- Therapeutic Use of Self
- BEST
(Powerfully You, 2021)
We talk about safety, body sensing, body battery, activation and arousal, and self-compassion. We offer them tools, both sensory and motor, mind and body awareness, therapeutic use of self, and last but not least, the BEST lesson.
Lessons
- Core Lesson
- Body Sensing
- Body Battery
- Activation
- Tool Lesson
- Body Based Tools
- Thought Based Tools
- Feeling your Feelings Awareness
- Best Process
(Powerfully You, 2021)
The core lessons are body sensing and understanding what you are feeling internally or interoception. It also talks about the body battery. Is your battery nice and high and complete, or is it low? How do we get it to the middle? How do we activate our sensory systems to ready ourselves for learning? After we go over those core lessons, then we go into the tool lessons to teach the child how to provide those strategies through body-based tools, thought-based tools, feeling your feelings awareness, and then the BEST process.
Safety
- Increase body connection with your body and, in turn, yourself
- Be aware of one’s basic needs and validate them
- Sleep
- Physical activity
- Nutrition
- Connection with others
- Be an example for non-judgment and compassion
- Emphasize the importance of individual differences
(Powerfully You, 2021)
In safety, this is where we increase body connection with our body and, in turn, ourselves. We need to ensure that our children are getting sleep, physical activity, nutrition, and connection with others. We need to teach them that it is nonjudgmental. Again, for your emotions, these are all normal. We need to be compassionate to how they are feeling. We also need to validate the importance of individual differences.
Body Sensing
- Interoception
- Sensations related to the physiological/physical condition of the body as it relates to the five senses
- What the body organs are feeling
- Detects responses that guide regulation
- Hunger
- Heart rate
- Respiration
- Elimination
(Powerfully You, 2021)
Body sensing is interoception. What are your organs feeling? If your stomach is growling, you are hungry. You need to take care of that to feel balanced. Is your heart racing fast? You need to take a couple of deep breaths to bring down that heart rate, or you need to sit calmly. Even elimination is essential for our kids on the spectrum who battle with constipation. This is going to impact their mood. I could tell you tons of stories.
Body Battery & Activation/Arousal
- Is your battery at full charge?
- Sleep
- Nutrition
- Physical activity
- Connection with others
- Young children have little control with this concept
- Socioeconomic
- high-quality food
- safe environments
- Medical and metabolic issues can have an impact on sleep
- Arousal is a continuum
(Powerfully You, 2021)
Is your body at full charge? Did you get sleep? Did you get nutrition? Did you get your physical activity? Did you have a positive connection with others? Young children have a hard time with these concepts, as these things are hard to define. They do not have a lot of control over it either. Sometimes, parents do not put their children to bed until10:00 o'clock at night. Or, some children are not privileged to be exposed to nutritious foods. This will impact the way that they feel. They may not be living in safe environments. There are also medical and metabolic issues that can affect one's ability to sleep. We know that we need our sleep, as do our babies. Remember, arousal is a continuum. Our moods will fluctuate throughout the day, just like our sensory systems are.
Take This To Heart
- “When little people are overwhelmed by big emotions, it’s our job to share our calm, not join their chaos.” L.R. Knost
(Powerfully You, 2021)
When our little people are being overwhelmed by big emotions, it's our job to share our calm, not to join them in their chaos. We can calm our children, make them feel safe, and help them ready themselves for better learning.
Summary
This has been wonderful y'all. Thank you for joining me. If you want to email me, please feel free. I have also included references and websites for the Zones of Regulation and Powerful You. Please check them out. They are excellent resources, and it is worth getting training. I hope to see you again really soon. Thank you so much.
Questions and Answers
I have used the Zones of Regulation with a number of my clients. They seem to understand it and can state all the colors and emotions until they are blue in the face. The problem I seem to have is getting them to use the coping skills and the strategies. What have you found to be the best way to calm a child or incorporate the zones?
I find that stopping whatever they are doing is the first thing. We need to help them use those strategies of deep breathing, counting down, deep pressure, etc. We need to alter the environment and what is going on in that situation to help calm them.
What have you found to be the best way to go about diagnosing mental health in a student if you suspect something is going on?
That is a great question. One of the best things that I have in my toolbox is a good relationship with my teachers. Case in point, I have one child who quickly cycles from going from depressed to a state of mania. And when I bring the child back to the classroom after therapy, the teacher and I talk about what we did, what I observed, and how it was handled. One day as we were chatting, she said, "He presents to me very much as somebody who has bipolar disorder." And I was like, "You know what? I think that's a very accurate description." I asked the teacher, "Do you know if this runs in his family?" She did know and did not feel comfortable asking the parent. I inquired with the parent, and sure enough, the mom has bipolar disorder, as does her maternal grandfather. That was one way of bringing up some mental health issues.
Considering this high rise in mental health issues, how can we best, as OT practitioners, be effective in helping the children during this challenging year? Can you recommend the top strategies to address this?
OTs are nurturing individuals by nature. As our clients are coming in for therapy, we are great observers and can intuitively feel if they are doing well or not. We need to embrace that moment and confidently say, "Hey, what's going on today? What can I help you with?" I think that we have a gift of having these types of conversations with our clients. I like to remind my kids that if they have had a bad day and made some poor choices, that is part of life. "We learn from that, but what can we do differently tomorrow?" I want to rejoice with my clients when they do something great. I tell them that I am proud of them. They are smart, have incredible potential, and can make an impact in this world.
It does not have to be a specific program per se, but we need to be able to intuitively connect with our clients and help them through difficult times. You can ask them how they have been doing in this challenging year. "How does it feel to be back in the classroom? How did you feel when you had to be stuck at home, and you couldn't go outside and play?" This affirms them and validating their feelings. You are letting them know that how they feel is okay. And if they are not doing ok, you can give them some ideas of how they can better handle it.
When children live with dysfunctional parents, do you sometimes feel you are swimming?
If we can help these children feel safe and validated while they are with us, we have done our job. Then, we will see better results in their academics and their performance during the therapy time.
Are you familiar with the integration of Ayres' sensory integration with mental health? If so, can this be applied in a school setting?
Sensory integration is very much a part of mental health. Jean Ayres' philosophy certainly can be applied to mental health. If our sensory systems are not balanced, then, of course, it will throw off our mood, emotions, and regulation as a whole. For example, if we are riding high, of course, it will impact our mood and make us jittery, nervous, or even excited and giddy. It depends on the individual, but we need to bring all that excitement down. We get the child's mood, emotions, and sensory system back down to ready them for learning through sensory strategies.
References
Sunbelt Staffing. (2021). Retrieved from https://www.sunbeltstaffing.com/resources/schools/school-based-physical-therapy-role-faqs/
Resources
ZONES OF REGULATION: https://zonesofregulation.com/index.html
POWERFULLY YOU: https://www.powerfullyyou.org/
Citation
Keen, M. (2021). School-based occupational therapy and student mental health: Are we helping?. OccupationalTherapy.com, Article 5458. Retrieved from http://OccupationalTherapy.com

