Editor's note: This text-based course is a transcript of the webinar, Skilled Nursing Facility Interventions: An Introduction To Teepa Snow And Positive Approach to Care, presented by Laurie Walther, MS, CCC-SLP.
Learning Outcomes
- After this course, participants will be able to compare and contrast the different approaches and skills to support a person living with dementia and the rationale for the utilization of each one.
- After this course, participants will be able to recognize GEMS® states and how they apply to a person living with dementia and the progression of their disease process.
- After this course, participants will be able to identify PAC skills and appreciate the possibilities of how they can be integrated in one’s daily interactions with persons living with dementia to maximize care partnering through supportive techniques.
Introduction
This talk is meant to be interactive. After each area, I am going to ask you to stop and think about it. I am also allowing some "chat time."
What Words Come to Mind With Dementia?
When you think about dementia, what are some of the words or thoughts that come to your mind? Here are some of the answers from the live event: confusion, memory loss, impaired cognition, and altered reality. Those are popular answers. I'm hoping that as we continue through this presentation, we'll be able to make a little bit of a shift. Not that these things don't happen, but how can we help them through some of those things?
What is Dementia?
- It’s an umbrella term.
- There are over 120 different types that fit under the umbrella.
This is not a basic course, so this is a quick overview. Dementia is an umbrella term. There are actually over 120 different types that fit under the umbrella.
Dementia Symptoms
- It is important to know the symptoms.
- A 100% true diagnosis cannot be determined until after death.
- We need to take inventory of what the PLwD (Person living with dementia) is capable of doing.
It's important to know the symptoms as this is the best way to try and determine what type of dementia someone has to help guide our treatment. A 100% diagnosis cannot be determined until after death, but you may see on MRIs, as an example, things like small vessel changes, senescent changes, and atrophy. Ideally, they note where some of those changes are so that we can use our neuroanatomy and knowledge and figure out what might be going on.
It is also imperative to know what the person living with dementia is able to do and what abilities they still have versus what they can't do or have lost.
Four Truths About Dementia
- “At least 2 parts of the brain are dying.”
- “It is chronic – can’t be fixed.”
- “It is progressive – it gets worse.”
- “It is terminal – it will kill, eventually.”
Compare these two brains in Figure 1.
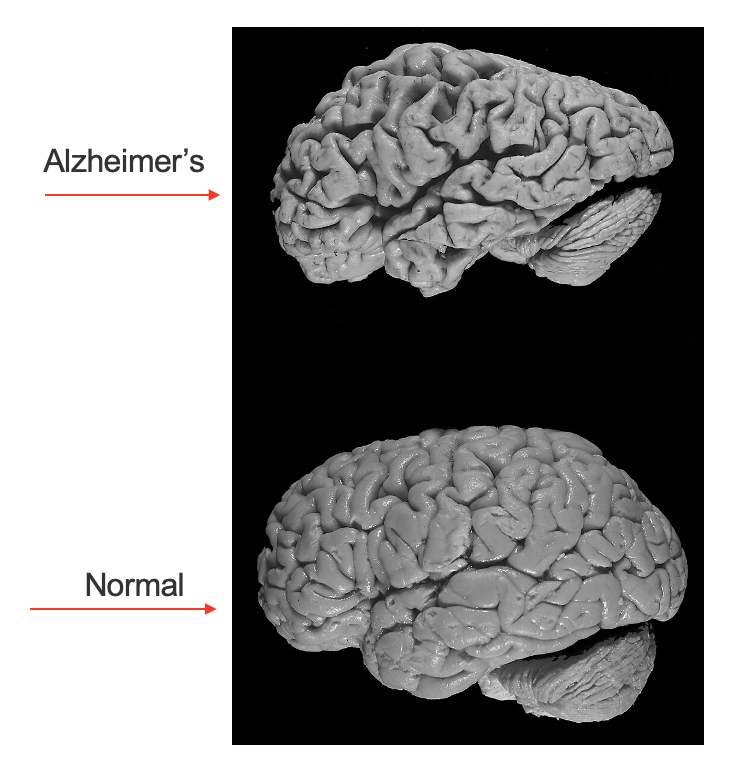
Figure 1. Brain from someone with Alzheimer's in comparison to a normal one. (Image Source: Hersenbank, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons)
There is a normal brain and then a picture of the brain of someone with Alzheimer's. There are four truths about dementia. The first is that at least two parts of the brain are dying. The next two are that it's chronic and can't be fixed, and it's progressive and gets worse. The last is that it's terminal, and it's eventually going to kill the person. At the end of life with dementia, the brain is one-third of its original size. You can see in the picture how the brain starts to atrophy.
Teepa Snow
You may have heard of Teepa Snow. She is a dynamic occupational therapist, and I'm excited to share her expertise with all of you.
- Occupational Therapist for 40-plus years
- Dementia Care Specialist
- Created the Positive Approach to Care (PAC) in 2007
- Collaborating in over 30 countries
- Leading advocate and educator for PLwD
Who is Teepa Snow? Besides being an OT for 40-plus years, she's a dementia care specialist, who created the Positive Approach to Care or PAC in 2007.
She collaborates in over 30 countries and is a leading advocate and educator for persons living with dementia and other forms of brain change. She has a wealth of clinical, teaching, and research experiences that have informed and influenced her philosophy, approach, and practice. She's engaging, knowledgeable, personable, animated, skilled, funny, and empathetic.
Video of Teepa in Action
This is a great video that shows you all about her. What she does in this example is act like she is dealing with a person with dementia who is saying, "I want to go home." She gets the reaction of a team member who's out in the audience trying to role-play through getting her home. She uses role-playing to teach skillsets by using real-life experiences and interactions.
Teepa's Trainings
She believes that rewiring our own perceptions, attitudes, communication strategies, actions, and responses provides that shift that promotes change for others around us. This is actually about our ability to learn what we don't know or relearn what we know so we provide the right support at the right time to maximize the person living with dementia's abilities and success in their environment. This is also about being open to possibilities of what a person living with dementia is capable of doing.
Teepa's Guiding Beliefs
We need to destigmatize dementia and help the world see how capable people living with dementia are. We want to avoid doing things to or for them, but instead do things with them. Teepa has worked to provide people living with dementia the platform to be their own advocates, answer questions, and highlight how skilled, intelligent, and charismatic they are. We have to be open to understanding that the person living with dementia is an expert through their own experience. Effective partnering is about empowering those who are living with dementia and also empowering those who are caring for them to improve the quality of care and quality of life for everyone on their journey.
You can find Teepa all over social media. She has a YouTube channel with plenty of videos to support your venture.
Dementia Trainings
- Bravo Zulu
- CDP-Certified Dementia Practitioner
- Dementia Capable Care Training
- Dementia Friendly
- The Eden Alternative
- Montessori
- Teepa Snow’s Positive Approach to Care (PAC)
Although today, we are talking about Teepa Snow's Positive Approach to Care, I would be remiss if I didn't mention that there are many other dementia trainings out there as well, like Bravo Zulu, CDP, Certified Dementia Practitioner, Dementia Capable Care Training, Dementia Friendly, the Eden Alternative, Montessori, and many others.
About PAC Skills
PAC Concept
The PAC concept uses knowledge and practical interventions to aid in the development of a partnership between the care and the person with dementia. PAC endorses the term brain change for dementia, explaining that as the structure and function of the brain alter, the person with dementia may change in response, particular symptoms may develop, abilities may change, and understanding and response may alter.
PAC Training
- “PAC training is based on the experiential learning cycle.” (AELC)
- AELC allows you to learn and practice your skills through a hands-on approach.
- Experience
- Share
- Process
- Connect
- Apply
PAC training is based on what's called the experiential learning cycle, or AELC, the adult experiential learning cycle. It allows you to learn and practice your skills through a hands-on approach. This is where you go and do something and then share about what happened and how it felt. You process why something happened. You connect and generalize the information, and then you apply it. By using these steps, we allow ourselves to tap into our own senses and our varying learning styles. Some of us are auditory learners, some of us are visual learners, and some of us are hands-on learners. This training allows us to tap into those varying learning styles to be able to walk away from the training with skills that we can immediately use with patients and residents that we serve.
PAC Positive Approach
The positive approach is a different way of understanding dementia's pathologies. Most significantly, it gives practical advice on how to connect and interact with people with dementia to "do with" rather than "do to." Sensitivity, compassion, understanding, and flexibility are encouraged in PAC, enhancing and preserving the dignity of the person with dementia. Snow's mantra is that "Dementia doesn't rob someone of their dignity. It is our reaction to them that does." By promoting a positive approach to care, dignity is preserved and positive outcomes are experienced.
Core Aspects of PAC
- GEMS®
- Hand under Hand™
- Positive Physical Approach™
Today, we will delve into key elements of PAC, focusing on three core aspects. I will now provide an overview of these concepts, which will be explored further throughout the presentation.
The initial concept is GEMS, which perceives a person living with dementia as a precious gem, emphasizing retained skills rather than those that have diminished. This perspective enables an understanding of changes in the brain, shedding light on the reasons behind the behavior of individuals with dementia. GEMS empowers care partners to align their approach with the specific needs of the person living with dementia.
The second concept, Hand under Hand, is a practical and physical method employed when working with individuals with dementia. This approach facilitates connection and caregiving on multiple levels, a topic we will delve into more deeply shortly.
The third concept is the Positive Physical Approach. This approach entails connecting with the person with dementia and responding to their invitation to enter their environment and space. By doing so, it enhances communication and receptiveness for both parties, fostering a more positive interaction.
PAC Skills
- Provide the why and how
- Empower caregivers with practical, hands-on techniques
- Put the person and your relationship first
- Partner to create the most dignified and meaningful dementia care journey
PAC Skills involve leveraging the remaining abilities of individuals and engaging in activities together, fostering an authentic partnership. This approach has proven to reduce friction and enhance positive care outcomes.
By focusing on both the "why" and the "how," we empower caregivers with practical, hands-on techniques. Our emphasis is on prioritizing the individual and their relationship, creating a framework that places dignity and meaning at the forefront of the dementia care journey. Through this collaborative effort, we aim to establish a genuine and meaningful partnership between caregivers and individuals receiving care.
GEMS® and Dementia Progression
Again, we're learning all about Teepa and PAC today.
Dementia Scales
- Allen Cognitive Levels
- Clinical Dementia Rating
- Dementia Severity Rating Scale
- Functional Assessment Staging Tool (FAST)
- GEMS®
- Global Deterioration Scale
- Global Assessment of Functioning Scales
GEMS is the dementia scale that we will be discussing. However, it's important to acknowledge other scales integral to our practice and routinely utilized. These include the Allen Cognitive Levels, Clinical Dementia Rating Scale, Dementia Severity Rating Scale, FAST (Functional Assessment Staging Tool), Global Deterioration Scale, and Global Assessment of Functioning Scales. These instruments play a crucial role in our daily assessments and contribute to our comprehensive approach to understanding and addressing dementia.
Teepa Snow's GEMS States
- The only constant with dementia, or brains in general, is that they are ever-changing.
- The GEMS Brain Change Model recognizes six different brain states.
The only constant with dementia, and with brains in general, is their inherent and continual state of flux. Daily, all individuals, ourselves included, undergo changes in brain function. The GEMS model, developed by Teepa Snow and rooted in the Allen Cognitive Scale, recognizes six distinct brain states. While the progression, pattern, and changes associated with dementia may vary across different types, the movement through the GEMS states exhibits a degree of predictability. However, it's essential to note that these transitions can also be fluid, altering throughout the day, in response to medical status changes, across days, and over an extended period.
GEMS State Overview
Let's look at the GEMS states.
- Sapphires: True Blue, Healthy Brain
- Diamonds: Clear and Sharp, Routines and Rituals Rule, Change is Hard
- Emeralds: Green/On the Go with Purpose, Naturally Flawed
- Ambers: Caution Required, Caught in a Moment of Time
- Rubies: Others Stop Seeing What is Possible, Deep and Strong
- Pearls: Hidden in a Shell, Beautiful Moments to Behold
As evident from the visual representation, the GEMS model introduces various states, each associated with distinct colors: sapphire, diamond, emerald, amber, ruby, and pearl. Let's briefly explore each state.
Sapphires represent a healthy brain, analogous to a true blue state—akin to you and me on a good day.
Diamonds, on the other hand, are characterized by clarity and sharpness. Those in a diamond state exhibit routines and rituals, but changes can be challenging. It's comparable to everyday situations when we, too, might slip into a diamond state, such as feeling hangry or reacting to a traffic incident.
Now, envision a stoplight for the next three states: Emeralds, depicted in green, signify individuals on the go with purpose, inherently flawed but actively engaged. Ambers, analogous to yellow, indicate caution. Individuals in an amber state are momentarily caught in time, akin to the decision-making process at a yellow traffic light. Rubies, represented in red, symbolize a stop on the metaphorical stoplight. In this state, others may struggle to perceive what is still possible, as rubies are characterized by depth and strength.
Lastly, consider pearls as the analogy for the GEMS state. Much like an oyster shell that appears unremarkable on the outside, individuals in a pearl state may seem tough externally. However, upon closer inspection, they reveal moments of profound beauty and connection, akin to the opening of an oyster shell to reveal a precious pearl. This state involves sharing beautiful moments, though individuals in a pearl state may intermittently withdraw.
Let's break this down a little bit more.
Sapphire ~ Optimal Cognition, Healthy Brain
- Us on a good day
- Clear and true to ourselves
- May feel ‘blue’ over changes
- Can typically choose our behavior
- May have other health issues that affect behaviors
- Recognize life experiences, achievements, and values
Sapphires, representing optimal cognition and a healthy brain, describe a state where cognitive function is at its best. In this true blue state, individuals, whether aging normally or experiencing distress, may encounter occasional difficulty finding words. Despite this, they can articulate thoughts to ensure understanding. On good days, clarity prevails, and self-expression is genuine.
During moments of change, individuals in the sapphire state might experience a tinge of blue, symbolizing a transient emotional response. Importantly, they retain the ability to choose their behavior, even if affected by other health issues. Recognition of life experiences, achievements, and values persists. While capable of learning new things and adapting habits, such changes may require time and effort.
Honoring the choices and preferences of those in the sapphire state is paramount. They may need additional time for decision-making, and specific prompts, such as notes, calendars, or reminder calls, can be beneficial in supporting their cognitive well-being.
Diamond ~ Clear and Sharp
- Many facets, still often clear, can really shine
- Rigid, inflexible, can cut
- Can complete personal care in a familiar place
- Resent takeover or bossiness
- Misplace things and can’t find them
- Vary in self-awareness
- Use old routines and habits
- Usually can follow simple prompted schedules
Diamonds, characterized by clarity and sharpness, thrive on routines and rituals, making change challenging for them. In a positive and supported state, individuals in a diamond state can shine brightly, displaying impressive capabilities. However, when distressed, they may exhibit cutting behavior, akin to the rigid nature of a diamond.
While they can complete personal care tasks in familiar settings, diamonds may resent takeover or bossiness. Misplacing and struggling to find items is common, and self-awareness may vary. Relying on old routines and habits, they typically follow simple prompted schedules. Despite social engagement, understanding others' perspectives may be challenging, and awareness of boundaries might diminish or become more progressive.
Individuals in a diamond state can encounter agitation, such as when someone occupies their usual chair, as they seek clarity on who is in charge. It's essential to recognize that being in a diamond state can result from factors beyond dementia, such as hunger or changes in medical status like a UTI. Just as we experience fluctuations in mood, individuals in a diamond state may also be influenced by various external factors.
Emerald ~ On the Go with a Purpose
- More vague
- On the go, need to ‘do’
- Flaws may be hidden
- •Remember the past, and I go there
- Do what is seen, but miss what is not seen
- Must be in control, but not able to do it correctly
- Do tasks over and over, or not at all
Emeralds, symbolized by the color green, are individuals who are consistently on the move with purpose, driven by a sense of needing to accomplish tasks. Imagine someone who anxiously believes they must reach the office by 9 o'clock every day or a night security guard who roams the halls, motivated by a sense of duty.
In their state of perpetual motion, emeralds may appear more vague, with flaws hidden beneath their active exterior. They recall the past readily but might overlook what is not immediately visible, as illustrated in the example of missing utensils rolled up in a napkin during a dining experience.
Emeralds feel the need to be in control, although they may struggle to execute tasks correctly. They may repeat tasks or, conversely, neglect them altogether. Their focus centers on immediate wants and needs, with potential unawareness of safety or changing abilities. While the details of interactions may fade, emeralds retain a strong emotional memory of how they were made to feel.
It's crucial to note that correcting or arguing with emeralds can lead to resentment or suspicion. Effective assistance involves going with their flow, adopting a positive approach, and modifying the environment to meet their needs. Emphasizing emotional impact over verbal communication forms the foundation for building meaningful relationships with individuals in the emerald state.
Amber ~ Caught in a Moment
- Amber Alert: Caution!
- Sensory tolerance, easily over or under-stimulated
- May be private and quiet or public and noisy
- No safety awareness
- Explorers, get into things, invade others’ space
- Do what they like and avoid what they do not
Ambers exist in a moment of time, symbolizing caution due to sensory tolerance issues, making them prone to over or under-stimulation. They may display a spectrum of behaviors, ranging from being private and quiet to public and noisy. Safety awareness is diminished, and they become explorers, engaging with their surroundings and invading others' personal space.
Consider the amber who, upon entering a dining room, is captivated by a flower, picking its petals and placing them in their pocket or attempting to eat it. Their actions reflect a preference for what they like and avoidance of what they do not. At this point, they may not know you, but they find comfort in simple tasks repeated over and over, involving movement, touch, smell, taste, or disassembling objects.
While these repetitive actions might exhaust or frustrate caregivers, they serve as a soothing mechanism for individuals in the amber state. Daily activities like eating, taking medication, mouth care, bathing, dressing, or toileting may distress them. Object confusion further complicates these tasks, emphasizing the importance of adapting approaches to accommodate their needs and ensure a more comfortable experience.
Ruby ~ Deep and Strong in Color
- Major loss of fine motor and oral skills, but can do gross motor like walking, rolling, and rocking.
- Comprehension and speech halted
- Limited visual awareness
- Balance, coordination, and movement losses
- Eating and drinking patterns may change
- Wake-sleep patterns are very disturbed
- Follows gross demonstration and big gestures
Rubies, characterized by their deep and strong color, often have obvious losses that make it challenging for others to recognize their remaining abilities. Caregivers play a crucial role in identifying and supporting these remaining capabilities. In the ruby state, wake-sleep patterns are highly disturbed, leading to restlessness and potential self-stimulation, such as walking and humming.
While fine motor and oral skills may experience significant loss, gross motor skills like walking, rolling, or rocking remain intact. Comprehension and speech may be halted, and balance, coordination, and movement losses become apparent. Eating and drinking patterns may change, and individuals in the ruby state follow gross demonstrations and respond to big gestures.
Care for those in the ruby state involves anticipating needs, creating a supportive environment, and providing assistance with daily activities. Similar to a crossing guard directing traffic, caregivers guide movements and transitions, as individuals in this state may struggle to initiate or stop on their own. Switching gears becomes challenging, so caregivers are advised to move with the individual first and then use their body to demonstrate desired actions step by step.
Hand-under-hand assistance is beneficial for instilling a sense of safety and security, particularly since individuals in the ruby state may have difficulty using objects correctly. Despite these challenges, moments of joy can still be experienced when caregivers are able to provide activities that bring pleasure and comfort.
Pearl ~ Hidden Within a Shell
- Primitive reflexes
- Spends much time asleep or unaware
- Bed or chair bound, frequently fall forward or to the side
- May cry out or mumble often, increases vocalizations with distress
- Can be difficult to calm, hard to connect
- The end of the journey is near, multiple systems are failing
- Knows familiar from unfamiliar
- Beautiful and layered
Pearls, concealed within a shell, are individuals ruled by reflexes and prone to easy startle responses, retaining primitive reflexes reminiscent of the theory of Retrogenesis. Spending a significant amount of time in sleep or unawareness, they may be bed or chair-bound, often falling forward or to the side. Vocalizations, including crying and mumbling, increase with distress.
In this advanced stage, individuals in the pearl state can be challenging to calm and may seem hard to connect with. Approaching the end of their life, multiple systems are failing. Despite these challenges, they retain a sense of familiarity over the unfamiliar, and their beauty and layered essence endure.
Moments of alertness and responsiveness punctuate this stage, creating opportunities for connection that foster a sense of wholeness and value. Caregivers are urged to utilize their time not only for providing care but also for comforting and connecting with the individual. Treating them with dignity, it's essential not to speak about them as though they are not present. Familiar voices and gentle rhythmic movements are more likely to evoke positive responses.
As individuals in the pearl state near the end of their journey, difficulty breathing and swallowing may become evident. Their bodies may no longer desire food and drink as they prepare to transition from life. Teepa emphasizes that, like gems, each person is precious, valuable, and unique, and with the right setting and care, they can continue to shine even in their final stages.
Chat Time/Key Takeaways
It's chat time. I know that this is a ton of information, but I want you to think about some of the key takeaways for the concepts of GEMS and the progression of dementia.
Here are some answers from the live course chat.
- Fluidity: Oh, I love that. Yes, they can move through it.
- Valuing the person: I love that as well.
- Make sure you know their ability.
- They're precious until the end.
- Focusing on their strengths in each GEMS state.
- Focusing on those feelings and relationships.
You guys are fantastic. I love all of these answers.
Hand under Hand®
Let's talk about Hand under Hand.
- “HuH is an evidence-based, research-proven care technique developed by dementia expert Teepa Snow.”
- “It utilizes the remaining muscle memory of a person living with dementia to offer comfort and initiate activity. It also enables care partners to better assist with activities of daily living, such as eating, drinking, or personal care.”
The Hand under Hand concept is an evidence-based and research-proven care technique developed by dementia expert Teepa Snow. This approach leverages the remaining muscle memory of individuals living with dementia to provide comfort and initiate various activities.
In essence, Hand under Hand involves the care partner placing their hand under the hand of the person living with dementia, with their palms touching. This physical connection offers a comforting and supportive link between the care partner and the individual receiving care. For instance, when used for assistance with feeding, this technique allows for a natural eating movement, triggering muscle memory and providing the person with dementia a sense of control.
The application of Hand under Hand is versatile, extending to activities of daily living such as eating, drinking, and personal care. By utilizing this technique, care partners can effectively support individuals with dementia, improving their overall comfort and enhancing their engagement in various daily tasks. Specifically, when applied to feeding, it contributes to a more natural eating experience, promoting muscle memory and empowering the person with dementia to maintain a sense of control over the activity. Overall, Hand under Hand is a valuable tool for caregivers, fostering a more supportive and comforting connection with those they care for.
Impact of HuH®
• Compared to the commonly used Direct hand and Hand over hand approaches, HuH® elicits the least amount of resistive behaviors while giving the person living with dementia a greater sense of participation in their daily care.”
The impact of Hand under Hand is that compared to the commonly used direct hand or Hand over Hand approaches, Hand under Hand elicits the least amount of resistive behaviors while giving the person living with dementia a greater sense of participation in their daily care.
HuH® Steps Via Pictures
Let's talk about what this looks like. An example is in Figure 2.

Figure 2. An example of Hand under Hand.
The Hand under Hand technique begins with a simple handshake. As illustrated, the caregiver initiates a handshake, then slides their hand up and around, lowering their fingers as if preparing for arm wrestling. The crucial shift occurs by turning the hand so that the caregiver's hand is positioned under the hand of the person living with dementia.
This intentional positioning allows the individual with dementia to feel a sense of control, fostering a more supportive and comforting connection. To recap the steps:
1. Initiate a handshake.
2. Slide your hand up and around.
3. Lower your fingers.
4. Rotate your hand so that it is underneath the hand of the person living with dementia.
This technique, known as Hand under Hand, serves as a versatile tool with numerous applications, offering a comforting and supportive connection during various activities, such as feeding, drinking, or personal care. Its simplicity and adaptability make it a valuable approach for caregivers seeking to enhance their interactions with individuals living with dementia.
Positive Physical Approach
- PPA is a method used to approach and connect with a PLwD.
- PPA is a way to ascertain if the PLwD is willing, comfortable, and has the ability to engage and interact.
- PPA uses the retained skills of the PLwD to do with, not to when supporting care.
The Positive Physical Approach (PPA) is a method consisting of six to nine steps designed to approach and connect with individuals living with dementia. Its goal is to minimize the likelihood of agitation and promote greater collaboration and comfort during interactions.
PPA serves as a systematic approach to assess whether a person with dementia is willing, comfortable, and has the ability to engage and interact, thus allowing caregivers to enter their environment and personal space. This method is centered on utilizing the retained skills of individuals with dementia, emphasizing doing with them rather than doing to them when providing care and support. By following the principles of PPA, caregivers can enhance the quality of their interactions and create a more positive and supportive environment for individuals living with dementia.
Impact of PPA™
- Care partners learn how to adjust their actions, and how to use this personal connection to encourage participation in care tasks or situations for improved quality of care and quality of outcomes.
The impact of PPA is that care partners learn how to adjust their actions and how to use this personal connection to encourage participation in care tasks or situations for improved quality of care and quality of outcomes.
PPA™ Steps via Pictures
Here are the PPA™steps (Figure 3).

Figure 3. Example of the PPA™ steps using role players.
In the Positive Physical Approach (PPA), the initial step involves carefully approaching the person with dementia. Begin by standing approximately six feet away, placing your open hand next to your face, and offering a warm greeting by name.
Extend your hand in a familiar handshake position, as handshakes are a lifelong custom that can capture their attention. If they reciprocate the handshake, approach slowly from the front with your hand extended. Gradually transition from the handshake to the Hand under Hand position, moving from the front to their side.
Assume a supportive stance when at their side, and if the person is seated, ensure you are at or below their eye level by kneeling or squatting. This approach fosters a more equal and less intimidating interaction.
While at their side, be mindful of personal space. Avoid leaning too far into their personal space, maintaining a distance that allows them to see you clearly and feel comfortable.
By following these steps, caregivers can initiate positive interactions with individuals living with dementia, reducing the likelihood of agitation and creating a more comfortable and collaborative environment.
Video: Putting It All Together
Here is a video example.

Video: Feeding Technique
Let's put this into play and see how we use that with a feeding technique.

In this scenario, the Positive Physical Approach (PPA) is applied to the feeding technique. By using Hand under Hand, the caregiver offers support and comfort during the meal. The joint pressure adds an extra layer of stability, creating a positive and collaborative experience. Additionally, adjusting the bowl's angle allows the person to participate more actively in the feeding process, promoting a sense of control and engagement.
Chat Time/Key Takeaways
Certainly, the Hand under Hand technique offers a versatile approach that extends beyond feeding. It can be seamlessly integrated into various caregiving activities.
- Dressing: Assisting with putting on clothes while using Hand under Hand for support.
- Grooming: Applying the technique when combing hair, shaving, or engaging in other grooming activities.
- Brushing Teeth: Offering support and guidance during teeth brushing with Hand under Hand.
- Bathing: Using the technique to provide assistance during bathing for comfort and control.
- Medication Management: Supporting individuals while taking medications, ensuring a positive experience.
- Engagement in Activities: Applying Hand under Hand during various activities to promote participation and collaboration.
By seamlessly incorporating Hand under Hand into different caregiving tasks, caregivers can elevate the overall experience for individuals living with dementia. This approach not only provides physical support but also fosters a sense of connection and empowerment, contributing to a positive and dignified care environment.
SNF Interventions
Training for Improved Care
- “Incorporation of PAC into current CNA curriculum may equip CNAs with the knowledge and skills required to provide better care, with the potential to improve the overall quality of life for persons living with dementia.”
- Dementia Collaborative Coaching showed preliminary positive outcomes for both CNAs and PLWD. It showed the intervention was acceptable, appropriate, and feasible for routine providers and warrants further study.
The incorporation of a Positive Approach to Care (PAC) into a Certified Nursing Assistant (CNA) curriculum has been shown in studies to equip CNAs with the necessary knowledge and skills to enhance the quality of care for persons living with dementia. Preliminary positive outcomes were observed in a study on Dementia Collaborative Coaching, indicating that the intervention was acceptable, appropriate, and feasible for routine providers, warranting further investigation.
Now, consider the impact when team members possess the skills required to care for patients and residents. When equipped with these skills, caregivers are more confident, providing better, more efficient, and effective care. They experience a heightened sense of purpose and carry out their duties in a more dignified manner. As therapists, it becomes evident that our skill set plays a crucial role in elevating the provision of care by care partners, ultimately increasing their comfort levels in caregiving.
Now, taking it a step further, think about how persons living with dementia respond when caregivers utilize these enhanced skills.
Video: Bathing
The provided link leads to a one-minute video demonstrating the impact of applying Positive Approach to Care (PAC) skills during the process of selecting someone for a shower or bath. The first half depicts a scenario without the use of PAC skills, while the second half showcases the application of PAC skills during the bathing process. Although the video might be a bit uncomfortable, it mirrors situations commonly encountered in professional settings.
As you watch the video, consider what might work to create a more comfortable experience for the person living with dementia. Some key highlights include:
- Creating a Supportive Environment: Wrapping a towel around the person for increased comfort and dignity.
- Tone of Voice: Using a soft and comforting tone of voice to promote a calming atmosphere.
- Communication: Getting down to the person's eye level when communicating; Using short phrases, and matching verbal and visual cues.
- Mobility Assistance: Enabling the person to participate in their mobility, especially if using a shower chair.
These highlights exemplify how implementing PAC skills can significantly enhance the comfort and dignity of individuals during care activities, extending beyond just bathing to various aspects of care provision.
Changes in Abilities
Figure 4 shows an overview of changing abilities.
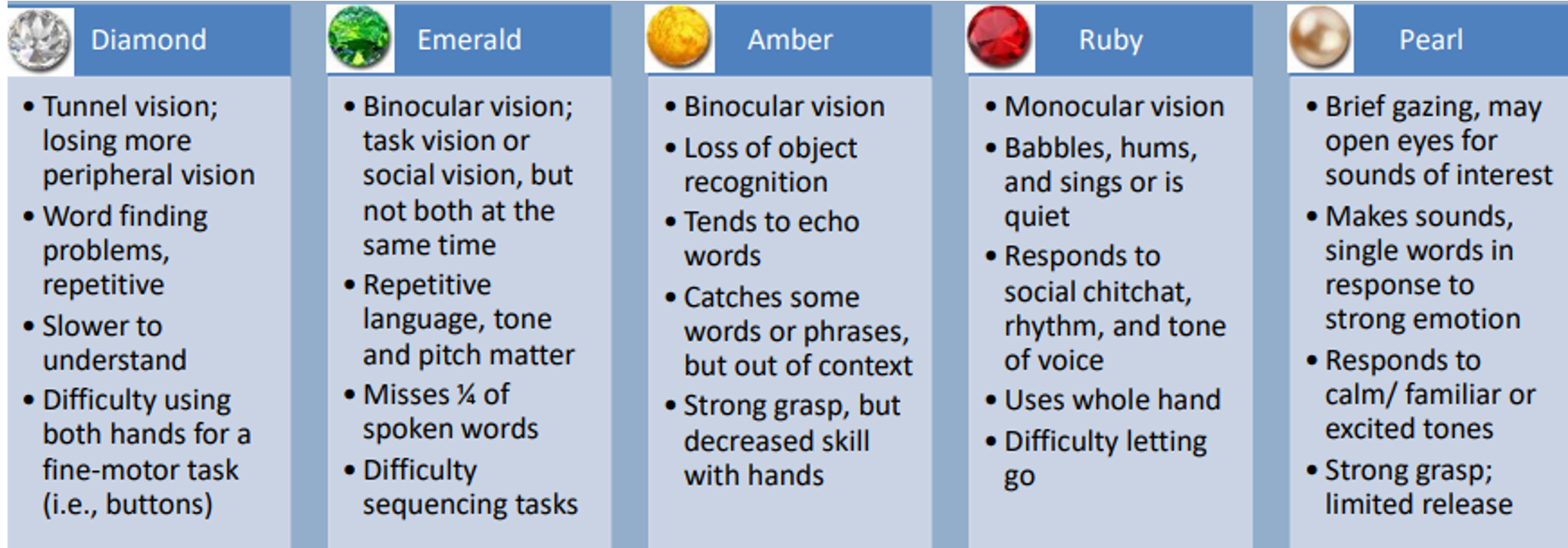
Figure 4. An overview of changing abilities.
I'm going to break this further down by vision, communication, and motor movements.
Changes in Vision
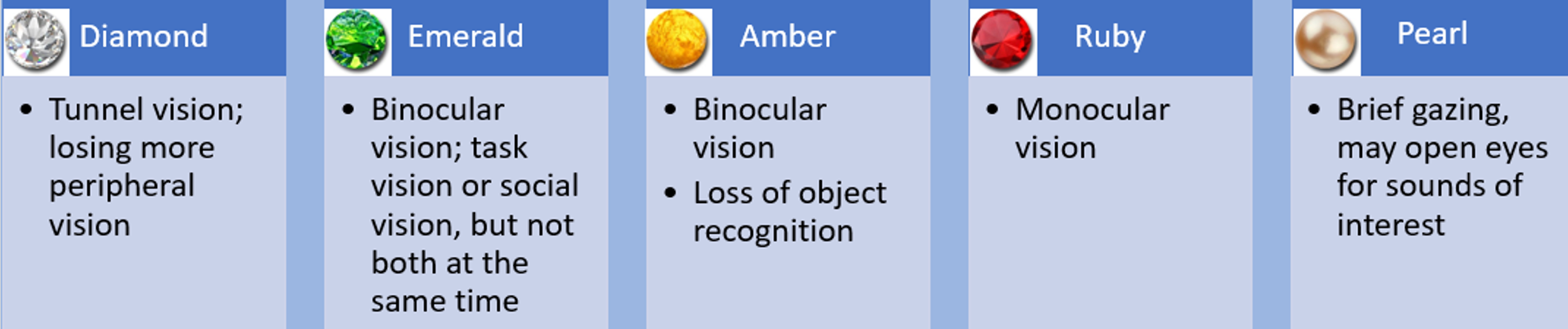
Figure 5. Vision changes by Gem states.
Let's explore visual changes associated with different GEMS states. As we age, around 50, we start losing peripheral vision. To demonstrate, extend your hands to the sides, wiggle your fingers, and observe when you start seeing them. This illustrates peripheral vision loss. In a diamond state, individuals experience tunnel vision.
Now, simulate this by creating a scuba mask with your hands around your eyes. Notice the narrowing of your visual field. These changes relate to visual disturbances in people living with dementia, beyond known conditions like glaucoma or macular degeneration.
Transition to an emerald state by forming binoculars with your hands. This represents task vision when looking down for a plate and social vision when looking up, reflecting the difficulty individuals face in shifting their focus. For ambers, who still have binocular vision, there's a loss of object recognition, making tasks trickier.
For rubies, close your left eye, maintaining monocular vision through the right eye. Experience the challenge of visual perception with only one eye open, emphasizing why fall risks increase.
Now, for pearls, keep monocular vision and make the hole smaller, representing brief gazing. This aligns with their tendency to open their eyes to sounds of interest. Understanding these visual perspectives enhances empathy and informs caregiving approaches.
Changes in Communication
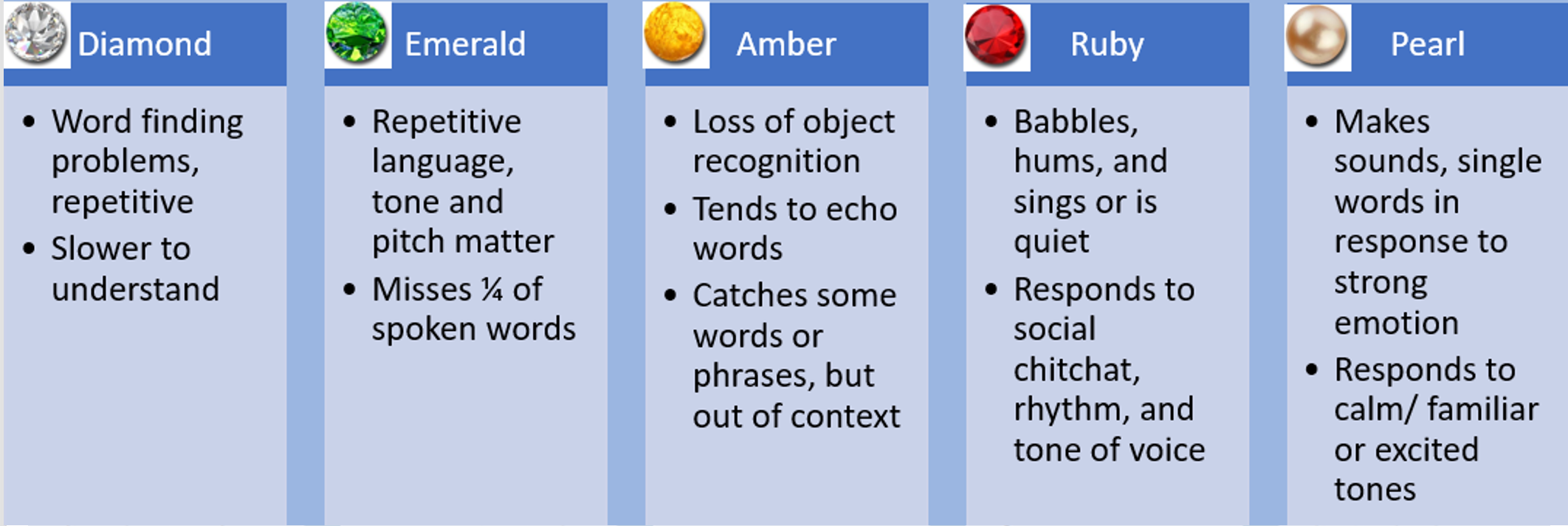
Figure 6. Communication changes by Gem states.
In each GEMS state, communication presents unique challenges and characteristics:
For Diamonds, word-finding problems, repetitive speech, and slower comprehension are common.
Emeralds exhibit repetitive language, where tone and pitch significantly impact communication. They begin to miss every fourth word, necessitating concise and incremental dialogue.
Ambers face a loss of object recognition, leading to echoing words and grasping phrases out of context.
Rubies may babble, hum, or sing, drawing on the retained rhythm in the right side of the brain. They respond to social chitchat and varying tones, potentially being quiet and withdrawn.
Pearls may utter single words and respond to strong emotions. They react positively to calm, familiar, or excited tones. Recognizing these communication patterns aids caregivers in tailoring their interactions for better understanding and connection.
Changes in Motor Movement
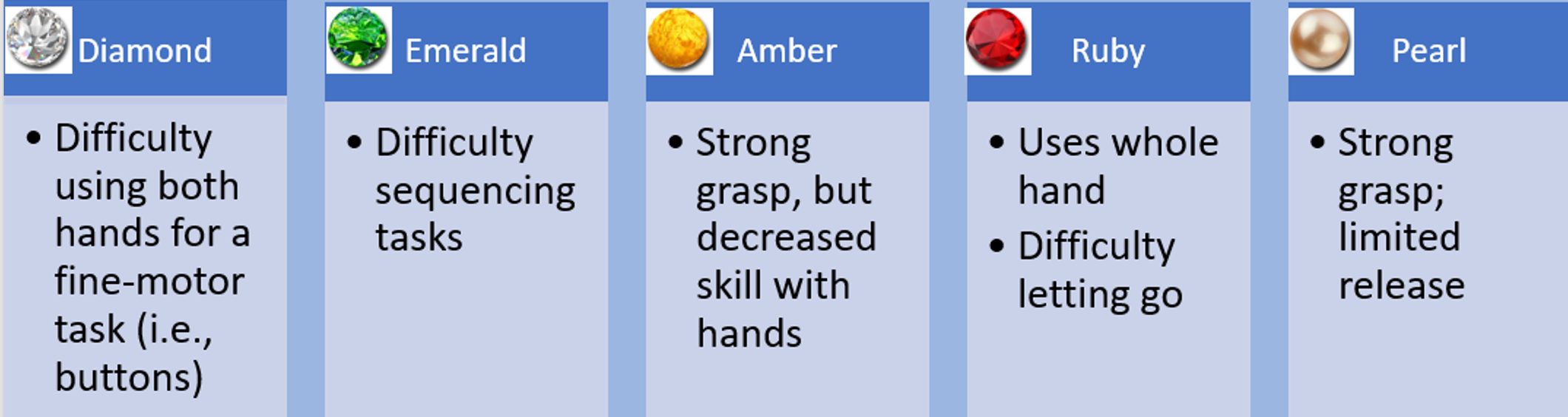
Figure 7. Motor movement changes by Gem states.
In each GEMS state, there are specific challenges related to fine motor skills.
Diamonds struggle with tasks requiring both hands, such as buttoning.
Emeralds face difficulties in sequencing tasks due to cognitive processes.
Ambers have a strong grasp but diminished hand skills.
Rubies use the whole hand, struggling to isolate movements and release. Substitution, not subtraction, is advised.
Pearls exhibit a strong grasp with limited release, contributing to contractures in later stages. Understanding these challenges is crucial for providing appropriate support and care.
Video: Connecting With Rubies and Pearls
Now, here's another video, a longer one, but highly informative, focusing on rubies and pearls.
As you watch someone working with a ruby, considering their visual, language, and motor skills, think about what strategies might be effective. Take a moment, about 20 seconds, to ponder this. For instance, going slow is crucial, providing ample time for processing. Kneeling in front of them ensures you're within their visual field, considering they're likely seated. Notice in the video that minimal talking is involved. Remember, with rubies, red means stop, where people often overlook possibilities. Yet, with appropriate support, you can establish a powerful connection.
PLwD and Motor and Procedural Memory
Persons living with dementia often face challenges in completing tasks due to the loss of memory for how to perform them. An occupational therapist emphasizes that leveraging familiar objects taps into procedural memory, which remains relatively intact throughout the disease process. Combining this approach with Hand under Hand technique helps maximize their functional abilities. Additionally, using verbal, visual, and tactile cues proves to be a supportive technique in enhancing their engagement and performance.
Environmental Modifications
Let's talk about some environmental modifications.
- Music
- Physical adaptations
- Aromatherapy
- One-on-one activities
- Safety
- Labeling/visual cues
- Spatial layout
- Lighting
- Routines
Reviewing key strategies for environment modification to facilitate engagement and maximize function:
Utilize music for cognitive, behavioral, and psychosocial benefits. Rhythms, retained in dementia, can support language, mobility, and balance through activities like dancing, tapping, and playing instruments.
Incorporate essential oils like lemon, rosemary, lavender, and orange to improve cognitive function and reduce agitation, enhancing mood for individuals with dementia.
Recognize the importance of tailored activities, considering the individual's preferences and sensitivities, to avoid overstimulation or understimulation.
Knowing personal details about the individual, such as their past work, hobbies, and military service, helps create meaningful interactions and activities.
Implement visual cues by labeling drawers, closets, exits, bathrooms, and other areas, reducing confusion and supporting daily activities.
Consider the layout of the environment, especially when individuals transition to a new setting. Mimic familiar arrangements to positively impact mood, behavior, safety, and cognition.
Pay attention to lighting, ensuring sufficient light while being mindful of shadows to prevent visual confusion and potential hallucinations.
Understand and maintain the individual's previous routines for activities like showering and teeth brushing, as consistency is crucial for individuals with dementia.
Recognize the correlation between brain plasticity and stimulating environments, emphasizing the positive impact on an individual's quality of life.
All About Function
- Self Care Skills (ADLs)
- Household/Community Activities (IADLs)
- Leisure Pursuits
Consider the progression of dementia and its impact on late-loss ADLs. Understand the contributing factors to these losses and recognize how your skillset can be instrumental in maximizing function with the remaining abilities of individuals with dementia. Leverage your knowledge to approach ADLs, IADLs, and leisure pursuits in a way that aligns with the unique needs and challenges posed by dementia. This holistic understanding empowers you to provide more effective and compassionate care tailored to the individual's evolving condition.
Cueing
Hierarchy
- Visual
- Verbal
- Physical/Touch
A cueing hierarchy includes visual, verbal, and touch, including Positive Physical Approach and Hand under Hand.
Putting the Cues to Work
- Use visual combined verbal (gesture/point)
- “It’s about time for… “
- “Let’s go this way…”
- “Here are your socks…”
- Don’t ask questions you don’t want to hear the answer to
- Acknowledge their response/reaction to your information
- Limit your words – Simple is better always
- Wait, Pause, Slow Down
Use a combination of visual and verbal cues in your communication. Incorporate gestures or pointing to enhance understanding. Keep your instructions simple and direct, avoiding unnecessary questions. Acknowledge and respond to their reactions and responses to the information you provide. Recognize the importance of limiting your words, especially as cognitive decline progresses. Understand that starting from an emerald state, individuals may begin to lose every fourth word, so simplicity is key. Embrace moments of silence and avoid the urge to fill them, allowing individuals time to process information at their own pace.
If, at first, you don’t succeed...
- Stop
- Back off
- Think it through
- Re-approach
- And do something different
If initial attempts are unsuccessful, it's crucial to pause, step back, and reconsider your approach. Be flexible and open to adjusting your plans based on the individual's needs and responses. Recognize that your agenda may not align with their priorities, and it's essential to adapt to their pace and preferences. Remember that effective communication and interactions involve a two-way dynamic, and your actions can influence the outcome.
Video: Oral Care with a Pearl
Adapting and being responsive to the individual's needs is crucial, especially with someone like a pearl. In the described scenario, Teepa demonstrated the importance of patience, adjusting her approach when the initial attempt didn't work. Applying gentle tactile and verbal cues, providing support at the joint, and allowing Edna the space to willingly engage all contributed to a positive outcome. It emphasizes the significance of recognizing and respecting the unique preferences and responses of individuals in the pearl state.
Summary
Team Collaboration
- As clinicians, we are a valued part of the team.
- The person living with dementia is the “expert” by experience.
- Our actions and reactions can change the outcome of the situation.
- It is critical to know the person with whom you are working - all the ins and outs, likes and dislikes, and what matters most to them.
Recognizing the expertise of the person living with dementia is fundamental. While we, as clinicians, bring valuable skills and interventions to the table, it's crucial to empower and educate the entire care team, including CNAs. This collaborative approach ensures a more holistic and sustainable care environment. Understanding the unique experiences and perspectives of individuals living with dementia helps tailor interventions to better meet their needs and enhances overall care. It's not just about providing solutions but fostering a supportive and informed community around those affected by dementia.
Effective Partnering
- Providing care to someone living with dementia may get a job done, but it fails to see the person as a whole person. We advocate for providing care with those living with dementia. This may be a small word shift, but it is an important distinction that takes into account the values and preferences of the person for whom we are caring.
The shift from providing care to partnering with those living with dementia is not merely a semantic change but a profound shift in perspective. It emphasizes the importance of recognizing the individuality, values, and preferences of the person receiving care. By understanding the person as a whole, with their unique background, culture, and values, a more meaningful and collaborative relationship can be established. This approach fosters a sense of shared responsibility and empathy, creating a more supportive and enriching care environment for individuals living with dementia. It's not just about completing tasks; it's about honoring and respecting the personhood of each individual.
Steps for Success
- Know the person and the situation.
- Match your help to remaining abilities.
- Know their GEMS state and understand this can be fluid.
- Treat the symptoms.
- Connect through emotions and senses.
- The presence, grace, kindness, and gentle approach of the care partner will be felt even if the words cannot be comprehended.
Knowing the person, understanding their GEMS state, and connecting through emotions and senses are crucial aspects. The focus on how you make them feel, rather than the words spoken, is a fundamental principle in dementia care. The presence, grace, kindness, and gentle approach contribute significantly to the well-being of individuals living with dementia.
From a PLwD Perspective
- “Christine Bryden, who writes about her own journey with dementia, reminds us that all is not lost. The human soul, the human treasure is always still there. As we [persons with dementia] become more emotional and less cognitive, she writes, it’s the way you talk to us, not what you say, that we will remember. We know the feeling but don’t know the plot. Your smile, your laugh, and your touch are what we will connect with. Empathy heals. Just take us as we are. We’re still in here, in emotion and spirit, if only you could find us.”
Christine Bryden's perspective is incredibly powerful and insightful. Her emphasis on the enduring human soul and the importance of emotional connections despite cognitive challenges is a poignant reminder. The emphasis on how we communicate, the non-verbal cues, and the emotional connections are what individuals with dementia often remember. The recognition of the emotional and spiritual presence within individuals living with dementia is a call for empathy and understanding.
Questions and Answers
Do these traits apply to all types of dementia or just Alzheimer's disease?
There are 120+ different types of dementia. Alzheimer's is the most common one, but these traits, GEMS states, Hand under Hand, and a positive physical approach can all be used. Each dementia type may present differently, so it's crucial to adapt strategies.
Is this getting taught in OT schools currently?
It varies across schools, and lifelong learning is crucial. Some programs may cover it, but it's recommended to add these skills to your toolbox for effective dementia care.
What about writing goals?
Goals remain the same, focusing on functional outcomes. Strategies like Hand under Hand can be specified for caregiver carryover to achieve functional success.
Which stage is too late to introduce adaptive equipment?
There's no one-size-fits-all answer. Even at later stages, adaptive equipment, introduced with support at the right time, can enhance function. It's about trial and individualized approaches.
Any measurable goals, such as one task completion by 50% of the time?
Absolutely. Incremental goals, like task completion, are effective. Tailor goals to the individual's abilities and aim for measurable progress.
Are there structured training programs about these approaches currently being offered at SNFs for CNA staff?
Training programs vary, and individualized and organizational training is crucial for effective implementation.
What Gem level would not be appropriate to return home from a skilled stay?
Gem-level considerations are subjective. It depends on individual factors, the support available, and the unique needs of the person. Outside-the-box thinking is essential.
References
Content provided by Positive Approach is used with permission and based on the GEMS® and the techniques, strategies, and overall approach to care created and developed by Positive Approach, LLC. www.teepasnow.com. This content is based on the work of Teepa Snow's Positive Approach to Care® methods and education.
Allen, J., Caiquo, J., Sumner, M., and Tawil, A. S., & Mele, J. (2021). Environmental modifications for dementia care. Retrieved from https://repository.stanbridge.edu
Brown, J., Reddy, P., Nwakasi, C., Nolan, B., Snow, T., & Ehlman, K. (2020). Dementia knowledge and caregiving skills improvement from using the PAC Model: A pilot comparative evaluation. Innovation in Aging, 4(Suppl 1), 89. https://doi.org/10.1093/geroni/igaa057.293
CDC. (n.d.). The truth about aging and dementia. https://www.cdc.gov/aging/publications/features/Alz-Greater-Risk.html
Dixon, E., Anderson, J., & Lazar, A. (2022). Understanding how sensory changes experienced by individuals with a range of age-related cognitive changes Can effect technology use. ACM transactions on accessible computing, 15, 10.1145/3511906. https://doi.org/10.1145/3511906
Douglas, N. F., Browning, S., & Claypool, K. (2023). Preliminary evidence for dementia collaborative coaching. American journal of speech-language pathology, 32(5), 2146–2157. https://doi.org/10.1044/2023_AJSLP-22-00367
https://freesound.org
Citation
Walther, L. (2023). Skilled nursing facility interventions: An introduction to Teepa Snow and positive approach to care. OccupationalTherapy.com, Article 5657. Available at www.occupationaltherapy.com
