Editor's note: This text-based course is a transcript of the webinar, Skilled Nursing Facility Interventions: Positioning Around The Clock Matters, presented by Tamara Kittelson, MS, OTR/L, ATP/SMS.
Learning Outcomes
- After this course, participants will be able to recognize the interaction of 3 forces impacting development of posture problems like kyphosis and flexion contractures.
- After this course, participants will be able to compare and contrast destructive unsupported and healthy supported lying postures for persons with limited mobility.
- After this course, participants will be able to identify the unique characteristics of individuals with dementia that increase their need for posture support day and night.
Introduction
It's good to be here, and I'm excited to have a chance to share this topic with this particular audience. My daughter, Eleanore, has been gone for about 22 years now, but she taught me an awful lot about living with a loved one with a disability as part of the family. These are the sort of lessons that you don't learn when you're in OT school. I always like to give her credit as my best teacher.
Lying Posture
- Most people spend 1/3 of their time in a lying orientation for rest and sleep (including sofas and recliners).
- In SNFs, this may be even more prevalent and contributes to altered body shapes.
- Health and therapy goals are more readily attained and maintained with a symmetrical, balanced body.
Discussing lying posture is essential due to the significant amount of time individuals spend in a lying orientation for rest and sleep, constituting about one-third of their daily activities. This prevalence is potentially even higher in Skilled Nursing Facilities (SNFs), contributing to alterations in the body shapes of residents.
It is crucial to emphasize the importance of maintaining a symmetrical and balanced body for achieving and sustaining health and therapy goals. A body's natural state is typically symmetrical at birth, and aligning with this balance is fundamental for overall well-being.
While I haven't worked directly as an SNF therapist, I firmly believe that the principles governing the human body remain consistent across populations. Despite not specializing in SNF therapy, I have dedicated myself to updating my knowledge and conducting research to understand the unique characteristics of individuals in SNFs. This includes those with chronic long-term disabilities and individuals with dementia. I am particularly interested in exploring how proper positioning, both during the day and night, can contribute to the well-being of individuals in these settings.
24 Hours Per Day: Three Human Postural Orientations
- Lying – first and foundational
- Sitting
- Standing
In our daily allocation of 24 hours, three fundamental human postural orientations shape our interactions with the environment. As therapists, our focus often centers on sitting and standing orientations, addressing functional tasks individuals engage in throughout the day. However, I propose that lying is the primary and foundational postural orientation, as it constitutes our initial state when we are born.
During the natural course of development, individuals progress through milestones, moving from lying to sitting, standing, walking, and performing various activities of daily living. The developmental journey is expected to unfold as we grow.
In the United States, there appears to be a significant oversight regarding the lying orientation. While much attention is given to sitting and standing, there is a tendency to neglect the importance of lying. In contrast, some parts of the world recognize the crucial role of learning to lie in balance and control posture. This emphasis acknowledges that success in sitting and standing is closely linked to mastering the lying posture.
Today, I aim to shed light on the significance of lying as a foundational postural orientation. I hope to illustrate that by understanding and refining lying posture, we can contribute to individuals' success in sitting and standing, fostering a comprehensive approach to posture management.
What Does 24 Hours in a Day Really Mean?
Figure 1 shows a graphic that was made by a friend of mine with whom I co-presented.
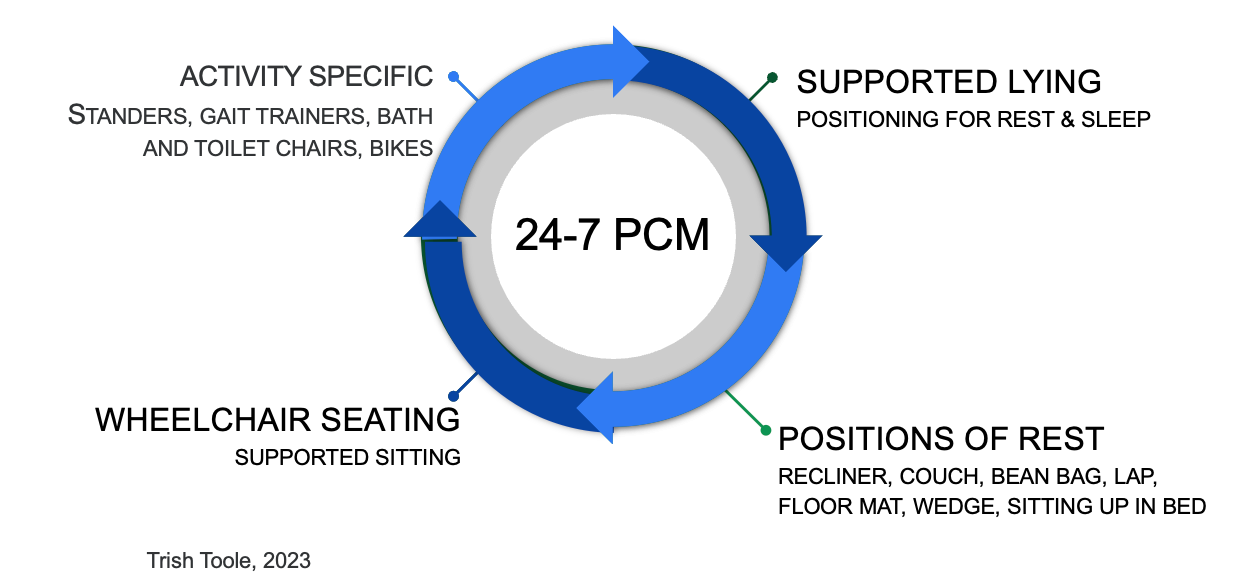
Figure 1. Illustration of what a 24-hour day may look like.
Throughout the day, individuals may find themselves in various postural orientations, depending on their activities and needs. Some individuals may spend a portion of their day in wheelchair seating or supported sitting, with the duration varying based on individual circumstances. Specific activities may involve the use of standing frames, bath and toilet chairs, gait trainers for younger populations, or walking frames for those in skilled nursing facilities.
There are also periods of rest where individuals may be in a recliner, on a couch, sitting up in bed, or in other positions, not necessarily sleeping but taking a break. One crucial aspect that often goes unnoticed is supported lying, a topic we will extensively cover today. This pertains to positioning for deep rest and sleep, a critical component of overall well-being.
It's worth noting that the assumption that everyone can comfortably lie on a flat bed at night is not always applicable. Today, we'll delve into the importance of considering and optimizing the positioning for deep rest and sleep, recognizing that individual comfort and well-being during these periods are vital aspects of overall health.
Posture Care Management (PCM)
- “A postural management programme is a planned approach encompassing all activities and interventions which impact on an individual's posture and function…” (Gericke et al., 2006)
- This statement focused on children with cerebral palsy – but a human body is a human body!
The definition provided, published in 2006 and authored by Tina Gericke in collaboration with a multidisciplinary team, emphasizes the importance of 24-hour posture management for children with cerebral palsy (CP). This consensus statement involves therapists, nurses, physicians, and others who recognize the significance of comprehensive posture management for children with CP.
What I would like to emphasize is that while the context of the definition is specific to children with cerebral palsy, the underlying principles are applicable to any human body. The forces and considerations discussed today regarding posture management will impact individuals of any age and with various diagnoses or conditions. The ability to move easily in and out of a diverse range of positions is crucial for the well-being of the human body, irrespective of age or specific health challenges.
Who Benefits From 24-hour PCM?
- People who:
- have a limited movement repertoire
- are unable to easily change position independently
- will develop contractures/distortions
- This is for many less active elderly people in skilled nursing facilities.
The focus of our discussion today will center around individuals with what I refer to as a "limited movement repertoire." I will illustrate and define this concept, providing you with a tangible understanding. As you follow along, I encourage you to reflect on individuals you may have encountered in your professional experience to see if this concept resonates with their situations.
Individuals with a limited movement repertoire face challenges in independently and effectively changing positions with sufficient variety. This limitation can lead to the development of contractures and distortions. This issue is particularly relevant for less active elderly individuals in skilled nursing facilities, where mobility may be compromised, and individuals may find themselves stuck in certain positions, somewhat beholden to the effects of gravity. Today, we'll delve into the implications of this limited movement repertoire and explore strategies to address and mitigate its impact on individuals' well-being.
Understanding Postures
Let's look at different postures.
Sitting
Here are some images of sitting postures (Figure 2).
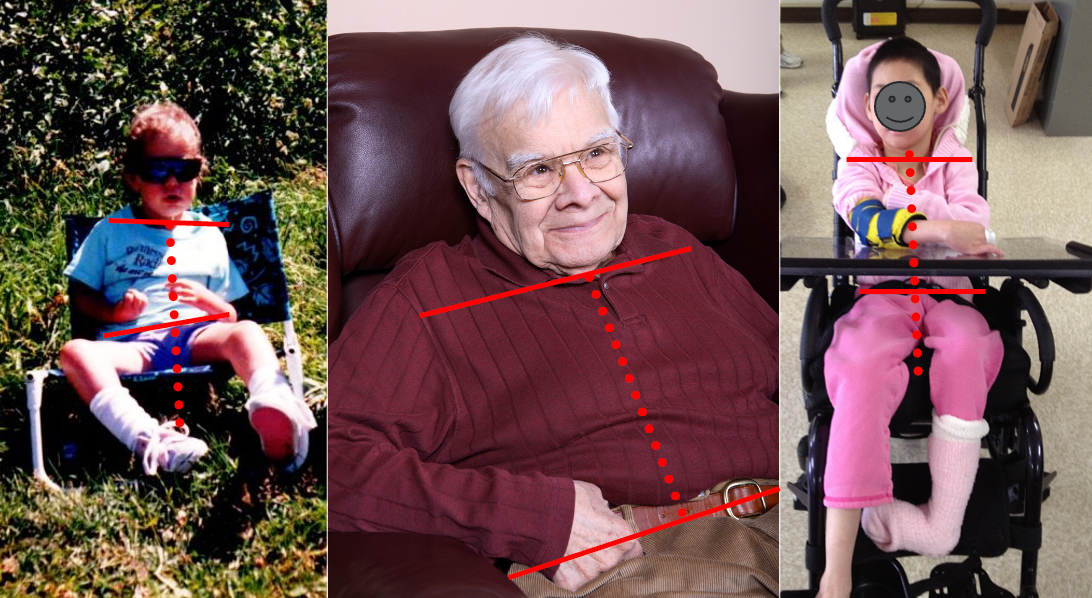
Figure 2. Examples of seated postures.
In the images on the left, you can observe my daughter Eleanore during her early years. She is visibly struggling to maintain an upright posture, dealing with asymmetrical tone while sitting in an unsupportive chair during a camping trip. On the right, BaoNHia serves as a contrast, sitting in a highly supportive environment with shoulders level over her pelvis, exhibiting good midline orientation. The stability provided allows her to engage with her surroundings comfortably.
Now, let's shift our attention to an elderly gentleman seated in a recliner. I must express a strong bias against recliners, particularly those adorned with large, plush head pillows. These pillows tend to push individuals' heads forward, encouraging a slouched posture, as evident in the gentleman's position. I perceive recliners as potential contributors to what I term a "kyphosis machine," poised to induce undesirable postural changes.
In subsequent slides, I will elaborate on how habitual lying postures can exacerbate this kyphosis machine concept, promoting flexed postures that may impact overall posture and well-being.
Standing
Figure 3 shows some standing postures.
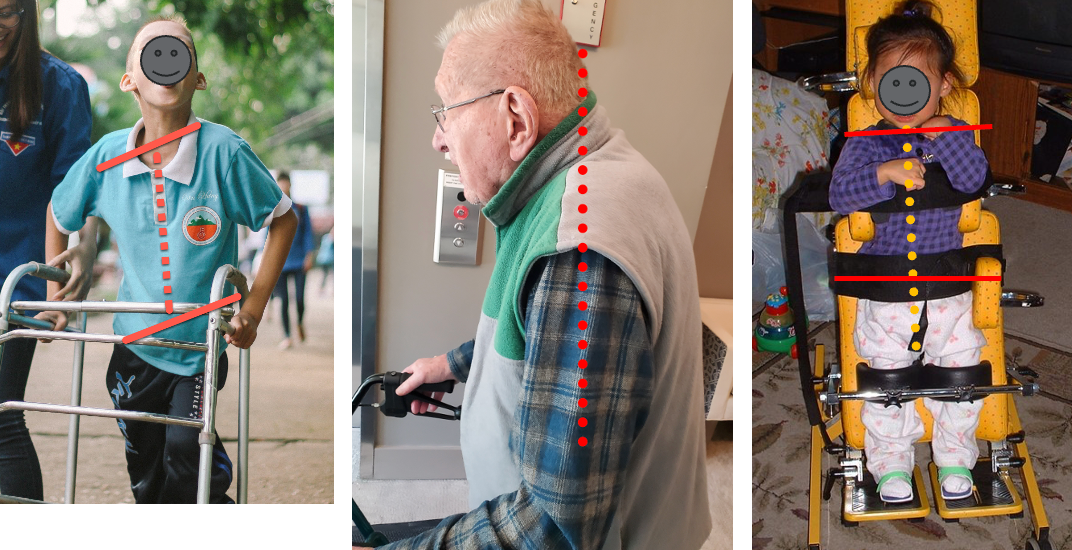
Figure 3. Examples of standing postures.
In the image on the left, you can observe a young boy who is working hard to stand up in a stander, displaying noticeable asymmetry in his posture. On the right, BaoNHia is provided with comprehensive support, allowing her to stand with good alignment.
The middle shows my father, who lived with dementia for several years and passed away in April. This photograph was taken a week before his final fall. My father, a once very straight and erect man who enjoyed activities like downhill skiing and water skiing, became more sedentary as the years went by. Spending extended periods in a recliner and adopting a curled-up sleeping position contributed to the development of a kyphotic, rounded shoulder posture, as evident in the image. As his daughter, having witnessed his gradual shift from a more upright stance to this kyphotic posture, I can attest that this change occurred over time and was not indicative of his lifelong posture.
Lying
Lying postures are shown in Figure 4.

Figure 4. Examples of lying postures.
In the image on the left, we have Dominic lying down at the age of 15, showcasing his habitual sleeping posture. His legs are inclined to one side, causing a twist in his upper body due to tightness in his legs and knee flexion contractures. The inability to fully straighten his legs prompted them to seek support, resulting in asymmetry. In the image on the right, taken during a home visit, you can see the transformation when using simple materials like roll towels and cushions. With supports at his sides and a cushion under his knees to address the contractures, Dominic achieved a more symmetrical and midline orientation for rest. This example emphasizes that individuals like Dominic can achieve symmetry with proper postural supports.
The other images show common postures that many elders, and possibly many of us, tend to adopt. These postures often promote asymmetry, flexion, and a forward head position, which we aim to mitigate. I encountered clients in Missoula, Montana, where I had my practice for many years. An internist's observation about older patients frequently looking down inspired a trial of posture care management. This led to significant insights into the effects of habitual side sleeping, curled-up positions, and extended time in recliner chairs that encourage forward head postures—topics we'll explore further today.
Linked - Lying, Quadruped, Sitting, Standing

Figure 5. Examples of postural deformities in different positions.
In Figure 5, we observe a client showcasing a consistent postural tendency across various positions. On the left, you can see the client lying in bed, displaying a sloped shoulder and trunk curve. This pattern persists in quadruped, unsupported sitting, and even in the standing frame before we implemented improved trunk support. This consistent presentation is indicative of a limited movement repertoire.
While this example involves a child with disabilities, it's important to recognize that similar postural tendencies are observed in adults with acquired injuries, dementia, and various other situations. There is often a prevailing postural inclination in lying that may favor one side over the other, leading to asymmetry in chest and leg positions. It's noteworthy that these tendencies may align or go in opposite directions, but the common thread is a restricted movement repertoire that manifests across different positions.
Limited Movement Repertoire
This is a little girl that I worked with in 2017 with Eleanore's Project in Peru (Figure 6).

Figure 6. A child with postural deformities while lying on a mat.
In the process of waiting for her wheelchair modifications, I had the opportunity to observe her over an extended period and capture a series of photographs. During her naps, she would occasionally shift positions. In the bottom-left image, I briefly hoped she might change her typical direction, but she consistently landed in the same orientation. This illustrates the concept of a limited movement repertoire, where individuals tend to consistently adopt a specific orientation and spend extended periods in that position over hours, weeks, months, and, ultimately, years. This persistence in a particular posture can have long-term effects on an individual's musculoskeletal alignment and overall well-being.
Lying and Sitting Are Linked
In the case of this little girl, you can see that even though she was only three years old, she was receiving her first wheelchair. Already, all the years of spending time in that preferred lying orientation posture have made a difference in how she is sitting in this chair.

Figure 7. Showing the same client lying and sitting in a wheelchair.
In the case of this three-year-old girl receiving her first wheelchair, the impact of spending significant time in a preferred lying orientation posture is evident. Even at her young age, the influence of those years is reflected in how she is positioned while sitting in the chair. This underscores the importance of early intervention and thoughtful consideration of postural habits, as they can have lasting effects on an individual's musculoskeletal alignment and functional abilities, even at a very young age.
24-Hour Posture Care Management – What is Needed?
- Understanding:
- What is happening or will happen to the body
- Careful attention to all postures and activities
- Day and night
- Analysis of lying and sitting positions
- They are linked
- A team approach
To make the management of postures successful, several crucial elements come into play. Firstly, there is a need for a comprehensive understanding of the changes that occur or may occur in the body. This involves careful observation and analysis of postures and activities, both during the day and at night. It is essential to recognize the interconnectedness of lying and sitting positions, understanding that they are not independent of each other. Additionally, adopting a team approach is crucial for success.
In a skilled nursing facility (SNF) setting, achieving a unified team approach can be challenging, especially in aligning certified nursing assistants (CNAs) and nursing staff with therapy goals. Acknowledging the difficulties in this alignment is based on limited experiences and numerous comments shared during courses and workshops. Addressing these challenges and fostering collaboration within the team is essential for effective posture management in SNF settings.
How Do Distorted Body Shapes Occur?
How do distorted body shapes, as seen in Figure 8, occur over time?

Figure 8. A boy with distorted body shapes on a mat.
The mirror image presented here depicts an individual I worked with extensively, who spent his formative years in an institution in Boulder, Montana. While his circumstances differ from those of individuals who have experienced able-bodied growth and later face conditions like dementia, strokes, multiple sclerosis, or Parkinson's, the underlying principles remain consistent because a human body is a human body.
In this example, the individual is in a supine position on the right and a prone position on the left. Despite the different orientations, his body shape maintains a C-shape due to the impact of gravity over time, flattening his body against the support surface. This phenomenon is often referred to as the "human sandwich effect," a term coined by Noreen Hare, a physiotherapist from the United Kingdom and one of the pioneers of this approach. The concept visualizes the constant interaction between the human body, the support surface (such as the floor, chair, or bed), and the force of gravity acting upon us, creating a dynamic interplay that significantly influences our posture and well-being.
Gravity, Immobility, and Time- 1976
- Fulford and Brown - Identified the cause of “deformities” thought to be unavoidable as resulting from habitual postures and the effects of gravity over time in babies with CP.
- They called this postural or positional molding.
- A human body is a human body! It can happen to anyone with mobility impairment.
(Fulford and Brown, 1976)
The concept of postural or positional molding was first discussed in 1976 by two Scottish doctors named Fulford and Brown. They aimed to understand and address the deformities thought to be unavoidable in babies, kids, and people with cerebral palsy (CP). To investigate, they studied two cohorts of babies: one with severe CP and another with typically developing infants.
Over the course of months, Fulford and Brown observed similarities in the postures and orientations of the babies as newborns. However, as time progressed, they noted a divergence in the postures of the two groups. Typically developing babies achieved milestones, developed anti-gravity responses, and demonstrated a reduction or disappearance of asymmetries. In contrast, babies with CP became increasingly asymmetrical and often got stuck in those positions.
They termed this phenomenon postural or positional molding, focusing on babies with CP. Yet, the conviction is that the principles are applicable to any human body with mobility impairment. Based on observations, it is believed that nobody is immune to the potential impact of postural molding, emphasizing the importance of proactive intervention for individuals with mobility challenges.
The Premise
- Altered body shapes are caused by:
- Asymmetrical, habitual postures
- Gravity
- Time
- “A human body is a human body.”
The premise put forward by Fulford and Brown is that altered body shapes are a result of three key factors: asymmetrical habitual postures, gravity, and time. These forces collectively impact individuals who have a limited movement repertoire, which can stem from various reasons, including but not limited to diagnosis-related factors.
The focus has shifted from concentrating solely on diagnoses to a more comprehensive consideration of postures and their evolution over time. By understanding the impact of asymmetrical postures influenced by gravity and time, it becomes possible to appreciate the effects on an individual's body shape.
One notable aspect highlighted is the potential for the body to bounce back to its original shape with frequent position changes, as illustrated by the examples of my dog in Figure 9. This underscores the importance of proactive and intentional position changes in mitigating the effects of asymmetrical postures over time.

Figure 9. Examples of postural changes in a dog.
He can go into just any posture, but he goes back to the beginning shape. However, when movement is limited, eventually, the body does not bounce back. This is the difference between this baby on the left and my former client, Ken, on the right (Figure 10).

Figure 10. Examples of different body shapes- flexible vs. rigid.
Ken, who was raised in an institution, didn't have opportunities for interventions and positioning like we would hope he would have today. He spent lots of time in an asymmetrical posture, where he got flattened and stuck. The baby on the left is showing an asymmetrical tonic neck reflex, which we know is normal for her stage of life. In a minute, she's going to roll over, do something different, and things are going to be okay.
We see these fixed deformities in Abdullah in Figure 11.

Figure 11. Fixed postural deformities.
The images depict a 17-year-old boy with cerebral palsy (CP) whom I worked with in the Middle East in 2007 through Eleanore's Project. He is positioned in an obligatory asymmetric lying posture, which was the only available option for him at that time. Over the course of 17 years, the impact of this posture on his body is evident. One side of his body has become overstretched, while the other side has experienced soft tissue shortening, leading to micro-tears and subsequent lengthening.
In the second image, the boy's mother is pointing to his rib cage, expressing concern about the connection between his pelvis and rib cage. This illustrates the severe distortions that can occur when a person's body is consistently flattened against a surface. While such extreme distortions may not be common in many skilled nursing facility (SNF) patients, there is a possibility of encountering varying degrees of distortions, depending on factors such as the individual's upbringing, the circumstances leading to their presence in the SNF, and the quality of care they have received.
Figure 12 shows more images that provide valuable insights into the effects of prolonged asymmetric postures on individuals with mobility challenges.
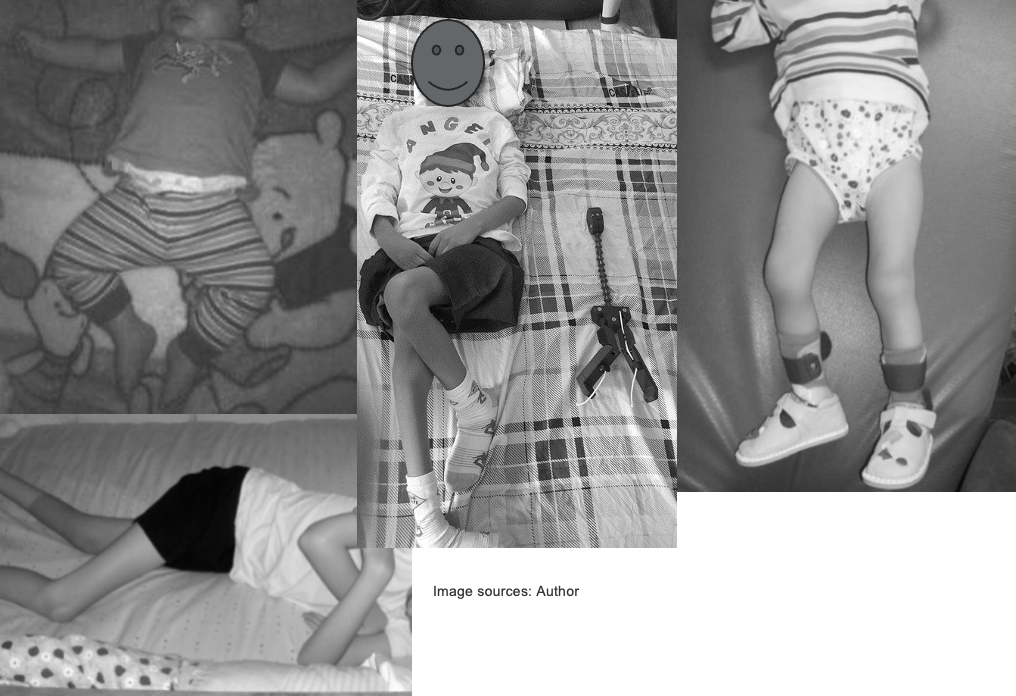
Figure 12. Other images of postural deformities.
The images illustrate different leg postures commonly observed in individuals with mobility challenges. When individuals have tight hip flexors or knee flexion contractures, their legs may adopt specific positions to find support or relief. In the center image, the boy demonstrates tight adductors, causing his legs to turn inward. On the right, the girl showcases a "wind-swept" posture, where both legs tend to move to the same side. In the top image, the boy exhibits abduction of the legs, pointing outward. These postures are indicative of the adaptive responses the body adopts in the presence of muscle tightness or contractures, emphasizing the importance of addressing these issues to prevent prolonged deformities and promote musculoskeletal health.
Lying & Sitting Postures– Fetal Tendency
There can be all kinds of combinations of asymmetries, especially due to a fetal tendency, as shown in Figure 13.
Figure 13. Examples of flexed and fetal-type postures.
Cognitive Impairment, Posture, and Balance
- Studies suggest impaired balance and gait are early signs of mild cognitive impairment.
- One study suggested this can be improved with therapy.
(dos Santos Ferreira et al., 2016)
The discussion now turns to the relationship between cognitive impairment, posture, and balance, incorporating recent insights from international research. Notably, the information presented here draws from sources in Belgium, Taiwan, and other countries, as there were limited references from United States sources on these topics.
Several studies, listed in the provided references, indicate that impaired balance and gait serve as early signs of mild cognitive impairment. Recognizing these changes early on becomes crucial, given that mild cognitive impairment often serves as a precursor to dementia. The implications of these findings suggest that targeted therapy, initiated during the mild cognitive impairment stage, could potentially slow down or mitigate the progression toward more severe cognitive decline.
For further exploration and access to these studies, the references provided in the reference list can be consulted, and many of them may be accessible through platforms like ResearchGate or Google Scholar for those without library access.
Contractures and Participation
- Joint contractures and osteoarthritis are common in the elderly population and limit mobility.
- This limits social participation and quality of life.
- Joint contractures in upper and lower limbs increased the risk of activity limitations, compared to upper limbs only.
(Chen et al., 2022)
Another study highlighted in the presentation focuses on joint contractures and osteoarthritis in the elderly population. The study underscores the impact of joint contractures in both upper and lower limbs, emphasizing the increased risk of activity limitations associated with such conditions. The presence of joint contractures, whether in the upper or lower body, contributes to limitations in daily activities, thereby affecting social participation and overall quality of life for individuals. This information highlights the multifaceted impact that musculoskeletal conditions can have on an individual's functional abilities and well-being.
Paratonia and Dementia
- “Paratonia is a dementia-induced motor abnormality. Although paratonia affects virtually all people with dementia, it is not well known among clinicians and researchers.”
- Dementia affects perceptual-motor function.
- “Often, movement disorders are present prior to detectable cognitive changes.”
- In advanced dementia, paratonia may lead to fixed postures (contractures).
(Drenth et al., 2020)
Shifting our focus to paratonia, a motor abnormality induced by dementia, it's worth noting that while I don't claim expertise in this area, active research in Belgium and the Netherlands is shedding light on this phenomenon. The exploration involves learning from experts in these regions.
Paratonia is a form of hypertonia characterized by involuntary variable resistance during passive movement. It emerges as dementia develops, distinct from its absence in individuals before the onset of dementia. The impact of dementia on perceptual-motor function is well-established, and it's noteworthy that movement disorders often precede detectable cognitive changes, resembling the patterns seen in balance and gait issues observed in individuals with mild cognitive impairment.
As dementia progresses, paratonia may contribute to developing fixed postures and contractures. In the upcoming visuals, we'll explore how paratonia manifests and its implications for individuals' postures and movements.
Typical Flexed Paratonia Posture
- “…a compulsive body position taken on because they are searching for their own body feeling, -scheme & -position sense that is lost because of sensory-motor disintegration of their brain & because they try to stabilize their body against gravity.”
De Clercq, Jo (2021)- personal communication
This is a line drawing that I was permitted to use by Hans Drenth, in Figure 14.

Figure 14. Line drawing showing paratonia in a client.
He is one of the authors in your references who did quite a good overview of paratonia. He is a physiotherapist, I believe, in Belgium and has been working in nursing home contexts.
The above comment is from another therapist with whom I've been in personal communication since 2020. He talks about the typical flexed paratonia posture as a compulsive body position taken on because people are searching for their own body feeling, their body scheme, and their position sense that is lost because of sensory-motor disintegration of their brain and because they try to stabilize their body against gravity.
Perceptual Motor Function in Dementia
- “People with more advanced dementia have a less & less rational reasoning brain & a more & more emotional sensory brain.”
- “This makes them live in the actual now-moment, which means that direct 'surroundings' offered to them will be extremely important to prevent signal behavior!” De Clercq, Jo (2021, personal communication)
- People are defensive, not sure where their body is in space. We need to help them relax!
Drawing from our expertise in sensory processing and integration, it's crucial to comprehend and show interest in the evolving challenges individuals with dementia face. According to European experts in this field, as people live with dementia and encounter changes in their brains, primitive responses take precedence. The rationale behind this shift is the uncertainty about their body's position in space, resulting in feelings of insecurity and unsafety.
In this context, individuals rely less on rational reasoning and increasingly on emotional sensory processing, with the limbic brain playing a more dominant role. The environment and surroundings profoundly impact their comfort levels and can trigger defensive responses akin to a fight-or-flight reaction as they strive to protect themselves. In essence, people in this situation become defensive due to their uncertainty about their body's spatial orientation.
As OTs, our role is to aid individuals in relaxing, especially when they are lying in bed without adequate supports to provide a sense of their surroundings. Without such supports, individuals may tighten up as they try to establish their position in space. Moreover, elderly individuals, who often experience difficulty maintaining body temperature, tend to adopt a fetal position during sleep to conserve warmth. Addressing these challenges becomes a critical aspect of our work, recognizing that individuals may react differently than they would have before experiencing dementia.
Good News- Posture Support Can Help!
- “This explorative study revealed beneficial short-term effects on range of motion for…SC [supporting cushions] and a positive effect of SC on upper limb muscle tone.”
- Van Deun et al., 2019
- “The results suggest that the implementation of a 24-hour Postural Care programme in a Care Home environment can result in the reduction of contractures and improvement in quality of life and ease of care.”
- Owens & Daly, 2017
Amidst the challenges posed by dementia-related changes in posture and sensory perception, there is encouraging news - posture support can make a significant difference. Two European studies shed light on the positive impact of interventions.
In 2019, Van Deun et al. conducted a study examining two interventions: supporting cushions and harmonic tones (a form of music therapy). The findings revealed that both interventions had a positive effect on relaxing upper limb muscle tone. Notably, supporting cushions were even more effective than harmonic tones in this regard.
The second study, conducted by two occupational therapists, focused on addressing knee flexion contractures. Although this study is not published in a peer-reviewed journal, it is accessible online as a PDF through a National Health Service area publication. The occupational therapists implemented a 24-hour postural care program in a care home setting (nursing home). The outcomes were promising, indicating a reduction in contractures, along with improvements in the quality of life and ease of care for the individuals involved.
While these studies represent early evidence, they offer hope and insights into the potential benefits of posture support interventions. It's important to note that research in this field is still evolving, and challenges persist in conducting high-level studies, such as randomized control trials, due to the diverse and unique nature of the populations involved. Despite these challenges, the emerging evidence underscores the importance of exploring and implementing posture support strategies in dementia care.
Goals of 24-hour PCM in SNFs
- Protect body symmetry/shape/range of movement
- Improve sleep quality
- Lessen flexion posture, agitation, and pain
In my perspective, the objectives of a 24-hour posture care management program within a skilled nursing facility (SNF) should be safeguarding body symmetry, shape, and range of movement for individuals, where feasible. The primary aim is to enhance sleep quality, supported by existing evidence that demonstrates the positive impact of strategic positioning on sleep. Moreover, the program seeks to address the discussed flexion posture concerns and mitigate any agitation or pain that individuals, particularly those with dementia, may face.
Leg Posture in Lying
- Tight knee and hip flexors limit leg extension
- Legs are 35% of adult body weight
- When they cannot straighten, their legs fall:
- Knees together (adducted)
- Knees out to the side (abducted)
- Both knees to one side (“windswept”)
The leg posture in a lying position initiates a notable domino effect. Given that legs constitute 35% of the adult body weight, any difficulty in straightening them leads to a search for support, causing them to fall in a specific direction. Our role is to assess the situation, identify where the legs naturally tend to fall and determine the type of support that can be provided. Tailoring interventions to individuals, given the substantial variation in circumstances, becomes crucial in addressing leg posture challenges.
What Can We Do For Legs and Hips?
- Relaxed, aligned positioning
- Varies for individuals
- 15-30 degrees hip abduction
- Mild flexion/external rotation
You'll see a short case study with this lady toward the end of this presentation, but this is a before-and-after example in Figure 15.

Figure 15. A before-and-after example of leg positioning with and without intervention.
This illustration depicts the contrast between the initial, less therapeutic posture and the corrected, more beneficial posture for the individual. The emphasis is on achieving symmetry, midline orientation, and an overall therapeutic alignment rather than allowing prolonged periods in a destructive, asymmetrical posture.
When addressing healthy postures, the consideration revolves around the impact of sustained positions, especially for individuals with limited mobility. The logical consequence is that extended periods in an asymmetrical posture tend to exacerbate asymmetry while focusing on symmetrical lying aims to safeguard the individual's body shape. The suggested 15- to 30-degree hip abduction range is a generalized guideline that acknowledges individual variability and draws from practices in pediatric standing frames incorporating hip abduction for hip health.
Posture Affects Chest and Spine
Posture also affects the chest and spine. This brief video shows the effects of asymmetry on a person's torso and rib cage.
Video: Effects of Asymmetry on the Torso and Rib Cage

This video was crafted by a colleague in Australia, who graciously permitted me to share it. An average person's chest exhibits a width greater than its depth, like a balloon filled with flour, demonstrating symmetry. An ideal state involves a straight spine and a balanced posture. However, when subjected to gravity, approximately 7.8 kilos of pressure, the chest flattens, impacting the heart and lungs adversely.
This flattening isn't confined to front-to-back compression. Individuals who adopt a side-sleeping fetal position experience lateral compression. The consequences manifest in a deep, narrow chest, detrimental to cardiopulmonary function. Even when lying symmetrically on the back or side, the sternum shifts, influencing the spinal column and creating a slanted sternal-spinal line.
Maintaining symmetry while lying on one's side is challenging, as the top leg and arm tend to move forward or backward, causing the sternum to shift and the sternal-spinal line to slant. This phenomenon occurs similarly in both right and left-side lying positions. Preventive measures through appropriate positioning with lateral supports can be employed to address these distortions, such as rib flares and back prominences associated with scoliosis.
Prevention is emphasized over cure, and with diligent positioning that ensures central sternum alignment, gravity can contribute to straightening the chest and mitigating flattening effects. For a more in-depth exploration, the detailed demonstration is available on YouTube.
Compression Looks Like This

Figure 16. Examples of the effects of chest compression.
Compression manifests in various ways, as depicted in these images. The initial two examples showcase individuals with chests compressed from front to back, resulting in a wide yet shallow appearance. A notable contrast is observed in the image on the right, featuring a young boy who predominantly slept on his side during his formative years.
Examining the width of his axilla in relation to his pelvis highlights a narrow but deep chest, characteristic of a barrel-shaped torso with a significant kyphosis.
Rotation Looks Like This
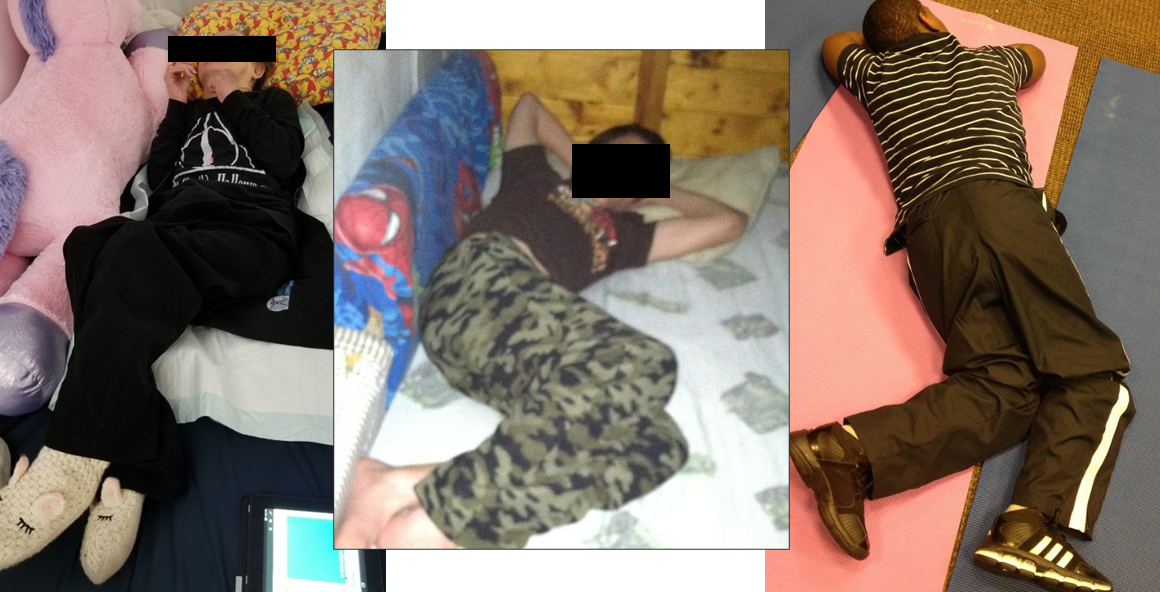
Figure 17. Examples of the effects of rotation.
The depicted rotation not only contributes to substantial asymmetry but also results in pronounced differences between the right and left sides of the body as the sternum drifts to one side. The boy, in Figure 18, exhibited 45-degree scoliosis when I conducted these measurements.
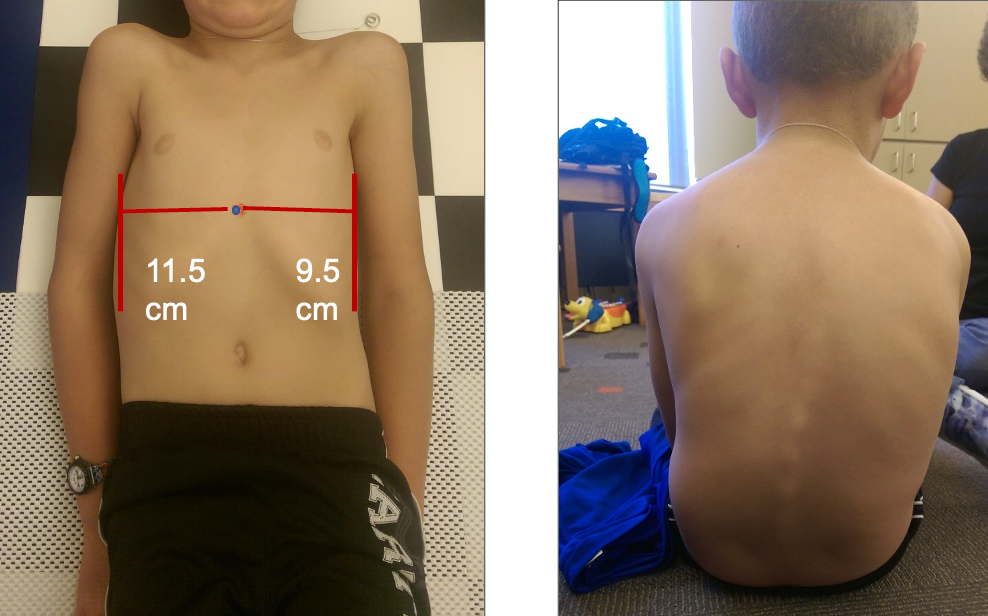
Figure 18. A boy with scoliosis.
Using Supports at Night – Sternum in the Middle
To address this issue, we can implement nighttime supports to assist in maintaining the person's sternum in the middle. As evidenced in the visual, you can observe the corrective impact (Figure 19).

Figure 19. Correction to positioning to maintain the sternum in the middle.
Take Home Message
- A level pelvis and balanced sternal spinal line provide postural stability in all orientations.
- If the body is stable and balanced, then gravity can be harnessed for good.
The key takeaway here is that achieving a level pelvis and a balanced sternal-spinal line allows us to leverage gravity positively, promoting postural stability for individuals.
Montana Postural Care Project
- Three-year pilot project
- 2016-2018
- 24-7 intentional posture support
- Supported lying posture focus
- 74 participants enrolled, ages 1-67
- 55 participants completed the study
This is an overview of a pilot study I did that I'm currently working on getting published. We found quite a large heterogeneous group of people who ranged in age from one to age 64.
Body Symmetry, Pain & Sleep Results
- Each participant improved in at least one area
- For all measures, 64% of those captured improved
- Pain: 55% reported a decrease in pain levels
- Sleep quality: 69% reported improvement in overall sleep quality
We saw improvements in body symmetry, pain, and sleep quality in most people, as shown in Figures 20 and 21.
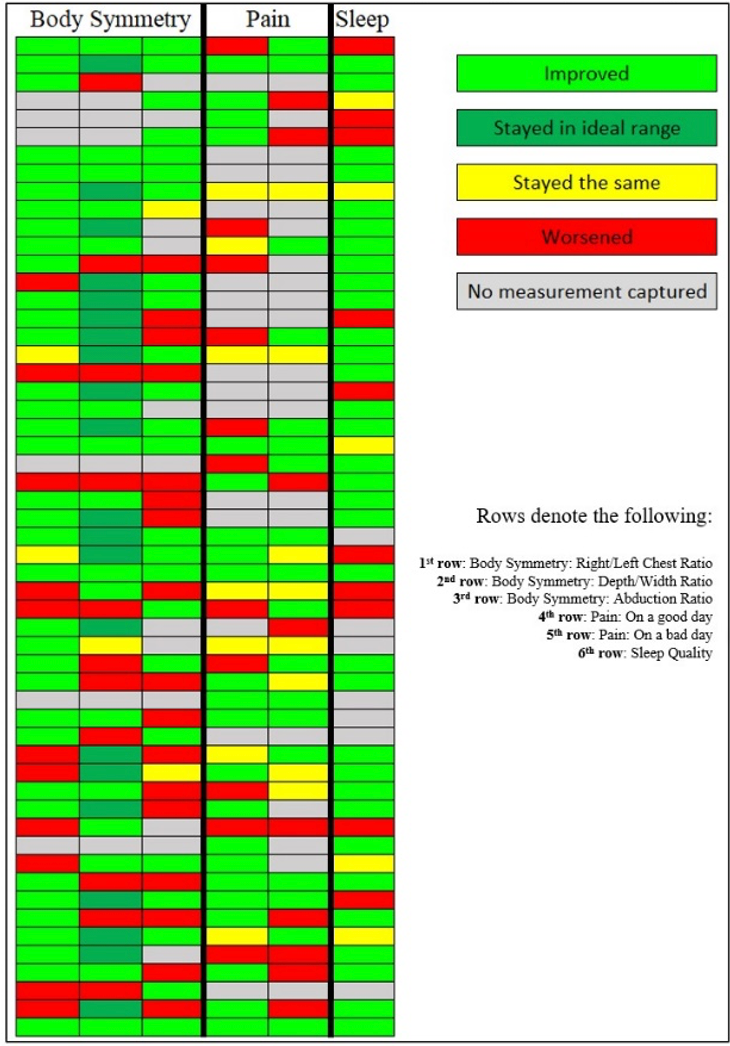
Figure 20. Individual Results for Body Symmetry, Pain, and Sleep.
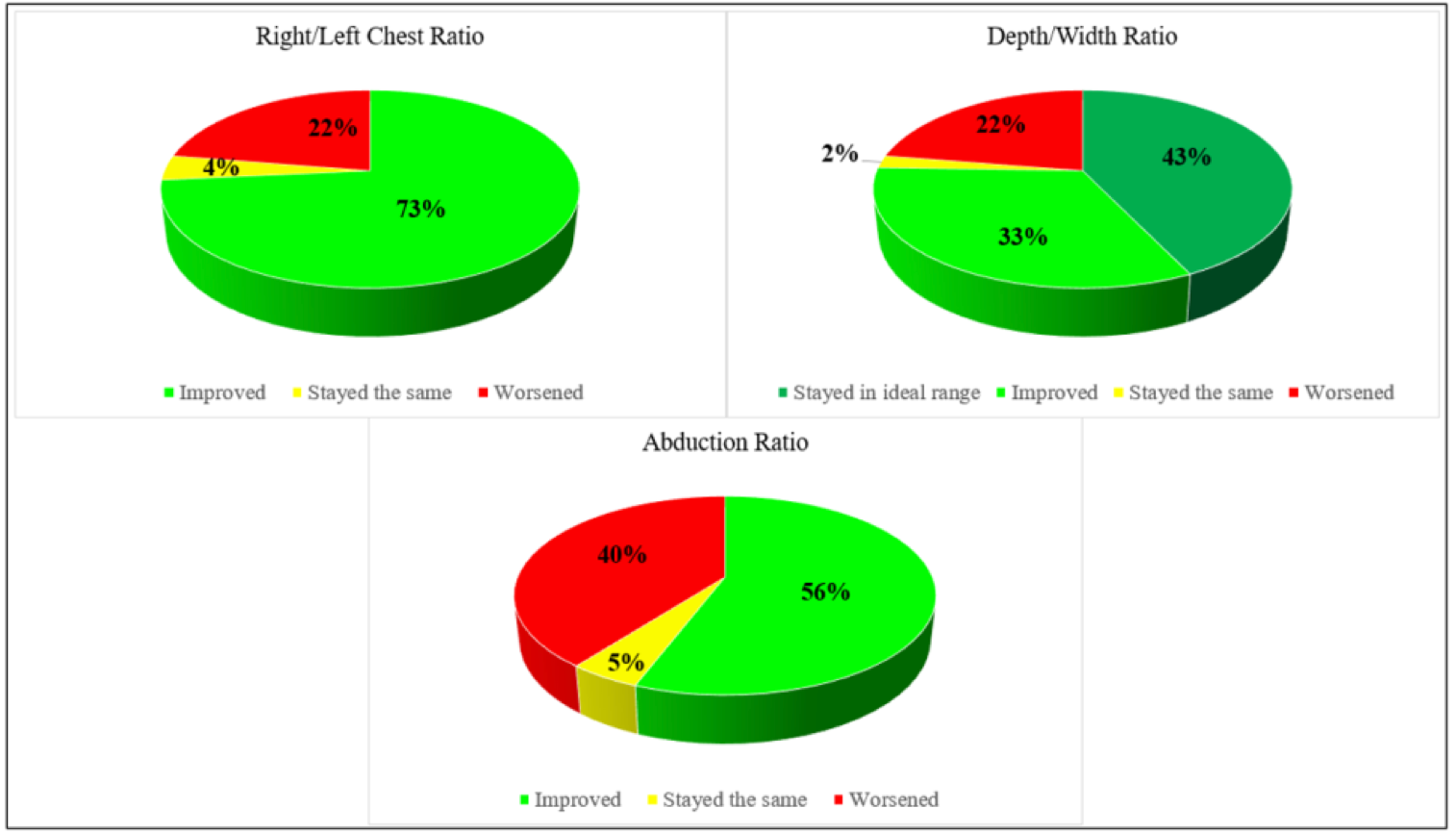
Figure 21. Body Symmetry Results Among Participants Who Completed the Study.
Supports in Lying: Overview and Safety
Let's talk about just what this might look like.
Supports Go Beneath a Fitted Sheet
Figure 22 shows how we put the supports beneath the fitted sheet.
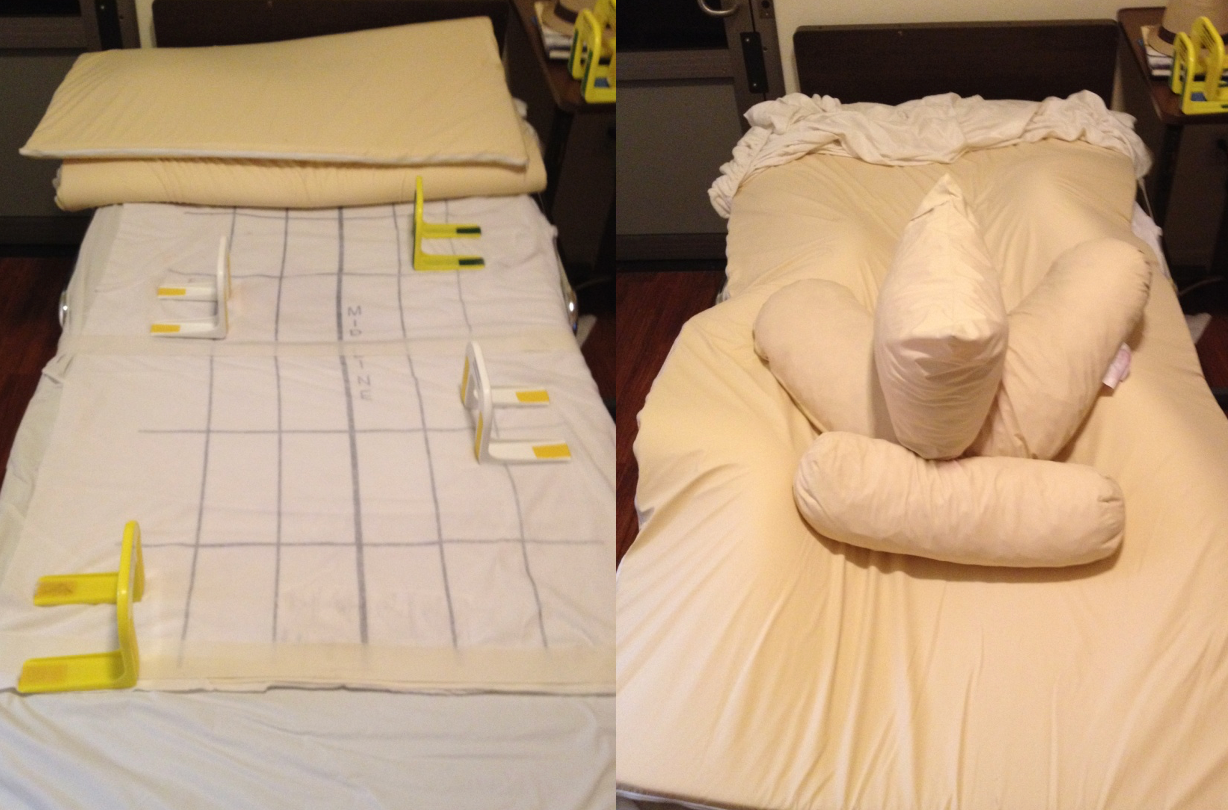
Figure 22. Example of how supports go under the sheets.
We're always going to individualize them and help bring a person into better alignment.
Always Individualize Supports
Figure 23 shows another image and shows how this is individualized to the client.

Figure 23. Example of individualized support for this client's legs.
Support Options: Pool Noodles, Towels, Cupboard Liners, Etc.
These are some of the homemade things that I have used over the years with people to help things stay in place underneath the fitted sheets.

Figure 24. Example of a bed set up (© Eleanore’s Project, Inc. 2018-2019 All Rights Reserved).
You can roll towels, wrap them with Coban, and stick them under a fitted sheet to help them stay in place. Figures 25 and 26 show other examples of what our colleagues in Peru have done.

Figure 25. The first example is in Peru (© Eleanore’s Project, Inc. 2018-2019, All Rights Reserved).

Figure 26. The second example is in Peru (© Eleanore’s Project, Inc. 2018-2019, All Rights Reserved).
Solutions Do Not Need to be Costly
This was an American mother who used PVC pipe to keep the covers off of her daughter's toes as she was sleeping in her sleep system.
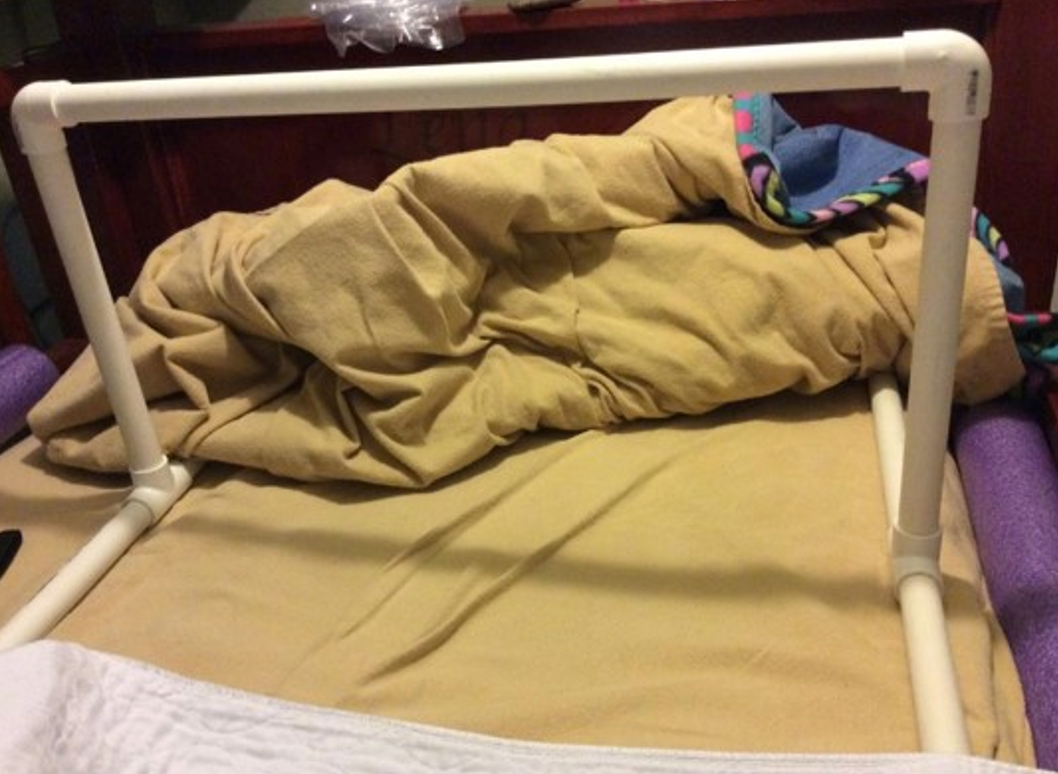
Figure 27. Example of PVC pipe created to protect a client's toes.
Consider and Mitigate Safety Risks of Therapeutic Positioning
We need to mitigate and think about risks when we are doing positioning with people in bed. We should weigh out the benefits versus risks because any therapy intervention we recommend or do will inevitably have some possible risk or unintended consequence.
Do Potential Benefits Outweigh Possible Risks?
- Reducing pain
- Improving sleep
- Stabilizing posture
- Improving body symmetry
These are some of the goals of therapeutic positioning.
Possible Safety Challenges
- Breathing/aspiration
- Thermal regulation
- Pain
- Pressure
Here are some possible safety challenges. We need to be careful for people who have problems in this area. For instance, head elevation can make a big difference for these folks in an adjustable bed or when using wedges. We must know that building supports around people may cause them to build up more heat. We also must address pain. Lastly, I want to spend time on pressure because this is often a big worry for people.
Age 65 - Down Syndrome, Alzheimer's, No Postural Supports
This 65-year-old has Down syndrome and Alzheimer's, which is commonly seen. This was a pressure mapping that was done with her on a low-air-loss mattress, which is very pressure-relieving. Her preferred habitual posture was rolling more to her right side, and as a result, she had significant pressure (Figure 28).
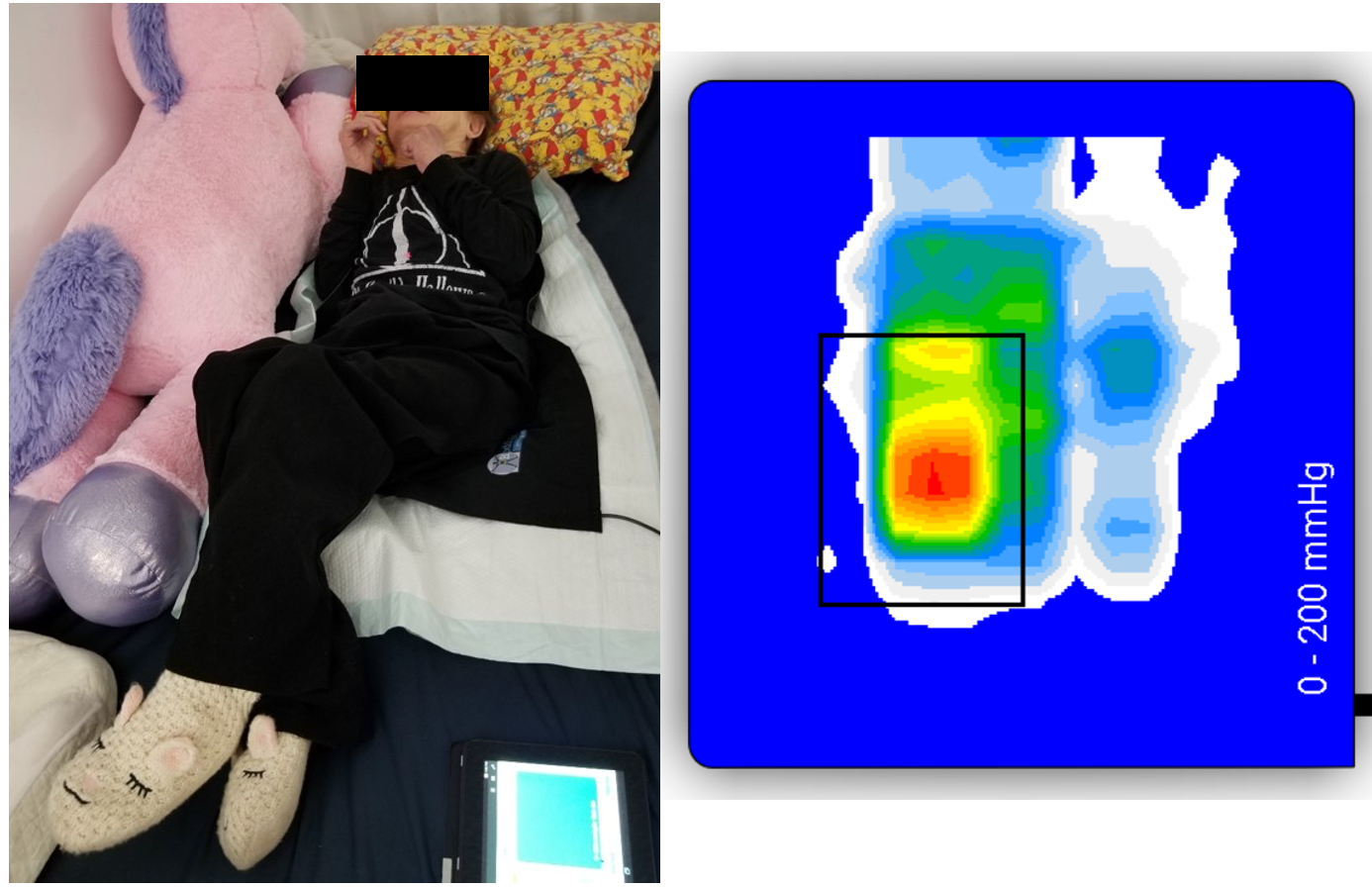
Figure 28. Client without supports and with increased pressure shown.
Age 65 - Down Syndrome, Alzheimer's, With Postural Supports
Figure 29 shows the client after the postural supports are provided. The pressure map does not show any pressure areas.
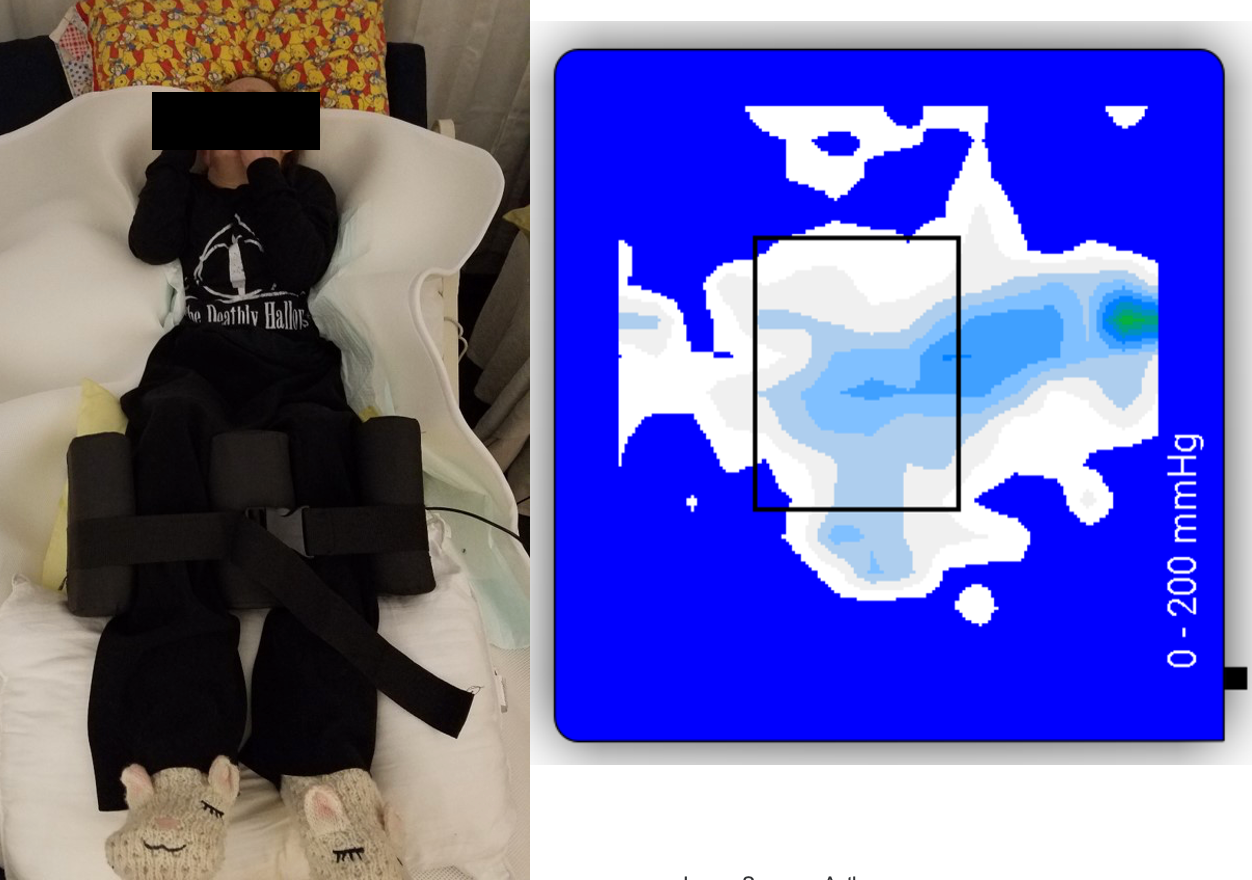
Figure 29. Client without supports and decreased pressure shown.
However, when we provided her with posture supports that brought her into symmetry and midline orientation, the weight was distributed more evenly throughout her whole body.
Case Studies: Using Low-Tech and Informal Supports
BaoNHia
- Diagnosis: Aicardi Syndrome
- Slept on alternating sides for 11 years
- Turned every two hours by her mother
- Hmong community member
This case study was published in the RESNA Assistive Technology Journal last March (Figure 30).

Figure 30. BaoNHia in 2003 versus 2011.
If you're interested in this case study, it is accessible on ResearchGate. The case involves an individual with a deep and narrow chest due to 11 years of side sleeping, with alternating turns every two hours by her mother. This client from Missoula, Montana, exemplifies characteristics similar to the previous example, highlighting the narrowness of the chest at the axilla level (Figure 31).
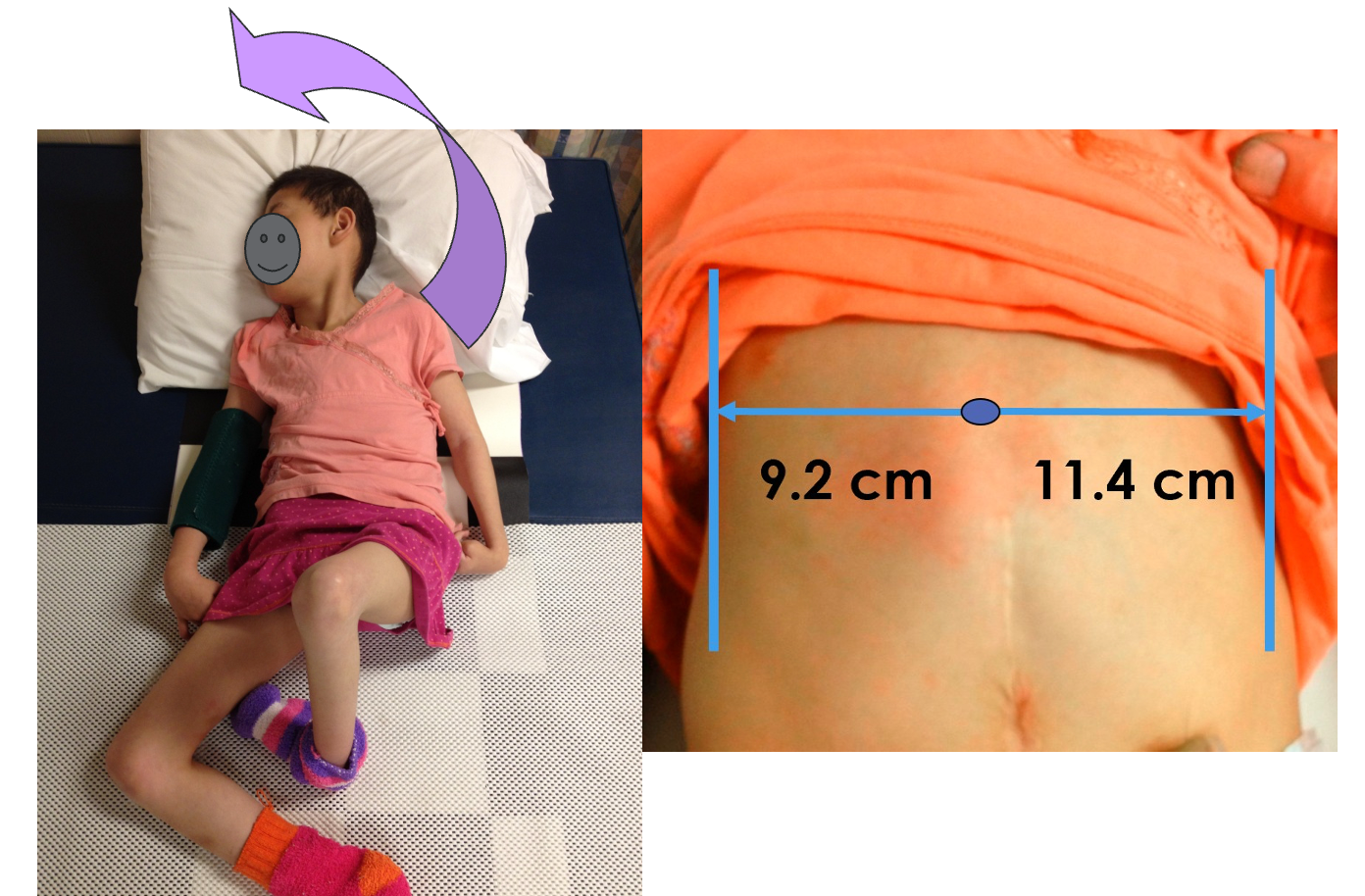
Figure 31. BaoNHia showing the chest deformities and measurements.
If you compare that to the width of her pelvis, there's quite a big difference. She was off the charts for how flattened her chest had become from side to side. Her mother learned to position her therapeutically at night, as seen in Figure 32.

Figure 32. BaoNHia's mother positioning her at night.
Her mother learned to position her so her pelvis was level with her sternum in the middle. The arrow shows how she derotated her sternum so that her sternum would be in the middle of her chest instead of drifting off to her right side. Figure 33 shows the results over six years, from June 2012 to June 2018.
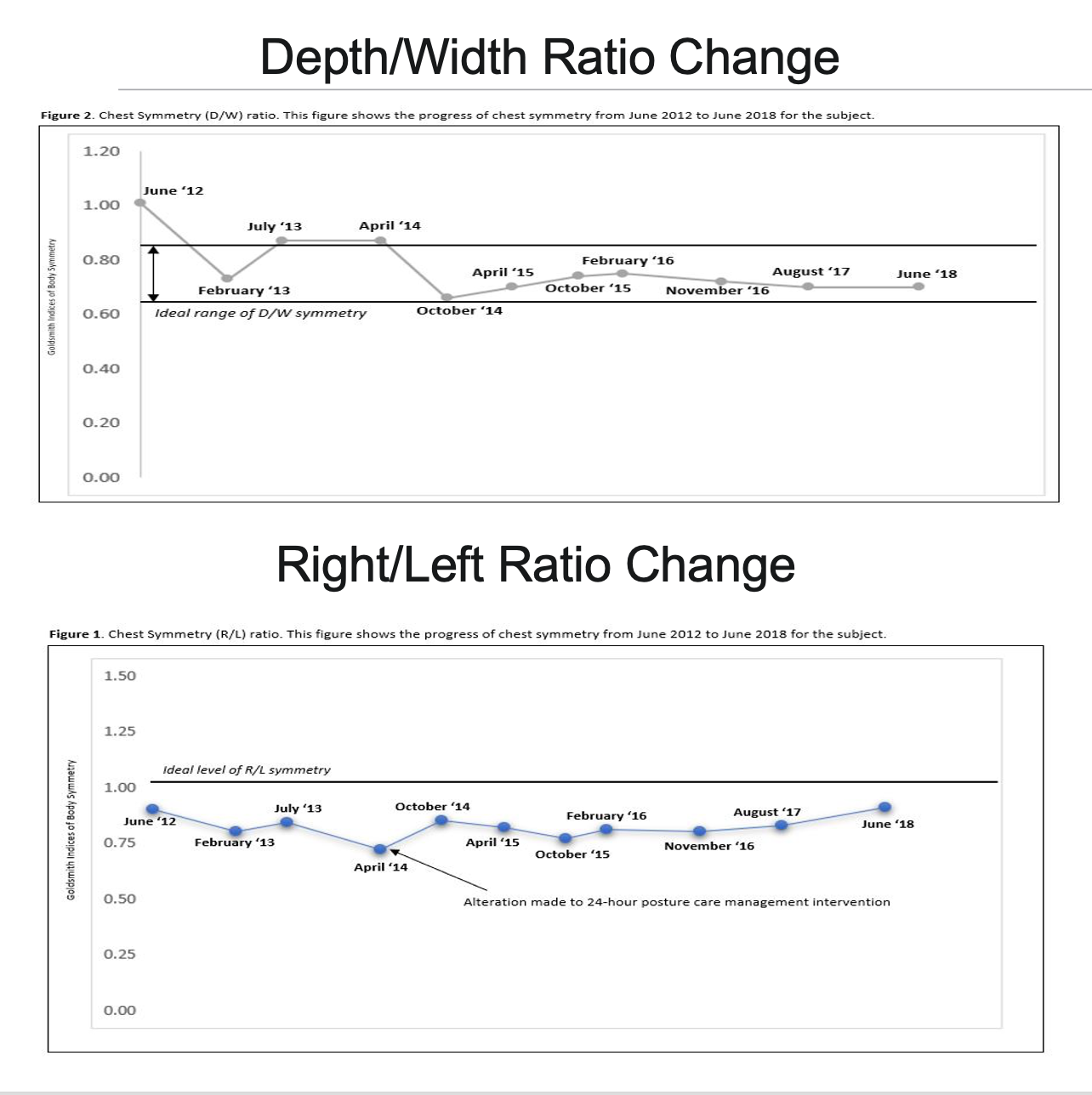
Figure 33. Anatomical changes noted in BaoNHia over 6 years.
In the top image, you can observe the initial flattening of her chest, with the normal rounded chest indicated between the two dark lines in the middle. Although she started off the charts, she quickly descended into the typical range and remained there throughout subsequent measurements.
In the lower section, the graph depicts her progress from June 2012. Initially, the focus was on addressing the chest flattening's impact on cardiopulmonary function. However, as her right-left asymmetry and sternum drift became more pronounced, firmer supports were introduced in 2014, resulting in a noticeable improvement.
While she didn't achieve perfect symmetry, it's worth noting that achieving absolute symmetry is rare, even among able-bodied individuals, as evidenced by a recent workshop I taught at the Kennedy Krieger Institute. In a group of 20 therapists, able-bodied OTs and PTs took turns measuring each other and were surprised to discover that almost nobody in the group was perfectly symmetrical.
- Benefits
- Sleeps supine all night – no turning/no skin breakdown
- Her mother sleeps all night, too.
- Improved swallowing - faster and easier
- Strong cough and respiratory function
- Typically wakes up relaxed
- Improved chest/spine symmetry – without surgery
These are the benefits BaoNHia experienced. This can be used for anybody of any age, and I feel pretty strongly that our people in SNFs need to have access to this intervention.
Cherie
- Lives in a group home
- Cerebral palsy diagnosis
- Drives a power chair
- Attends day program
- 60 years old
When I met Cherie, she was about 60 years old. She had cerebral palsy, lived in a group home, and was part of the Montana Postural Care Project.

Figure 34. Cherie is in her power wheelchair.
Here was her typical posture in January 2018 (Figure 35).

Figure 35. Cherie's typical positions.
Her sitting posture in the recliner showcases challenges related to hip and knee flexion contractures. Placing her in the recliner, which lacked adequate leg support for extension due to her contractures, resulted in a curled-up position. While the intentions were positive, the unintended consequences of her seating arrangement became apparent. Subsequently, efforts were directed toward implementing proper positioning strategies for her bed, as shown in Figure 36.

Figure 36. Cherie has better positioning in bed.
We also did not want to forget sitting. Examples of before and after can be seen in Figure 37.

Figure 37. Cherie with before and after sitting with supports.
Fortunately, the reclining chair allowed for adjustment, enabling the placement of the leg support down while maintaining the reclined position. Utilizing available pillows and incorporating the same leg pillow positioner from her sleep system enhanced her side support and centrally positioned her legs. This modification eliminated the need for the extended leg rest, offering her a comfortable seated position that accommodated her body's natural alignment. Additionally, noteworthy changes in chest symmetry were achieved even at the age of 60, showcasing the potential for impactful transformations (Figure 38).
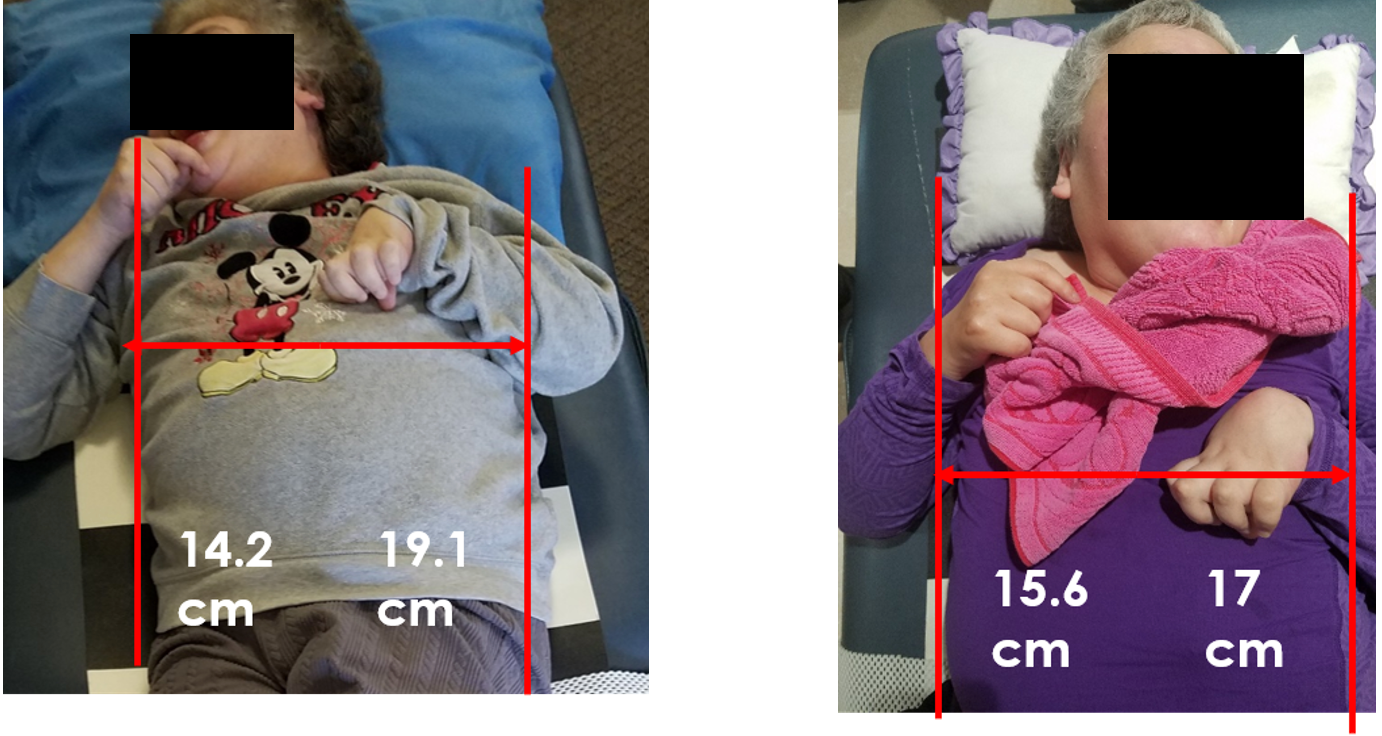
Figure 38. Chest symmetry measurements of Cherie.
Measuring from her xiphoid process under the sternum to the left and right sides of her rib cage revealed a substantial five-centimeter difference. Remarkably, within nine months, significant progress was observed, with the asymmetry reduced to just a one-centimeter difference. The transformation highlighted the positive impact of maintaining a centered sternum during sleep.
- Benefits
- Her breathing and coughing/choking were a little better; there is no change in her saliva control.
- Her sleep quality and daytime alertness are a lot better, and her emotional state is a little better.
- Her muscle tone is a lot better, and getting dressed is a little better.
- Her sitting posture, sitting tolerance in her wheelchair and transfers are a lot better.
- Her lying posture without supports is a little better.
Cherie's caregivers reported several positive benefits after nine months of implementing the changes. They noticed improvements in her breathing, coughing, and choking, even though her saliva control remained unchanged. Sleep quality and daytime alertness significantly improved, as expected when experiencing better sleep at night. They observed enhanced muscle tone, making activities like getting dressed more manageable. Her sitting posture, sitting tolerance in the wheelchair, and transfers were notably better. Even Cherie's lying posture without supports improved, reflecting the positive impact on unsupported postures over time.
Summary
Thanks for your attention today. I will now take some questions.
Questions
Will lying in a supine position still cause flattening of the chest?
Excellent question! It's crucial to use lateral supports at the sides to provide boundaries for the chest and prevent flattening. Even in side-lying positions, supports at the front and back are necessary.
I'm amazed at the differences created by positioning without surgeries. Thank you for emphasizing this.
Thank you! It's crucial to spread awareness that improvements can be achieved through non-surgical approaches.
In an SNF setting, which codes should be billed for these interventions?
I haven't billed in an SNF, but typical CPT codes like OT eval and re-eval can be used. Also, consider neuro reeducation and therapeutic activities. Someone mentioned CPT 97530 for dynamic activities.
How are upper extremities addressed in 24-hour posturing systems? Do you recommend reactive splinting?
Splints can be used, but we focus on relaxed positions for the upper extremities. Customized approaches, like using wrist weights for spasming, can provide comfort.
When seated, should a person with kyphosis use a reclining wheelchair for extension?
I'd recommend a tilt-in-space chair over a recliner to prevent sliding and potential risks. Also, building support under the upper legs and knees can enhance comfort.
Any recommendations for kyphotic positioning other than pillows?
Using available items in the environment, like rolling towels with Coban wrapped around them under the fitted sheet, can be effective. Ensure strong supports on both sides during side-lying to avoid rotation.
Could the pain management code be used for positioning?
Absolutely! Considering pain management codes for positioning is a great idea.
If a person can move themselves in bed, are these support systems still indicated?
Consider how they move. If they consistently land in a similar position, providing support could be beneficial.
Have you used cooling blankets for thermal regulation or maternity pillows for support?
Yes, both are valuable tools. Exploring modern options for thermal regulation, such as cooling blankets, can be beneficial.
References
Agústsson, A., Sveinsson, T., Pope, P., & Rodby-Bousquet, E. (2019). Preferred posture in lying and its association with scoliosis and windswept hips in adults with cerebral palsy. Disability and Rehabilitation, 41(26), 3198-3202. https://pubmed. ncbi.nlm.nih.gov/30010440/
Casey, J., Agustsson, A., Rosenblad, A., & Rodby-Bousquet, E. (2021). Relationship between scoliosis, windswept hips and contractures with pain and asymmetries in sitting and supine in 2450 children with cerebral palsy. Disability and Rehabilitation, 1–6. Advance online publication. https://doi.org/10.1080/09638288.2021.1971308.
Citation
Kittelson, T.(2023). Skilled nursing facility interventions: Positioning around the clock matters. OccupationalTherapy.com, Article 5660. Available at www.occupationaltherapy.com
