Introduction
I am thrilled to be here to discuss this topic that is rooted in firsthand experience and quite an anxiety producer I must say. I was first introduced to telehealth about two years ago. At the time, there were not a lot of resources, and I did not know a lot of therapists who were doing telehealth. I was so intimidated. This is one of the reasons I decided to delve into this presentation.
The first thing I did was look up the research. However, I found a lot in adult rehab but not much with the pediatric population. I am sure all of you are aware that pediatrics is a whole different animal, and there is a lot more research now than there was before. But still, I think it has left clinicians feeling quite trapped about delving into pediatric telehealth. Hopefully this presentation will help ease that anxiety and give you some solutions and strategies that you can use.
AOTA's Telehealth Position Paper
•“…the application of evaluative, consultative, preventative, and therapeutic services delivered through telecommunication and information technologies” (AOTA, 2013, S69)
Whenever I enter a new arena, I like to look at the AOTA website and the research. This position paper was really helpful when I first started telehealth. It provides you a lot of general guidelines, existing research, qualifications, ethics, and the regulations. I would really suggest reviewing this before you delve into telehealth.
State Licensing Requirements
Licensing requirements are very stringent, and it depends on your location, the client's location, and the feasibility of telehealth for your specific client, whether it is based on the technology or their surroundings (Figure 1).
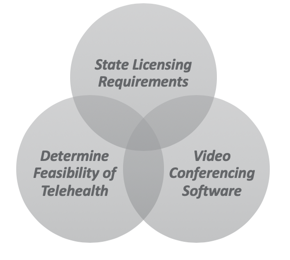
Figure 1. Considerations for telehealth.
And, if they live in an environment where it is feasible, then you need to assess the software needs, make sure it is HIPAA compliant, etc.
Delivery Models
- Asynchronous delivery refers to store-and-forward technologies, such as therapy websites offering informational videos and other tools to families, or self-paced Internet training for therapists
- Synchronous delivery refers to telehealth services delivered through interactive technologies in real-time, such as a live VoIP consultative or treatment session with a child and their family, while..........
- Store-and-forward technology means the asynchronous transmission of a patient's medical information from a healthcare professional at an originating site to a healthcare professional at a distant site
(AOTA, 2013)
As far as delivery models, there are several. Asynchronous is where you store and forward the information. Videos are asynchronous. Synchronous is what most of us are doing now which is a live video conferencing environment. Store and forward is an asynchronous form of information. An example might be a patient's medical information that you forward to another team member.
AOTA Telehealth Decision Guide
- Considerations:
- AOTA position paper/research?
- State regulation and agency requirements?
- Payer Coverage for Telehealth?
- Consent?
- Technical considerations?
- Ethical considerations?
If you are an AOTA member, they have this beautiful flowchart. It highlights what you need to think about, and it gives you a very clear distinction of whether you have met the state regulatory agency requirements. It asks you questions to guide your problem-solving. It also discusses consent, technical considerations, and ethics.
Pediatric Telehealth: Challenges and Solutions
- Comfort with technology
- Need for a facilitator
- Receptiveness to parent training
- Keeping children engaged
- Sensory strategies
- Accessibility to devices and supplies
Telehealth has several challenges. There is a recent article called Use of Telehealth in Early Intervention in Colorado: Strengths and Challenges with Telehealth as a Service Delivery Model (Cole et al, 2019). This highlighted that most practitioners claimed that technology management was the primary structural barrier that interfered with telehealth services. Generally speaking, technology is a major issue. However, when dealing with a pediatric population, there are secondary layers as well. Adults can usually follow instructions, but with pediatric clients, we may have to also use some parent coaching. As such there are two layers of instruction: occupation-based coaching vs. direct therapy. You have to instruct the parent and the child. And if you have a child that is older, you may not only be instructing them in different treatments, but you may also have to instruct them on how to use the technology.
Some of the major challenges I have encountered and what I have heard from other practitioners is being comfortable with technology. If you are using a parent as a facilitator, sometimes that is hard. Obviously, if it is working with a child, they also have to know what to do. The parents may have to be involved and require parent training, and some parents do not want to do it. This is okay, but that can definitely be a barrier.
We also need to figure out how to keep children engaged. I hear this all the time, and we will go through some scenarios to help you with that. I think this is where my ABA training really helped me.
Many people ask me how to employ sensory strategies via telehealth? And yeah, there are definitely some different elements that we will be discussing.
Not all families have accessibility. There are several choices when you have a pediatric telehealth client. The first one is how are you going to do your telehealth? Occupation-based coaching is really the same thing as parent training. That is your first decision. This can be a cumbersome decision in itself because you have to make sure the parent is willing to participate in parent training. If a child can follow directions, I usually use direct therapy. However, if they do not follow directions, I definitely go with parent training and coaching. Many parents prefer that even if their kids are independent. "I know Johnny works really well with you, but I want to learn what he is doing."
Mode of Telehealth Treatment
Whenever I have a client, I need to think about what mode I am going to use. Asynchronous, synchronous, or hybrid? Figure 2 is a chart that shows this.
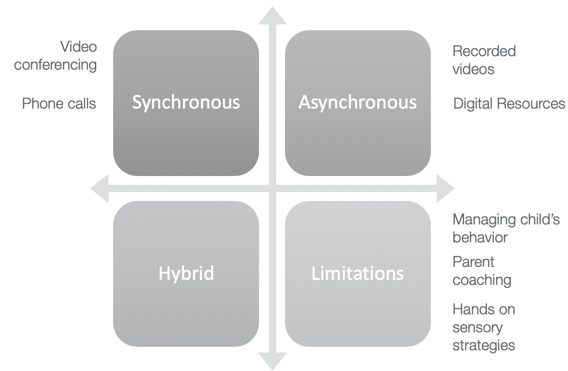
Figure 2. Modes of telehealth treatment.
In this schemata, I have highlighted the different modes and limitations of each mode of delivery. If the client has major behavioral issues, that is something you need to consider. Are recorded videos or video conferencing better for this client? Are you wasting a lot of time in video conferencing sessions? Do they want/need parent coaching? How can you do hands-on sensory strategies? If you want to do that, perhaps synchronous would be better to show them hands-on techniques. Or, the parent may be more receptive to asynchronous due to scheduling. The only thing I would be careful of with an asynchronous mode is that if you are referring them to some resources outside of what you are showing them, you need to have a disclaimer that these are resources only.
Parent Training = Occupation Based Coaching
- Rooted in principles consistent with Occupational Performance Coaching (Graham, Rodger, & Ziviani, 2009, 2010),
- Directly involves parents in creating goals and strategies to increase child participation in everyday contexts. (see Little et al., 2018a for a full description of intervention).
- Reflective questioning and commenting to problem solve through potential strategies.
- This process allows parents to gain a deeper understanding of possible solutions, and ways to implement and evaluate the effectiveness of these solutions (Dunn, Little, Pope, & Wallisch, 2017; Little et al., 2018a; Rush & Shelden, 2011)
Let's talk more about parent training. This is what I typically use with students who do not have an easy time following directions. Occupation-based coaching is what is going to be referred to in this presentation, but again, it is the same thing as parent training. It is rooted in the same principles. It is the coaching of families with young children. It is used a lot with children with an autism spectrum disorder, and it is highlighted as best practice in the literature. An article by Little et al. in 2018 is one such article. It looks at the caregiver and child as a family unit and provides strategies for intervention. It coaches parents and helps them to create goals and strategies to increase participation. Thus, caregivers are an integral part of the intervention. It involves reflective questioning and problem solving and allows the parent to gain a better understanding of what the child's limitations are and what solutions can be offered. Again, a parent has to be receptive to this. Otherwise, it really does not work as it is a team approach. The one thing that is a shift in occupation-based coaching is that it is not so much a skill focus but rather more of a participation focus. This can be very prominent in telehealth intervention as you are watching the clients complete their activities of daily living.
Skill Focus Vs. Participation Focus
- By focusing on specific child skills (as happens in traditional therapy programs) as opposed to overall family participation, occupational therapists may be limiting the extent to which children are able to attend birthday parties, go to holiday events, or participate in music classes.
- However, when occupational therapists work with parents to practice their own strategies in the everyday occupations that may pose challenges, children may be able to participate more fully.
(Little, L. M., Pope, E., Wallisch, A., & Dunn, W., 2018)
Typically in a clinic setting, we focus on a skill set, and we may limit the extent of a child's ability to participate. When you do telehealth, it is important to focus on what are we working on and how will it improve participation. The other aspect is that when OTs work with parents to practice these strategies, they are going to practice it more because it is part of participation rather than just one skill. For example, if I say, "I want you to work on 10 reps of this with Johnny," it probably will not happen. Whereas, if I say, "Every day when you are doing the dishes, make sure Johnny stacks the cups like this." That is more likely to happen. It is changing your paradigm to a participation focus versus a skill focus.
Occupation-Based Coaching
The 5 Key Principles of Occupation-Based Coaching
- Authentic contexts
- Family's interests and routines
- Caregiver interaction and responsiveness
- Reflection and feedback
- Joint plans
(Adapted from Rush & Shelden, 2011)
There are several key principles of occupational-based coaching. It is about encouraging the parent to create their own strategies so that they can match their unique setting. It is really important for them to look into their home life and say, "These are the struggles I am having within the context of the family." The principles highlight this.
The first is an authentic context. We are in the client and caregiver's home. We need to make sure that it is an authentic context. This is easier to do with telehealth because you are treating in that setting.
Second would be the family's interests and routines. We need to create strategies that occur with natural routines and interests. As I mentioned before, rather than saying to mom, "Let's do this x times," if you incorporate it into the daily routine, it is more likely to occur.
Caregiver interaction and responsiveness need to be supported. Behavior is a component of that. If we can help the caregivers to understand the behavior and know what it means, we can then create a transaction between the child and the parent. Using the family's patterns and what they do every day can foster family relationships. This is more of a psychological bonding aspect that I really love as part of OT. We are knowledgeable about mental and emotional health.
Reflection and feedback are also crucial and this is the part of what people miss in telehealth, especially with pediatrics. I know I did when I first started. You are asking the parent to be something they are not. They are not qualified to be a therapist nor are they qualified to provide these interventions. Thus, you need to take the time to guide their reflection and feedback. The provider and the caregiver need to talk and reflect on what happened during the session. "How can we change that?" Or, "You did a brilliant job with this."
You also have to have joint plans. This is where the provider and caregiver identify what each will accomplish between sessions to address the family goals. You might send the parent an email and say, "I was hoping to work on cooking with you on Tuesday. Do you have these items?" These are some strategies that you would want to do. But again, we are a team. We are not just going in there, treat, and then say goodbye. It is a collaborative approach.
OBC: The Process
- Setting goals
- Exploring options
- Planning action
- Carrying out the plan
- Checking performance
- Generalizing
(Rush & Shelden, 2011)
What is the process of occupation-based coaching? The model gives caregivers power. It empowers them to create strategies to increase their child's participation across natural contexts. This is what it is really about. OBC or occupation-based coaching is an intervention that combines several principles. It is coaching with occupation-centered reasoning. The process of this model includes setting goals, exploring options, and then planning an action with the parent. You then carry out the plan and check performance so you know what is working and what is not. Finally, you want to see if the information is generalizing to other situations. Those are the components that can make a parent training really effective.
Although many studies have indicated like hybrid approaches of teletherapy are very effective with occupation-based coaching, there is not much research on pure telehealth services and occupational-based coaching. We definitely need more research. The direction is showing that there is some efficacy with our students with autism. And, I like to broaden it to say students who have a hard time with following directions and significant sensory issues. Parents identify goals that align with their families' current needs, and then they identify how they could achieve such goals in their daily routine.
Guiding Parent Into Creating Achievable Goals
- Many parents identify children’s adaptive behavior as a target for intervention (Simpson, 2015).
- Caregivers identify goals and therapists ask reflective questions and make reflective comments, affording caregivers an opportunity to gain a deeper understanding of their own current knowledge and the impact of their strategies on their children’s adaptive behavior (Rush & Shelden, 2011).
The studies have shown that through OBC, many parents identify adaptive behaviors as part of their intervention for things like toileting, eating, and sleeping. These strategies seem to be the core of parent training. The combination of four elements (parent identified strategies, parent identified goals, parent implementation, and the evaluation of the effectiveness of strategies) are the hallmark of occupation-based coaching. It makes it unique from any other intervention process. The parent is such an integral part of this type of training so it is a very effective method of increasing parent efficacy and child participation as per the literature.
It also increases positive child-caregiver interactions and capitalizes on the family's strength. The families are using their own resources and learning how to problem-solve their child's behaviors and challenges. Caregivers identify goals and therapists ask reflective questions and comments to afford caregivers a deeper understanding.
Part of occupational-based coaching is guiding a parent to create achievable goals. And like I mentioned before, it is very much about the parent being an integral part of this and identifying adaptive behaviors they want to be addressed.
Tips for Reflective Questioning
- Ask only one reflective question at a time.
- Be comfortable with silence while waiting for the person to think about his/her response.
- An analysis question always follows informative feedback (e.g., What are your thoughts about the idea?”).
- A self- attribution question is “ what did you do to make that happen/ cause that progress?”
- A yes/no question should only be used to ask permission or not make an assumption ( e.g. would you like to try it?)
- What if when you ask a reflective question, the person says I don’t know?
- rephrase the question to ensure he/she understands, or
- provide affirmative feedback about an observation you made in the past that confirms he/she knows
Rush, D. D. & Shelden, M. L. (2011). The early childhood coaching handbook. Baltimore, MD: Paul H. Brookes Publishing Co
I found this resource for reflective questioning. It is asking one question at a time and creating a pause. For some of us, this can be difficult as we have to constantly instruct. There are also self-attribution questions like, "What do you think?" These are some suggestions and ideas that I found in the literature that I thought was really helpful. I have used some of these especially when I have had a parent who is a bit contentious and not quite happy with the format. I have noticed if I use this reflective questioning, it dissipates some of the anxiety with parent training. It can be a lot of work for the parent, and they may not just be used to that.
Tips on Providing Feedback
- Feedback occurs after the learner has had the opportunity to reflect on his or her observations or actions, or after the learner has practiced a new skill.
- Feedback can be affirmative:
- statements that describe, restate, or acknowledge what the person said. “I see what you mean.”
- Feedback can be evaluative:
- Comments that evaluate or critique the person’s words or actions. Evaluative feedback should be used in moderation so that it does not stifle the person’s efforts.
- Feedback can be informative.
- Informative feedback includes instances where the coach is sharing new information with the person.
- Feedback can be affirmative:
Rush, D. D. & Shelden, M. L. (2011). The early childhood coaching handbook. Baltimore, MD: Paul H. Brookes Publishing Co.
If you are going to use reflective questioning, you also need to provide feedback. Feedback is really important. It occurs when the parent or the caregiver has been instructed on a skill, and then they perform it. There are different types of feedback. An example is affirmative, "I understand what you mean." Or, "I see what happened."
It can be evaluative which is when you are giving them a critique, albeit softly.
Lastly, it can be informative. For example, if I had a student whose mom said that she did not listen, I might say, "For her age, that is fairly typical." Or for a child with sensory issues, I might say, "For a child who has this type of sensory issue, that is fairly typical." I am informing the parent.
Creating a Mindful Space in Everyday Parenting
- A shift in parent perception
- Requires non-judgmental intervention
- Team approach
Overall, you want to create a mindful space for parents when they are parenting. This is really hard for them. I cannot emphasize this enough because I get feedback from parents all the time. After 6-8 sessions, I email a feedback form and say, "Please be as honest as you can because this will help me provide better service to you." This sort of feedback is really important for growth. And as therapists, we need to shift our thinking. We are not trying to increase skills or control the session, but rather we are trying to help the parent shift their perception of the child in order to help their child. It really does require a lot of non-judgmental intervention. Often parents do not get the results as fast as we would and this can be awfully frustrating as a therapist. However, keep in mind that our job is to be non-judgmental, and it does require a lot of patience. It is a really strong team approach that you are implementing. For those that have received parent training, it really shows as they have the perspective of focusing on what their child can do rather than what they cannot do. This was a theme that I saw in the literature. Studies also suggested that focusing on strengths resulted in parents increasing their own positive statements and changing their perceptions of their child's disability. I thought this was really profound. It also increases their physical affection with their child. How lovely is that?
Grading Activities
- Grading activities at a slower more monitored pace
- Telehealth therapy: Families generate their own solutions and are ultimately responsible for carrying out the intervention and evaluating its effectiveness (Dunn et al., 2012; Graham et al., 2013)
How do you grade activities? This is something that you have to be very careful of when you are completing occupational-based training or parent training. Research shows that we go at a slower pace when it comes to parents. "Families generate their own solutions, and are ultimately responsible for carrying out the intervention, and evaluating its effectiveness." We cannot expect them to be as fast as we are in this. We are partnering with parents, and this is so important for us as a profession. The anticipation is that you are going to go back into the clinic setting at some point. After being an integral part of the intervention process, parents are going to value you so much more because they know what you can do via telehealth. They are going to be that much more supportive of the outcomes and the progress you are able to achieve in person.
Partnering With Parents
- In a coaching model, parents’ goals and priorities guide intervention (Rush & Sheldon, 2011).
- .....family-centered care and parent-therapist relationships are active ingredients for interventions (e.g., Foster et al., 2013; Law et al., 2003)
- .........focus on strengths may result in parents increasing positive statements, changing their perception of their child’s disability, and increasing their physical affection with their child (Carlson et al., 2010; Steiner, 2011)
It is important for us to use this coaching model to really focus on the parents' goals and priorities. This is being family-centered and goal-oriented by focusing on the strengths of the child. There is a lot of literature out there that really supports this.
Case Study 1: George
- Age: 3 yrs.
- Diagnosis: Autism
- Background:
- George was referred to OT for sensory processing difficulties. He lives in a rural area and has been unable to receive OT services. He does receive speech therapy in the home setting. He is currently on a waitlist for ABA services. George’s parents are very eager to start with telehealth OT services to address his sensory needs. OT goals established by the team are to help George get ready for pre-school and stay seated for activities like mealtime or other fine motor tasks.
- Family:
- George has a teenage sister and is primarily cared for by his mother. His father works nights therefore is typically only available on the weekends to help with George. George was recently diagnosed with Autism and was assessed by EI for OT. Parents identified their main concerns are about managing George’s sensory needs. They report that George’s sensory needs continue to seem to impact everyday activities: eating together for family meals, following simple directions, and going places.
Let's move on to a case study. We are going to start with George. George is three years old with a diagnosis of autism. He was referred for OT for sensory processing difficulties. He lives in a rural area and has not been able to receive OT services. He does receive speech therapy in the home setting. He is currently on a waitlist for ABA services. George's parents are very eager to get started with telehealth OT services to address his sensory needs. OT goals have been established by the team to help George get ready for pre-school, stay seated for activities like mealtime, and other fine motor tasks. This is similar to a real case, but I have added a little bit of information for teaching purposes.
Based on the medical records, George has a teenage sister, and he is cared for by his mother as his father works at night. He is only available on the weekends to work with him. George has a recent diagnosis of autism and was assessed for early intervention by OT. The parents' main concern is managing George's sensory needs. They report that George's sensory needs continue to impact everyday activities like eating together, George following simple directions, and going places. Based on that, I bet you are thinking, "Is this going to be a direct therapy child or parent coaching?" While there are some three-year-olds who can do direct therapy in telehealth, George is not a good candidate due to his age and sensory issues. We also know that following directions is difficult for him. Thus, treatment was given via parent coaching.
Step 1: Evidence-based Decision Making
- What does the research say about efficacy in pediatrics?
- Autism spectrum disorder (Sutherland R., & Trembath D. et al., 2018)
- Children with complex communication needs (Douglas et al., 2018)
- Telepractice when training parents/caregivers of children ages birth to three (Behl et al., 2017)
- Family-Centered occupational therapy and telerehabilitation for children with autism spectrum disorders (Gibbs et al., 2011)
What would I do first? After I have read the medical history and made sure that he qualifies for telehealth services based on the AOTA decision-making guide, I would look at all the autism research. This is fairly easy to do on Google Scholar. I have highlighted a few for you. Some of them are fairly recent. I liked this one from 2011 because it really gave a family-centered approach. The first thing you want to think is, "Is there efficacy to support what I am about to do?"
Step 2: Schedule a Pre-session Screening
- Observe the setting.
- Observe the parent interaction with the child.
- Build rapport with the parents and the child.
- Explain the process involved in telehealth.
- Troubleshoot possible technology issues.
- Check logistics (connectivity, privacy, etc.).
- Establish parameters for technology issues and sessions.
- Assess the child’s behaviors.
- Discuss the child’s preferred vs. non- preferred activities.
- Review evaluation results.
I would then schedule a pre-session screening. "I really would like to be a silent observer." I would not put my video on because I would not want to influence George's behavior. There is a term for that called reactivity. By my mere presence, his behavior might change, and therefore, I may not be able to really learn about their situation. I want to observe how the parent interacts with the child. Are they passive? Are they authoritative?
You also want to build rapport with the parent(s) and child. I like to do this at the end. Let's say it is a 30-minute observation session. I will observe for about 15-20 minutes, and then for the last 10 minutes, I might try to talk to the parent and possibly engage with the child. I will also explain the process involved in telehealth, make sure I go through all the technical issues and logistics, and educate on privacy and informed consent. I am also taking lots of mental notes on the child. I want to look at preferred and non-preferred activities and review all the evaluation data before I end the session.
Step 3: Troubleshooting Telehealth: How Did the Session Go?
- Telehealth appointments initially occurred in the living area of the main floor, which seemed ideal because George was very active and the large open floor plan provided him with plenty of room to run.
- The family positioned a laptop in one corner of the room to provide a wide view of the entire living area.
- George began to run from the living area to rooms outside of the camera’s view and to hide behind furniture in the room when the parent initiated interaction.
- Repositioning the laptop did not provide a complete view of all areas surrounding the large couches and recliner chairs in the room.
- George’s mother blocked attempts to elope from the living area and to move the laptop whenever he hid behind furniture so that he would be in the therapist’s view.
- George’s father also assisted with blocking when he was available.
- However, blocking often evoked aggression toward his parents.
How did George do? When I observed George, we were situated in the living room that was a very big open space. It was an open floor plan with plenty of room. The family had positioned the laptop in one corner of the room so I could see a nice big area which was great. However, George ran from one end to the other, and sometimes I could not see him as he would go behind the furniture. Every time his mom asked him to do anything, he would just run away. He was a happy little guy, but he liked to run. I had the mom reposition the laptop so I could see more of the space. I also asked her, "What do you typically do when he runs off?" She replied, "I try to block him." Mom also stated that when dad was available they could contain him a little better. George also hit and threw things, especially when he was blocked.
- What We Learned From the Screening
- Behavior:
- He had difficulty sitting still.
- He left the room several times.
- Did not purposefully play with a toy.
- He was not able to follow 1- step directions.
- He was constantly running and jumping on the couch.
- He covered his face often with objects and liked to smell things.
- He dumped toys on the floor and walked/laid on them.
- Setting:
- Family room with a lot of toys
- A cat named Toby.
- TV on in the background
- Teen sister on her phone in the room
- Parent interaction:
- Mom chased after George most of the session.
- Used bribing to get him to follow directions
- Had difficulty with getting George to listen
- George’s Preferences
- Loves to eat bacon
- Watching YouTube videos on water parks/slides
- Behavior:
What did I learn from the screening? As I mentioned, I did try to build rapport with George during the last 10 minutes. It was very difficult as he kept running off. I asked the mom if she had bubbles. With her blowing those, he came for a little bit, but then he took off. At this point, I did not know what George liked and was trying to randomly figure it out. She did indicate that he liked the iPad so we did do a little of that, but it was not a very engaging session.
After the session, I sat down and looked at each area and started with behavior. He had an awful time sitting still, and I did not see any purposeful play. There was a lot of dumping of toys, jumping, walking on toys, and just running around. Mom gave him many one-step directions like "pick this up," "come sit down," "give me the remote," and other commands that were familiar to him. He was constantly moving, covered his face often, and liked to smell things. For example, he smelled his mom's shirt during the session.
The setting was in the family room and it had a lot of toys. There was a cat, a TV, and his sister was on her phone.
As far as parent interaction, I saw a lot of passive parenting. Mom was chasing George a lot, and there was a lot of bribing going on to no avail. George was unable to attend.
Lastly, I jotted down George's preferences. After the session, I asked George's mom to tell me a few things that George liked. She told me that he liked Curious George, water slides, and bacon. I decided to use this as his "currency." It is what makes them want to do different activities.
Step 4: Exploring Options
- Transitioned sessions into a playroom to address the escaping behavior and so parents could gain some control over the session.
- Toys were placed in bins with lids
- Created a sensory bin of activities George enjoys.
Step four is exploring options. With the preliminary data, I needed to determine options. The family room was a disaster, and I talked to the mom about modifying certain things like choosing his bedroom or a playroom where it was a little more confined. I wanted her to be able to close the door so chasing was not the activity. I also advised her to put the toys away in bins with lids so she could control that. I also suggested a sensory bin based on his sensory needs.
Step 5: Establish Parent-training Friendly Goals
- “I want George to sit and actually play with his toys. All he does is throw things, dump containers. He does not follow any directions, and I cannot get him to sit still and to do anything. I am so exhausted by chasing him around all day and trying to keep him quiet so my husband can rest before his night shift. Plus, my daughter needs me too. We are all so tired and frustrated.” -George’s mom
- George will sit down for meals at the table with his family. -EI goal
- George will sit and complete 1 activity at the table with parent independently.- Parent training goal
We need to establish goals that are parent-oriented and not based on early intervention (EI) or an outside setting. George's mom said, "I really want him to sit and play with his toys. I don't want him to throw things. I want him to follow directions and don't want to chase him around." It was really important for George's mom and their family to get George to actually sit and do something purposeful and to follow directions as it was impacting the family dynamic. For the EI goal, it was that George will sit down for meals at the table with his family which is a perfectly brilliant goal. The problem with this goal is that it is too big. When you are doing pediatric telehealth, you need to shave down the goal to the basic skills using task analysis. The goal that George's mom and I came up with was, "George will sit and complete one activity at the table with the parent independently." This seems like a small thing, but it was very hard for George so this is where we started.
Step 6: Sensory Vs. Behavior?
- Sensory Profile
- Need to smell things
- Seeking movement/ proprioceptive input
- Visually distracted
- Difficulty with tolerating sounds (multiple directions)
- Behavioral Profile
- Task avoidance
- Sensory seeking behavior
- Reinforcers: Curious George, water slides YouTube-videos
I also needed to figure out what was sensory and what was behavior. I typically make two columns and write down what I see. I also refer to the sensory profile. However, I like to be very objective in what I have seen during the session. I know that he needed to smell things and was seeking movement. He also was very distracted and had difficulty tolerating sound. Behaviorally, I know he was avoiding tasks and demonstrated sensory seeking behavior. His reinforcers were Curious George and water slide You-Tube videos. I could use these to troubleshoot with George.
Step 7: Troubleshooting Telehealth
This chart in Figure 3 also helped me figure things out.
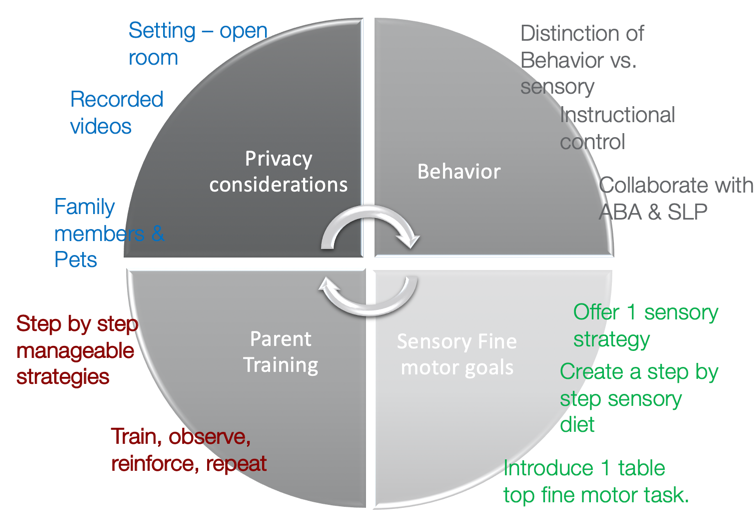
Figure 3. Telehealth chart.
I went through each area to figure out my strategies. I needed to figure out his behavior to determine whether it was behavioral or sensory. I also talked to his SLP as she was already working with him. I also looked at fine motor and sensory goals. I need to figure out which ones were what and how would I create those. I decided to offer one sensory strategy at a time and create a very step-by-step sensory diet for mom. For parent training, I made sure to go step-by-step, train, observe, and then reinforce. Lastly, I need to look at privacy considerations. The teenage sister was on her phone when I was observing. That was a privacy issue, and I needed to make sure mom is aware of that. I also needed to consider the pet in the room (cat) and how that impacted treatment. You have to be careful with liability issues as well because that is your session. For example, if I say, "Mom, I want you to record your nighttime routine," I need to consider privacy when she is sending those videos to me. The setting was an open room, and anyone could be coming in.
- What sort of asynchronous methods would I consider for George?
- Resources on sensory processing: websites, videos, books, etc.
- Photographs
- YouTube videos
- OT blogs
- Recorded videos.
I referred mom to certain resources online, visual schedules, videos, blogs, etc. using the disclaimer that they were only resources. "I am happy to talk to you and work through them to make sure there are applicable to George."
Step 8: Set Up a Sensory Diet (Synchronous)
- Daily at 8:45 am for 20 mins
- Transition into George’s bedroom
- Limit options of toys to 1 box with a lid
- Let George do what he likes to do: running and jumping but suggest he carries a heavy backpack while engaging in these activities
- Have an activity set up at the table and an edible reinforcer
I set up a sensory diet and started very small. This is the schedule I created for his mom. Every day for 8:45 I had her go to his room for 20 minutes and limit how many toys he could have. He could play with those select toys, but he also had to carry a heavy backpack while he was doing it. She was then to try to get him to come to the table with her. And because bacon was his reinforcer, she was not to give him bacon at any other time. It was only available as a reinforcer if he sat at the table. Once seated, she was to offer him one activity and present the reinforcer.
Step 9: Choosing the Right Fine Motor Activity
- The activity criteria:
- Easy motor skill
- Purposeful play
- Grasp and release
- Setting up for success
- Repetitive
- Short
It was also really important to choose the right activity for George. A simple idea was putting coins in a piggy bank. It needed to be short, repetitive, and easy.
Step 10: Change Parent Behavior to Change Child’s Behavior
- DO’s
- Set small expectations.
- Short succinct directions.
- Boundaries (table and chair)
- Short sessions (starting with 5 mins)
- Praise desired behavior
- Be a light switch
- 1:1 ratio for reinforcement
- DON’Ts
- Give attention to undesired behavior.
- Save preferred reinforcer for playtime with mom.
- Block and redirect to the desired behavior.
You have to change parent behavior to change the child's behavior. It is important to set small expectations with very short directions. It is also important to use a boundary like a table and a chair. Praise whenever possible. Be a light switch. This means go crazy with reinforcement and accolades when they do something right. "You did brilliantly!" And then when they are not doing what you want, you shut off like a light switch and give them no reaction whatsoever. Use a one-on-one ratio for reinforcement. For every one thing that they do for you, they get one thing they want to do. This could be a YouTube video, bacon, or whatever. Again, anytime he is running off or doing an undesired behavior, as long as the door's closed, you ignore him. It is important for the caregivers to save the preferred reinforcer for playtime, and then block and redirect desired behavior.
Step 11: Is the Intervention Working?
- Review warning signs of sensory overload.
- Make it easy for parents to collect data.
- Collective data-based decisions.
You want to then see what is working. You want to make sure mom understands the signs of sensory overload because that may happen. You are not going to be there all the time, and she needs to know. Figure 4 shows a chart that can be used to collect data.
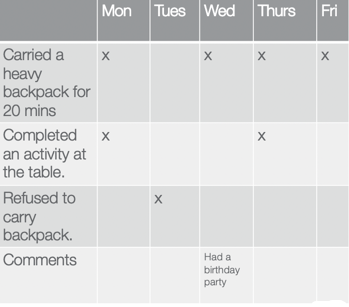
Figure 4. Data chart.
Make it super easy for the caregiver to collect data that can then inform your decisions.
Step 12: Observe & Provide Reflective Feedback
- Vocal prompts and feedback while observing a parent implementing the procedures.
- Parents may video record sessions throughout the day/week.
- Generalization?
You want to observe and then provide feedback. For example, you may say, "You did brilliantly. I want you to do the same thing every day, but next time with a different activity, record it, and send it to me." This is so you can see if the instruction is generalizing.
Step 13: Grading Activities/Reinforcement for Success
- Increase the expectation: Make it a 2-step activity: Find coins in rice and then place them in a container.
- Increase the duration: Add a variety of similar activities.
- Use the 1: 3 ratio.... i.e. For every 1 (difficult) novel task engage in 3 familiar (easy) activities.
- Fade out prompts.
- Decrease frequency of reinforcement: 1:3 ratio...
How can you make tasks easier or harder? It is important to grade activities and there are some suggestions above. I also like to use a 3:1 ratio. For every task that you perceive as difficult for George, you want to do three easy things like blowing bubbles or something very simple. You also want to fade out prompts or decrease the frequency of reinforcement to make things a little harder. For example, for every one task you do, I am going to give you reinforcement. Then, I start to space that reinforcement out.
Parent Perceptions of Telehealth Parent Training
- Research suggests that OBC significantly increases parent self-competence (Little et al., 2018a).
- Parents perceived the parent-therapist relationship supported parents’ feelings of self-efficacy.
- Parents reported that the process of analyzing and reflecting with the therapist serving as the ‘coach’ was a core component of increasing self-efficacy (Foster, Dunn, Mische, Lawson, 2013).
What do parents think of this type of training? Based on the research, there is a lot of positive feedback. While I am very confident that parent-based coaching works, it does not always fit every family.
Feedback is Important for Growth
- What was different about your experience with telehealth versus other services?
- What was the quality of your experience?
- What did you like most about telehealth?
- What did you like least or would like to change about telehealth?
- What would you like to share with other parents about this experience?
- Tell me some things that you understand differently after our experience together.
- How was the telehealth intervention consistent with the services you have used in the past?
- Is there anything that you are doing differently after the telehealth intervention?
- How do you problem-solve challenges now?
- What was the most helpful component of the intervention process?
(Wallisch et al., 2019)
Feedback once again is the most important thing. This is an article in 2019 by Wallisch and colleagues that provides you with some questions that you can ask the parent if you want some feedback. In this article, most parents felt parent empowerment, a collaborative relationship, and improved compatibility with daily life.
Case Study 2: Ryan
- Ryan
- 7 yrs. Old
- Handwriting goals:
- letter reversals
- sizing & placement
- letter formation
This is an older student and a school referral, so handwriting. Ryan's issues included letter reversals, sizing, placement, and poor letter formation.
Step 1: Informed Consent and Parent Expectations
- Become familiar with and maintain video technology.
- Communicate with me before each session through emails to receive documents and a list of materials that would be needed for the session.
- Plan and set up the treatment area prior to the session.
- Review the session plans and gather materials prior to the session.
- Photograph and email their child’s completed homework before the session.
- Provide guidance prompts to the child if required during the session.
- Meet during the last 5-10 minutes at the end of the session to allow for questions, feedback, and goal review.
- Provide feedback to the therapist and engage in open communication to problem solve concerns.
We needed to make sure that we got informed consent and reviewed parent expectations. This could be done via email or a video session. We would also want to watch them writing and see samples of their work.
Step 2: Review the Research
- Criss, M. J. (2013). School-based telerehabilitation in occupational therapy: Using telerehabilitation technologies to promote improvements in student performance. International journal of telerehabilitation, 5(1), 39–46. https://doi.org/10.5195/ijt.2013.6115
- Peterson, C. Q., Nelson, D. L. (2003). Effect of an occupational intervention on printing in children with economic disadvantages. American Journal of Occupational Therapy, 57:152–160.
- Bayona, C. L., McDougall, J., Tucker, M. A., Nichols, M., & Mandich, A. (2006). School-based occupational therapy for children with fine motor difficulties: Evaluating functional outcomes and fidelity of services. Phys Occup Ther Pediatr., 26(3):89‐110.
I have highlighted above some really nice articles that can help you get an idea of the efficacy of this type of intervention with students.
- Assess the efficacy of telehealth OT for school-related goals
- Direct OT services in the public school environment, typically consisting of 20-30 minutes per week, do not always result in the most ideal or effective outcomes if there is limited follow-through in the classroom or home environments during other times of the week.
- The most successful outcomes: consultation OT services, in which the therapist provides strategies and solutions to staff and caregivers to use at school and at home with the student.
- There is some conflicting evidence: several studies reveal positive outcomes, including functional outcomes and teacher perceptions, with its use (Bayona et al., 2006; Casillas, 2010; Dreiling & Bundy, 2003; Dunn, 1990)
What type of goals are you going to set for this student? Again, it is important to complete a pre-session screening observation.
Step 3: Pre-session Screening Observations
- Fairly compliant- moderate cues to stay on task
- Would walk away randomly
- Verbal outbursts
- Does get distracted easily
- Responds well to a visual schedule
- Does not need a facilitator present
- Likes tactile activities (i.e. sensory play and candy)
- Send parent with available items checklist
(sample attached in downloads)
For Ryan, he was fairly compliant. He would walk away sometimes, have verbal outbursts, or get distracted somewhat easily. However, he did very well with a visual schedule as per the parent report and teachers' notes. Thus, I did not feel like he needed a facilitator. He likes sensory activities so I sent the family a checklist of items to use.
Step 4: Environmental Modifications
- Use of a pencil grip
- Modified paper style
- Change in paper position
- The slant of paper on the desk
- Use of easel
- Seating position
- Distractions
- Parent engagement during the session
- Siblings
There are several areas to look at for environmental modifications. Does he need a pencil grip, a slant board, or special seating? Where is he located? He worked in his room because his siblings were an issue. Here is a sample of a visual that I used with him in Figure 5.
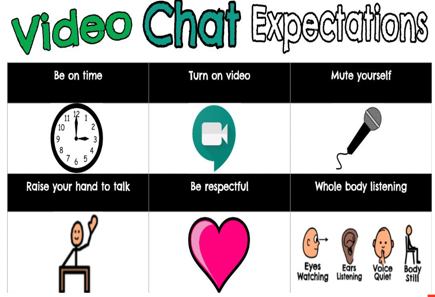
Figure 5. Visual schedule.
This gave him the expectations for our session. I also used the following checklist in Figure 6.

Figure 6. Checklist.
"Do we have everything we need?" He was able to click off the items on the checklist when I shared a screen. He knew that we had to do these three activities before he got a break. Every time he completed one, he would check it off. This is a great way to engage a student. You can also add different elements within PowerPoint, like sound effects. Sometimes as a reward, he could choose or change the sound effects.
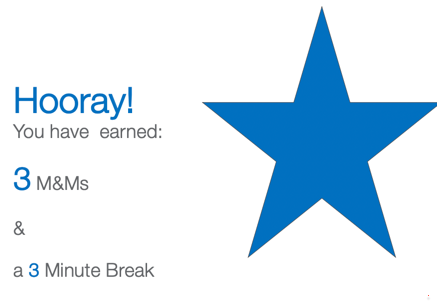
Figure 7. Visual about a break.
You could even create a slide about the child's reward such as this one.
Step 5: Review the Research on Handwriting
- The use of a combination of intervention approaches has been found to be effective in improving handwriting performance (Peterson & Nelson, 2003)
As the goal was handwriting, I reviewed the research on handwriting and figured out options for telehealth.
- Employing multisensory strategies in telehealth
- Finding treasures in therapy putty, feeding “tennis buddy,” and playing frog jump races using finger isolation to make plastic frogs bounce across the table.
- Sensory, strengthening, stretching to prepare the student for seat work....eg.“boxing” or “archery” using therapy band, treasure go noodle, and brain gym exercises.
- Stamp-and-See Screen, as well as the Wet-Dry-Try Method using sponges, chalk, and chalkboard.
- Building and tracing letters using manipulatives such as Wikki Stix, Play-Doh, or spaghetti.
- The whiteboard tools to trace or dot to dot activities.
- Other kinesthetic strategies included air writing and palm writing with eyes open and closed.
- Visual charts and/or checklists were also used to encourage the students to evaluate their written work.
Some of the data used a multisensory approach, stamp and screen, wet-dry method, spaghetti, Wikki Stix, etc.
Step 6: Handwriting Synchronous Vs. Asynchronous Methods
- Synchronous
- Mirror iPad to draw.
- Doc- cam
- Sign in with 2 devices
- Asynchronous
- Workbook
- Printable sheets
- Send Photograph of work
You could use a hybrid approach using both synchronous and asynchronous methods. I used an iPad with a stylus so I can see how he was writing. You can also use a doc cam. Another way if for the parent to use her phone and FaceTIme to see his writing in real-time. This is signing in with two devices. Asynchronous formats would be sending a workbook, printables, and sending photographs of the work during the session.
Step 7: Keeping Students Engaged
- Pair yourself with reinforcement
- Fixed ratio 1:1 of reinforcement
- Stickers on your face
- Puppets
- I Spy game
- Visual timers
- Reinforce desired behavior
- Trade places
- Withhold reinforcer
- Difficulty of exercises
Some of our older students can be hard to keep engaged. The best thing you can do is pair yourself with reinforcement. Going back to the previous example, George loved bacon. If every time I have my session with him on telehealth his mom has a plate of bacon, he is going to pair me with that reinforcer of bacon. He knows that any time I am around, he is going to get that reinforcer. This is basic applied behavior analysis.
Initially, I paired myself with sitting with mom on the screen and bacon. Then I asked him to do something. "George put the coin in," and he put the coin in. I very enthusiastically praised him, and then his mom gave him the bacon. He knows that every time he sees me, it is going to be a positive experience. This is the setting that we want to create. We are using a fixed ratio of reinforcement.
Ryan was the funniest thing. One day, I put a sticker on my face, and he just thought it was the funniest thing. He began to work for me to put stickers on my face. He was having fun and being silly. This is what pediatric telehealth is all about. The more fun you are having, the more you are pairing yourself with fun. When you can do that, you have greater compliance and progress.
I used visual timers a lot and shared my screen to do that. Trading places was one of my favorites with Ryan as the therapist and I was Ryan.
Step 8: Parent Perceptions
- 86% observed improvements in the students’ school performance related to the IEP goals as a result of telehealth OT.
- 71% disagreed with the statement, “I would prefer that occupational therapy in a clinic instead of virtually.”
- 86% of the learning coaches (all but one who checked the neutral response) revealed that they were happy that the services were provided in an online format.
- Criss M. J. (2013). School-based telerehabilitation in occupational therapy: using telerehabilitation technologies to promote improvements in student performance. International journal of telerehabilitation, 5(1), 39–46.
Most parents really like this type of intervention for school-aged kids in the telehealth intervention. Ryan's mom said that initially, it was work but that she liked it. Now, Ryan is independent, and she does not really have to do much. Again, this is not for everyone. I saw that a family said this on Facebook. "I am not having fun, and it's too much work. I just see the OT or whoever sitting there and I am doing all the work."
- Always consider clinical & ethical judgment
- AOTA clearly states in its 2013 paper titled, “Telehealth,” ........
- It is not an indication that it is appropriate for all situations. The fact is that telehealth as a service modality “has potential” and should be utilized only after each case has been evaluated individually based on “the variability of client factors, activity demands, performance skills, performance patterns, and contexts and environments using clinical judgment, the client’s informed choice, and professional standards of care (p. P S70)”
If it is not appropriate, what other alternatives can be offered?
Time for Telehealth
- Session preparation for items to sent to parents
- Preparing scanned items
- Additional emailing required
- Receiving and printing items sent from the parents
- Troubleshooting technology
- Lesson planning
Lastly, make time for telehealth. Telehealth takes a lot of work. There is a lot of time you have to spend preparing items, scanning, and reviewing. Make sure you are taking time to do that and planning that into a day. It cannot just be sessions back to back because you will get burned out.
Questions and Answers
What is your recommendation when families just are not interested in being involved at all?
It depends on the age of the child, and this is where your clinical j
