Editor's note: This text-based course is a transcript of the webinar, Understanding Asthma And Anaphylaxis In The Occupational Therapy Setting, presented by Nancy Nathenson, RRT.
Learning Outcomes
- After this course, participants will be able to evaluate the overall impact of asthma and anaphylaxis in the US.
- After this course, participants will be able to apply the essential knowledge and self-management for asthma and anaphylaxis for patients and caregivers.
- After this course, participants will be able to identify the difference between the early and late warning signs of an asthma attack
Introduction
My decision to pursue a career as a respiratory therapist was greatly influenced by my mother's struggle with severe allergic asthma. Her journey with this condition began when she was just 14 years old. I vividly recall the story she shared with me about visiting the doctor, only to be told that her symptoms had miraculously disappeared. The explanation? She had supposedly "outgrown" her asthma due to her active lifestyle, particularly her penchant for riding her bike.
However, life took a turn when my father, a military personnel, was stationed in Japan. The environmental conditions, particularly the presence of volcanic ash in Yokohama (Yokohama asthma), triggered a resurgence of my mother's allergic asthma. The challenges she faced during this time left a profound impact on me.
Every day, as I work in the field of respiratory therapy, I carry with me the memory of my mother's struggles. This dedication to her serves as a constant reminder of the importance of my work and fuels my commitment to helping others manage their respiratory conditions with compassion and expertise.
What is Asthma?
- Chronic (life-long) disease of the airways often related to allergies and may cause:
- Wheezing, breathlessness, chest tightness and nighttime or early morning coughing
- Symptoms may come and go, but the threat of an asthma attack is always there.
- ***Episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment.***
Asthma is a chronic and lifelong condition affecting the airways, often linked to allergies. Approximately 50% of adults grapple with allergic asthma, which can manifest in various symptoms, including wheezing, breathlessness, chest tightness, and nighttime or early morning coughing. Though symptoms may fluctuate, the specter of an asthma attack looms persistently.
Episodes typically entail widespread variable airflow obstruction, which can often be reversed spontaneously or with treatment. Treatment commonly involves bronchodilators or short-acting beta-two agonist therapy to alleviate symptoms and restore airflow.
Asthma Pathophysiology
- Bronchoconstriction
- Airway narrowing and subsequent interference with airflow
- Airway hyper-responsiveness
- Exaggerated response to stimuli
- Airway Edema
- As the inflammation becomes progressive edema, mucous hypersecretion and plugs further limit airflow.
The pathophysiology of asthma encompasses several key mechanisms. Bronchoconstriction, characterized by the narrowing of airways, impedes airflow due to the contraction of the smooth muscle surrounding the bronchial tubes.
Additionally, individuals with asthma often exhibit airway hyperresponsiveness, an exaggerated reaction to various stimuli that trigger symptoms. Airway inflammation leads to progressive edema, contributing to further obstruction.
Moreover, mucus hypersecretion and the formation of mucus plugs exacerbate airflow limitation, compounding the challenges faced by individuals with asthma.
Asthma Causes
- Genetic and environmental factors
- Family Hx of allergies or asthma
- Mother’s smoking, exposure to secondhand smoke or air pollution while pregnant
- Early childhood exposure to secondhand smoke, air pollution, indoor allergies
- Damage to lung development from premature birth or early childhood respiratory illnesses
- For adults, exposure to industrial dusts or chemicals in the workplace
Asthma is influenced by both genetic and environmental factors. The hereditary component of asthma is significant, with a child having a 25% higher likelihood of developing asthma if one parent has the condition and a 50% higher likelihood if both parents are affected.
Environmental factors also play a crucial role. The environments we inhabit, whether at home, outdoors, or in the workplace, can contribute to asthma development. Factors such as a family history of allergies or asthma, maternal smoking during pregnancy, exposure to secondhand smoke, and air pollution during pregnancy are known to increase the risk.
Furthermore, early childhood exposure to secondhand smoke, air pollution, and indoor allergens, as well as lung damage from premature birth or frequent respiratory illnesses, can heighten susceptibility to asthma. Occupational exposure to industrial dust or chemicals can also lead to a condition known as occupational asthma.
Asthma Statistics
These are asthma statistics from 2023 from the Allergy and Asthma Network (Figure 1).
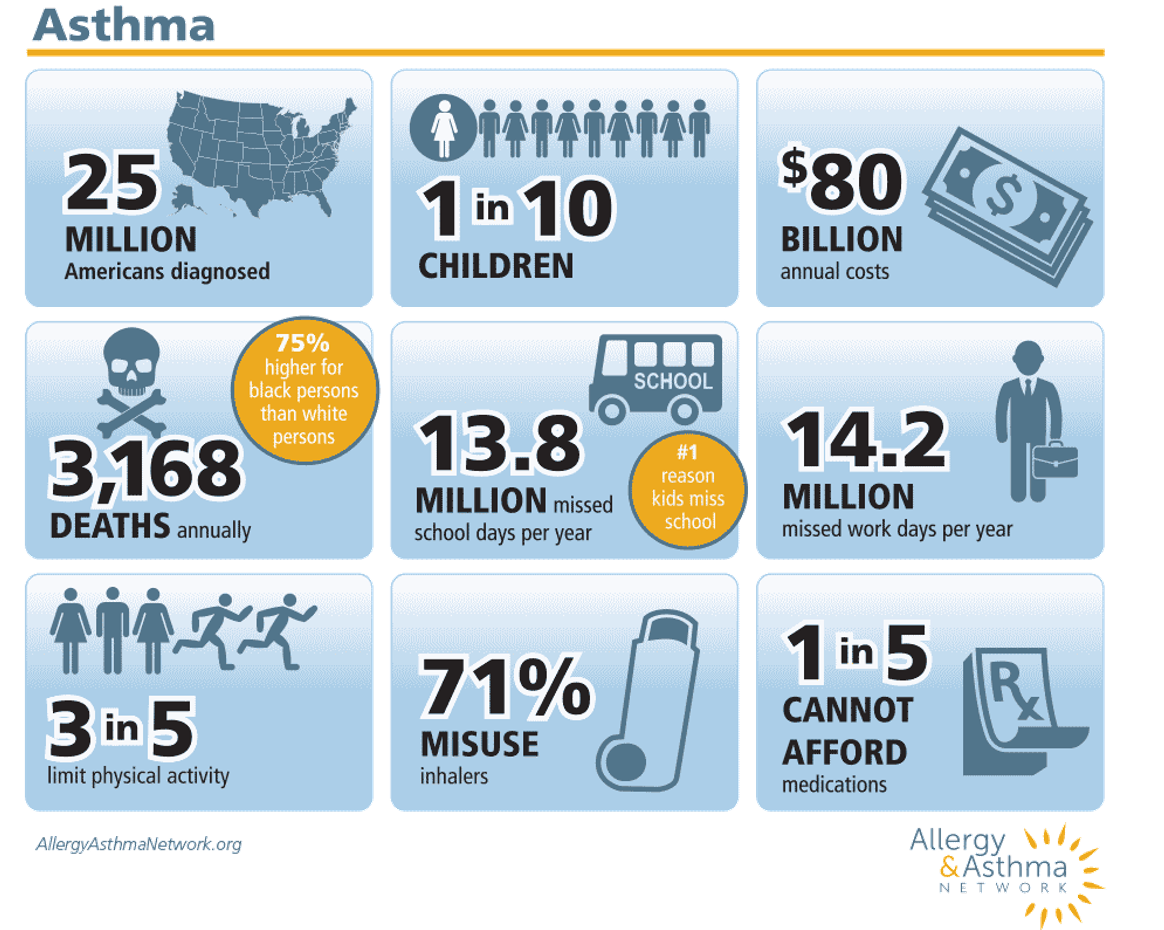
Figure 1. Asthma statistics. Free download from the Allergy & Asthma network.
Asthma affects a significant portion of the American population, with approximately 25 million diagnosed individuals and an undisclosed number who remain undiagnosed. Among children, one in ten is impacted by this condition, resulting in considerable financial burdens attributed to expenses such as medications, emergency room visits, and hospital admissions.
Tragically, over 3,000 deaths occur annually due to asthma-related complications, with mortality rates disproportionately affecting Black individuals, who face a 75% higher risk compared to their white counterparts. Alarmingly, a significant portion of these deaths—about one-third—occur in individuals diagnosed with only mild forms of the disease, amounting to approximately 1,000 lives lost each year.
The ramifications of asthma extend beyond mortality, with an estimated 13.8 million missed school days annually, making it the leading cause of absenteeism among students. Similarly, 14.2 million workdays are lost each year due to asthma, impacting not only individuals but also their families and the economy at large. Moreover, three in five individuals with asthma report limitations in their daily activities due to the condition.
A concerning trend emerges regarding inhaler misuse, with a staggering 71% of patients failing to use their inhalers correctly. This underscores the critical need for healthcare providers to possess comprehensive knowledge of asthma management and the proper administration of medications. By enhancing our understanding of asthma and optimizing asthma care practices, we can strive for improved outcomes and better quality of life for patients.
Compounding the challenges faced by asthma sufferers is the issue of medication affordability, as one in five individuals struggle to afford their prescribed medications. Asthma patients may incur expenses of up to $3,000 or more annually solely on inhalers, further highlighting the economic strain associated with managing this chronic condition.
Asthma Disparities/Rates
- Factors that contribute to disparities:
- Access to care
- Income
- Environmental Allergens and Irritants
- Education Inequality
- Language and Cultural Differences
- Asthma Rates
- More women than men have asthma
- Highest Asthma rates in U.S. are with persons:
- on Medicaid
- living below the poverty level
Disparities in asthma prevalence and outcomes stem from a myriad of interconnected factors, many of which are well-documented. Access to healthcare services, influenced by income levels and geographic location, plays a pivotal role, as does exposure to environmental allergens and irritants, which can vary significantly based on socio-economic status and residential area.
Educational disparities, income inequality, and language and cultural differences further compound the issue, exacerbating disparities in asthma rates and outcomes. Despite the existence of evidence-based guidelines for asthma evaluation and treatment, adherence to these guidelines among healthcare providers remains inconsistent. Coupled with the prevalent issue of patient misuse of medications, these factors contribute to suboptimal outcomes for many asthma sufferers.
In the United States, asthma rates persist at alarming levels, with certain demographic groups disproportionately affected. Individuals enrolled in Medicaid and those living below the poverty level experience the highest rates of asthma. Additionally, according to data from the American Lung Association, African Americans, Hispanics, and non-Hispanic individuals bear the brunt of asthma's impact in the country, highlighting profound disparities in asthma prevalence and outcomes across racial and ethnic lines.
Anxiety and Depression in Asthma Patients
- Individuals with asthma are 25%-49% more likely to have symptoms of anxiety and depression.
- Asthma is the leading chronic illness for children and adolescents.
- Research shows that there is evidence of anxiety disorders 3 times higher in pediatric asthma than in children without asthma.
- Causal relationship between developing anxiety and depression and dyspnea
The intersection of respiratory diseases and mental health, particularly anxiety and depression, is a significant yet often overlooked aspect of patient care. Anxiety ranks as the fifth leading cause of years lived with disability in the United States, while depression holds the second position in terms of years lived with a disability. Individuals with asthma face heightened risks, with research indicating that they are 25% to 49% more likely to experience symptoms of anxiety and depression.
Asthma stands as the predominant chronic illness affecting children and adolescents, further underscoring the importance of addressing mental health concerns in this population. Studies reveal a threefold increase in the prevalence of anxiety disorders among pediatric asthma patients compared to those without asthma. Moreover, a causal relationship has been identified between the development of anxiety and depression and the sensation of dyspnea or difficulty breathing, as seen in Figure 2.
Understanding the psychological impact of respiratory symptoms is crucial, as individuals may instinctively avoid activities that exacerbate breathlessness, thereby compromising their quality of life and overall well-being. Recognizing and addressing the mental health needs of patients with respiratory conditions is essential for comprehensive and effective health management.
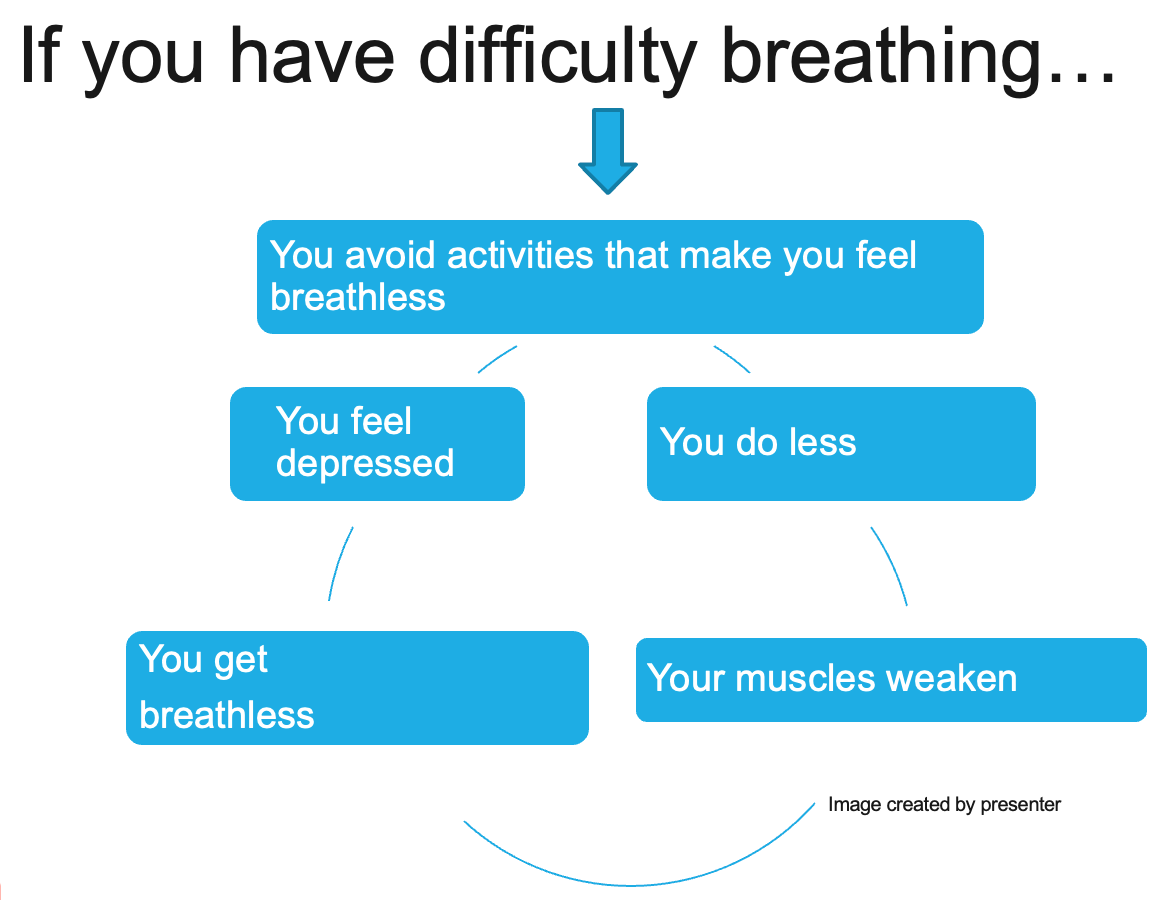
Figure 2. Difficult breathing cycle illustration.
This cycle of decreased activity, resulting in muscle weakness, increased breathlessness, and subsequent feelings of depression, perpetuates a challenging cycle for individuals with respiratory conditions. The avoidance of activities exacerbates breathlessness, further diminishing their quality of life and sense of well-being.
As healthcare providers, our role is crucial in breaking this cycle and empowering individuals to regain control of their lives.
Anxiety in Asthma Patients
- This anxiety is associated with…
- Dyspnea
- Inability to perform ADLs
- Inability to fulfill social roles
- Rehospitalizations
Anxiety is associated with dyspnea. The constant struggle with shortness of breath is closely associated with feelings of anxiety and depression. These emotional challenges are exacerbated by the limitations imposed on individuals, preventing them from fulfilling their roles and participating in activities they enjoy. Additionally, recurrent hospitalizations due to respiratory exacerbations further contribute to the cycle of anxiety and depression. Our role as healthcare professionals is to provide comprehensive support and interventions to address both the physical symptoms and the emotional toll of respiratory conditions, thereby improving the overall quality of life for our patients.
Common Symptoms of Asthma
- Frequent cough, especially at night
- Shortness of breath or rapid breathing
- Chest Tightness
- Wheezing
- Behavior changes (i.e., anxious, lethargic, agitated, confused)
When it comes to diagnosing asthma, it's essential to conduct a thorough assessment to rule out other conditions that may present with similar symptoms. Conditions such as gastroesophageal reflux disease (GERD), obstructive sleep apnea, and sinus issues can mimic asthma symptoms, making accurate diagnosis crucial.
While I won't delve into the detailed diagnostic process here, it's important to recognize that asthma symptoms can vary widely in both presentation and severity. Not all children experience the same symptoms, and manifestations may differ from one individual to another.
Common symptoms of asthma include frequent coughing, particularly at night, as well as shortness of breath or rapid breathing, chest tightness, and wheezing. Additionally, behavioral changes such as increased anxiety, lethargy, agitation, or confusion may accompany asthma exacerbations. It's crucial to understand that symptoms can manifest differently in each child or individual, highlighting the importance of personalized assessment and management strategies.
Categories of Asthma
- Based on “triggers” that cause symptoms or attacks
- Seasonal
- Exercise-Induced
- Allergic
- Nocturnal
The categories of asthma are based on triggers that cause symptoms or attacks.
Seasonal
Seasonal asthma is triggered by trees, grasses, flowers, or climate.
Exercise-Induced
- Triggered by vigorous or prolonged exercise or physical exertion
- Symptoms
- Coughing, chest tightening, wheezing, unusual fatigue, shortness of breath
- May begin during exercise and can worsen 5 to 10 minutes after exercise
- Prevention
- Warm-up and cool down
- Take Quick Relief medications 15-20 minutes prior to exercise
- Symptoms
Exercise-induced bronchospasm can be triggered by vigorous or prolonged physical activity, leading to symptoms that overlap with those of asthma. These symptoms may include coughing, chest tightening, wheezing, unusual fatigue, and shortness of breath. Importantly, symptoms can onset during exercise and may worsen five to ten minutes after cessation.
Preventive measures such as warming up and cooling down are crucial for all individuals engaging in exercise but are particularly important for those with asthma. Additionally, asthmatic patients should consider taking their quick-relief or rescue medications 15 to 20 minutes prior to exercise. These medications help relax the tiny smooth muscles surrounding the bronchial tubes, keeping the airways open and enabling them to participate in physical activities comfortably.
Allergic
- Most common type
- Hypersensitivity to any allergen
- Antibodies trigger a reaction which results in swelling and inflammation
- Sneezing, itchy, watery eyes, runny nose
- Muscles around the airways tighten
Allergic asthma remains the most prevalent form of asthma, characterized by hypersensitivity to various allergens. When exposed to these allergens, the immune system produces antibodies that trigger a cascade of reactions, leading to swelling and inflammation in the airways.
In addition to typical lung symptoms such as wheezing and coughing, allergic asthma often manifests with upper airway symptoms. These can include sneezing, itchy and watery eyes, a runny nose, and overall nasal congestion. Furthermore, the muscles surrounding the airways may tighten, exacerbating breathing difficulties and contributing to the overall symptomatology of allergic asthma.
Nocturnal Asthma (NA)
- Nocturnal asthma is any nighttime worsening of asthma symptoms.
- awakenings
- cough
- wheeze
- difficulty breathing
- Parents often are unaware when their child falls asleep, if they have awakenings, or if they cannot recognize nighttime wheezing.
- NA is linked to an increased risk of mortality.
Nocturnal asthma, characterized by the worsening of asthma symptoms during nighttime hours, is a prevalent and concerning aspect of the condition. Approximately 60% of asthma patients experience nocturnal symptoms, and these episodes are associated with a higher risk of mortality, accounting for 70% of asthma-related deaths and 80% of respiratory arrests caused by asthma.
Symptoms of nocturnal asthma include coughing, wheezing, and difficulty breathing, which can disrupt sleep and significantly impact quality of life. Parents may be unaware of their child's nighttime awakenings and may not recognize the presence of nocturnal wheezing, further complicating management and treatment.
Given the increased risk of mortality associated with nocturnal asthma, it is essential for healthcare providers to educate patients and caregivers about recognizing and managing nighttime symptoms effectively to mitigate the risk of serious complications.
Asthma Control Goals
Asthma control goals begin with the healthcare provider.
Decrease Impairment
- Preventing symptoms such as coughing, breathlessness day or night, or after exercise
- Decrease the need for RESCUE Rx to < 2 days/week
- Maintain near normal lung function
- Maintain normal activity levels
- Meet patients and family's expectations of and satisfaction with asthma care
Our primary goal in managing asthma is to minimize the patient's impairment by effectively preventing symptoms such as coughing, breathlessness, and exacerbations, whether they occur during the day, at night, or after physical activity. To achieve this, we aim to reduce the need for rescue medication to less than two days per week.
Additionally, our objective is to maintain near-normal lung function, allowing patients to engage in their usual activities without limitation. Equally important is meeting the expectations and ensuring the satisfaction of both patients and their families with the asthma care provided. Their buy-in and adherence to the management plan are crucial factors in achieving successful outcomes and optimizing their quality of life.
Decrease Risk
- Prevent asthma exacerbations and minimize ED visits or hospitalizations
- Prevent loss of lung function or in children's lung growth
- Provide optimal drug therapy with few or no adverse side effects
In addition to minimizing impairment, our focus is on reducing the risk associated with asthma by preventing exacerbations and minimizing emergency room visits or hospitalizations. We strive to safeguard lung function and ensure optimal lung growth, especially in children, by effectively managing the condition.
Central to achieving these goals is providing optimal drug delivery while minimizing adverse side effects. It's crucial to address any potential side effects promptly, as they can significantly impact adherence to the treatment plan.
Respiratory Treatments
The treatment of asthma is primarily medication. The Allergy and Asthma Network provides a free download of a plethora of medications that are used (Figure 3).
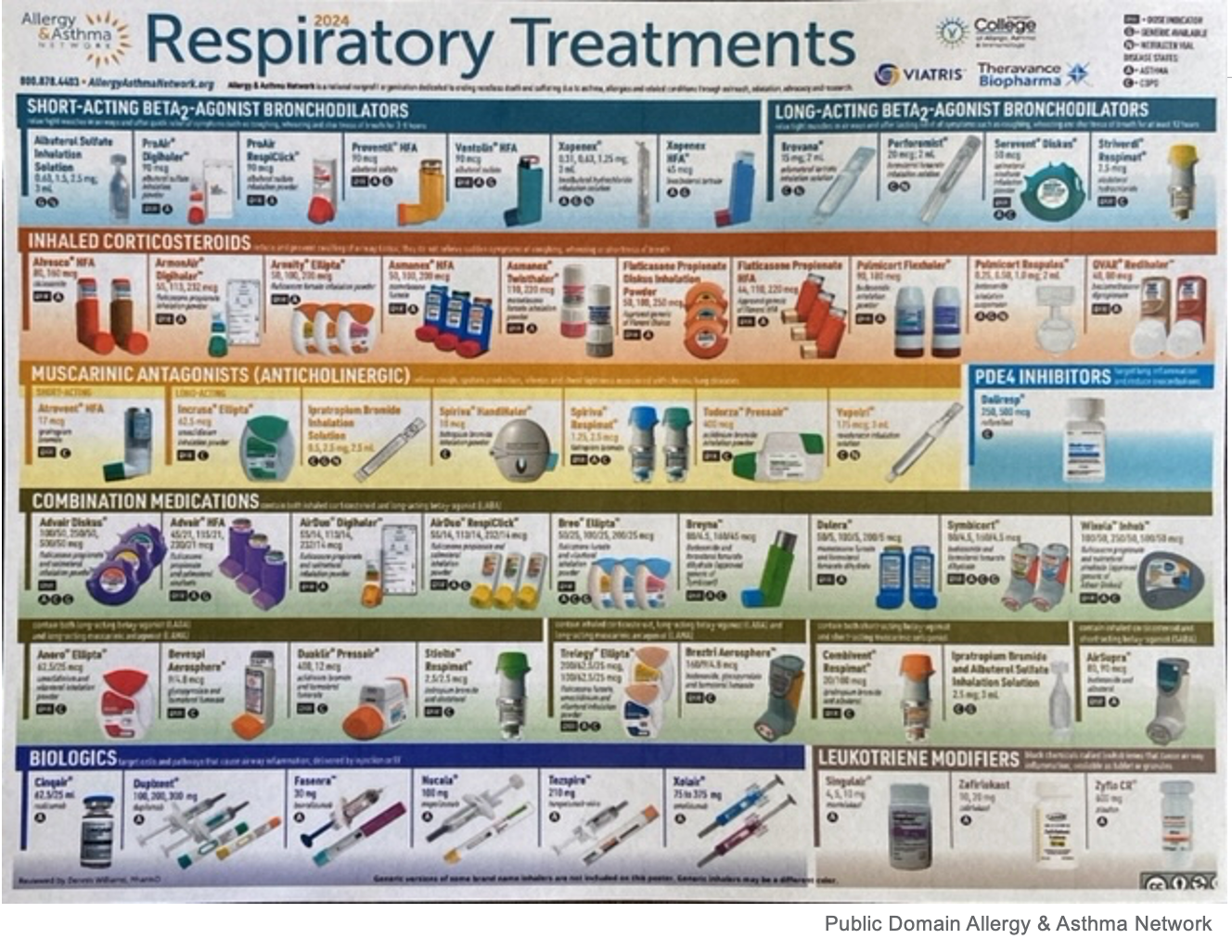
Figure 3. Free download of respiratory treatments from the Allergy and Asthma Network.
Medications for asthma management encompass a variety of options tailored to individual needs. Short-acting beta-agonists, such as albuterol, act as bronchodilators for quick relief of symptoms, providing rapid dilation of the airways. In contrast, long-acting beta-agonists offer sustained bronchodilation over a twelve-hour period, providing extended symptom control.
Inhaled corticosteroids are anti-inflammatory agents that target airway inflammation to reduce the frequency and severity of asthma symptoms. Additionally, combination medications offer a blend of a short-acting beta agonist and an inhaled corticosteroid in a single inhaler, providing both quick relief and long-term control.
There is a new one called AIRSUPRA®, which has albuterol, a short-acting beta two agonist, and Budesonide, an anti-inflammatory or steroid. Together, they are the first FDA-approved rescue combination medication.
Medication Assistance
- Shop around
- Compare prices at other pharmacies
- Check prices at:
- GoodRx-www.goodrx.com
- Medicine Assistance Tool-www.medicineassistancetool.org
- Needymeds- www.needymeds.org
Medication assistance programs offer valuable support to patients managing asthma by providing resources to compare prices and access discounts at various pharmacies. Platforms like GoodRx and Needymeds offer convenient tools that enable patients to compare medication prices and locate the most affordable options available nearby.
For instance, GoodRx provides a user-friendly website and mobile app where patients can input their location and specific medication to view nearby pharmacies offering the medication at discounted prices. This accessibility empowers patients to make informed decisions about their medication purchases and alleviates financial burdens associated with asthma management.
Asthma Age Groups/Severity Classifications
- Age Groups
- Children up to age 4
- Children aged 5-11
- Children aged 12 or older and adults
- Severity Class
- Intermittent
- Mild Persistent
- Moderate Persistent
- Severe Persistent
When assessing and managing asthma across different age groups, it's essential to consider distinct approaches tailored to specific developmental stages. Age groups commonly used for evaluation and treatment include children up to age four, children aged five to eleven, adolescents aged twelve or older, and adults.
Furthermore, asthma severity is classified into four main categories: intermittent, mild persistent, moderate persistent, and severe persistent. These classifications help guide treatment decisions and the intensity of therapy required to manage asthma effectively.
Despite advancements in asthma treatment and management strategies, asthma rates remain elevated, emphasizing the ongoing need for comprehensive asthma care and continued efforts to improve outcomes for patients of all ages.
Determining Asthma Severity/Control
S.A.L.S.A. is a really helpful tool.
- Symptoms
- Activities
- Lung function
- SABA use
- Awakenings
The "SALSA" acronym provides a comprehensive framework for assessing both asthma control and severity. It stands for Symptoms, Activities, Lung function, SABA use (Short-Acting Beta Agonist), and Awakenings.
In terms of severity, individuals with intermittent asthma typically experience symptoms two days a week or less, have no limitations in activities, exhibit normal lung function, use SABA medication two days per week or less, and may awaken with asthma symptoms no more than two nights per month.
Conversely, severe asthma is characterized by persistent symptoms throughout the day, severe limitations in activities, significantly reduced lung function, frequent SABA use (sometimes required multiple times a day), and awakenings due to asthma symptoms occurring throughout the week.
By utilizing this tool, healthcare providers can efficiently assess asthma severity and control, enabling tailored treatment plans to be developed based on individual needs.
Stepwise Approach for Long-Term Asthma Control
- Six Steps
- Rx tailored to the level of asthma severity or control
- NOT to replace clinical decision-making
- Step UP: After checks on Rx adherence, inhaler technique, environmental factors, and co-morbidities- Reassess 4-6 weeks
- Step DOWN: When asthma controlled for 3 months
- Consult an Asthma Specialist:
- Step 3 or > in 0-4yrs
- Step 4 or > in 5-11yrs and 12-adult
www.nhlbi.nih.gov
The stepwise approach and guidelines for long-term asthma control provide a structured framework for managing asthma effectively. These guidelines outline six steps within each severity category, tailoring medication options to address the needs of patients across different levels of asthma severity.
Starting with the intermittent patient and progressing through mild, moderate, and severe classifications, medication adjustments are made based on the patient's response to treatment and level of asthma control. It's crucial to ensure that patients adhere to their prescribed medication regimen and address factors such as inhaler technique, environmental triggers, and comorbidities that may impact asthma management.
Regular reassessment, ideally every four to six weeks, allows healthcare providers to monitor progress and make necessary adjustments to the treatment plan. When asthma is well-controlled for three months, consideration may be given to stepping down medication dosages.
The guidelines also offer guidance on when to consult an asthma specialist, typically indicated at higher steps of the treatment regimen. Additionally, preferred medications are identified, with alternatives available if the preferred option proves ineffective for a particular patient.
Central to effective asthma management is patient education. Studies emphasize the importance of educating patients about their condition and regularly evaluating their progress to prevent the development of misconceptions and ensure they are empowered to achieve optimal outcomes. By prioritizing patient education and engagement, healthcare providers can support patients in managing their asthma effectively and realizing their full potential in terms of health and well-being.
Essential Patient Teachings
- Teach and reinforce with patients at every opportunity
- Basic Asthma Facts
- Role of inflammation
- What happens to the airways during an asthma attack
- Role of Medications
- Rescue
- Controller
- Proper use of medications and delivery devices
- Monitoring control
Above are the things that we want to teach and reinforce with patients at every opportunity.
Asthma Control
Asthma cannot be cured, but it can be controlled. Many patients are unaware of what asthma control even means and that they can expect to live a normal life if it is well managed.
Role of Inflammation
- Quiet Asthma
- Inflammation & swelling
- Unable to see
- Noisy Asthma
- You can hear the wheezing.
- Coughing, shortness of breath
The role of information inflammation can be seen in Figure 4.
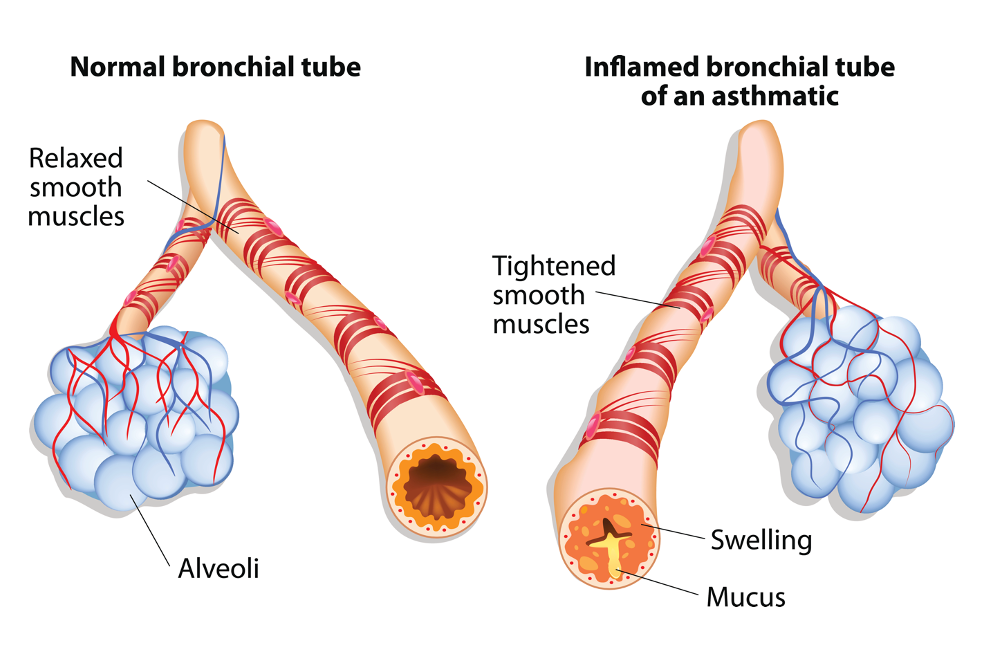
Figure 4. Illustration of a normal versus inflamed bronchial tube. Image: Continued (licensed from Getty Images)
Patients may experience different manifestations of asthma, ranging from "quiet asthma" to "noisy asthma."
Quiet asthma refers to a situation where there's inflammation and swelling in the airways, leading to difficulty breathing, but outwardly, there may be minimal observable signs or symptoms. On the other hand, noisy asthma is characterized by audible wheezing, along with symptoms like coughing and shortness of breath, making the condition more apparent to the individual and those around them. Understanding these distinctions can help patients recognize and manage their asthma more effectively.
Asthma Attack
- In asthma, the airways of the lungs become narrow and obstructed.
- Swelling and increased mucus causes the airway to become rigid and interfere with airflow.
- As the airways become obstructed, it becomes harder to breathe out.
- This causes chest tightness and shortness of breath.
Figure 5 shows what happens during an asthma attack.
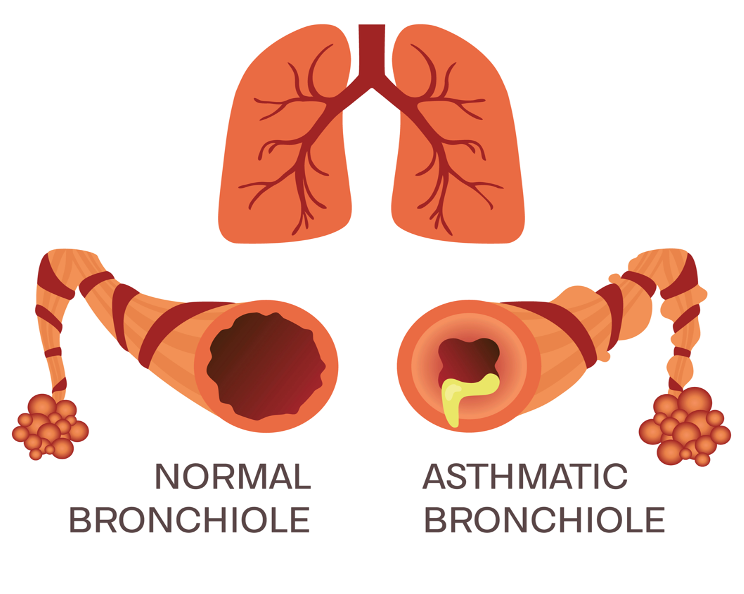
Figure 5. Illustration of an asthma attack. Image: Continued (licensed from Getty Images)
Patients should understand that asthma affects the airways of the lungs, causing them to narrow and become obstructed. Even small airways, sometimes as narrow as a pencil lead, can swell and produce excess mucus, leading to increased rigidity and interference with airflow.
As the airways become obstructed, it becomes increasingly difficult to breathe out, resulting in symptoms such as chest tightness and shortness of breath. This understanding can help patients recognize the underlying mechanisms of their symptoms and better manage their condition.
The Role of Medications
- RESCUE
- Used to reverse asthma symptoms IMMEDIATELY
- Gives QUICK RELIEF
- CONTROLLER
- Used for LONG TERM DAILY CONTROL/MAINTENANCE of persistent asthma
- Steroid (anti-inflammatory) inhalers or pills may be prescribed
Understanding the role of asthma medication is crucial for effective management, yet patients often struggle with when and why to take it.
Rescue medications are designed to provide immediate relief by reversing asthma symptoms and airflow obstruction. They offer quick relief during asthma attacks or exacerbations. In contrast, controller medications are used for long-term daily control to manage persistent asthma, regardless of its severity. These medications, which may include steroids delivered via inhalers or pills, work to reduce inflammation and prevent symptoms from occurring.
To help patients distinguish between rescue and controller medications, visual aids such as graphics depicting a frowny face for rescue inhalers and a yellow smiley face for controller inhalers can be beneficial. This simple representation reinforces the idea that rescue medications are for immediate crisis relief, while controller medications maintain inflammation control over time.
Rescue/Quick Relief Medications
- Relax smooth muscles surrounding the airways
- Albuterol, ProAir, Ventolin, Proventil, Xopenex
- Best as rescue medication
- Effective 3-6 hrs.
- Few side effects
- Albuterol, ProAir, Ventolin, Proventil, Xopenex
Rescue or quick relief medications play a crucial role in relaxing the smooth muscles of the airways during asthma attacks. Examples of these medications include Albuterol, ProAir, and Ventolin. They are primarily used for immediate symptom relief and are best suited for acute situations.
These medications typically provide relief for about three to six hours and generally have few side effects. However, it's worth noting that older medications like Bronchosol, which was used in the past, often cause side effects such as elevated heart rate and jitteriness in patients.
Controller/Maintenance Medications
- Inhaled Corticosteroids (ICS)
- Treat chronic inflammation
- Most effective for persistent asthma
- Side effects are rare
- Pulmicort, QVAR, Fluticasone, ArmonAir Asmanex
- **Rinse mouth after using**
- Treat chronic inflammation
Controller and maintenance medications, such as inhaled corticosteroids, play a vital role in managing chronic inflammation associated with asthma, particularly for persistent cases. Examples of these medications include Pulmicort, Qvar, and fluticasone.
Side effects of inhaled corticosteroids are rare, but it's essential for patients to rinse their mouth after each use to minimize any potential issues. Patients should understand that these medications work gradually, with changes in lung tissue typically noticeable after ten to 14 days and maximum improvement occurring within six to eight weeks.
It can be challenging for patients to grasp the need for long-term use of these medications, as they may prefer instant relief. However, understanding the gradual but significant benefits of inhaled corticosteroids is crucial for maintaining asthma control and preventing future exacerbations.
- Oral Corticosteroids (OCS)
- Treat inflammation
- ONLY for the most severe hard to control persistent asthma due to the risk of side effects
- Prednisolone
- Prednisone
- Often OCS are10 x’s as strong as Inhaled Corticosteroids (ICS)
- Treat inflammation
Oral corticosteroids are another treatment option for managing inflammation in asthma, but they are typically reserved for severe, hard-to-control cases due to the risk of side effects. Examples of oral corticosteroids include Prednisone and Prednisolone.
However, it's important to note that oral corticosteroids can have significant side effects, as experienced by your mother. These side effects may include a swollen or "moon" face, brittle bones, and conditions like osteomyelitis, which involves inflammation of the bones and muscles.
Compared to inhaled corticosteroids, oral corticosteroids are often much stronger, sometimes up to ten times as potent. Due to their potency and potential side effects, oral corticosteroids are typically used sparingly and for short periods under close medical supervision.
Rules of 2
- When would an individual need more than a Quick Relief medication?
- Does an individual take a quick relief inhaler more than 2 times per week?
- Does an individual awaken at night with asthma symptoms more than 2 times per month?
- Is the Quick Relief inhaler refilled more than 2 times per year?
- If the answer to these questions is yes, a Controller (anti-inflammatory) medication may be needed.
The "Rules of Two," a tool trademarked by Baylor Healthcare Systems in 1997, offer valuable insights into assessing the need for additional asthma management beyond a rescue inhaler. By asking three key questions, healthcare providers can determine if an individual may benefit from a controller medication:
Does the individual use a quick-relief inhaler more than two times per week? Does the individual experience nighttime awakenings due to asthma symptoms more than two times per month? Is the rescue inhaler refilled more than two times per year? If the answer is yes to any of these questions, it suggests inadequate asthma control and the potential need for a controller medication, such as an inhaled corticosteroid.
It's crucial to address inflammation effectively because relying solely on quick-relief medication may not adequately control the underlying inflammation. Over time, this can lead to desensitization of receptors and persistent inflammation, which can contribute to lung remodeling and permanent lung damage. Utilizing the "Rules of Two" helps healthcare providers identify individuals who may benefit from additional asthma management strategies to prevent long-term complications.
Essential Asthma Skills
- Skills
- Taking or delivering medications correctly, including inhalers, valved holding chambers (spacers), nebulizers
- Monitoring to assess control Asthma Control Tests and utilization of a written Asthma Action Plan
- Identifying and avoiding asthma triggers
- The greatest benefit is when a written Asthma Action Plan is used.**
To effectively manage asthma, patients need to develop various skills. This includes mastering the correct administration of medications, such as inhalers, nebulizers, and valve-holding chambers. Understanding how to monitor asthma control through tools like asthma control tests is essential for patients to track their symptoms and adjust their treatment accordingly.
Additionally, having a written asthma action plan is crucial. This plan provides clear instructions on what steps to take during different situations, such as asthma attacks or worsening symptoms, ensuring patients know when to adjust their medication or seek medical assistance.
Furthermore, patients should learn to identify and avoid common asthma triggers. By recognizing these triggers and taking proactive measures to avoid them, patients can reduce the likelihood of asthma exacerbations and improve overall control of their condition.
Research indicates that the utilization of a written asthma action plan offers significant benefits in asthma management. By acquiring these skills, patients can play an active role in managing their asthma and achieving better health outcomes.
Metered Dose Inhaler (MDI)
- Use a “spacer” or valved holding chamber delivers medication more effectively and safely
- Sit up or stand
- Shake well
- Exhale completely
- Activate the dose
- Inhale SLOWLY and Deeply
- Hold breath up to 10 secs.
- Wait 1 minute between inhalations
When using a metered-dose inhaler (MDI), employing a spacer or valve-holding chamber significantly enhances the effectiveness and safety of medication delivery. Unlike direct inhalation, where the medication is released turbulently, a spacer or chamber slows down the medication particles upon release. This ensures that the entire dose remains available for inhalation.
To use an MDI effectively, patients should follow these steps: sit up or stand, shake the inhaler well, insert it into the spacer or chamber, exhale completely outside the device, place the device in the mouth or around the face, activate the dose, inhale slowly and deeply, and hold the breath for up to 10 seconds. It's essential to note that patients should wait for about a minute between inhalations if instructed to take more than one dose at a time.
However, individual circumstances may vary. In emergencies, healthcare providers may advise taking doses consecutively. Patients commonly encounter issues with MDIs, such as waiting too long to inhale or inhaling too quickly, which can compromise treatment effectiveness. Mastering the correct technique ensures optimal medication delivery and improves asthma management outcomes.
Dry Powder Inhaler (DPI)
- Sit up or stand
- Load dose of medication
- Activate the dose
- Hold the device level
- Exhale completely
- Put mouth tightly around the mouthpiece
- Inhale QUICKLY and DEEPLY
- Hold breath for 5-10 seconds
- Do not exhale in the device, shake it, or wash it
- **If steroid component rinse mouth**
When using a dry powder inhaler (DPI), patients should follow specific steps to ensure proper medication delivery. Whether sitting or standing, the process begins by loading the dose of medication into the device. This typically involves opening the device, inserting a capsule containing the medication, and then closing it, puncturing the capsule with a tab or caulking mechanism to activate the dose.
Once the dose is loaded and activated, patients should exhale completely outside of the device before inhaling the medication quickly and deeply. It's crucial not to exhale into the device or shake it afterward. Additionally, if the DPI contains a steroid component, rinsing the mouth after inhalation is necessary to prevent thrush.
One common issue with DPIs is inhaling too slowly, which may result in patients not receiving the full dose of medication. To maximize the effectiveness of treatment, patients should aim to inhale quickly and deeply and hold their breath for five to 10 seconds after inhalation. Mastering the correct technique ensures optimal medication delivery and enhances asthma management outcomes.
Delivering a Nebulizer Treatment
- Change's liquid medication into a fine mist
- Sit upright
- Take SLOW, DEEP breaths until the medicine is gone.
- Cough and clear any loosened secretions
- Properly clean and store equipment
- Take apart and rinse after each use
- Soak in vinegar and water once per week and air dry
- Many portable options for nebulizer machines
When using a nebulizer, it's essential to maintain an upright position and take slow, deep breaths until the medicine is fully administered. This doesn't mean every single breath should be slow and deep; rather, patients should intersperse slow, deep breaths with normal breathing throughout the treatment.
Using the nebulizer with a mouthpiece is preferable, as it allows the medication to be delivered directly to the lungs. Patients should observe the disappearance of the medication cloud as they inhale, ensuring effective delivery of the medication.
While using a mask for aerosol treatment is an option, it's not as effective as using a mouthpiece. Patients should cough and clear their secretions as needed during and after the treatment. Additionally, proper cleaning and storage of nebulizer equipment are crucial for maintaining its effectiveness and preventing contamination.
Nebulizers, typically consisting of three or four pieces, can be disassembled for cleaning. After each use, rinsing the components is recommended, and once a week, soaking them in a solution of one part vinegar to three parts water for an hour can help sanitize the equipment. Portable nebulizer options are available, often with good reimbursement from durable medical equipment (DME) companies. These options provide convenience and accessibility for patients needing asthma treatment on the go.
Asthma Action Plan (AAP)
- Key components:
- What medicines to take
- When to take them
- How much to take
- When to get help
- Remember to share the plan!!!
- ***Update every 3-6 months with your healthcare provider ***
The Asthma Action Plan is a vital tool that outlines specific guidelines for managing asthma based on a patient's symptoms or peak flow measurements. It provides clear instructions on which medications to take, when to take them, the appropriate dosage, and when to seek further medical assistance if needed.
Ensuring that the Asthma Action Plan is widely shared and understood is crucial for effective asthma management. In places like public schools, where children spend a significant amount of time, it's essential for teachers and staff to be aware of students' asthma action plans. Previously, my local public school in Lincoln, Nebraska, required parents to provide asthma action plans for their children with asthma, highlighting the importance of communication between healthcare providers, parents, and school personnel.
Additionally, it's crucial to share the Asthma Action Plan with other caregivers, such as grandparents, coaches, and athletic trainers, who may also be responsible for the child's well-being. These plans should be updated regularly, ideally every three to six months, to reflect any changes in the child's asthma symptoms or management strategies. Regular evaluation by healthcare providers ensures that the Asthma Action Plan remains current and effective in addressing the child's evolving needs.
Here's an example of the asthma action plan (Figure 6).
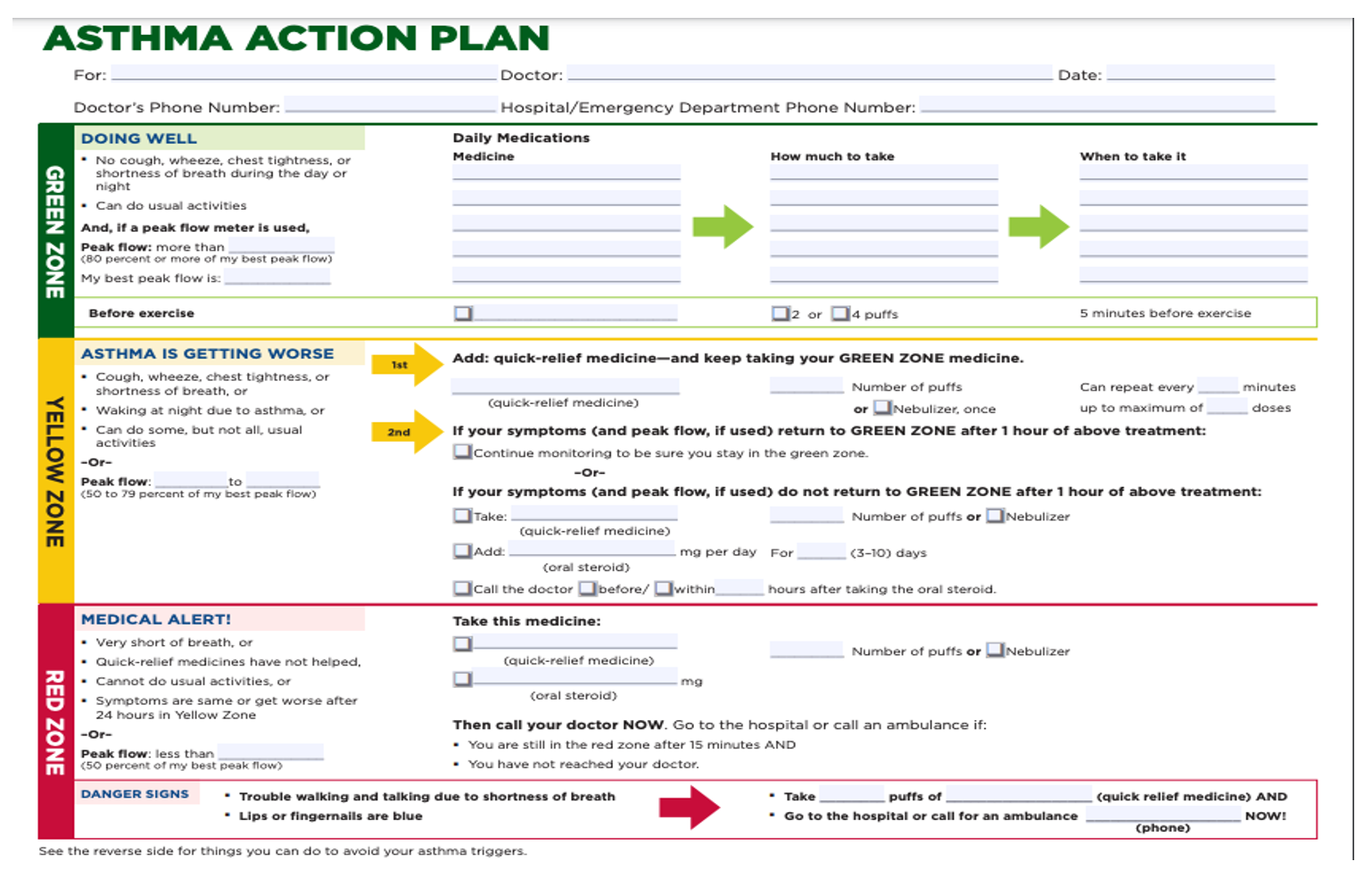
Figure 6. Free download of the Asthma Action Plan.
The Asthma Action Plan provides guidance based on symptoms or peak flow measurements, facilitating effective asthma management. It includes instructions for medication use and environmental modifications to reduce triggers, enhancing patient safety. Occupational therapists play a role in modifying environments for patients' well-being. This plan educates patients about common indoor allergens, empowering them to minimize exposure.
Peak Flow Monitoring
- Measures the amount and velocity of air exhaled from the lungs after a deep breath
Peak flow monitoring is a valuable tool for assessing lung function in asthma management. These devices measure the amount and velocity of air exhaled from the lungs after a deep breath. While peak flow meters may not always be included in the Asthma Action Plan, they can provide crucial insights into asthma control.
There are various types of peak flow meters available, each with its own features. When using a peak flow meter, the maneuver involves taking the deepest breath possible and exhaling forcefully and rapidly to expel all the air from the lungs. This process provides a measurement of peak expiratory flow rate (PEFR), which can help indicate the degree of airway obstruction and the effectiveness of asthma management strategies.
Personal Best Peak Flow
- A key component of the Asthma Action Plan
- Your Personal Best is the highest measurement you can reach during a two-week period when you are feeling your best or FREE of asthma symptoms.
- Take your readings when you wake up and when you go to sleep
- Take additional readings before and after you take your inhaled medications
Your "personal best" peak flow measurement is a crucial component of the Asthma Action Plan. This value is determined by monitoring peak flow readings over a two-week period when the individual is experiencing minimal or no asthma symptoms. During this time, peak flow measurements are taken upon waking and before going to bed, as well as before and after using inhaled medications.
Encouraging patients to consistently monitor their peak flow meter, particularly during periods of symptom-free days, provides valuable data for establishing their personal best reading. This allows healthcare providers to tailor asthma management strategies based on individual needs and fluctuations in lung function over time. Regular monitoring empowers patients to take an active role in managing their asthma and optimizing their respiratory health.
The 3-Zone System
- Green Zone = 80-100% of your ideal number
- Signals All Clear
- Yellow Zone = 50-79% of your ideal number
- Signals Caution- Follow your plan or call your doctor.
- Red Zone = <50% of your ideal number
- Signals Medical Alert- Take your Quick Relief medication and call your doctor
Once the personal best peak flow measurement is established, it serves as a reference point for determining the severity of asthma symptoms and guiding appropriate actions. The Asthma Action Plan typically divides peak flow measurements into three zones based on the percentage of the individual's personal best.
The green zone, representing 80% to 100% of the personal best, indicates that asthma symptoms are well-controlled and no immediate action is needed. The yellow zone, encompassing 50% to 79% of the personal best, signifies caution, prompting individuals to follow the action plan or consult their healthcare provider if symptoms worsen. The red zone, indicating less than 50% of the personal best, signals a medical emergency. Individuals in this zone should promptly take their quick-relief medication and seek urgent medical attention, which may include contacting their doctor or even calling emergency services.
By categorizing peak flow measurements into these zones, the Asthma Action Plan provides personalized guidance for individuals with asthma, regardless of the severity of their condition. Whether someone has intermittent asthma or mild, moderate, or severe persistent asthma, the action plan offers clear instructions tailored to their specific needs, ensuring timely and appropriate management of asthma symptoms.
Early Warning Signs
- Cough, chest hurts, wheezing
- Changes in behavior:
- Unusually tired, not wanting to play, restless, trouble sleeping
- Quick Relief medication causes
- No improvement
- Exposure to know triggers that result in symptoms
Early warning signs of an asthma attack include coughing, chest discomfort, wheezing, and changes in behavior such as unusual tiredness or restlessness. Difficulty sleeping and reluctance to engage in therapy may also be indicators. If rescue medication fails to alleviate symptoms or if the individual has been exposed to a known trigger, it can signal the onset of an asthma attack. Recognizing these warning signs allows for prompt intervention and management to prevent the escalation of symptoms.
Handling An Asthma Attack
- STOP Activity
- Remain calm and reassure
- Don’t leave the individual alone
- Follow Asthma Action Plan
- Administer “RESCUE” inhaler
- (Refer to AAP)
- Look for improvement
- Document
- Watch for late warning signs
During an asthma attack, it's crucial to take immediate action. Firstly, advise the individual to stop the activity and remain calm. Your reassurance can help alleviate anxiety. Never leave the person alone during an asthma attack. Refer to their Asthma Action Plan for guidance. Administer the rescue inhaler if available and monitor for any signs of improvement. It's essential to document the events and watch for any late warning signs. Upper respiratory infections are a common trigger for asthma attacks in children, so being vigilant about symptoms during such times is particularly important.
Late Asthma Warning Signs
- Call 911 if any of the following occur:
- You are not sure what to do
- Blueness of lips or nails
- Unable to walk, talk, or drink
- Struggling to breathe
- Chest and neck muscles working hard (sucking in)
- Breathing does not improve or is worse after the treatment
Late warning signs of an asthma attack warrant immediate medical attention, including calling 911. Look out for blueness of the lips or nails, although in individuals with darker skin tones, this may not be as apparent externally. Check for blueness inside the mouth, on the tongue, and gums, indicating oxygen deprivation. Additionally, observe for blueness in the perineum area. If the person is unable to walk, talk, or drink, or if they exhibit extreme respiratory distress with visible strain on chest and neck muscles, it's imperative to seek emergency assistance. In toddlers and infants, inward chest movement during breathing may indicate severe distress. If breathing fails to improve or worsens after initial treatment, immediate medical intervention is necessary. It's always better to err on the side of caution and seek professional help promptly.
Assessing Asthma Control at Home
- Asthma Control Test 4-11 Years
- An easy tool to help a parent know if their child’s asthma may not be well controlled
- The child answers the first 4 questions
- Parent answers the rest
- No matter what the score share this information with your healthcare provider
Another useful tool for assessing asthma control at home in children aged four to eleven is a simple questionnaire. The child responds to the first four questions by indicating their level of symptoms using smiley faces and frowny faces. Questions inquire about the severity of asthma symptoms and their impact on daily activities and sleep. Parents answer the remaining questions. Regardless of the overall score, it's essential to share this information with the healthcare provider. A total score below 19 suggests inadequate asthma control and warrants further evaluation and management.
- Asthma Control Test 12 yrs. & older
- Easy tool to assess asthma control
- All of the questions are answered by the person with asthma
- No matter what the score, share this information with your healthcare provider
For individuals aged twelve and older, another tool for assessing asthma control includes a set of questions answered by the person with asthma themselves. These questions, available from Glasgow SmithKline, cover aspects such as frequency of shortness of breath, its impact on daily activities, and disturbances during sleep. A total score below 17 suggests potential inadequate asthma control and prompts the need for further evaluation and management.
Asthma Triggers
- Tobacco smoke, wood burning
- Mold and mildew
- Pollutants resulting from poor ventilation
- Pets with fur or feathers
- Cockroach or mouse droppings
- Strong odors (chemicals, cleaning agents, paint, air fresheners, perfumes, dry erase markers, magic markers, glue/paste, fumes from soldering or welding)
- Cold/damp weather
- Exercise
- Extreme emotional expression (stress, anxiety, anger, or crying)
- Prolonged sneezing, yelling, or laughing
- Hormonal
- Common cold, influenza, or other respiratory infections
- Certain foods –peanuts, milk, soy, shellfish, eggs
Remember, always share information about triggers as knowledge is power. Here's a comprehensive list to consider: extreme emotional expressions like anxiety, anger, crying, sneezing, yelling, or laughing can trigger asthma in some individuals. Make sure to review this list when evaluating your client's environment or discussing it with their family.
Keeping Your Environment Asthma Friendly
- This booklet helps you FIND and FIX what can worsen asthma in the Home, at School, and at Play.
- New Resource:
These tools are invaluable resources for managing asthma triggers in various environments. The booklet provided in your handouts offers user-friendly guidance for identifying and addressing asthma triggers at home, school, and during play. It covers a wide range of information, including tips on using natural cleaners and other relevant topics.
Additionally, the new resource called "Exhale" from the Allergy and Asthma Network seems promising. You can find the link to this resource for further exploration.
Pediatric practitioners have recognized the importance of assessing and modifying environments to reduce asthma triggers. This falls well within the scope of occupational practice. Implementing these low-cost interventions, as I've experienced in my work in Nebraska, can significantly improve quality of life by mitigating asthma triggers and improving overall health outcomes.
Goal of Patient Education
- Increase patient’s understanding of asthma and medications
- Improve self-treatment skills
- Enhance patient satisfaction
- Boost patient confidence
- Increase patients' and families' adherence to the treatment program
Ultimately, patient education aims to foster a deep understanding of asthma and its management, including medications. By enhancing self-treatment skills and increasing satisfaction with care, patients can gain confidence and feel empowered to take control of their condition. Understanding asthma triggers and learning effective strategies to alleviate symptoms are key components of this education process.
Moreover, the goal is to improve adherence to treatment regimens. Patients and their families need to grasp the importance of consistent medication use and understand how to administer them properly. Suboptimal adherence can lead to poor disease control, increased mortality rates, and heightened healthcare resource utilization. Through comprehensive education, patients can achieve better outcomes and lead healthier lives.
The Goal of Asthma Management
The goal of asthma management is for individuals to live happy, healthy, physically active lives without asthma symptoms slowing them down.
Anaphylaxis
Let's round this out and talk about anaphylaxis. Anaphylaxis is a sudden, severe, potentially fatal systemic allergic reaction that can involve various areas of the body (Figure 7).
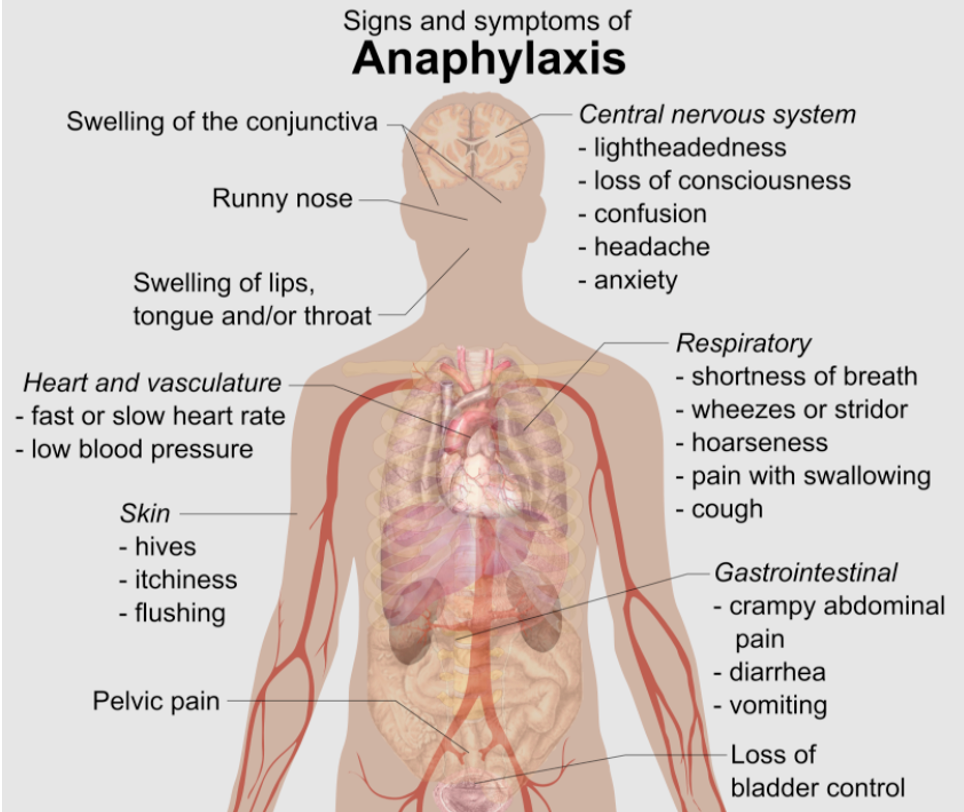
Figure 7. Signs and symptoms of anaphylaxis.
Anaphylaxis is a sudden and severe, potentially fatal, systemic allergic reaction that can involve various parts of the body.
Symptoms
- Skin:
- Itching, redness, swelling
- Mouth:
- Itching, swelling lips, tongue, metallic taste
- Stomach:
- Vomiting, diarrhea, cramping
- Lungs:
- SOB, wheezing coughing, chest pain
- Heart:
- Weak pulse, dizziness, faintness
- Headache
- Nasal congestion
- Watery eyes
- Sweating
- Confusion
- Impending doom
- Loss of consciousness
Anaphylaxis reactions can present with a range of symptoms, and they vary from person to person. Common signs include itching, swelling, and redness of the skin or mouth. Swelling of the lips and tongue, along with a metallic taste in the mouth, are particularly concerning indicators of potential airway obstruction. When these symptoms occur, there's a heightened risk of airflow blockage into the lungs.
Moreover, anaphylaxis can affect multiple organs, including the stomach, lungs, and heart, leading to diverse symptoms. Some individuals may experience a sense of impending doom, akin to an aura preceding a seizure, while others may lose consciousness. These upper airway symptoms and other manifestations require prompt recognition and intervention to prevent serious complications.
Categories
- Food allergies
- Insect/bee/wasp stings
- Latex
- Medications
Anaphylaxis can arise from various triggers, categorized into distinct groups. Food allergies represent a common category, with peanuts, tree nuts, eggs, milk, fish, and soy among the typical culprits. Insect stings, such as those from bees, wasps, fire ants, and spiders, are another prevalent trigger. Additionally, latex exposure, although less common nowadays due to its avoidance in medical settings, can provoke anaphylactic reactions. Medications like penicillin, aspirin, and NSAIDs also have the potential to induce anaphylaxis.
Exercise-induced anaphylaxis is a unique phenomenon where physical activity triggers allergic reactions, sometimes mimicking asthma symptoms. Furthermore, exercise-induced paroxysmal vocal cord dysfunction can escalate into a full-blown anaphylactic episode, emphasizing the diverse nature of triggers that can lead to severe allergic reactions.
Figure 8 shows an example of life-threatening allergies.
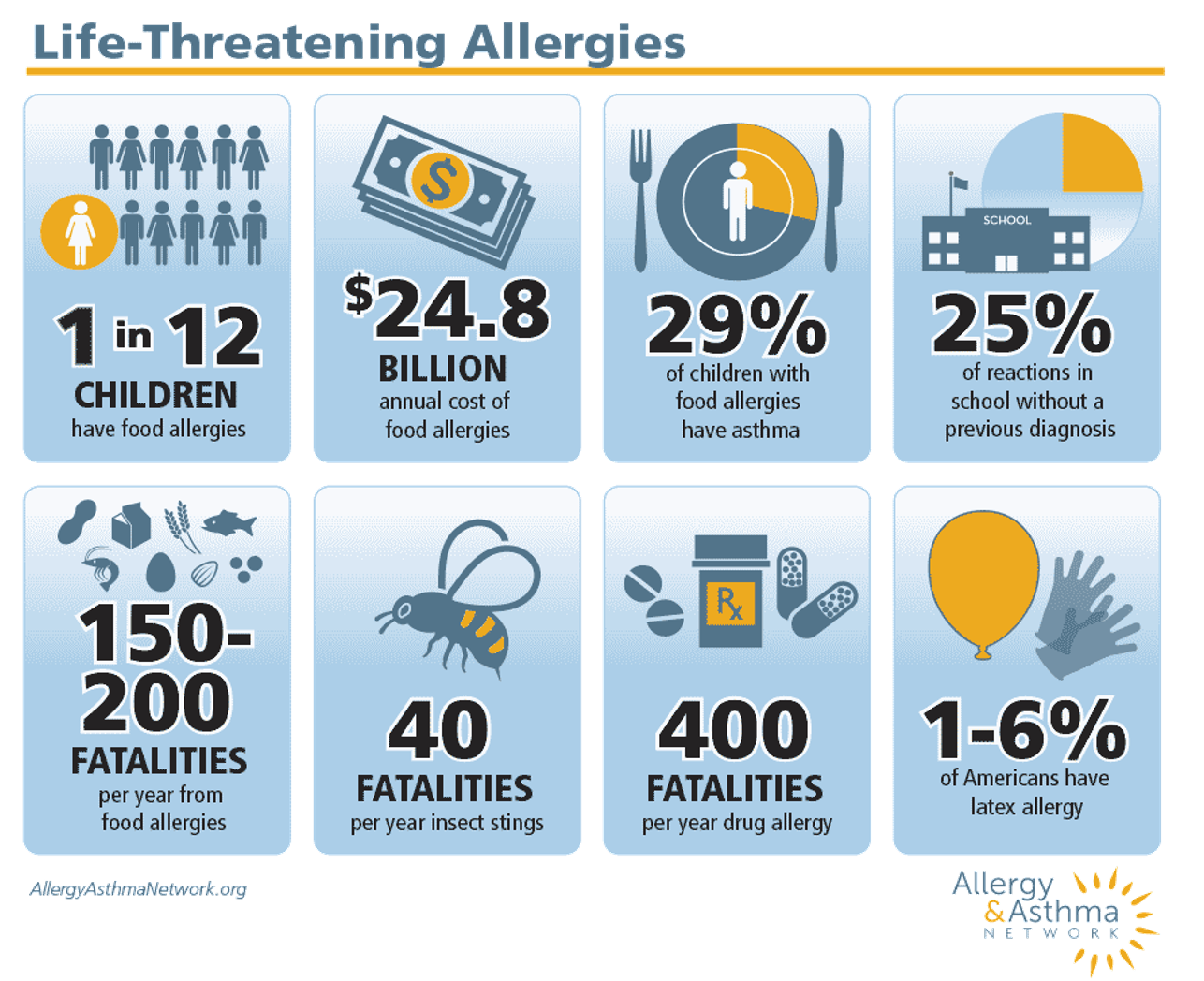
Figure 8. Illustration of life-threatening allergies. Free download from Allergy & Asthma Network.
The prevalence and impact of life-threatening allergies underscore the significance of understanding and managing these conditions effectively. Among children, one in twelve is affected by severe allergies, which can lead to anaphylactic reactions. Notably, 29% of children with food allergies also have asthma, highlighting the interconnectedness of these conditions.
Alarmingly, 25% of anaphylactic reactions occurring in school settings happen without a prior diagnosis, emphasizing the need for heightened awareness and preparedness. Fatalities related to severe allergies are a sobering reality, with 40 deaths attributed to insect stings and a staggering 400 fatalities from drug allergies. Additionally, latex allergies affect a significant portion of the population, with one to six percent of Americans affected by this condition.
Allergy and Anaphylaxis Emergency Plan
Here is an allergy and anaphylaxis emergency plan. It details what medications to take, what to observe, when to take them, and how much to take. This tool is very similar to the asthma action plan in helping individuals know what to do. School teachers, coaches, you know, family members know what to do for this anaphylactic reaction.
Epinephrine/Epi-Pen
- PULL OFF THE SAFETY CAP
- Firmly swing and push tip into the outer thigh
- HOLD in place for 10 seconds
- Massage the injection site for 10 seconds
- SEEK EMERGENCY MEDICAL ATTENTION
- Side effects
- Uncontrolled shaking, twitching, feelings of panic and anxiety
Epinephrine stands alone as a medication with no contraindications for use in severe allergic reactions, making it a crucial tool in managing anaphylaxis. Whether the reaction is mild or severe, administering epinephrine is considered safe and effective, with no risk of harm to the individual. The EpiPen, a well-known brand of epinephrine auto-injector, simplifies the process of delivering this life-saving medication.
To administer epinephrine using an auto-injector, the safety cap is removed, and the device is firmly pressed against the outer thigh. It's essential to hold the injector in place to ensure proper delivery of the medication. After injection, massaging the site helps facilitate the absorption of epinephrine into the muscle tissue. While epinephrine can cause side effects such as shaking, twitching, and feelings of panic or anxiety, seeking medical attention promptly is crucial for further evaluation and management.
Auvi-Q Auto-injector
The Auvi-Q Auto-injector is like an automated external defibrillator. They talk you through what to do exactly. It will give you audio and visual clues. It will count down the five-second hold time in the case of this type of epinephrine auto-injector. And it has a retractable needle that goes back into the device.
Epinephrine First, Epinephrine Fast
- All 50 states guarantee the right to carry and self-administer.
- Most states allow or require schools to stock epi-pens.
All 50 states guarantee the right to carry and self administer this medication when the individual's been checked off to do so. Most states allow or require schools to stock epiphany. You can check your state with this link here to see whether or not your state allows that and has it in their schools at the ready.
Anaphylaxis at a Glance
This is another very nice visual tool that gives examples of allergens, kind of a list of the different allergens. It also shows common symptoms (Figure 9).
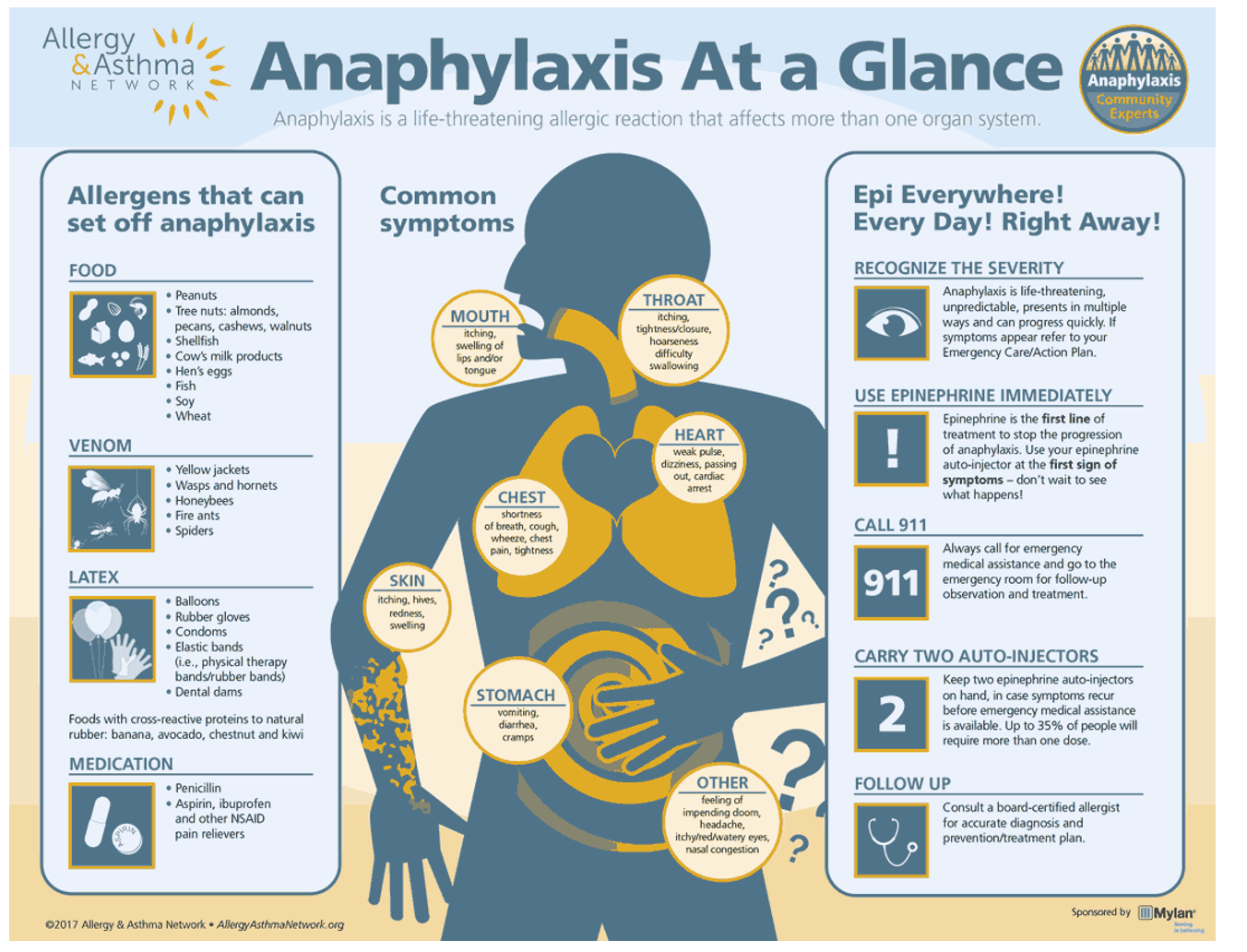
Figure 9. Downloadable handout from the Allergy & Asthma Network.
The motto "epi everywhere, every day, and right away" emphasizes the importance of having access to epinephrine in case of anaphylaxis. It's recommended to carry two epinephrine auto-injectors, as 35% of individuals may require more than one dose during a severe allergic reaction.
Epinephrine auto-injectors, like EpiPens, can be costly, with some inhalers reaching up to $636. However, pharmaceutical companies often offer assistance programs to help reduce the financial burden for patients. Some companies provide inhalers at a capped price of $35, although this may not be available for everyone, such as those on Medicaid or Medicare. Additionally, programs like the Auvi-Q auto-injector offer free options to eligible individuals.
It's essential for patients and their caregivers to explore these pharmaceutical assistance programs to alleviate the cost of necessary medications like inhalers and epinephrine auto-injectors.
Research
- The occupational therapy practitioner can play a role in treating children with chronic respiratory disease (CRD). OTPs and RTs require education; OTPs on chronic respiratory diseases and RTs on the scope of practice of OTPs (Lorenzo & Metz, 2013).
- Providers and families should consider adding an occupational therapy practitioner to their asthma treatment teams to address children’s ability to participate in desired daily activities (Jezioro et al., 2021).
- Having an understanding of asthma management and prevention can open a dialogue with the patient and caregiver and help towards better asthma control (Gruffydd-Jones & Hansen, 2020).
- Knowledge sharing of respiratory disease and patient management skills across disciplines is important in improving patient outcomes (Zamjahn et al., 2018).
- Patients that do not adhere to treatment regimens or know how to properly perform medication delivery leads to lack of symptom control lowering their ability to participate in activities, poorer health outcomes and increased mortality. Increasing awareness by the healthcare team on respiratory disease management can support better patient outcomes (George & Bender, 2019).
Research indicates that occupational therapy (OT) can play a crucial role in treating children with chronic respiratory diseases. However, it's essential for both occupational therapists and respiratory therapists to receive education on chronic respiratory diseases to ensure better care for patients. Occupational therapists should gain more knowledge about chronic respiratory conditions to provide effective care, while respiratory therapists should understand the scope of practice of OT to make appropriate referrals when necessary.
Including occupational therapy practitioners in asthma treatment teams can significantly benefit children's ability to participate in their daily activities. By understanding asthma management and prevention, occupational therapists can engage in meaningful dialogues with patients and caregivers, ensuring better asthma control. Sharing knowledge and patient management skills across disciplines is vital for improving patient outcomes, not only within occupational therapy but also across other therapeutic fields.
Patients who do not adhere to treatment regimens or fail to properly perform their medication delivery may experience a lack of symptom control, reduced ability to participate, and poor health outcomes, leading to increased mortality and decreased quality of life. Therefore, increasing awareness of respiratory disease and management among the healthcare team can support better patient outcomes overall.
Summary
It is my pleasure to have been with you today. I hope this information is helpful to you and your practice.
References
Chogtu, B., Holla, S., Magazine, R., & Kamath, A. (2017). Evaluation of relationship of inhaler technique with asthma control and quality of life. Indian Journal of Pharmacology, 49(1), 110.
Drake, S., Wang, R., Healy, L., Roberts, S. A., Murray, C. S., Simpson, A., & Fowler, S. J. (2021). Diagnosing asthma with and without aerosol-generating procedures. The Journal of Allergy and Clinical Immunology: In Practice, 9(12), 4243-4251.
George, M., & Bender, B. (2019). New insights to improve treatment adherence in asthma and COPD. Patient Preference and Adherence, 13, 1325.
Gruffydd-Jones, K., & Hansen, K. (2020). Working for better asthma control: How can we improve the dialogue between patients and healthcare professionals? Advances in Therapy, 37(1-9).
Jezioro, J. R., Gutman, S. A., Lovinsky-Desir, S., Rauh, V., Perera, F. P., & Miller, R. L. (2021). A comparison of activity participation between children with and without asthma. The Open Journal of Occupational Therapy, 9(3).
Kaplan, A., & Price, D. (2020). Treatment adherence in adolescents with asthma. Journal of Asthma and Allergy, 13, 39.
Konstantinopoulou, S., & Tapia, I. E. (2019). Sleep-related disturbances commonly associated with asthma. In Allergy and Sleep (pp. 153-161). Springer, Cham.
Lorenzo, R. F., & Metz, A. E. (2013). Occupational therapy practitioners’ knowledge and perceptions of childhood asthma and cystic fibrosis. Occupational Therapy in Health Care, 27(3), 256-270.
Papi, A., Blasi, F., Canonica, G. W., Morandi, L., Richeldi, L., & Rossi, A. (2020). Treatment strategies for asthma: Reshaping the concept of asthma management. Allergy, Asthma & Clinical Immunology, 16, 1-11.
Rickards, T., & Kitts, E. (2018). The roles, they are a changing: Respiratory therapists as part of the multidisciplinary, community, primary health care team. Canadian Journal of Respiratory Therapy, 54(4), 10.29390/cjrt-2018-024. doi: 10.29390/cjrt-2018-024
Unni, E., Gabriel, S., & Ariely, R. (2018). A review of the use and effectiveness of digital health technologies in patients with asthma. Annals of Allergy, Asthma & Immunology, 121(6), 680-691.
Zamjahn, J. B., Beyer, E. O., Alig, K. L., Mercante, D. E., Carter, K. L., & Gunaldo, T. P. (2018). Increasing awareness of the roles, knowledge, and skills of respiratory therapists through an interprofessional education experience. Respiratory Care, 63(5), 510-518.
Resources
- Allergy & Asthma Network:
- American Association for Respiratory Care:
- Centers for Disease Control and Prevention:
- American College of asthma, allergies and immunology:
- U.S. Department of Health and Human Services:
- National Center for Biotechnology Information:
- Asthma Control Tests:
- GoodRx:
- Medicine Assistance Tool:
- Needymeds:
Citation
Nathenson, N. (2024). Understanding asthma and anaphylaxis in the occupational therapy setting. OccupationalTherapy.com, Article 5703. Available at www.occupationaltherapy.com
