Primitive Reflex Overview
- Definition: adaptive responses that develop during the neonatal period and integrate over time as the brain matures
- These reflexes are automatic movements that are controlled by the brainstem and require no conscious thought (cortical involvement)
- These reflexes are present for survival and development in the early months of life.
- One of the most common tools used by physicians and therapists to assess the integrity of the central nervous system in infants and children (Zafeiriou, 2004)
- Causes of retained reflexes: Cesarean section, trauma, exposure to toxins, anesthetics, medications
- Other possible causes: decreased tummy time in infancy, short period or lack of crawling, walking early, chronic ear infections, head injuries
- Primitive Reflexes
- Moro Reflex
- Rooting Reflex
- Palmar Grasp
- ATNR
Primitive reflexes are adaptive responses that develop during the neonatal period that integrate over time as the brain matures. These are automatic movements and are controlled by the brainstem, meaning there is no cortical involvement. They are present for survival and development in the early months of life. Physicians and therapists commonly use these to assess the integrity of the central nervous system.
We see the retention of these primitive reflexes based on the birth method, like Caesarean section versus vaginal delivery, trauma, exposure to toxins, anesthetics, and medications. Obviously, all of these things do not result in retained reflexes, but they are possible causes.
Additionally, other possible causes for retained primitive reflexes are decreased tummy time in infancy, a lack of crawling, early walking, head injuries, or chronic ear infections. In the OT world, we are always looking at decreased tummy time and that lack of crawling during our intakes and assessments. Often, we ask families about when the child started crawling, how long they crawled, and when they started walking. When we see the motor and sensory deficits, crawling (time, quality) can be a good indicator of that.
What The Research Is Saying
- One study’s findings showed that children with retained reflexes had scores associated with sensory discrepancies like sensory-vestibular disorders, dyspraxia, and postural disorders (Pecuch et al., 2020).
- One study discussed how a 12-week program significantly reduced the presence of retained primitive reflexes and improved performance on motor and cognitive testing measures (Melillo et al., 2020).
- Another article showed that integrating retained reflexes positively benefited psychomotor development in preschool children (Gieysztor et al., 2018).
- Overall, there is limited empirical research about integrating reflexes; however, there is adequate research on primitive reflexes and the presence and impact of retention.
- Research and AOTA through the Choosing Wisely Campaign (Frauwirth et al., 2019) are promoting the awareness and understanding of primitive reflexes and strategies that can help children with ADL participation who show signs of retention, rather than therapeutic intentions that “integrate retained reflexes.”
Today, we are going to talk about the eight primitive reflexes. To get a better understanding of all of this, before we dive into each one, I wanted to talk some about what the research is saying. Multiple studies show that children who have retained reflexes have discrepancies in sensory development, postural disorders, decreased motor/cognitive performance, and decreased psychomotor development. And, we do have a good amount of evidence-based research about primitive reflexes and what they look like if they are retained. Where this topic gets a little more controversial and complicated is when we talk about integrating those reflexes. There is limited empirical research on integration. AOTA is launching a campaign called Choosing Wisely. What we are talking about is part of that. As a profession, we know that primitive reflexes are important. A lot of research shows what they look like when they are not integrated and retained. We want to work on primitive reflexes as a therapeutic modality to support the child's participation in ADLs rather than an integration of those. What I am going to talk about today is not a cure per se, but rather these techniques can be used as a part of treatment, along with other modalities, to help support increased independence and participation in ADLs.
How To Use Information About Primitive Reflexes in Practice
- Another tool in your toolbox for assessment and intervention
- Incorporate into movement breaks, home programs, and sensory activities
- Incorporate into evaluation screenings and progress monitoring
- Understand how primitive reflexes may impact the sensory system and utilize this knowledge to tailor a treatment that supports those sensory needs
Information about primitive reflexes can be another tool in your toolbox. I like to include this in assessment and intervention, and it helps me understand why a child might be presenting a certain way. Often, you will see retained reflexes in children on the autism spectrum and with different attention disorders. Instead of making a treatment plan or writing goals specifically working on certain movement patterns, we will use that information to help us be skilled and purposeful with what we are doing during movement breaks, sensory activities, home programs, and sensory diets. If we see that a certain reflex is retained, we can use certain exercises/activities (that we will talk about today) and incorporate that into what we are doing more broadly. Again, we know that there is a relationship between sensory and motor development and the retention of reflexes.
Figure 1 shows an overview of all primitive reflexes.
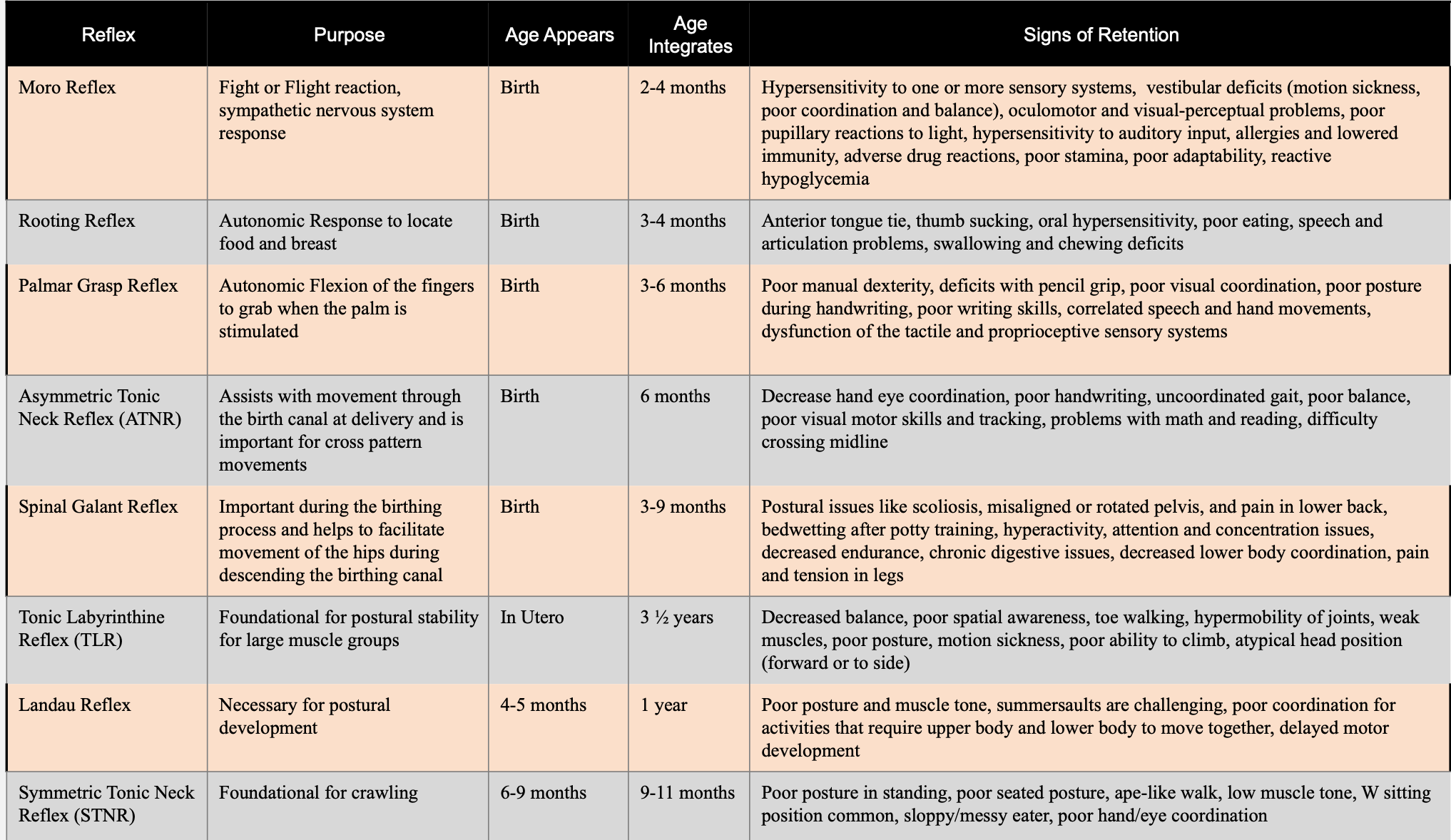
Figure 1. Chart of primitive reflexes.
This is something that I have on the wall in my office. I also have it in my assessment binder. This might be worth having to print out. My email is at the end of this talk. If you cannot print this, I would be happy to send you a PDF out of it. This is a generic overview of each reflex, their purpose, when they typically appear, when they typically integrate, and then things that we would see in a child's presentation that would give us reason to believe that they are not integrated. You can see that signs of retention could be correlated to a lot of other things. This is why we will use reflexes and exercises as part of the bigger picture and not a single solution.
As a side note, if you do not have a lot of experience with early intervention (zero to one-year-old population), I would highly recommend Googling and looking at the typical presentation of reflexes. It is really a lot easier if you see what is typical to then identify atypical. It helps you to understand what you are seeing.
Moro Reflex
Overview
- “Startle Reflex”
- Fight or Flight Reaction
- Common Diagnoses: ADD, ADHD, Autism Spectrum Disorder
- Common Health Problems: Allergies, Asthma, Adrenal Fatigue
- Signs of Retention/Impact on ADLs:
- Hypersensitivity to one or more sensory systems
- Vestibular deficits (motion sickness, poor coordination, and balance)
- Oculomotor and visual-perceptual problems
- Poor pupillary reactions to light
- Hypersensitivity to auditory input
- Adverse drug reactions
- Poor stamina
- Poor adaptability
This is the startle reflex. We will start with the Moro reflex in Figure 2.
Figure 2. Moro reflex.
This is going to be induced by sound, movement, or anything that startles them. In infancy, this is typically a huge movement. It is a big opening of the arms and then bringing them into the body in response to that stimulus. It is a fight-or-flight response and part of the sympathetic nervous system.
It appears at birth, and it is typically integrated by four months of age. There are some common diagnoses and health problems where we see signs of retention impacting ADLs. We may also see a lot of hypersensitivity, poor attention, poor adaptability, impulsivity, and adverse reaction to drugs.
Moro Reflex: Testing For Retention
- Have the child seated in a chair or laying down on their back, instruct them to open their arms and legs like a star, and then bring them and cross them. You can demonstrate this for the child or show them pictures.
- Typically children will cross their arms and legs opposite (arms-right over left, legs-left over right). This is normal.
When testing in the clinic, you would have the child seated either in a chair or laying down on their back on a mat. If they are lying down, we should have a pillow or something underneath their back so that they can have good head extension. This is an example in Figure 3.

Figure 3. Testing for retention of the Moro reflex.
You will just instruct them to open their arms and legs up, like a star, and then bring them together. With all of these, you can demonstrate the movement for the child or show them a picture. They also do not have to be able to understand the verbal directions.
Typically, a child will cross their arms and legs in the opposite manner. You can see this in the second picture. His right arm is on top, while his left leg is on top. You will have them go into a starfish position, and first, cross their right arm on top. Then, you will have them do the same thing on the left side of the body. If age or cognitive ability limits them (e.g., knowing right from left), you can put a sticker on their hand to cue them. Knowing their right and left sides are not part of the testing. If a child has difficulty doing the same side of the body on top for both arm and leg, this will indicate that the reflex is possibly retained.
Exercises for Retained Moro Reflex
This is one of the exercises that can be used to help with that reflex in Figure 4.
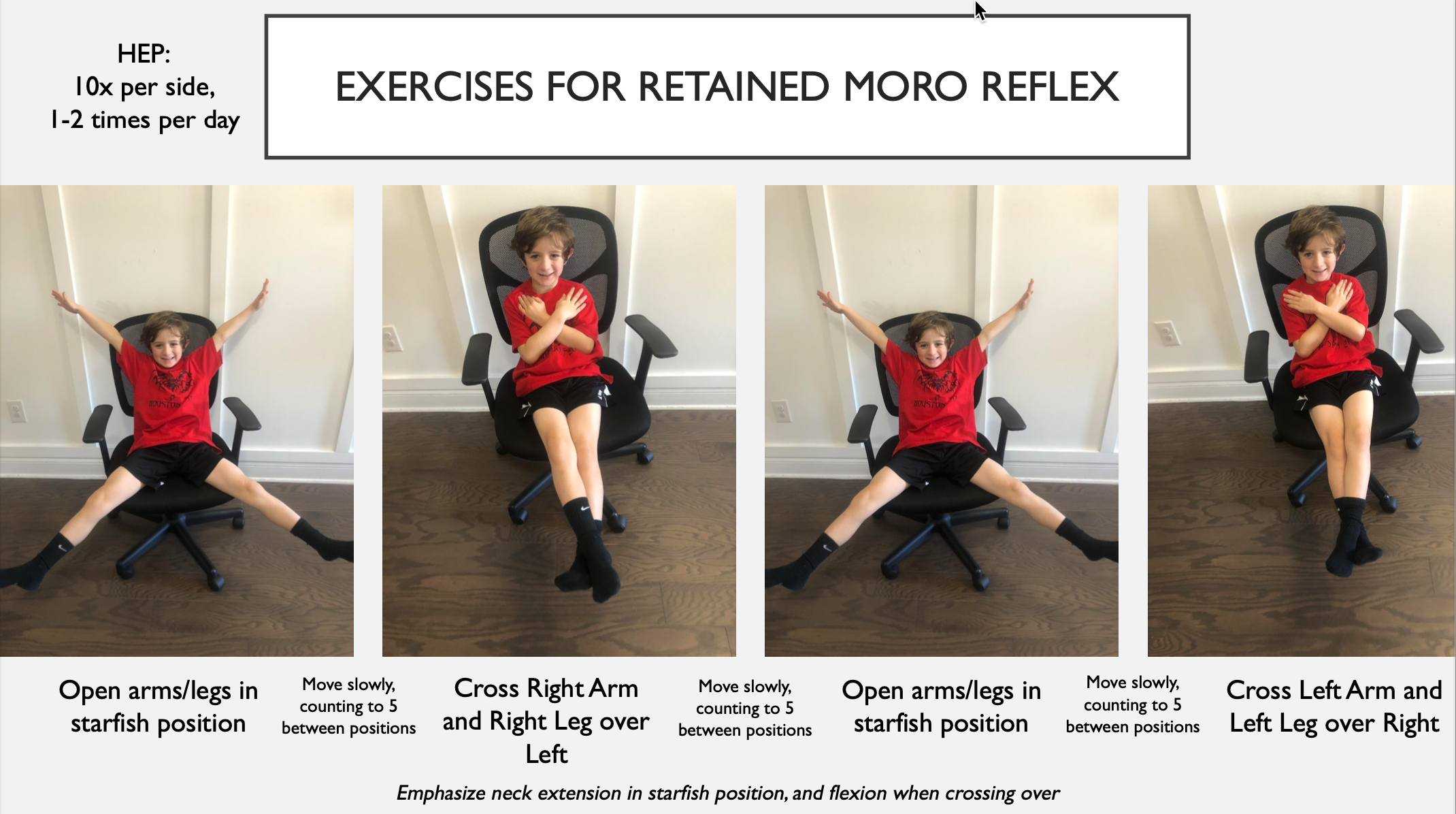
Figure 4. Exercises for a retained Moro reflex.
Many exercises work in similar patterns to the testing as we are trying to perfect that movement. This will help with the dissociation that they do not have yet. Also, on each slide, you will see a mention of the home program, as this one has at the top. We will go over that at the end. This is just there for your reference.
You will have them open up into the starfish position with their arms and legs extended out. We want them to do this slowly. We want slow, purposeful movements so that they have control. Then, they are going to extend out and cross over with the right arm and leg on top. They will repeat that with the left extremities on top.
One thing to know (that is not pictured here) is to use a chair with a lower neck rest or position them supine on a mat with a pillow underneath their back for good neck extension. Additionally, as they are coming in to cross their arms/legs, we want them to bring their chin into flexion.
Rooting Reflex
Overview
- Automatic response to locate food or breast
- Common Diagnoses/Health Issues: deficits with speech, writing, eating, thyroid issues, autoimmune disease/disorders, hormone imbalance
- Signs of Retention/Impact on ADLs :
- Anterior tongue-tie
- Thumb sucking
- Oral hypersensitivity
- Poor eating
- Speech and articulation problems
- Swallowing and chewing deficits
- Dribbling
This reflex is a response to finding a bottle or breast to get food. It is very easy to observe in a typically developing infant. Retention of this reflex impacts ADLs like feeding, speech, and swallowing. Signs of retention include an anterior tongue-tie, thumb-sucking, a lot of hypersensitivity in the oral cavity, feeding discrepancies, and speech problems.
Rooting Reflex: Testing for Retention
- Stroke from nose to chin around corner of mouth, x3 times on each side of the child’s face. Move strokes slightly lateral each time. Repeat on each side of the face.
- Observe for twitch/movement at mouth and same-sided hand. If movement is observed, exercises are needed to integrate reflex.
I am a feeding therapist. I often test this on children that have feeding issues. It is another tool in your toolkit if you are working on those types of skills.
In Figure 5, you can see the little marks on his face.

Figure 5. Testing for retention of the Rooting reflex.
For testing, you take your finger or the eraser end of a pencil and swipe by the child's mouth. You will go from the nose down to the chin, and you are going to start closest to the mouth and move outward each time. You will make each stroke and then move laterally. You want to give some light pressure so that it does not tickle. You do this on each side of the mouth.
We are looking for a twitch or movement at the mouth. We also want to see if their hands twitch on the same side of their body. Both of these would be a sign that the reflex might not be integrated. If you are doing this with a really young child, someone still in the first year, they might demonstrate more of a head turn. It is unlikely that they will have a full head turn as this reflex is typically integrated at three to four months. If you see the twitch of the face or hand, we do two exercises for this.
Exercises for Retained Rooting Reflex
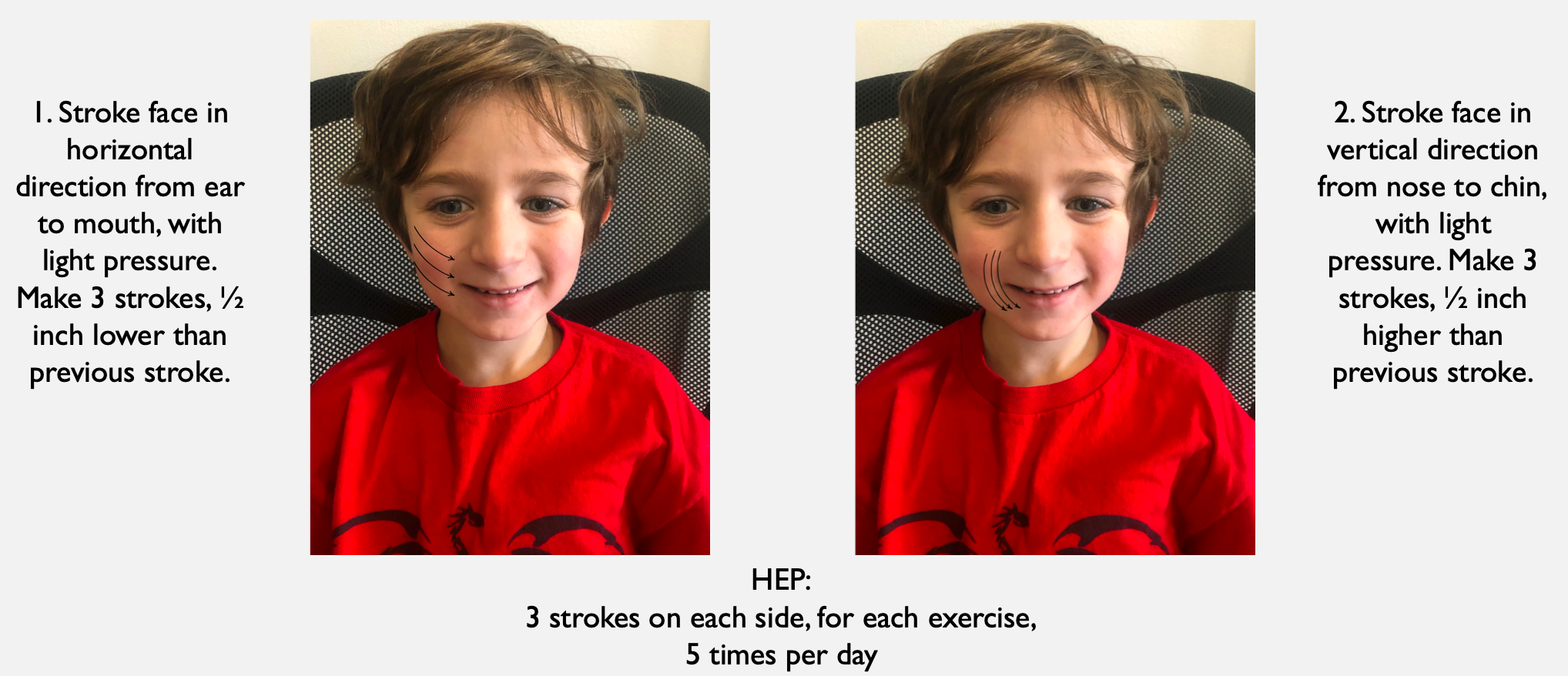
Figure 6. Exercises for a retained Rooting reflex.
You are going to start closer to the ear and stroke horizontally towards the mouth. For this, you start higher. You do this for three strokes. This is essentially the same thing we did for testing, but you will do it purposefully as part of the exercise. This is providing input to integrate and decrease that automatic response. You do that on both sides of the face. You also do vertical strokes, as demonstrated.
Palmar Grasp Reflex
Overview
- Autonomic Flexion of the fingers to grab when the palm is stimulated
- Common Diagnoses: dysgraphia, speech and language problems
- Signs of Retention/Impact on ADLs :
- Poor manual dexterity
- Deficits with pencil grip
- Poor visual coordination
- Poor posture during handwriting
- Poor writing skills
- Correlated speech and hand movements
- Dysfunction of the tactile and proprioceptive sensory systems
This next reflex is the Palmar Grasp. This is very easy to see in infancy.
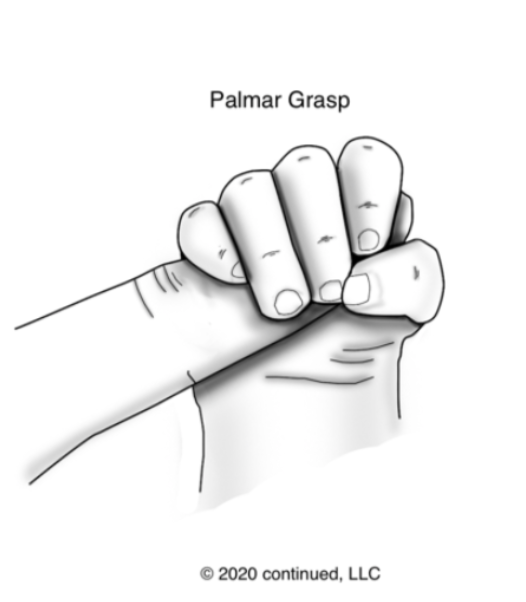
Figure 7. Palmar Grasp reflex.
This is why when a young child is playing, and they grab something, they are unable to drop it on purpose. They do not have that voluntary release yet, and the reflex is still present. This is when the palm is stimulated, and the hand closes. This is present at birth and typically integrates between three and six months old.
Signs of retention may include poor manual dexterity, difficulty with pencil grip, visual coordination, posture during handwriting, handwriting skills in general, correlated speech and hand movements, and tactile and proprioceptive sensory system dysfunction.
Palmar Grasp Reflex: Testing for Retention
- Have the child hold their hand out with palm up and open flat, stroke along the life line crease in the hand, towards the middle of the wrist. Repeat this stroke 3-5 times. Observe for finger twitches or the elbow to twitch or slightly bend. If these observations occur, integration exercises are needed.
As I said, you can use the eraser of a pencil. In Figure 8, it looks like the child's hand is up.

Figure 8. Testing for Palmar Grasp reflex
However, I would have the child's hand out and extended flat with their arm straight in front of them. You will take an eraser tip and create an arching motion from the web space down to the middle of the wrist using the "life line" as a guide. This is done about three to five times. You need to use firm but hard pressure. We are looking for twitching of the fingers and at the elbow and bending of the elbow to show that this reflex might not be integrated.
With all of these, it is appropriate to tell the child what you are doing. "I'm going to put my pencil on your hands and move it down towards your wrist. I want you to keep your hand and your arm still." It is fine to give them those cues. Remember, these are automatic responses. They are not going to be able to control them if they are not integrated.
Exercises for a Retained Palmar Grasp Reflex
One of the exercises we can do for this is using a resistance ball, Play-Doh, resistive putty, or whatever you have (Figure 9).
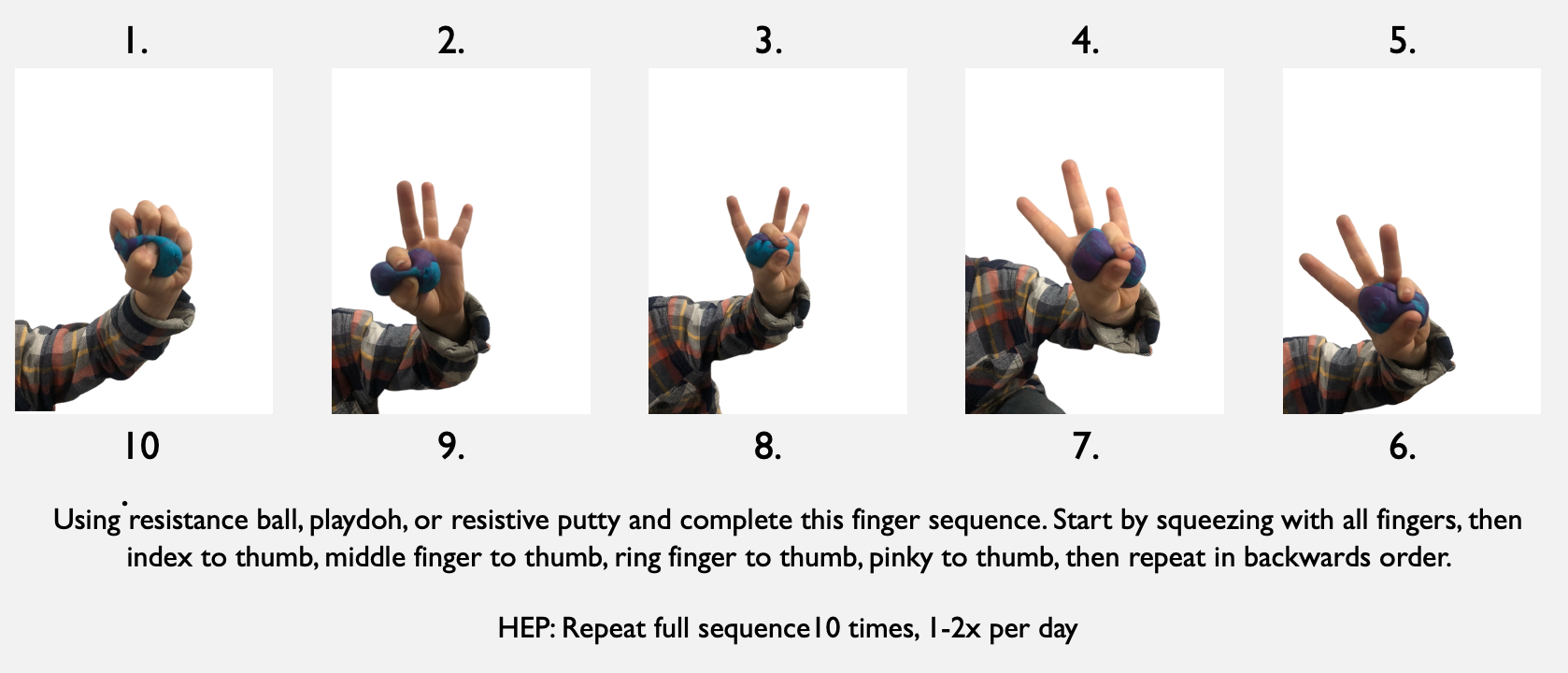
Figure 9. Exercises for a retained Palmar Grasp reflex.
You want to use something with a little bit of resistance that they can squeeze. Obviously, you also need to take into account their sensory discrepancies. If Play-Doh or something like that is going to be too hard, resistance balls can be used as they are not as large of a sensory ask. You are going to ask them to go through a grasp pattern. First is a full fist. They are going to pinch with their index finger, middle finger, ring finger, and pinky. Then, they go back in the other direction. This is a total of 10 different movements in this sequence for one repetition. You want them to do that for 10 repetitions. By putting a ball, Play-Doh, or putty in their hand, we provide that input and have them actively move their fingers to dissociate the fingers' movement from the stimulation on the palm. We are trying to dissociate those movement connections that are currently still paired.
Asymmetric Tonic Neck Reflex (ATNR)
Overview
- “Fencer’s reflex”
- Assists with movement through the birth canal at delivery and is important for cross pattern movements
- Signs of Retention/Impact on ADLs:
- Decreased hand-eye coordination
- Poor handwriting
- Uncoordinated gait
- Poor balance
- Poor visual-motor skills and tracking
- Problems with math and reading
- Difficulty crossing midline
The Asymmetric Tonic Neck Reflex, more commonly called the ATNR. This is the fencer pose position (Figure 10).

Figure 10. Asymmetric Tonic Neck Reflex.
The purpose of this is to help with movement through the birth canal. It is also purposeful for a cross-pattern movement like crossing midline and bilateral integration activities. We typically see this until about six months of age, and then it should be integrated at that point.
Some of the signs of retention and how retention will impact ADLs would be decreased hand-eye coordination, poor handwriting, uncoordinated gait, poor balance, difficulty with visual-motor skills and tracking, problems with math and reading, and difficulty crossing midline.
ATNR Reflex: Test #1 for Retention
- With the child in standing, have them put their arms out straight. Have the child maintain this position while turning head right to left. Observe for elbow bending or shoulder turning in the same direction of the head. If the child is able to move the head without any arm/elbow/shoulder movement, the reflex is likely integrated. If the arm/shoulder/elbow move with the neck motion, it is likely retained.
To test for this, there are a couple of different ways. Example one is in Figure 11.
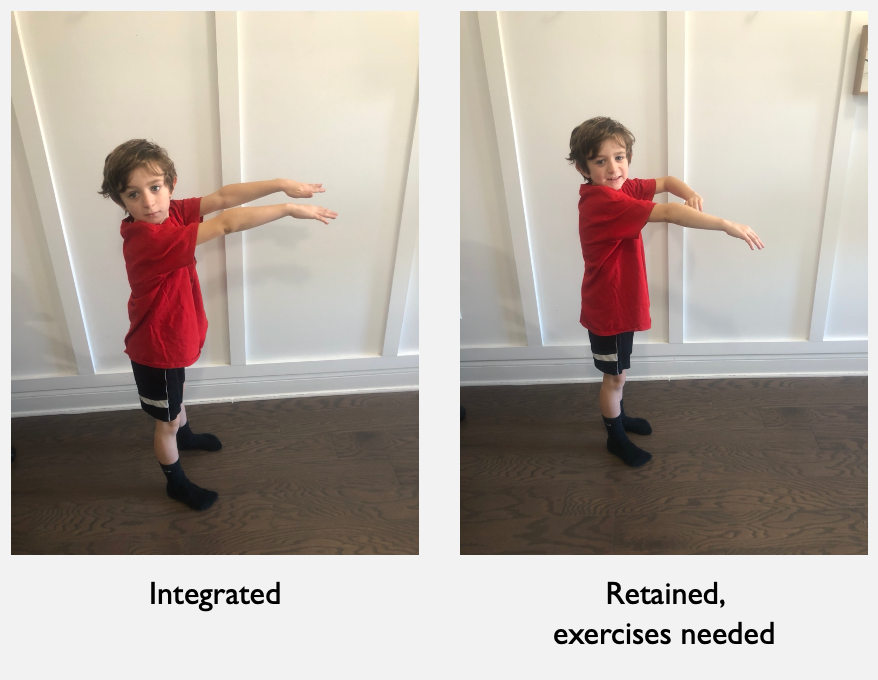
Figure 11. Testing for the ATNR in standing.
One test is to have the child standing up with their arms straight in front of them. You will have them start with their face facing forward in the same direction as their arms. Then, you will have the child turn their head from left to right in a slow pattern. This movement does not need to be quick. You need to instruct them to keep their arms straight. We are looking for the child's ability to keep their arms straight while turning their head. If this reflex is still retained, they will not have the ability to have those two movements broken up. They are still having some relationship of their neck to shoulder movement. If the child is noted to bend one of their arms during turning, then that is a sign that the reflex could be retained.
ATNR Reflex: Test #2 for Retention
- Have the child get in quadruped with their head facing forward. Ask them to turn their head from right to left (side to side) while keeping their neck and arms straight. While they turn their head, observe for bending at the elbows or shifting of the body from side to side. If these movements are present, the reflex is likely retained due to neck and shoulder movements continuing to be connected and not yet independent of each other.
Another way you can test is in quadruped (Figure 12). This is a very similar principle.
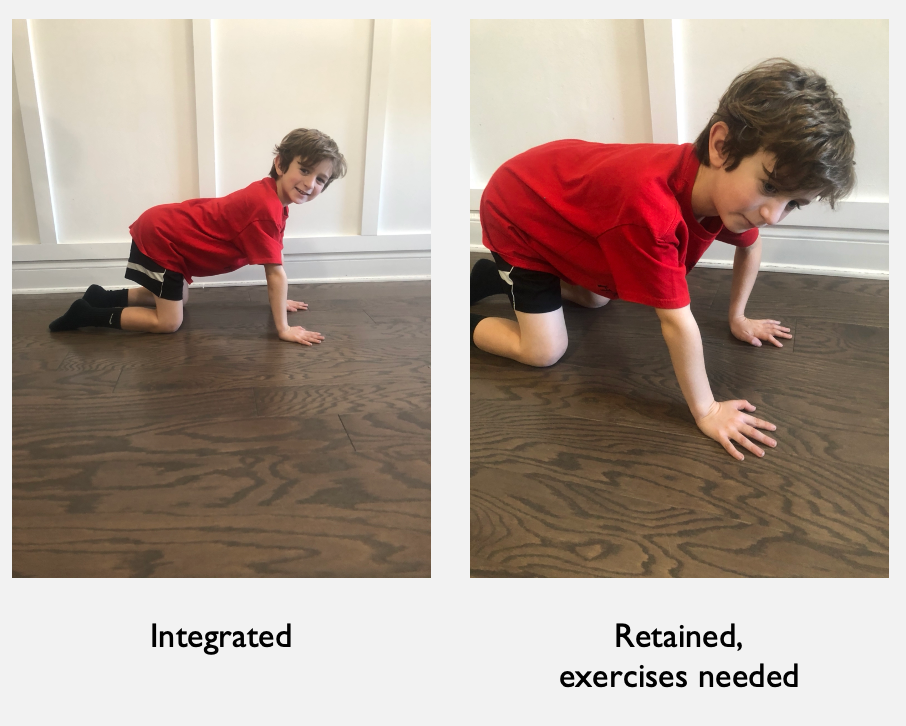
Figure 12. Testing for the ATNR in quadruped.
You have them assume quadruped with a neutral spine, initially with them facing forward. This is where their head faces forward with a neutral neck. We then have them turn their neck to the right and the left. We want them to see if they can stay in this stable quadruped position. If you observe any bending of the elbows or swaying of the body from side to side (like weight shifting) with the movement of the head, these are signs of possible retention for the ATNR reflex.
Exercise #1 for a Retained ATNR
Figure 13 shows the exercise pattern for children that show signs of retention.
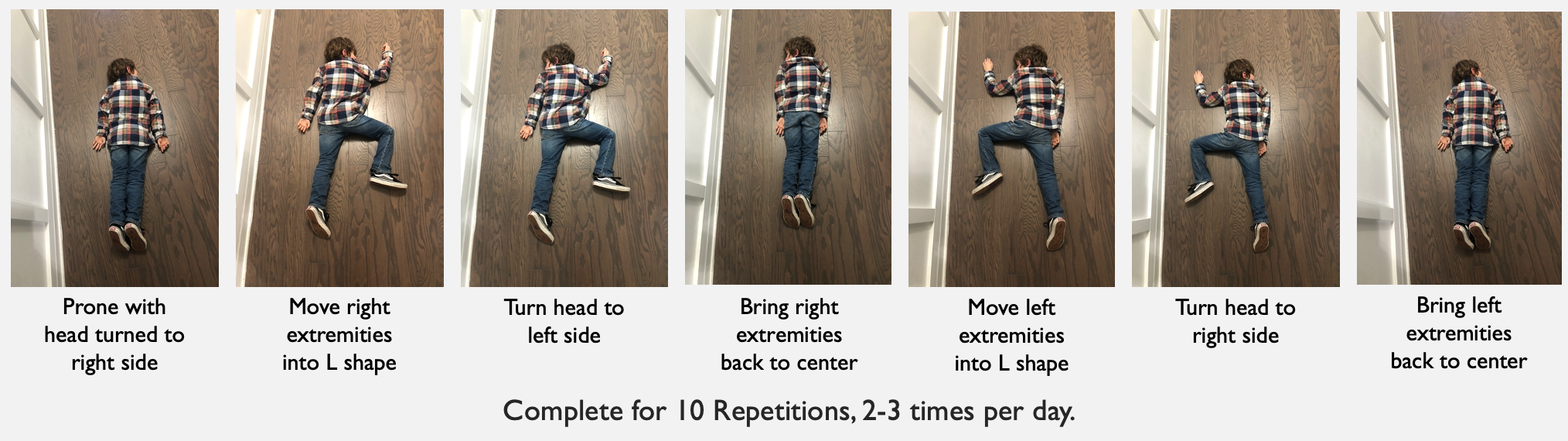
Figure 13. Exercise for a retained ATNR in prone.
You would start with the child in prone with their head turned to the right. They would then move their right extremities into an L position. In this position, they move their head to the opposite side. Then, they would go back to the center. They then make the same L position on the left side, and then they will turn their head to the right and move their arms down and back to midline. We are trying to break up that response and control the ability to integrate that reflex automatically with the motion of the head and arm.
Exercise #2 for a Retained ATNR
- Have the child stand with arms straight out, palms down. Instruct the child to turn their head to one side and run in place, bringing knees high for 10 seconds, and then left head to left for 10 seconds in a continuous motion. Complete 3 times on each side.
- If necessary, support them at the elbows, so there is no bending.
- HEP: Complete 3 repetitions, 1-3 times per day.
Figure 14 shows another exercise for a retained ATNR.
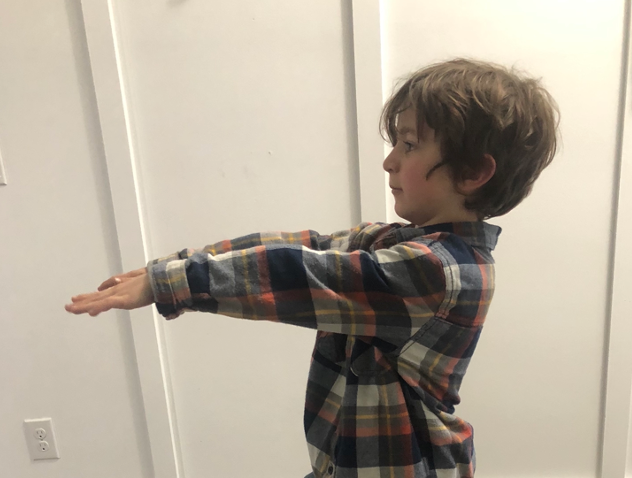
Figure 14. Exercise for a retained ATNR in standing.
Another way you can work on exercises for ATNR retention is to have the child stand up with their arms straight out with their palms down. You will have them turn their head to one side and run in place, trying to bring their knees up high. This is similar to the L position of the knees in the previous exercise. You will have them do this with their head turned to one side. They will run in place with high knees for a count of 10. Then without stopping, they will turn to the other side and continue to run in place for a count of 10. Have them repeat this three times on both sides.
Spinal Galant Reflex
Overview
- Tested in newborns to assist with ruling out brain damage
- If stimulated on both sides of the spine while present, it will educe urination
- Signs of retention/Impact on ADLs:
- Postural issues like scoliosis, misaligned or rotated pelvis
- Pain in the lower back
- Bedwetting after potty training
- Hyperactivity
- Attention and concentration issues
- Decreased endurance
- Chronic digestive issues
- Decreased lower body coordination
- Pain and tension in legs
Our next reflex is called the Spinal Galant in Figure 15.
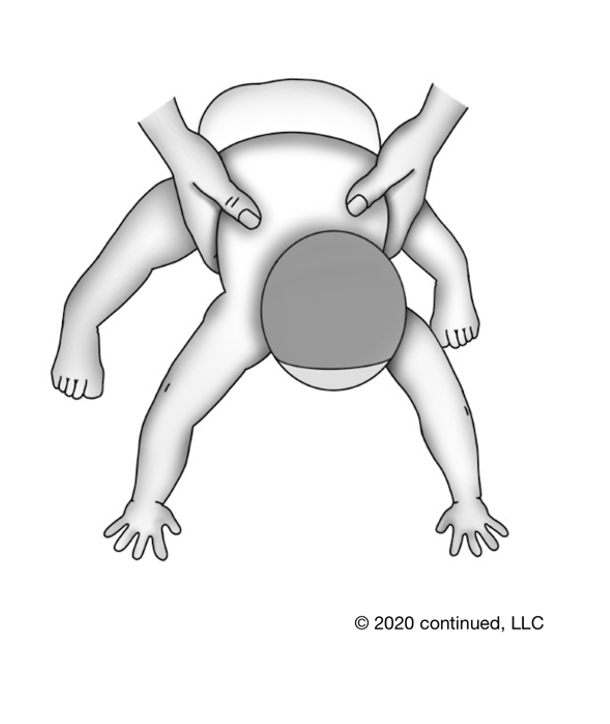
Figure 15. Spinal Galant reflex.
This is tested in newborns and one way that doctors test to rule out brain damage during the birthing process. It is important to note that when you test this, you will apply pressure down the spine. If this reflex is not integrated and you apply pressure down both sides of the spine simultaneously, it can elicit urination. So, we do not do that in testing.
Retention can impact ADLs like bedwetting or potty training. There can also be issues like scoliosis and a malaligned or rotated pelvis. You can visually observe this in some children. Children can also display hyperactivity, attention and concentration issues, decreased endurance, chronic digestive issues, making sense with that misalignment, decreased lower body coordination, and even pain and tension in the legs. This reflex is present at birth and typically integrated by three to nine months.
Spinal Galant Reflex: Testing for Retention
- In quadruped position, stroke down one side and then the other side of the spine at the lower back. Observe for tightness, twitching, or jerky movements on the same side of the input. If observed, the reflex is likely still present.
When testing for this, I typically use the eraser of a pencil, as noted in Figure 16.

Figure 16. Testing for Spinal Galant reflex.
For this, you have the child in quadruped. You stroke down the side of the lateral side of the lower spine. Make sure you are not on any bony parts of the spine. We are looking for twitching, jerking, any type of tightness, or movement on the same side where you are providing the input. If you see any of that, then likely it is not integrated. With a test like this, I give a lot of direction to the child because I want them to know what I am doing as this is different from what they have felt before, and I do not want them to respond just because this feels weird. I also apply more of a firm pressure in this one as well as I do not want to elicit any tickling.
Exercise for a Retained Spinal Galant Reflex
- Have the child slowly move arms and legs up and out to a count of 10 going out and then back in.
- HEP: 10 repetitions, 1x per day
If you suspect retention based on your testing, one of the exercises is to have the child lie down with arms by their side, feet straight out, and feet extended. They will then move into a star position. (Figure 17).

Figure 17. Exercise position for a retained Spinal Galant reflex.
You want them to do this very slowly, counting from 10 to 15 going out and then the same count coming back in. You want this to be a very slow, methodical movement.
Tonic Labyrinthine Reflex (TLR)
Overview
- Foundational for postural stability for large muscle groups
- Common in kids with ADD, ADHD diagnoses
- Signs of Retention/Impact on ADLs:
- Decreased balance
- Poor spatial awareness
- Toe walking
- Hypermobility of joints
- Weak muscles
- Poor posture
- Motion sickness
- Poor ability to climb
- Atypical head position (forward or to side)
The TLR reflex is foundational for postural stability for large muscle groups. Here is an image of it in Figure 18.
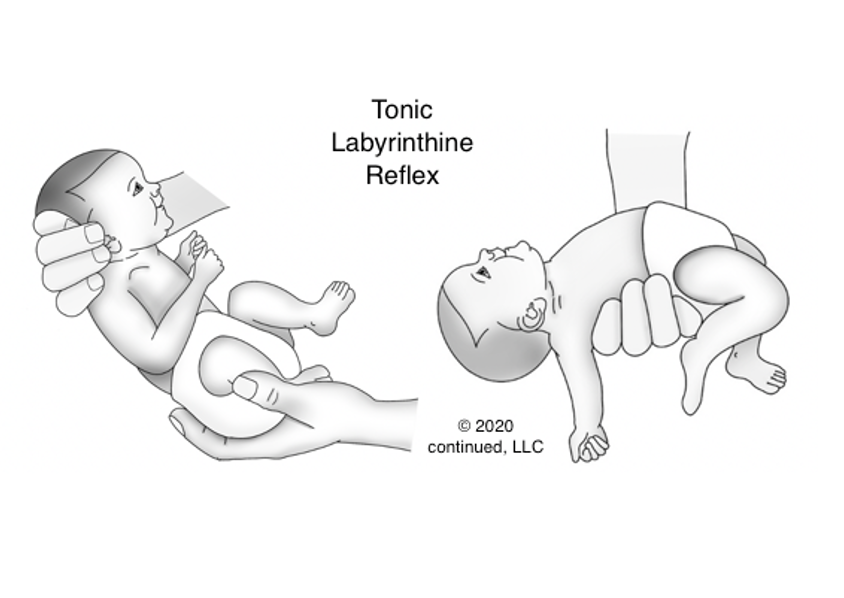
Figure 18. Tonic Labyrinthine reflex.
This reflex prepares the baby for the movements of rolling over, crawling/quadruped position, standing, and walking. Commonly, kids with ADD and ADHD have retention of this reflex. This is present in utero and up until about 3 1/2 years old. This is very different from many other reflexes that integrate within the first six to nine months of life. Depending on the age of your child, it is normal for them to have this reflex still.
After 3 1/2 years old, signs of retention include decreased balance, poor spatial awareness, toe-walking, hypermobility of the joints, weak muscles, poor posture, motion sickness, poor ability to climb, and atypical head positioning. We may also see a forward, sideways, or tilted-to-the-side head position.
TLR: Testing for Retention
- In prone, have the child put their arms down by their sides and feet/legs extended flat. Instruct the child to lift their head, legs, and arms off the ground while keeping arms and legs straight. If a child is observed to have difficulty keeping extremities straight, likely their reflex is still present.
To test for this, we will have the child lie prone with their arms down by their side and their feet extended (Figure 19).

Figure 19. Testing for the TLR.
We would instruct the child to lift their head, chest, legs, and arms off the ground. The arms should be palms up. This does not need to be a very excessive lift of the arms or legs. The chest should be completely off the ground, though. If this is hard for them to keep their arms and legs straight when they are doing this, then the reflex may still be present.
Exercise #1 for a Retained TLR
- Exercise #1: In prone, have child extend legs and put arms up in front of them. Instruct them to lift arms and legs off the ground and hold for 15 seconds.
- HEP: 15-second holds, 10 repetitions, 1x per day
Figure 20 shows the Superman position.

Figure 20. Superman position.
Once the child is prone, you instruct them to extend their legs out and their arms up in front of them. They need to hold this for 15 seconds. It is important to note that they may not be able to assume this position when you first start working with them. They may have difficulty with these exercises because of the retained reflex or any other diagnosis or delays. They may only be able to hold this position for a few seconds, or you may have to provide hand-over-hand assistance when you first start working on it. They may even need support to get into this position if they do not know how to move their body in that pattern. With all of the exercises, do not be afraid to be hands-on and show them how to do it. Using videos, pictures, and demonstrations can be helpful. Mirrors can also be helpful, especially with older children.
Exercise #2 for a Retained TLR
- Exercise #2: In supine, have child slowly pull knees to check with arms wrapped around legs (elbows pointed out) and tuck chin to chest with eyes closed, hold then slowly lower back to flat on the ground. Progress to holding for 15 seconds.
- HEP: 15-second holds, 10 repetitions, 1x per day
Another exercise for the TLR reflex is having the child pull their knees into their chest and wrapping their arms around their legs while supine (Figure 21).

Figure 21. Another exercise for TLR in supine.
When they wrap their arms, you want the elbows to go out when they're in that position. During this exercise, they should tuck their chin and close their eyes. They are going to go from a flat supine position to pulling into a tucked position. They need to hold this position for about 15 seconds. This is something that requires different muscle activation. Depending on their ability to get into this position and hold a static position, you might have to support them to keep their head up off the ground. This position requires a lot of core strength and postural stability. If they are not able to do this independently at first, that is fine. These are great exercises to use when a child needs a movement break or for a home program. With this, the child is working on integrating that reflex with more appropriate and mature muscle patterns while also working on the actual musculature for good stability.
Landau Reflex
Overview
- Necessary for postural development
- Signs of Retention/Impact on ADLs:
- Poor posture and muscle tone
- Summersaults are challenging
- Poor coordination for activities that require the upper body and lower body to move together
- Delayed motor development
- Pelvis rotates
- Commonly skips crawling in infancy
The Landau reflex appears in utero (Figure 21).
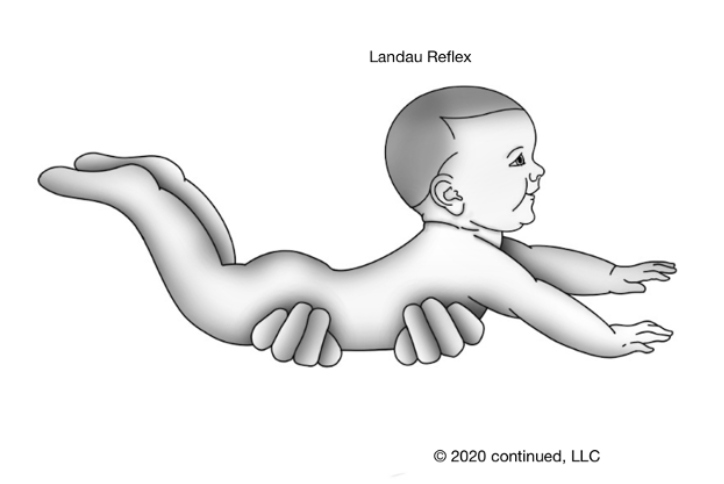
Figure 22. Landau reflex.
This reflex appears at four to five months of age. These last three (TLR, Landau, and STNR) are slightly different because they are typically present a little longer. Additionally, the Landau is slightly different because it does not appear at birth like the others. This one does not appear until about four to five months of age and integrates around one year old. This is necessary for postural development. If you hold a child in the air in prone, it would be typical to see their head in this upright extended position with a little bit of a convex arch in their back, and their legs flexed slightly. This would be a typical presentation of that reflex during the appropriate time period.
Some of the signs of retention that you would see after a year old would be poor posture and muscle tone. For example, somersaults would be very challenging. When you are working on a skill with a child and doing some of these gross motor movements, this may be something to look for. Perhaps a movement is hard because we have not looked at the reflexes yet, and some are not integrated yet. We can incorporate these into treatment to benefit other goals that we have.
Some more signs of retention we might see are poor coordination for activities that require upper and lower body movements together, like jumping jacks, cross crawls, and activities that have a difficult motor plan. Looking at reflexes is another way to consider what you are observing. Another thing to consider is crawling. Children that retain this reflex are likely to have skipped crawling, so it is important to note that during your intake.
Landau Reflex: Testing for Retention
- In prone on the floor, have the child lay face down with arms flat in front of them. Instruct them to lift their upper body and arms off the ground and keep their feet on the ground. Observe for the lifting of the feet. If seen, the reflex may still be present.
This is going to look similar to the Superman position. The biggest difference is that the child will be prone, face-down, with their arms in front of them. They are going to lift their upper body off the ground. We want their feet to stay in contact with the ground. If we see some lifting of the feet during this testing, as in Figure 23, this may indicate the reflex still being present.

Figure 23. Testing for TLR.
Exercises for a Retained TLR
And so, to help a child who has those signs of retention, the same positioning as testing would be, you'll just instruct them to lift their upper body and arms off the floor to a point that they're able to maintain their feet on the floor.

Figure 24. Exercises for TLR.
Most likely, the child will be able to lift their head off the floor, but then trying to move their arms off the floor will be where we see the challenge. You might need to help support their arms while also giving pressure at their feet or legs to help keep that positioning correct. They need to have their legs down and arms up. They will start really low, and we want to get them to a place where their head and chest, and arms are fully off the ground and hold that for 15 seconds. Again, at first, it may be one inch and one second off the ground. Feel free to show them what to do with their body and get into the correct positioning to make that muscle memory.
Symmetric Tonic Neck Reflex (STNR)
Overview
- Foundational for crawling
- Signs of Retention/Impact on ADLs:
- Poor posture in standing
- Poor seated posture
- Ape-like position in walking
- Low muscle tone
- W sitting position common
- Sloppy/messy eater
- Poor hand/eye coordination
The STNR reflex is often called the crawling reflex. It is foundational for crawling, and this picture is what it would typically look like (Figure 25).
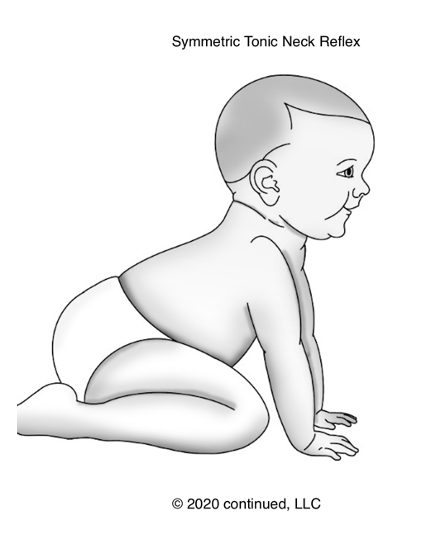
Figure 25. Symmetric Tonic Neck Reflex.
As the Landau reflex, this one does not present at birth, but rather it appears between six to nine months of age and integrates between 9 to 11 months. If you think about it, this makes complete sense as this is the typical crawling period of infancy. When placed in this position, the child would have their head up and extended, their arms straight, their legs in a position to go into a quadruped.
When we see signs of retention after about 11 months old, some of these might be poor posture and standing, poor posture when seated, an ape-like walking position, with a rounding of the back when ambulating, decreased muscle tone, and a W sitting position. The W sitting position shows a lot of hypermobility at the hips and decreased core strength. They may also have sloppy eating related to poor posture and low tone. Remember, with eating, there has to be proximal stability to have distal dexterity. If they do not have good postural control and are working way too hard to keep their body still and upright, they may not be able to use their hands independently and accurately to feed themselves. They may also have poor hand-eye coordination for the same reason. They cannot focus on what they are doing with their hands to catch a ball or bring their hand to their mouth.
STNR: Testing for Retention
- In quadruped, have the child with neutral/flat back, bend to tuck chin to chest in a slow-motion with 8-10 second count, and then lift the head bringing towards the back with 8-10 second count. Observe for back twitching, arch of the back, bending of arms, or weight shift back towards legs when moving head up. If any of these are observed, the reflex may still be present.

Figure 26. Testing positions for STNR.
In the middle picture, the child is in a quadruped with a neutral spine. Then, we would instruct them to go into the position of the child in the plaid shirt. They would tuck their chin to their chest and look down for about an 8- to 10-second count and then lift their head towards their back. We are looking for twitching of the back, a huge arch in the back, bending of the arms, or weight-shifting backward towards the legs. The weight-shifting is definitely what I see most prominently and most easy to observe. In the third picture, you can see all of that. The bending of that arm is a little bit exaggerated, and you will not likely see such an exaggeration with an older child. You can also see an arch in the back, and his bottom has moved a lot closer to his feet. His hips are no longer aligned with his knees as he is weight-shifting back to compensate for that movement.
Exercises for a Retained STNR
- The exercise is performed in the same position and motions as testing. Have the child hold the positions for 10-15 seconds.
- HEP: 10-15 repetitions, 1x per day
Figure 27 shows exercises for the STNR.
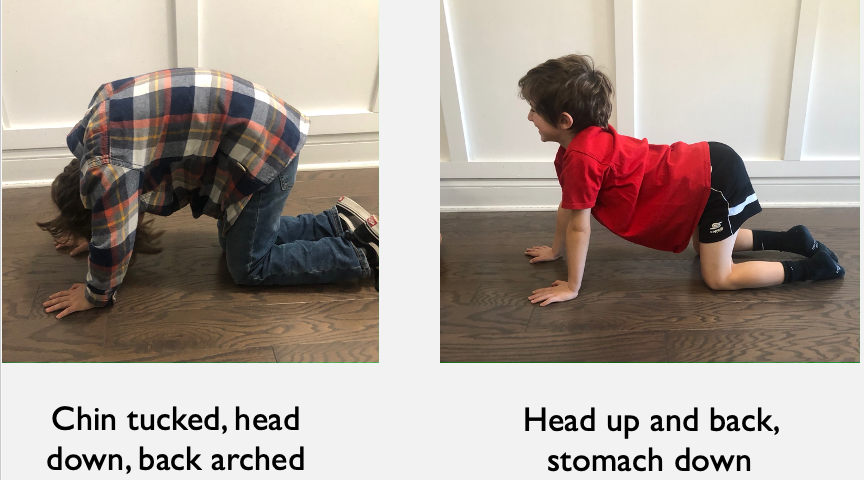
Figure 27. Exercises for the STNR.
The exercise for this particular retained STNR reflex would be doing the motion that we test it in. We want them to tuck their chin, bring their head down, and arch their back. We do not really emphasize the back arch in testing, but in the exercise, we do. They need to work on arching their back and bringing their chest down. Often, I give the cue of, "Try to touch your chin to your chest and look at your belly button." This puts them in the desired position without thinking about tucking their chin, moving their head, or arching their back. That is a lot of commands. They will then move from that position up to the upright position with their head up and their back and stomach down. For this position, I tell them to "Look towards the sky." Naturally, their stomachs will go down, and they will have a little bit more arch. You can help facilitate that for them as well. Show them what that feels and looks like in that position.
Home Program Overview Example
I would recommend that you go back and print out the chart that I put together on reflexes, the purpose, the ages, and the signs of retention. You can use this as an example (Figure 28).
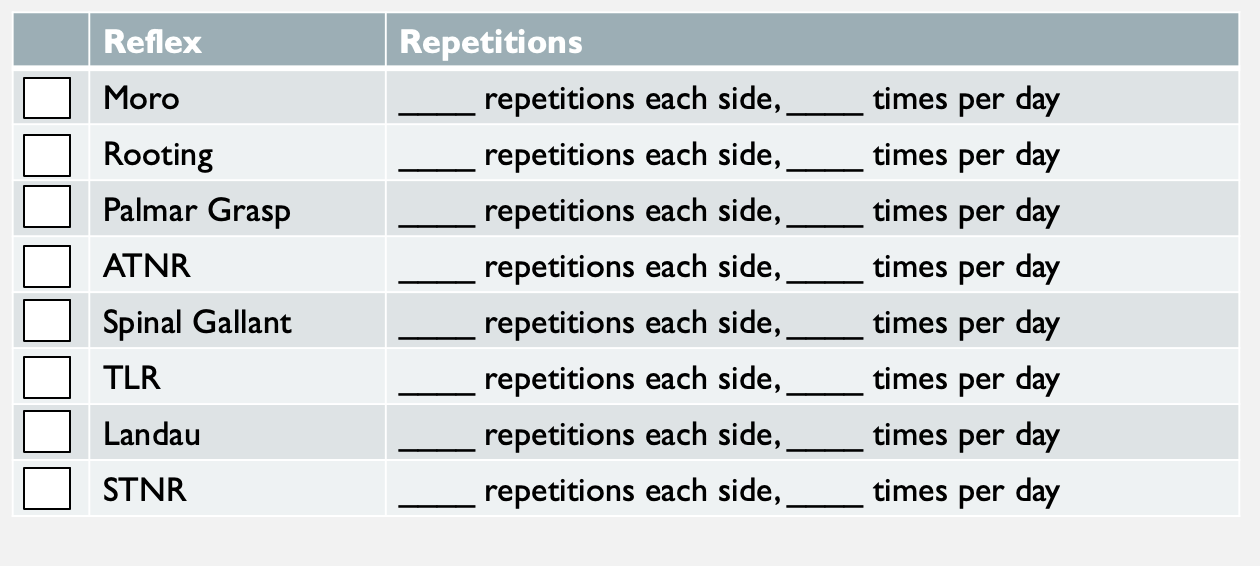
Figure 28. Home or clinic reflex checklist.
I include this in my kids' home program folders as an overview. I check off whichever one I am working on for that specific kid and the number of repetitions and the times per day. The ideal amount was written on each slide. You can use that as a goal to work toward. This might not be appropriate initially for your child. You also might not want to include this chart in your home program until the child is more successful with them in the clinic unless you have a caregiver that you can train during your session.
Along with this cover page as part of their home program, I also have a sheet for each reflex written out in a little bit more family-friendly language (Figure 29).
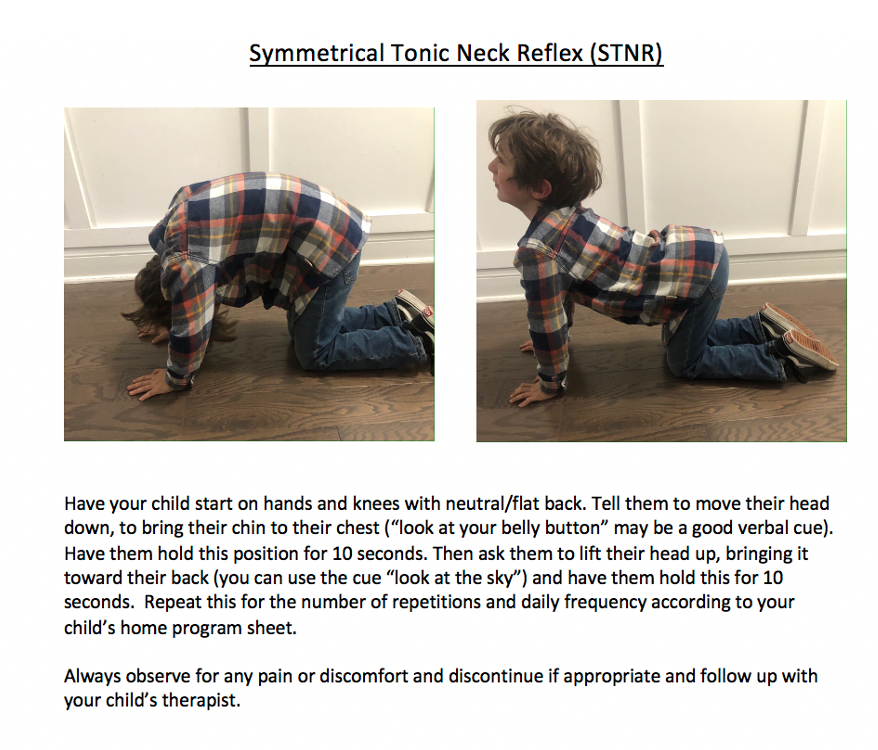
Figure 29. Example of a specific exercise included in a home program.
This gives them a simple overview of what we want them to tell the child, what we want the child to do, and then also the pictures for parents to refer to as well. I always add a disclaimer that if the child is in pain or uncomfortable, they should discontinue until they are back in the clinic. We do not want them to be uncomfortable in any of these positions.
Summary
Assessing for primitive reflexes and working on these positions is another way to help the child have more appropriate developmental skills.
Questions and Answers
Can you provide hand-over-hand for their Palmar reflex exercise, or does the child need to activate their muscles independently? I am thinking of an older child who will not actively participate due to cognitive age and disabilities.
You can provide hand-over-hand for the exercises. The purpose of the exercises is to get that exposure to the input and that purposeful movement to break that immature movement pattern. Hand-over-hand input is appropriate because we have to have them perform that movement. The goal would be to progress out of that.
How would you do the starfish exercise with an 11-month-old?
Again, this can be hands-on. This will be a lot harder to do with an 11-month-old because they are not going to be at a stage where they are imitating movements. Certainly, it would be appropriate to move them through that pattern. Most likely, it would take two people to do it effectively. This could be something that you would do with the parents.
Can a student have more than one retained reflex at the same time?
Yes, this is very common. If we see some reflex retention, there are likely multiple.
While assessing the ATNR, would it be appropriate to guide the head turn to pace the speed?
When assessing it, I would not want to be as hands-on. I would want them to try to do it on their own at first. If that is not possible, then, of course, being hands-on is fine. I would make a note of that. And, If they were not very successful with that, even with hands-on help, I would go ahead and work on some exercises as if it was retained. Then, you could assess it again during progress monitoring.
Just wondering how long the child should hold each position for the retained reflex exercises?
It should say that on each slide. They are all a little bit different. It just depends on which one you are talking about specifically. With most of them, we want the child to use slow, methodical movements, like an 8- to 12-second count. The static ones, like the Superman position, are held for 10 to 15 seconds.
Any ideas on how to get littles to do those movements and play?
This is a great question. With each of them, it is going to be a little bit different. The Palmar grasp for little ones is usually easier to work on because you can be hand-over-hand. You can use many different modalities to work on those movements with just some stimulation at the palm. You can do that with a lot of different play activities. I mean, as simple as squeezing a plush doll. It is important to think of ways to incorporate these exercises and positions into the child's interests and play activities.
Do they need to hold prone extension for testing for a certain length of time?
There are some different ones that you will be in prone extension, but 10 to 15 seconds is plenty. What we are looking for is those supplemental movements. If you see twitching, bending, or an inability to stay in those positions, those are the signs. However, we also have to take into consideration the muscle aspect of some of those positions. If they can hold it 8 to 10 seconds before they start moving, I would say that I would not be concerned about a retained reflex.
Did you say how often to do the exercises?
Again, this information is on each of the slides. As the clinician, you should consider what the child can do and what they can tolerate and adjust the parameters as appropriate. That recommended number on the slide would be what we are working towards. We should be getting to a point where we see less difficulty with the testing of those. If you do this testing at the beginning of treatment, you can see how they have changed when you go back. An example would be seeing a dissociation between the body movements compared to the beginning of treatment.
Have you been able to test children younger than three successfully?
You can use your clinical reasoning. You can easily observe the Palmar Grasp, Rooting, and Moro reflexes without even doing a purposeful test. Those are things that you can see while a child is playing. Grasp is obviously the easiest. You are going to see this in younger kids, especially those with developmental delays. Some of the other reflexes and test positions are harder. Getting some children younger than three into quadricep position is a challenge in itself. However, that is a reason to do it. If that position is extremely challenging and the child is three years old, we need to consider that from a clinical aspect. These are all ideal situations, of course. If you have a child like the one pictured above who is typically developing and following verbal cues, it is much easier. Be creative and keep all of these in mind when assessing and observing a child during play.
I started a running club at an elementary school. Do you think some of these gross motor exercises would be good to do as a warmup, even if only a certain amount of kids may have issues?
Absolutely. These exercises are not going to be detrimental or harmful to anyone. Like with anything you are doing, you need to make sure no one is in pain or having discomfort with them. Anytime that we are doing purposeful exercise and having a child imitate our body movements, hold dynamic positions or hold static positions, or move slowly through dynamic patterns, we are working on many skills that most kids need. These are great to incorporate whenever you can.
What changes are we looking for with the home program?
We are looking for the ability of the chile to eventually be able to do the test without having any signs of retention. We are looking for progress from being able to get in the position accurately, hold the position, and then be able to complete the test without any signs that there is difficulty.
Do you have to integrate one reflex before working on a different reflex?
There is not a continuum for reflexes. I would look at the chart. Obviously, the ones that are supposed to be integrated earlier in life, depending on how present or impactful those are, would be the ones to start with.
How would you document reflexes in an evaluation?
I document them as testing for primitive reflexes or noted signs of retention. There is a lot of research around primitive reflexes. The research says that primitive reflexes can impact development. Where the research is lacking is if doing these activities helps with integration. This is not what we are focusing on, not what AOTA is supporting. We are doing these exercises and activities to help facilitate more appropriate and mature movement patterns to help with survival and development.
References
Available in the handout.
Citation
Heidenreich, S. (2021). Understanding primitive reflexes: How they impact child development and intervention strategies for integration. OccupationalTherapy.com, Article 5409. Available at www.OccupationalTherapy.com
