Editor's note: This text-based course is a transcript of the webinar, Understanding Seizures And Epilepsy In The Occupational Therapy Setting, presented by Nancy Nathenson, RRT.
Learning Outcomes
- After this course, participants will be able to analyze the two types of seizures and their symptom manifestations.
- After this course, participants will be able to apply the three basic principles of seizure first aid.
- After this course, participants will be able to evaluate biomedical and holistic epilepsy management interventions.
Introduction
It's truly a pleasure to be here with all of you. I hold a deep appreciation for therapists and the tireless dedication they demonstrate in the field of rehabilitation. Today, we're diving into a crucial topic: seizures. If you've ever encountered someone experiencing a seizure, you know firsthand how unsettling and distressing it can be, especially when you're unsure of what steps to take. Seizures often catch us off guard, manifesting in various ways ranging from dramatic, with the body moving erratically, to subtle and easily missed. Our goal today is to explore this topic comprehensively, equipping ourselves with the knowledge and skills to navigate these situations effectively. Thank you all for joining me on this journey. Let's begin.
U.S. Demographics
- 1 in 10 people will have a seizure in their lifetime
- ≈ 1 million of them still have seizures even though they are on medication to prevent them
- ≈ 3 million Americans of all ages live with epilepsy
- 1 in 26 people will be diagnosed with epilepsy during their lifetime
- 25% of cases develop before the age of 5
- Males more likely than females
- African Americans more likely than Caucasians
In the United States, the impact of seizures and epilepsy is profound and widespread. Shockingly, one in ten people will experience a seizure at some point in their lives. Despite being on medication aimed at preventing seizures, almost a million individuals continue to have seizures. This persistence highlights the challenges in managing epilepsy effectively.
Epilepsy, a neurological disorder characterized by recurrent seizures, affects about 3 million Americans of all ages. The prevalence is striking, with one in 26 individuals receiving a diagnosis of epilepsy during their lifetime. Disturbingly, a quarter of epilepsy cases begin before the age of five, underscoring the significant impact on children and their families.
Moreover, there are notable disparities in the prevalence of epilepsy across demographic groups. Males have a higher likelihood of developing epilepsy compared to females, suggesting potential gender-specific risk factors or biological differences. Additionally, African Americans are more likely than Caucasians to be diagnosed with epilepsy, highlighting disparities in health outcomes within our society.
Seizures and the Brain
- Sudden uncontrolled electrical disturbance in the brain
- There is a “short circuit” in the way messages are sent.
- Seizures can occur with other medical conditions.
- **Not everyone who has a seizure has epilepsy.**
A seizure is a sudden, uncontrolled electrical disturbance in the brain. There's a short circuit in a way, messages are sent and these seizures can occur with other medical conditions and we'll get into that more in a bit. Not everyone that has a seizure has epilepsy.
Causes of Seizures
The causes of seizure here is the long list.
- Abnormal levels of sodium or glucose
- Brain infections
- Brain injury
- Brain diseases
- Tumors
- Heart disease
- Fever
- Poisoning
- Stroke
- Street drugs
- Electric shock
- Heat illness
- Genetic conditions
It makes sense when we're in healthcare that sodium and glucose levels when they're abnormal, could cause something like that. Brain infections, brain injury, brain diseases, tumors. I have experienced my husband having a brain tumor, and he developed a seizure disorder along with that and also became hemiplegic after his surgery. But he has had a seizure disorder for some time now. So I have some personal experience with this heart disease, fevers, poisoning, stroke, street drugs, electrical shocks, heat, illness.
And there are also genetic conditions that contribute to and can cause seizures.
Characteristics of a Seizure
- Seizures can result in changes in:
- Movement
- Sensation
- Behavior
- Speech
- Awareness
- **The area of the brain involved determines what a seizure looks like**
The characteristics of a seizure are situations that result in changes in movement. These can be sensation, behavior, speech, awareness, or some or all of these characteristics. The area of the brain involved determines what the seizure looks like. So imagine if the seizure is located in the motor strip.
That could affect motor function or abilities, and if it's in the frontal lobe, it could also affect speech more.
- Seizure signs and symptoms of seizures vary from person to person,
- But in most cases, they are usually consistent and predictable for each individual.
Seizure signs and symptoms vary from person to person, but in most cases, they are consistent and predictable for each individual. And that's really good to know because those consistent and predictable manifestations are really great to know throughout an individual's life.
General Symptoms/Warning Signs of a Seizure
- Staring
- Not responding to words or noises for brief periods
- Rapid eye blinking and staring
- Appearing confused or in a daze
- Nodding the head rhythmically when not aware or conscious
- Stiffening body
- Falling suddenly for no apparent reason
- Loss of consciousness
- Loss of bowel or bladder control
Here are some general symptoms or some warning signs of a seizure. As I mentioned, some are very subtle. like staring or not responding to words or noises for brief periods.
This is what my husband experienced. He also turned his head hard to the left and couldn't respond. He stared without blinking his eyes. A person can appear confused or in a daze. They can nod their heads rhythmically when they're not aware or conscious. The body can stiffen or fall suddenly for no apparent reason. Loss of consciousness and even loss of bowel or bladder control can also occur.
Did You Know?
- Most seizures are NOT medical emergencies.
- A person may NOT be aware they are having a seizure.
- Seizures are NOT contagious.
- A person can NOT swallow their tongue during a seizure.
- Epilepsy is a medical disease.
- A person CAN die from a seizure.
It's crucial to dispel some common misconceptions surrounding seizures. While seizures can be alarming to witness, most of them are not medical emergencies. In many cases, the person experiencing the seizure may not know what's happening.
It's important to understand that seizures are not contagious. They result from abnormal electrical activity in the brain and are not caused by external factors or infectious agents.
Another widespread misconception is the idea that a person can swallow their tongue during a seizure. This is not the case. The tongue may move around during a seizure due to muscle contractions, but it is physically impossible to swallow it. Attempting to put something in the person's mouth can be harmful and increase the risk of injury.
Epilepsy is indeed a medical condition, and seizures can have serious implications. While most seizures are not life-threatening, there is a risk of complications, particularly if the seizure is prolonged or if the person experiences injuries during the episode.
- **Anything the brain can do normally the brain can do during a seizure.**
Anything the brain does normally, it can do during a seizure. The heart will keep beating, and the lungs will keep breathing. Now, that doesn't mean a person may not develop difficulty with their breathing or something of that nature, but know that normally, the brain will do just what the body does automatically.
Risks Related to Seizures
- Physical injury
- Difficulty breathing
- Early death
- Accidents or drowning
- Breathing or heart problems
- Suicide
- Sudden unexpected death (SUDEP)
Significant risks are associated with seizures, and it's crucial to be aware of them. During a seizure, the individual may lose control of their muscles, leading to falls and injuries such as head trauma, broken bones, or cuts. Seizures can occur at any time, including while a person is engaged in activities such as driving or swimming, increasing the risk of accidents or drowning. Some seizures can interfere with normal breathing patterns, leading to respiratory distress or even temporary cessation of breathing, known as apnea. Seizures can also affect heart rhythm and function, posing a risk of cardiac complications such as arrhythmias or sudden cardiac arrest. Individuals with epilepsy, particularly those with uncontrolled seizures, may experience significant psychological distress and have an increased risk of suicide. Additionally, sudden unexpected death in epilepsy (SUDEP) is a rare but serious complication, occurring in approximately one in 1,000 individuals with uncontrolled seizures each year. SUDEP is thought to result from a combination of factors, including respiratory and cardiac dysfunction during or after a seizure.
Seizure Types
- Where they start in the brain
- Focal
- Generalized
- Unknown
- They can occur whether or not AWARENESS is affected.
- And whether or not the seizure involves other symptoms such as movement…
Seizures can be categorized into different types based on where they originate in the brain and how they affect neurological function. Focal or partial seizures originate in a specific area of the brain and may affect only one part or side of the body. Focal aware seizures (simple partial seizures) and focal impaired awareness seizures (complex partial seizures) are two subtypes.
Generalized seizures involve abnormal electrical activity that affects both sides of the brain simultaneously. There are several subtypes, including absence seizures, tonic seizures, clonic seizures, tonic-clonic seizures, and atonic seizures.
Unknown onset seizures do not have a clear focal or generalized onset and may involve a combination of symptoms or unusual presentations. The cause of these seizures is often unknown, and they can vary widely in their effects on awareness and movement.
Understanding these different seizure types is crucial for accurate diagnosis and appropriate treatment, as it helps healthcare providers tailor treatment plans to address the specific needs of individuals with epilepsy. Additionally, raising awareness of these seizure types can empower individuals and their caregivers to better understand and manage the condition. Examples are shown in Figure 1.
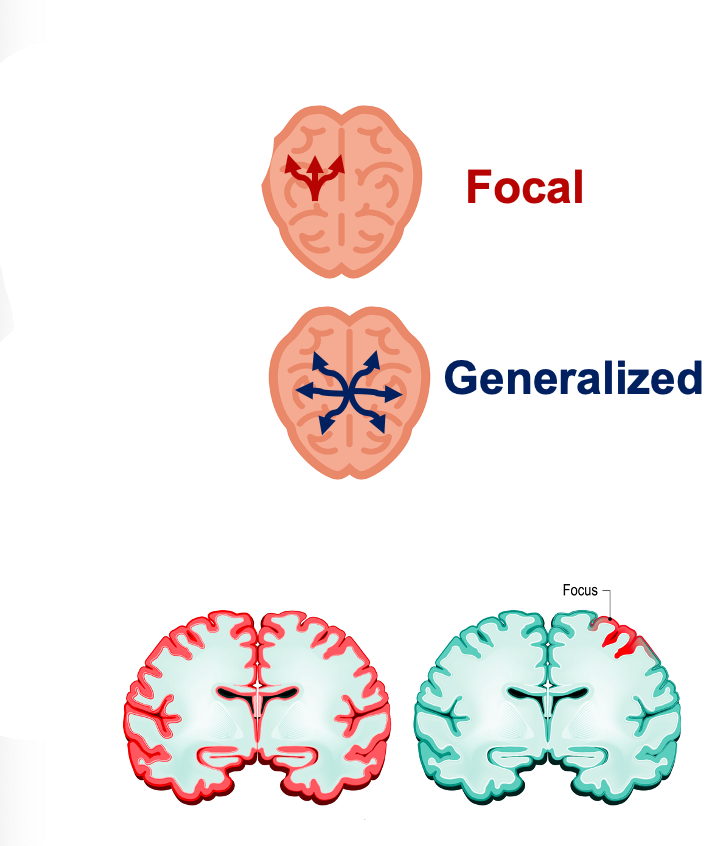
Figure 1. Focal versus generalized seizures.
Seizure With No Change in Awareness: Focal Aware Seizure
- Is fully awake and aware
- Any change in behavior
- Motor: rhythmic twitching or jerking (face and extremities)
- Sensory: tingling, sounds, smells, visual changes
- Psychic: change in thinking, feeling, perceptions (fear, anxiety, déjà vu)
- Length- 1-3 min.
During focal aware seizures (formerly known as simple partial seizures), individuals remain fully awake and aware of their surroundings. These seizures typically last from about one to three minutes and may involve various changes in behavior. Motor symptoms can include rhythmic twitching or jerking movements, affecting either the face and extremities or just one of these areas.
In addition to motor symptoms, focal aware seizures can involve sensory experiences. Patients may report tingling sensations or changes in sounds, smells, or visual perception. Some individuals may have warning signs or auras before the seizure, such as a metallic taste in the mouth or other unusual sensations. These psychic symptoms can include changes in thinking, feeling, and perception, leading to experiences such as fear, anxiety, or déjà vu, which the person may not fully recognize or understand at the time.
Seizure With Confusion or Not Aware: FOCAL Impaired Awareness Seizure
- Is fully awake and aware
- Any change in behavior
- Motor: rhythmic twitching or jerking (face and extremities)
- Sensory: tingling, sounds, smells, visual changes
- Psychic: change in thinking, feeling, perceptions (fear, anxiety, déjà vu)
- Length- 1-3 min.
During focal impaired awareness seizures (formerly known as complex partial seizures), individuals may experience a loss of awareness or be in a state of confusion. They may appear blank or dazed, and exhibit repeated purposeless movements known as automatisms. These movements can include actions such as lip-smacking, chewing motions, or picking at clothing. Additionally, individuals may display clumsy movements and may have difficulty speaking or responding to others.
Following the seizure, individuals may experience symptoms such as tiredness, headache, and nausea. These post-seizure effects can occur after most types of seizures, including milder ones. It's important to note that individuals experiencing a focal impaired awareness seizure may become combative if restrained, highlighting the need for careful management and support during and after the seizure.
These seizures typically last about one to three minutes, but the duration can vary depending on the individual and other factors. Understanding the characteristics of focal impaired awareness seizures is essential for providing appropriate care and support to individuals living with epilepsy.
Seizure With Staring and Not Aware: GENERALIZED Absence Seizure
- Pause in activity with a blank stare
- A brief lapse in awareness
- Possible chewing or blinking motion
- May occur many times a day
- After a seizure, returns to normal immediately
- ** Often followed by headache, confusion, tired, soreness, a bitten tongue, and speech difficulty**
- Length- Less than 20 seconds
A generalized absence seizure, or petit mal seizure, is characterized by a brief lapse in awareness accompanied by staring and a lack of responsiveness. During the seizure, there's typically a pause in activity, and the individual may exhibit repetitive movements such as chewing or blinking.
These seizures can occur frequently throughout the day, sometimes many times per day. They are brief, lasting less than 20 seconds, and afterward, the individual typically returns to normal consciousness without any memory of the episode. However, they may experience post-seizure effects such as headache, confusion, fatigue, and muscle soreness. Additionally, they may have bitten their tongue during the seizure, leading to discomfort and potential speech difficulties afterward.
Despite their short duration, generalized absence seizures can have a significant impact on the individual's daily life, especially if they occur frequently. Understanding the characteristics of these seizures and their potential effects is essential for providing appropriate support and management for individuals living with epilepsy.
Seizure With Loss of Consciousness: TONIC CLONIC Seizure
- A sudden hoarse cry
- Loss of consciousness
- A fall
- Stiff body, arms, and legs (tonic), then rhythmic jerking (clonic)
- Shallow breathing and drooling may occur
- Possible loss of bowel or bladder control
- Length: Typically between 1 and 3 minutes
During tonic-clonic seizures, also known as grand mal seizures, individuals experience a sequence of distinct phases. These seizures typically begin with a sudden loss of consciousness, often preceded by a loud, involuntary cry. This loss of consciousness is accompanied by a sudden fall, as the individual's muscles become stiff and rigid, known as the tonic phase. This stiffness may affect the arms, legs, and trunk.
Following the tonic phase, the seizure progresses to the clonic phase, characterized by rhythmic jerking movements of the limbs and sometimes the face. Due to impaired muscle control, breathing may become shallow, and drooling may occur. Additionally, some individuals may experience loss of bowel or bladder control during the seizure.
The duration of tonic-clonic seizures typically ranges from one to three minutes, although this can vary depending on factors such as the individual's overall health and the specific circumstances surrounding the seizure.
Other Generalized Seizures
- Change in muscle tone or tension
- Tonic-Stiffness may fall like a tree trunk
- Atonic- Loose or floppy, may fall like a rag doll, twitching/jerking of muscles
- Myoclonic- Brief jerks in muscle or group of muscles
- Clonic- Rhythmic jerking in part or all of the body
Generalized seizures can present with various muscle tone or tension changes, resulting in diverse movements.
Tonic seizures are characterized by increased muscle stiffness, often leading to a sudden rigidity resembling the collapse of a tree trunk. Conversely, atonic seizures involve a sudden loss of muscle tone, causing individuals to fall limply, akin to a rag doll.
In myoclonic seizures, brief, abrupt jerks or twitches occur in specific muscles or groups of muscles without necessarily involving the entire body. Clonic seizures, on the other hand, manifest with rhythmic jerking movements that can affect specific muscle groups or the entire body.
Understanding these different manifestations of muscle movement in generalized seizures is crucial for accurately diagnosing and effectively managing epilepsy. By recognizing the distinct characteristics of each seizure type, healthcare providers can tailor treatment plans to meet the individual needs of patients living with epilepsy.
Seizures in Children
Statistics
- ≈ 3% of all children have a seizure when < 15 yrs. of age
- 50% of these are febrile seizures
- Ear infection, chicken pox, cold
- Most common type
- Risk factors include:
- Genetics
- Developmentally delayed children
- 1 of 4 children who have febrile seizure repeat within 1 year
When discussing seizures in children, it's important to note that much of the information also applies to adults, particularly regarding first aid measures. Approximately 3% of all children experience a seizure before the age of 15, with half of these being febrile seizures. Febrile seizures are often triggered by infections such as chickenpox or the common cold, which induce a fever in the child.
Febrile seizures are indeed the most common type observed in children. Certain risk factors may predispose children to seizures, including genetic factors and developmental delays. Additionally, approximately one in four children who experience a febrile seizure will have a recurrence within one year.
Understanding these risk factors and the prevalence of seizures in children is crucial for parents, caregivers, and healthcare providers. By recognizing the signs and potential triggers of seizures, appropriate measures can be taken to ensure the safety and well-being of children who may be at risk. Later on, we'll delve deeper into febrile seizures and their management.
Other Disorders
- Children with seizures often have another disorder
- Fainting
- Breath-holding spells
- Night terrors
- Migraines
- Psychic disturbances
Children with seizures may also experience other disorders or conditions, such as fainting, which can occur due to inadequate blood flow to the brain, often triggered by factors like dehydration. Remedies for dehydration may include ensuring adequate hydration by drinking more water, maintaining regular mealtimes, and consuming salty foods when appropriate.
Breath-holding spells are another phenomenon observed in children, particularly between the ages of six months and six years, with the peak occurrence between six and 18 months. These spells often occur after the child experiences emotions like anger, frustration, or pain and may lead to temporary loss of consciousness.
There are two main types of breath-holding spells: cyanotic and pallid. Cyanotic breath-holding occurs after intense crying and may result in the child's face turning blue, typically due to anger or frustration. Pallid breath-holding spells involve the child's face turning pale, often triggered by similar emotional experiences.
It's important to note that children do not intentionally have breath-holding spells, and these episodes can last up to a minute or two.
Additionally, children may experience night terrors during deep stages of sleep, which can last around 45 minutes. Migraines, though less common in children than adults, can still occur and may be triggered by various factors, including genetics, certain foods and beverages, stress, anxiety, infection, and minor head trauma.
Furthermore, children with seizures may be at risk of developing other psychological and mood disorders as they grow, including anxiety disorders, personality disorders, and psychotic disorders. Understanding the potential comorbidities associated with seizures in children is essential for providing comprehensive care and support tailored to their individual needs. Moreover, addressing factors such as nutrition, stress management, and psychological well-being can play a significant role in managing seizures and promoting overall health and quality of life for children with epilepsy.
Infantile Spasms
- Occur in children < 18 mos.
- May be associated with intellectual disability
- Sudden, repeated, uncontrolled movements
- Flexed stature
- Frequently occur on awakening
- See the Signs
- Take a video
- Obtain a diagnosis
- Prioritize treatment
Infantile spasms can sometimes be mistaken for a seizure and typically occur in children under 18 months of age. These spasms may be associated with intellectual disabilities, which can be challenging to detect in babies. During an episode of infantile spasms, sudden, repeated, and uncontrolled movements occur, often accompanied by a flexed posture, head bobbing, and body crunching.
It's crucial to differentiate infantile spasms from the normal startle reflex observed in infants, which typically lasts only momentarily in response to loud noises or other stimuli. If you notice signs of infantile spasms in your child, it's essential to take a video recording of the episodes, seek a medical diagnosis, and prioritize appropriate treatment.
Raising awareness about infantile spasms is vital for early detection and intervention. December is recognized as Infantile Spasms Awareness Month, providing an opportunity to educate parents, caregivers, and healthcare professionals about this condition and its management. By promoting awareness and understanding of infantile spasms, we can improve outcomes and quality of life for affected children and their families.
Febrile Seizures (FS)
- Occurs in children between 6 mos. - 6 yrs.
- The most common type of seizure in children
- Most children with febrile seizures rarely develop long-term health problems.
- Possible genetic and environmental causes
- FS has no adverse effects on behavior, scholastic performance, or cognition.
- Most FS are short-lived and self-terminating and do not require long-term treatment with anti-epileptic drugs.
Febrile seizures are common in children between six months and six years of age, often triggered by fever. While they can be alarming for parents, most children with febrile seizures do not experience long-term health issues. These seizures are typically short-lived and self-terminate, meaning they stop on their own without the need for long-term treatment with antiepileptic drugs.
The causes of febrile seizures can vary and may include genetic factors as well as environmental triggers. Infections, particularly viral infections like the flu and the virus that causes roseola, are common culprits behind febrile seizures. Interestingly, febrile seizures are more commonly associated with viral infections than bacterial infections.
In addition to infections, other factors such as hypoglycemia and electrolyte imbalances can also contribute to febrile seizures. It's important to note that while febrile seizures may be frightening to witness, they generally do not have any adverse effects on a child's behavior, academic performance, or cognitive development.
Overall, febrile seizures are usually benign and tend to resolve without complications. However, if your child experiences a febrile seizure, it's essential to seek medical attention to determine the underlying cause of the fever and to ensure appropriate management and treatment.
The 3 Basic Principles of Seizure First Aid
- Stay
- Safe
- Side
Let's delve into the basics of seizure first aid, as outlined by the Epilepsy Foundation. You should remain with the individual until they are awake and alert and the seizure has ended. It's crucial to time the seizure and check for any medical identification the person may have.
To ensure the individual's safety during the seizure, guide them away from any potential sources of harm and protect them from injury. If the person is not awake and aware, gently turn them onto their side to help maintain an open airway. Loosen tight clothing and place something soft under their head to prevent injury.
Turning the person onto their side, especially if they are not fully conscious, can help keep their airway clear and reduce the risk of choking. Enlist the help of bystanders to assist with tasks such as placing something under the person's head or loosening tight clothing.
Knowing what to do during a seizure can be crucial, especially when bystanders feel unsure or anxious. These simple steps can help ensure the safety and well-being of someone experiencing a seizure. Later, we'll discuss what actions to avoid and when it's appropriate to call emergency services.
What NOT To Do
- Do NOT restrain or forcibly hold the person down.
- Do NOT put anything in their mouth.
- Do NOT give water or food until the person is awake and can swallow.
Knowing what actions to avoid when someone is experiencing a seizure is important. Here are some key "don'ts" to keep in mind:
Do not restrain or forcibly hold the person down. Restraining someone during a seizure does not stop the seizure and can lead to injury or increase confusion, agitation, or aggression. Remember, they are not intentionally resisting or fighting back.
If the person tries to walk around during the seizure, allow them to do so in a safe area, and gently guide them to safety if needed. However, do not attempt to restrict their movements forcefully.
Do not put anything in the person's mouth. Contrary to popular belief, placing objects or fingers in the mouth during a seizure can cause injury to both the person having the seizure and the person attempting to help. There is no risk of swallowing the tongue during a seizure, so inserting anything into the mouth is unnecessary.
While rescue medications may be part of the individual's treatment plan, they should be administered according to specific instructions, such as placing them inside the cheek. Avoid giving food or water to the person until they are fully awake and able to swallow safely. Giving food or water while the person is still in a state of altered consciousness can increase the risk of aspiration, where the substance enters the lungs instead of the stomach.
What to Look For During a Seizure
Early Signs
- What did you see or hear first?
- Was the person able to tell you they didn’t feel well?
Initially, we want to know what they saw or heard. Are they able to tell you they didn't feel well? A lot of times, individuals who have seizures do have this. Something tips them off that they are not feeling well, and they might expect a seizure during a seizure.
What to Look for During Seizure
- What happened next?
- Was the person awake, confused, or not conscious?
- What part of the face and body was involved?
- Did you notice changes in speech or behavior?
Check what happened next. Was the person awake, confused, or not conscious? We want to assess their alertness. What part of the face and body was involved? Did you notice any changes in their speech or behavior during the seizure? Of course, if this happens in your practice, you'll document this information.
Share What Happened During the Seizure
- How long did it last?
- What did you observe?
- Was the person injured?
- When & where did the seizure take place?
- Did the person take or was given any medicine?
- Was the seizure different from the usual?
- Provide written notes if possible.
Here are some different things that you would document.
What to Look for After a Seizure
- How long did it last?
- Did the person quickly return to normal?
- Was the person tired or confused? Describe other symptoms.
After the seizure, you want to determine its duration. This will impact whether or not a 911 call is needed. Did the person quickly return to normal, and were they tired or confused? Were there any other symptoms?
What to Expect After a Seizure
- The Recovery (*postictal period)
- Time immediately after a seizure, before the child returns to their usual state of awareness and function
- How a person feels and functions will depend on the type of seizure experienced.
- How to help?
- Help the child to a safe place to rest.
- Check if they are alert and aware.
- Stay with them until another adult arrives.
After a seizure, there is a recovery period during which things have calmed down. It's called the postictal period, and it's the time immediately after a seizure before the child or adult returns to their usual state of awareness and function. How that person feels afterward will depend on the type of seizure experienced.
Some of the after-effects may be more profound than others. How to help: Always help the child or individual find a safe resting place. Ensure they are alert and aware, and stay with them until another adult arrives.
Call 911 IF...
- Seizure lasts longer than 5 minutes
- The person does not return to their usual state
- The person is injured, pregnant, or sick
- Repeated seizure
- First time seizure
- Difficulty breathing
- Seizure occurs in water
If a seizure persists beyond five minutes, regardless of the individual's identity, and the individual does not revert to their typical state, it is imperative to seek medical assistance. This is especially crucial if the person is injured, pregnant, or experiencing illness or if the seizure recurs. Additionally, contacting emergency services is warranted if it is the individual's initial seizure episode, if they exhibit breathing difficulties, or if the seizure unfolds in a water environment. Real-world scenarios where seizures may manifest include the instances below.
Any Seizure Setting: Wheelchair
- Keep the person in a wheelchair or stroller if possible
- Secure wheelchair
- Fasten the seatbelt (loosely) to prevent the person from falling
- Protect and support the head
- Ensure breathing is not blocked and saliva can flow from the mouth.
- ** Follow Seizure Action Plan**
In situations where the individual is confined to a wheelchair or stroller, it's essential to maintain them in that position whenever feasible. Ensure that the seatbelt is securely fastened to prevent any risk of falling or tipping over. Given the possibility of head movement during a seizure, providing adequate head protection and support is crucial, especially to prevent impact against the sides of the stroller. Additionally, it is important to monitor their airway to prevent obstruction and facilitate saliva flow from the mouth by wiping it away as necessary. Following the established seizure action plan is paramount, and we'll delve into that shortly.
Any Seizure Setting: At the Bus Stop, On the Bus
- Guide the child away from the street
- Guide the child away from the streetHold back gently and call for help
- Don’t leave the person alone
- If there is a seizure with loss of consciousness, place the child on their side facing away from the seat back or in the aisle.
- Remain with the child until they are awake and alert
- Call 911 if necessary
Certain precautions are essential when dealing with a seizure scenario involving an individual at a bus stop, on a bus, or awaiting transportation outside a pediatric area. First and foremost, it's crucial to prevent the individual from entering the street or parking lot, gently guiding them away from any potential danger while immediately calling for assistance. It's imperative never to leave the individual unattended during this time. In the event of a seizure with loss of consciousness occurring while on a bus, van, or car, it's advisable to ensure that the individual is facing away from the seat back to minimize any risk of injury. Alternatively, laying them down in the aisle of the vehicle can offer a safer environment. It's vital to remain with the individual until they regains consciousness and alertness and to promptly dial 911 if necessary based on the criteria for emergency calls.
Seizure with Loss of Consciousness Setting: In the Water or When Swimming
- Support the head so that the mouth and nose are above the water
- Remove the child from the water as soon as can be done safely
- Give seizure first aid
- If the child is not breathing, begin rescue breathing
- Always call 911 even if they appear fully recovered
In the event of a seizure occurring while an individual is in the water or swimming, immediate action is paramount. Firstly, it's essential to support their head to keep their nose above the water's surface and swiftly remove them from the water, prioritizing safety throughout. Administering seizure first aid involves ensuring the individual's airway remains clear and providing necessary support until the seizure subsides. If the individual is not breathing, initiating rescue breathing is imperative. Regardless of whether the individual appears fully recovered after the seizure, it's crucial to promptly call 911. This precaution is necessary because the seizure may not have been immediately recognized, and there is a risk that the individual may have swallowed water, posing a potential medical concern requiring professional intervention.
Seizure Triggers
- Important to identify when a child has a seizure IF there is a particular “trigger.”
- Seizure Triggers:
- Missing seizure medication or stopping suddenly
- Not getting enough or “good” sleep
- Stress
- Being sick with another illness or fever
- Flashing lights if photosensitive
Seizure triggers encompass a broad range of factors, and while this list is not exhaustive, it highlights common triggers for children and adults. Missing doses or abruptly discontinuing seizure medication is a frequent trigger, as experienced by my husband. Inadequate or disrupted sleep patterns can also precipitate seizures, underscoring the importance of sufficient rest. Stress, illness, or fevers can exacerbate susceptibility to seizures, as can exposure to flashing lights for those who are photosensitive.
Moreover, sensory stimuli such as touch, light, movement, and sound—including church bells, music, or specific voices—can provoke seizures in some individuals. Patterns, such as those found in moving escalator steps or daily activities like toothbrushing or bathing in hot water, may also trigger them. Specific colors, times of day or night, and hormonal changes associated with menstrual cycles can further contribute to seizure onset. Additionally, substance use, particularly alcohol consumption, and its aftermath, along with menstrual cycles and hormonal fluctuations, may serve as seizure triggers for certain individuals.
Seizure Control
- Understand the details of a child’s medicine:
- What to take, how often, when, and why
- Follow special instructions
- Set a specific time to take the medicine
- Recognize side effects
- Get blood tests
- Track if medicines are working
Effectively managing seizures is crucial for individuals of all ages, necessitating a comprehensive approach that encompasses medication adherence and understanding. It's imperative to meticulously follow the seizure action plan, which delineates the prescribed medication regimen, including dosage, frequency, and rationale. Adherence to any special instructions provided is paramount.
In instances of breakthrough seizures or the need for additional medication, it's essential to establish a specific schedule for administration. Maintaining consistency in the timing of medication intake is critical, ensuring a specified duration between doses. It's also vital to be vigilant in recognizing and addressing any potential side effects associated with the prescribed medications, and regular blood tests are often employed to monitor medication levels in the bloodstream and assess their efficacy.
Keeping a seizure diary can provide valuable insights into seizure frequency, duration, triggers, and medication adherence, facilitating informed discussions with healthcare providers and optimizing treatment strategies. Individuals can enhance seizure control and improve overall quality of life by diligently adhering to medication regimens, monitoring for side effects, and actively engaging in self-management practices such as keeping a seizure diary.
Seizure Medication
- Generally, antiepileptic drugs (AEDs) are in pill form.
- Sometimes more is needed.
- Routes of Delivery
- Nasal sprays
- In the cheek
- Under the tongue
- In the rectum
Anti-epileptic drugs typically come in pill form, but in cases where additional intervention is necessary, alternative routes of delivery may be employed. These include administration via nasal spray, in the cheek (buccal area), under the tongue (sublingually), or in the rectum. These alternative methods are typically utilized when seizures persist despite standard medication regimens and aim to achieve better seizure control.
Caring For a Child With Seizures
- Ensure adequate sleep and a healthy diet
- Have a support system
- Keep your child active
- Monitor how your child is coping
- Keep a seizure diary
- Utilize a Seizure Action Plan
Caring for a child with seizures encompasses various essential aspects that can significantly impact their well-being. Prioritizing adequate sleep and maintaining a healthy diet is fundamental, as nutrition is crucial in managing seizures and overall health. Establishing a robust support system is vital, ensuring that the child remains engaged in activities they enjoy while promoting safety. Active participation and encouragement from caregivers can foster a sense of empowerment and resilience in the child.
Monitoring the child's well-being, both physically and emotionally, is essential. Parents should recognize the stress that may be experienced in managing their child's condition. Regular communication with the child to understand their experiences and concerns is invaluable in providing comprehensive care.
Maintaining a seizure diary facilitates tracking seizure activity and identifying patterns, aiding healthcare providers in treatment adjustments. Utilizing a seizure action plan collaboratively developed with healthcare professionals and the family ensures a coordinated approach to managing seizures and responding effectively in emergency situations. By prioritizing these strategies and fostering open communication, caregivers can better support children with seizures and optimize their quality of life.
When More Help Is Needed
- If seizures are different or more than usual
- Additional medication or treatments prescribed by the healthcare provider
- Can be given by non-medical people outside of the hospital and exactly as prescribed
- You may use rescue therapy for a child known to you if you have been shown how to use it.
- Does not take the place of usual seizure medication
- Additional medication or treatments prescribed by the healthcare provider
When additional assistance is required for managing seizures, it's essential to recognize that supplementary medications may be administered by non-medical personnel outside of a hospital setting, provided a doctor and the administration protocol are thoroughly understood. These medications are typically used when standard seizure medications are insufficient in controlling seizure activity.
Caregivers must comprehend how to correctly use these medications and recognize that they are not intended to replace the individual's regular seizure medication regimen. Rather, they serve as an adjunctive measure for acute seizure management when standard treatments are inadequate. Ensuring that caregivers are well-trained and informed about the proper administration of these medications is paramount in optimizing seizure control and minimizing risks during episodes of increased seizure activity.
Seizure Action Plan
- Emergency contact
- Type of seizure
- How long, how often, what happens
- Specific instructions
- When to call the provider
- When to call 911
- What NOT to do
- Rescue therapy:
- When and What to do
https://www.epilepsy.com/preparedness-safety/action-plans
A seizure action plan is a crucial tool for individuals with epilepsy and their caregivers. It typically includes several things like emergency contact information for healthcare providers, emergency services, and support personnel. It also should have details about the individual's seizures, including type, duration, frequency, and unique characteristics. Clear instructions on responding during a seizure, including administering prescribed medications and any additional rescue therapies, are also added. There should be clear guidance on when to contact the healthcare provider for assistance or further instructions, especially during prolonged or unusual seizure activity. Additionally, there should be criteria for when to call 911, such as prolonged seizures or signs of medical distress. Instructions on actions to avoid during a seizure event, such as restraining the individual or attempting to insert objects into their mouth, should be listed. Lastly, information on the use of rescue therapies to abort prolonged or recurrent seizures, including when and how to administer them.
A seizure action plan empowers individuals and caregivers to respond effectively to seizure events by providing comprehensive guidance, ensuring safety and optimal seizure management.
Mission of the Epilepsy Foundation
- To lead the fight to overcome the challenges of living with epilepsy to accelerate therapies to stop seizures, find cures, and save lives.
The mission of the Epilepsy Foundation is to lead the charge in overcoming the challenges associated with living with epilepsy. They strive to accelerate the development of therapies, ultimately aiming to halt seizures, discover cures, and save lives. For the most accurate, up-to-date, and detailed information on managing seizures, epilepsy, and its impact on individuals and families, I highly recommend visiting the Epilepsy Foundation. They offer comprehensive resources and support to empower individuals affected by epilepsy and their loved ones.
Research Shows...
- Epilepsy is the most common chronic neurological disorder. There is inadequate knowledge, skills, abilities, and misconceptions regarding epilepsy among healthcare providers that contribute to poor patient outcomes.
(Amoudi, Nairat, & Shawahna, 2021)
Increasing awareness and understanding of epilepsy is crucial, especially among healthcare providers. Research, such as that conducted by Amoudi, Nairat, & Shawahna, underscores the significance of addressing inadequate knowledge, skills, and misconceptions surrounding epilepsy within the healthcare community. By enhancing healthcare providers' knowledge and proficiency in managing epilepsy, we can significantly improve patient outcomes and ensure their safety and well-being.
I hope today has given you some essential knowledge and skills to effectively care for clients with epilepsy. Together, we can work towards fostering a more inclusive and supportive environment for individuals living with epilepsy, ultimately enhancing their quality of life and overall healthcare experience. If there's anything specific you'd like to learn or discuss regarding epilepsy management, please let me know!
What Is Epilepsy?
- A neurological disease that causes individuals to have recurrent unprovoked seizures
- 30% of children diagnosed continue to have repeated seizures into adulthood
- 70% of children diagnosed can improve over time
- Is a developmental disability if it starts before age 18
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures. According to the Mayo Clinic, epilepsy is diagnosed when an individual experiences two or more seizures at least 24 hours apart without any identifiable cause. It's worth noting that while some individuals may experience seizures only during childhood, around 30% of children diagnosed with epilepsy continue to have recurring seizures into adulthood. However, there's a positive aspect as well: approximately 70% of individuals with epilepsy experience improvement over time.
Additionally, if epilepsy onset occurs before the age of 18, there's a significantly elevated risk of associated developmental disabilities. This highlights the importance of early detection and intervention in managing epilepsy, particularly in pediatric populations, to mitigate potential long-term impacts on development and quality of life.
Epilepsy Stats
- 65 million people worldwide
- 3.4 million people in the U.S.
- 150,000 new cases each year
- 470,000 children and youth in the U.S.
- It can affect ANYONE.
- It is a syndrome associated with other health problems (cognitive, neurological, and psychiatric).
- Associated with learning difficulties and psychological and social problems
Epilepsy is a significant global health concern, affecting millions of individuals worldwide. According to statistics, approximately 65 million people worldwide experience epilepsy, with around 3.4 million affected in the United States alone. Each year, approximately 150,000 new cases of epilepsy are diagnosed.
Among those impacted by epilepsy, children and youth represent a significant portion, with almost half a million affected individuals in the United States. It's important to recognize that epilepsy can affect anyone, regardless of age, gender, or background.
Seizures do not just characterize epilepsy; it is often associated with a range of other health issues. These may include cognitive problems, neurological issues, and psychiatric disorders, all of which can contribute to the occurrence of seizures and the overall impact of epilepsy on an individual's life. Learning difficulties, psychological challenges, and social problems are common among individuals living with epilepsy.
The emotional toll of epilepsy diagnosis and management should not be underestimated. Newly diagnosed individuals may experience various emotions, including fear, sadness, shock, worry, and anger. Lifestyle changes, such as driving restrictions or participation in certain activities, can further exacerbate these feelings. Moreover, individuals may struggle with disclosing their condition to others, leading to feelings of isolation and embarrassment.
The cumulative effect of these challenges can contribute to anxiety and depression, leading to additional social and emotional difficulties. Therefore, it is essential to provide comprehensive support to individuals living with epilepsy, addressing not only their medical needs but also their emotional well-being and social integration.
Research Also Shows...
- Understanding parental and client knowledge, attitudes, and perceptions of epilepsy is a key step to address any social and cultural barriers towards epilepsy. Therapeutic relationships rely on identifying and overcoming these barriers to improve the chances of adherence and compliance with the treatment plan
(Rani & Thomas, 2019).
Understanding the knowledge, attitudes, and perceptions of epilepsy held by both parents and clients is crucial for addressing social and cultural barriers associated with the condition. Rani and Thomas's research highlights that therapeutic relationships between healthcare providers and clients rely on identifying and overcoming these barriers to enhance adherence and compliance with the treatment plan.
Empowering patients and their families with a comprehensive understanding of epilepsy not only fosters better treatment adherence but also facilitates informed decision-making and self-management. Healthcare providers play a vital role in assisting patients and families in navigating the complexities of epilepsy management, addressing their concerns, and providing support across various aspects of care.
By establishing open communication, fostering trust, and tailoring interventions to individual needs, healthcare providers can effectively support patients and families in managing epilepsy. This includes providing education about the condition, addressing misconceptions, offering practical strategies for seizure management, and addressing psychosocial concerns.
Common Causes of Epilepsy
- For many, the cause is unknown!
- Brain trauma
- Brain tumors
- Brain infections
- Brain injury at birth
- Changes in brain development
- Stroke
- Genetics
The common causes of epilepsy for many, the cause is unknown, and that is very troubling for individuals. Brain trauma again, tumors, infections in the brain, brain injury at birth, changes in brain development, stroke, and genetics are all common causes of epilepsy.
Types of Epilepsy
- Temporal Epilepsy- occur in the temporal lobes responsible for learning and memory
- Intractable Epilepsy- when a person’s seizures fail to come under control with treatment
- Reflex Epilepsy- when specific triggers bring on seizures
- Psychomotor Epilepsy- limited to the temporal lobe of the brain and results in impairment of responsiveness and awareness to one’s surroundings
- Photosensitive Epilepsy- when seizures are triggered by flashing lights or contrasting light and dark patterns
- Post-traumatic Epilepsy- is a recurrent disorder resulting from injury to the brain
Here is a list of different types of epilepsy, and I have links to all of these different types where you can find more information.
Temporal epilepsy occurs in the temporal lobes responsible for learning and memory.
Intractable epilepsy is a serious condition when a person's seizures fail to come under control with treatment, either with medication or all the other options that we'll talk about later.
Reflex epilepsy occurs when specific triggers bring on seizures that can be any of those things like tastes, smells, sounds, and lights.
Psychomotor epilepsy is also limited to the temporal lobe of the brain and results in impairment of responsiveness and awareness to a person's surroundings.
Photosensitive epilepsy is caused by flashing lights and contrasting light and dark patterns.
Post-traumatic epilepsy is a recurrent disorder resulting from a brain injury.
This is not an all-inclusive list. There are many types of epilepsy syndromes, some very specific. You can get more information about epilepsy at the Epilepsy Foundation.
Diagnosing Epilepsy
- By a medical professional
- No specific test is used.
- Blood tests
- Imaging tests
- (EEG) Brain wave testing
- Vital Information:
- Patient and Family Medical History
- Detailed description of the seizures
When a medical professional diagnoses epilepsy, no specific test is used. Blood tests, imaging tests, EEGs (electroencephalogram), or brainwave testing can be used. Vital information, though, is a key part of diagnosing epilepsy, which the patient and family provide. It is crucial to have a comprehensive medical history and a detailed description of the seizures when they happen, and what happens.
Status Epilepticus
- Status Epilepticus is a seizure that won’t stop after several minutes.
- Seizure > 30 min or repeated w/o return to normal
- Most common in children < 2 yrs. of age w/ history of tonic-clonic seizures.
- Suspicion of a status epileptic event requires emergency 911 response.
Status epilepticus is a situation where a seizure does not stop after several minutes, lasts more than 30 minutes, or involves repeated seizures without the person returning to normal consciousness. A seizure lasting more than five minutes is also considered status epilepticus, requiring immediate medical intervention. This condition is most common in children under two years of age who have a history of tonic-clonic seizures, making them particularly at risk for status epilepticus events. If there is any suspicion of a status epilepticus event, calling 911 is absolutely essential to ensure prompt medical attention.
Epilepsy Treatments
- Goals:
- Achieving complete seizure control
- Preserving Quality of Life (QOL)
- Avoidance of adverse events
- Treatments:
- Antiepileptic Drugs (AEDs)
- Epilepsy surgery
- Implanted stimulation devices
- Medically prescribed diet
- Complementary and Alternative Medicine (CAM)
Epilepsy treatments aim to achieve complete seizure control, preserve the patient's quality of life, and avoid any adverse events. The primary treatments include antiepileptic drugs, brain surgery, implanted stimulation devices, medically prescribed diets, and complementary and alternative medicine strategies.
Antiepileptic drugs are often the first line of treatment and work to prevent seizures. For some patients, brain surgery may be an option if the seizures originate from a specific, identifiable area of the brain that can be safely removed. Implanted stimulation devices, such as vagus nerve stimulators or responsive neurostimulation systems, can help control seizures by sending electrical impulses to the brain. Medically prescribed diets, like the ketogenic diet, have also been shown to reduce seizures in some patients.
Complementary and alternative medicine strategies are also considered. Complementary medicine refers to practices outside mainstream medicine used alongside biomedical treatments. Examples include acupuncture, aromatherapy, meditation, mindfulness, and herbal remedies. These practices aim to complement traditional treatments, potentially enhancing their effectiveness or helping manage side effects and overall well-being.
In contrast, alternative medicine involves using these types of interventions instead of traditional biomedical treatments. This approach forgoes conventional medical practices in favor of alternative methods entirely.
It’s important to distinguish between these two approaches. Complementary medicine is used in conjunction with traditional treatments to support overall health and well-being, while alternative medicine is used as a substitute for traditional biomedical treatments. We'll discuss specific, well-researched complementary interventions in more detail later.
Antiepileptic Drugs (AEDs)
- Introduced in 1857
- Anti-seizure drugs alone control seizures in only 2 out of 3 people.
- Drug levels monitored
- Watch for side effects
- It takes weeks to months to adjust.
- More than one medication may be needed
Antiepileptic drugs were introduced in the 1850s and remain a cornerstone of epilepsy treatment. However, these drugs control seizures in only about two out of three people. The levels of these medications in the blood are closely monitored through regular blood tests to ensure they are within a therapeutic range and to watch for potential side effects. Urine tests are also conducted to see how the body is reacting to the medicine.
Adjusting to seizure medication can be a lengthy and challenging process, often taking weeks or months. This period can be frustrating and difficult for both individuals with epilepsy and their families as they work to find the right medication and dosage. Sometimes, more than one medication is necessary to achieve optimal seizure control.
- Research Shows
- Drug-resistant epilepsy affects all aspects of daily living. Occupational therapy programs with drama activities helped build the body/mind connection of persons with epilepsy and positively affected the Quality of Life in persons with epilepsy (Pinelopi, Aikaterini, Anna, Alexandrina, Theofanis, Konstantinos, & Ioannis, 2022).
Research indicates that drug-resistant epilepsy significantly impacts all aspects of daily living. In a study by Pinelopi et al., occupational therapy programs incorporating drama activities were developed to help individuals with epilepsy build a body-mind connection, ultimately improving their quality of life. This study involved groups of individuals with epilepsy participating in various drama activities, highlighting the importance of emotions, feelings, communication, expression, and body participation in the well-being process.
The strategies used in these programs included both nonverbal and verbal expressions, recognizing that some people with epilepsy have difficulty communicating verbally. Techniques such as storytelling, improvisation, body movement, and voice work were employed. The study found that participants experienced reduced anxiety during seizures, an improvement in their sense of emotional well-being, and a newfound energy. These outcomes were significant and demonstrated the positive impact of incorporating creative and expressive therapies into the treatment and support of individuals with epilepsy.
Epilepsy Surgery/Implantation Stimulation Devices
- Surgery may be done to remove a part of the brain where seizures occur
- They are complex.
- Not an option for everyone
- Vagus Nerve Stimulation (VNS)
- Small battery placed in the chest- A magnet is held over the battery to activate small energy pulses to the brain.
- For 12 yrs. and older with uncontrolled seizures
Epilepsy surgery and the implantation of stimulation devices represent potential options for managing uncontrollable or intractable seizures. These measures are often considered last-ditch efforts when other treatments have failed. Surgery may involve removing a part of the brain where seizures originate, but it is complex and not suitable for everyone.
One specific device used in such cases is the vagus nerve stimulation (VNS) device, which I frequently encountered in pediatric and rehabilitation settings. This device involves implanting a small battery in the chest. When a child feels a seizure coming on, they can activate the device by holding a magnet over the battery, which sends impulses to help control the seizure.
However, the use of such implantation devices can lead to side effects, including a hoarse voice, throat pain, and changes in the sound or tone of the voice. These devices are typically used for children aged twelve and older who suffer from uncontrolled seizures.
Ketogenic Diet (KD)
- Used to treat epilepsy since the 1920s
- High fat/low carbohydrate diet
- Strictly followed diet
- Creates ketones in the body
- The brain and heart work normally with ketones for energy.
- Inhibits neurotransmission, reducing seizure frequency
- Studies have shown that some children become seizure free when using this diet.
The ketogenic diet has been used to treat epilepsy since the 1920s and remains a proven method for managing the condition. The Epilepsy Foundation notes this high-fat, low-carbohydrate diet as one of the oldest and most effective dietary treatments. It can reduce seizures by 50% or more in half of those who try it and may also allow for lower doses of medication.
The ketogenic diet is highly specific and requires careful adherence, including precise food weighing. Unlike carbohydrates, it produces ketones in the body, which the brain and heart can use effectively for energy. Ketones help inhibit neurotransmission, thus reducing the frequency of seizures. Some studies have shown that certain children can become seizure-free on this diet.
Other diets can also benefit individuals with epilepsy, although they are generally less complex than the ketogenic diet. The Modified Atkins Diet (MAD) limits carbohydrates to about 20 grams daily and encourages fat intake without specific meal plans. The low glycemic index diet focuses on consuming whole grains and berries while avoiding high-glycemic foods like white flour and sugar. This diet tends to be easier for teens and adults to manage.
Another alternative is the medium-chain triglyceride (MCT) diet, which emphasizes the use of MCT oil and allows for a higher carbohydrate intake than the traditional ketogenic diet.
It is crucial to approach the cessation of these diets carefully. Abruptly stopping can lead to significant issues, so weaning off the diet gradually over a few weeks is generally recommended to prevent any adverse effects.
Cannabidiol (CBD)
- CBD is the non-psychoactive component of marijuana and has anecdotal and scientific evidence of its usefulness.
- Several studies surveyed parents on a Facebook group and online internet surveys that used CBD to treat their children’s seizures.
- Overall, approximately 80% of parents reported a reduction in seizure frequency.
- On average, over 14% reported a positive effect, and their child became seizure-free.
There are other situations where EEGs are given to me before stopping a diet to make sure it is safe to try cannabidiol or CBD. This is something that my husband takes if he feels a seizure coming on, and it has actually been able to manage his seizures. He's also on a seizure medication. An antiepileptic, CBD is a non-psychoactive component of marijuana, and it has much anecdotal and scientific evidence of its usefulness.
Now, a little history on CBD. There are historical records from ancient times in 2700 BC and from the Sumerian and Akkadian people written on their clay tablets in 1800 BC on the use of cannabidiol. In the 19th century, several leading physicians published papers on its use as an anticonvulsant. It turns out the Marijuana Tax Act of 1937 led to the removal of cannabis from all pharmacies. However, researchers and physicians renewed their investigation with purified cannabidiol in the 1970s.
Over the last decade, several studies have surveyed patients on a Facebook group and in online internet surveys who use CBD to treat their children's seizures. Family advocacy groups, social media, and the internet—all of that has led to significant interest in CBD from myself and others. In this particular study, overall, approximately 80% of patients reported a reduction in seizure frequency when using CBD. On average, over 14% reported a positive effect and said their child became seizure-free.
Mindfulness-Based Therapy
- 80% of children with epilepsy have cognitive and mental health disorders, and 50% of parents are at risk for depression.
- Family environment has a greater influence on QOL and mental health than epilepsy-related issues.
- Making Mindfulness Matter (M3)
- Children 4-10 years of age and families
- An online program can benefit individual’s QOL and mental health
- Interventions must be implemented early.
- Can be a low-cost intervention and sustainable with the help of epilepsy support centers
(Tang, Poon, & Kwan, 2015)
In addition to cannabidiol (CBD), mindfulness-based therapy is another complementary intervention that can potentially benefit children with epilepsy and their families. It's important to note that around 80% of children with epilepsy face cognitive, medical, and mental health challenges, with 50% being at risk for depression.
Interestingly, research has shown that the family environment has a more significant influence on quality of life and mental health than epilepsy-related issues themselves. The "Making Mindfulness Matter" study, conducted over three years, targeted children aged four to ten years and their families. The program aimed to help kids manage stress and worries through education and group meetings, regulate emotions and behavior, improve focus and optimism, and enhance empathy and compassion.
Uniquely, the study also helped parents understand the brain's functioning and its relationship with emotions and behavior. It taught strategies for parents to calm themselves when upset and respond appropriately to their children's intense emotions related to their epilepsy. Additionally, the program included activities to promote self-regulation in children, foster appreciation for positive parent-child experiences, and exercises to express gratitude and kindness within the family.
The results showed that this mindfulness-based intervention benefited the participating families' quality of life and mental health. The researchers emphasized the importance of implementing such interventions early, as they can be low-cost and sustainable with the support of epilepsy centers, which are widely available across the United States through organizations like the Epilepsy Foundation.
Mindfulness, including practices like mindfulness meditation, forms the foundation of this intervention program. It aims to provide families with tools and strategies to better manage the emotional and behavioral challenges associated with epilepsy, ultimately improving their overall well-being.
Challenges For Individuals and Families Living With Epilepsy
- Side Effects
- Other Health Problems
- Emotional/Social
- Insurance, Finances, Housing
- Stigma, Discrimination, Fear
- Caregiver Stress
- Isolation, Work, Driving, Play
Individuals and families living with epilepsy face a multitude of challenges that extend far beyond the seizures themselves. The medications used to manage epilepsy can have significant side effects, including drowsiness, gastrointestinal discomfort, dizziness, and blurred vision. Cognitive impairments, such as reduced psychomotor speed, are also potential side effects of these medications. Consequently, it is crucial that these drugs are initiated at low doses and gradually increased to minimize adverse effects.
Beyond the medical ramifications, epilepsy can contribute to emotional and social issues, with behavior problems being more prevalent among children with the condition compared to their neurotypical peers. The financial burden associated with epilepsy treatment is substantial, encompassing not only the costs of medications but also potential housing accommodations and other expenses, which can strain financial resources even with insurance coverage.
For adults with epilepsy, securing appropriate housing that meets their needs can be a significant challenge. Across all age groups, individuals with epilepsy face stigma, discrimination, and fear stemming from misinformation and misconceptions about the condition. This can manifest in rejection, teasing, and bullying, with children being particularly cruel regarding perceived differences.
The stress levels experienced by both individuals with epilepsy and their caregivers are elevated. Self-isolation and disengagement from beloved activities, such as work, driving, or recreational pursuits, may occur due to the limitations imposed by the condition. The emotional, social, and financial tolls of epilepsy permeate nearly every aspect of daily living for those affected and their families.
Overall, while the medical management of seizures is a primary concern, the broader implications of epilepsy on quality of life, mental health, and overall well-being cannot be overlooked. A comprehensive approach that addresses the multifaceted challenges these individuals face and their support systems is necessary to improve their overall life experiences.
Parents’ Challenges
- 42% reported high levels of depression
- 31% reported high levels of anger
- 77% admitted their social life was disturbed due to their child’s epilepsy
- Economic burden reported:
- 96% from drug costs
- 83% from doctor’s fees
- 22% from hospitalizations
According to the World Health Organization, the profound impacts of epilepsy on families, especially parents of children with the condition, are evident. Alarmingly, 42% of parents reported experiencing high levels of depression, likely stemming from the constant stress and challenges associated with managing their child's epilepsy. Furthermore, 31% of parents admitted to experiencing high levels of anger, an understandable emotional response given the difficulties they face. A staggering 77% acknowledged that their social lives were significantly disrupted due to their child's epilepsy, as prioritizing care and accommodating the unpredictable nature of seizures became paramount.
The economic burden shouldered by families affected by epilepsy is also substantial. Medications, doctors' fees, and hospitalizations (with 22% reporting costs from hospitalizations) create a financial strain for many. The World Health Organization emphasizes that epilepsy's impact extends far beyond the individual patient, profoundly affecting family members, especially parents who may grapple with feelings of depression, frustration, guilt, and helplessness as they strive to provide care for their child.
The guilt of having a child afflicted with such a condition, coupled with the helplessness of being unable to fully control or cure it, takes an immense emotional toll on parents. Epilepsy disrupts family dynamics, psychological well-being, social engagement, and financial stability in significant ways. Addressing these broader psychosocial and economic impacts is crucial for improving the overall quality of life for those affected by this condition.
Strategies for Parents
- In common sense, intuition and experience can guide caring for a child with seizures.
- Research the condition
- Remain positive
- Avoid being overprotective
- Be open and honest with friends and family
When caring for a child with epilepsy, parents can rely on common sense strategies and intuition, as they inherently know their children best. Personal experience serves as an invaluable guide in this situation. Researching the condition from reputable sources and remaining positive are critical first steps.
However, it is important for parents to avoid becoming overprotective, as excessive restrictions can lead to a loss of self-esteem and behavioral problems in children. Striking a balance between providing appropriate care and fostering independence is essential for the child's overall well-being.
Furthermore, parents and caregivers must prioritize their needs by finding opportunities for respite and time away when possible. Being open and honest with friends and family about their challenges can alleviate stress and provide a crucial support system.
Maintaining open communication about the condition helps manage expectations and fosters a sense of understanding and empathy from loved ones. Ultimately, a combination of research, positivity, reasonable protective measures, self-care, and open communication can empower parents to provide the best possible care for their child with epilepsy while also tending to their own emotional and psychological needs.
Tips For All Caregivers
- Bullying by peers can occur due to a lack of understanding.
- A child may not be able to assert himself.
- Signs: temper tantrums, violence, truancy, or nervousness
- Communicate with the child’s parent/caregiver or teacher
- Support and encourage the child
It's important not to assume that epilepsy is the sole cause of behavioral problems. Learning difficulties and concerning behaviors may stem from the severity or type of seizures the child experiences, potential brain damage, or even side effects from certain medications used to treat epilepsy. Caregivers, especially teachers, should seek professional guidance to determine the underlying causes.
Bullying by peers can unfortunately occur due to a lack of understanding about epilepsy. Some children may adapt and cope better than others when facing such challenges. However, children often do not openly share their experiences with bullying, which underscores the importance for families to maintain open communication with their children. Parents may find bedtime routines an opportunity for children to feel comfortable opening up.
For children who struggle to assert themselves, teaching them language to explain their condition to friends or classmates could be invaluable. Bullying can manifest in various ways - temper tantrums, violence, school avoidance in younger children, or nervousness in older children. Maintaining communication between the child's parents, caregivers, and teachers is crucial so everyone is aware of potential issues.
Promoting a supportive environment by distributing seizure action plans, akin to asthma action plans, and consistently encouraging the child can make a significant positive impact. Overall, a multifaceted approach involving professional assessment, open communication, peer education, and a nurturing support system is vital for caregivers to effectively address any behavioral concerns in children with epilepsy.
Resources
Where Can I Learn More About Epilepsy?
- Visit www.epilepsy.com
- Call Epilepsy Foundation Hotline@1-800-332-1000
- Contact your local epilepsy foundation
- Become Seizure Recognition and First Aid Certified
Call the hotline or contact a local epilepsy foundation. Become seizure recognition and first aid certified, as it is very easy to do. Finally, direct your clients to these resources.
Lifestyle Redesign® for Epilepsy
- Living with epilepsy impacts the physical, emotional, and mental well-being of the individual. This guide describes the ways OTs can promote health-promoting habits and routines for individuals with epilepsy.
- (H. Chan, USC Chan Division of Occupational Science and Occupational Therapy)
The Lifestyle Redesign® program, developed at the University of Southern California, provides a valuable guide for occupational therapists to promote health-promoting habits in their patients and clients. This approach is particularly relevant for individuals with epilepsy, as the condition can lead to withdrawal from meaningful roles, routines, and activities despite a desire to participate.
This program allows occupational therapists to incorporate interventions specifically tailored to managing epilepsy. These include identifying and managing seizure triggers, recognizing and addressing stress, anxiety, and depression, and developing and maintaining restorative sleep routines, which are crucial for individuals with epilepsy and seizure disorders.
Additionally, occupational therapists can assist in improving medication management routines, promoting family involvement in these routines, enhancing time management and organizational skills, and teaching assertive communication strategies. Implementing pacing and energy conservation techniques and increasing participation in community activities can create a balanced lifestyle encompassing productivity, rest, and leisure.
The Lifestyle Redesign® program offers a comprehensive framework for occupational therapists to support individuals with epilepsy in various aspects of their daily lives. Through the development of health-promoting habits and routines, the program ultimately promotes better seizure management, mental health, and overall well-being.
Quick Links
- Temporal lobe epilepsy
- Reflex epilepsy
- Psychomotor epilepsy
- Intractable epilepsy
- Photosensitive epilepsy
- Traumatic epilepsy
Here are the quick links I mentioned about some of the different types of epilepsy.
Quick Links/Resources
https://www.stanfordchildrens.org/en/service/epilepsy
https://learn.epilepsy.com/courses/schools-and-seizure-preparedness-on-demand
https://chan.usc.edu/patient-care/faculty-practice/epilepsy
https://www.epilepsy.com/tools-resources/forms resources#Epilepsy-Foundation-Toolbox
https://www.epilepsy.com/tools-resources/forms-resources - More-Helpful-Resources
Here are more resources that you can click on and go to for the USC information.
Summary
Hopefully, we met the learning outcomes today. We will now proceed with the exam poll.
1)What is a general symptom or warning sign of a seizure?
It is all of the above. Excellent.
2)What is TRUE about seizures?
The correct answer is that they may not know they are having a seizure. They are not always medical emergencies and are not contagious. Additionally, a person would never swallow their tongue during a seizure.
3)What is a risk related to seizures?
All of those things can occur with a seizure.
4)What are the three basic principles of seizure first aid?
The answer is stay, safe, and side.
5)What should you do if someone is having a seizure?
The correct answer is c. You should stay with them.
Thank you for participating in the poll. I want to thank you so much for being with me today. Please reach out if you have questions.
Questions and Answers
Is verbal aggression a sign or a symptom of a seizure? In my TBI practice, we have had that in several cases.
I think that is part of a brain injury versus a seizure.
Are seizures more common in those born prematurely?
Premature babies may have developmental difficulties or delays that could increase their risk for seizures. I don't have specific statistics on premature babies, just infants.
Have you worked with clients who have myoclonus with a seizure disorder?
No, I have not.
Have there been any links between seizures and vaccines, like increased seizure occurrence with a growing vaccine schedule?
I am not aware of any link between the two. There is a lot of misinformation on the internet.
Have there been links between seizures and chemicals in our food?
That is a very interesting question. I am a holistic practitioner, and my husband's a naturopath, and we definitely teach about, you know, organics and pesticides and all of that and how that can really affect you. I don't know that there is anything specific that is related to pesticides and seizure activity. Keep in mind that pesticides, hormones, and things of that nature can make your body acidic. And, in acidic bodies, disease can proliferate. I am unsure if there is any literature to support this concerning seizures. In my practice, I teach about all different types of holistic care and self-care.
Nutrition is always the game changer, and that's the hardest thing for people to do.
What activities should adults with epilepsy avoid?
That is going to be dependent on each individual, how their epilepsy is managed, what happens during their epileptic event, and if they are well controlled.
I appreciate all of your time today.
References
Amoudi, M., Nairat, Q., & Shawahna, R. (2021). Knowledge, attitudes, and practices of physiotherapists with regard to epilepsy and patients with epilepsy: A systematic scoping review. Epilepsy & Behavior, 124, 108367.
Ben-Zeev, B. (2020). Medical cannabis for intractable epilepsy in childhood: A review. Rambam Maimonides medical journal, 11(1).
Detrick, A. (2021). Complementary and alternative medicine (CAM) for individuals with epilepsy.
Elliott, J., DeJean, D., Clifford, T., Coyle, D., Potter, B., Skidmore, B., ... & Wells, G. A. (2018). Cannabis for pediatric epilepsy: Protocol for a living systematic review. Systematic reviews, 7(1), 1-5.
Hussain, M. M., Zulfiqar, Z., Ishfaq, K., & Ghaffari, A. S. (2021). Psycho-social and economic problems faced by parent’s of children with epilepsy. Review of Education, Administration & LAW, 4(2), 521-530.
Iannone, L. F., Roberti, R., Arena, G., Mammone, S., Pulitano, P., De Sarro, G., ... & Russo, E. (2021). Assessing knowledge and attitudes toward epilepsy among schoolteachers and students: Implications for inclusion and safety in the educational system. PloS one, 16(4), e0249681.
Laino, D., Mencaroni, E., & Esposito, S. (2018). Management of pediatric febrile seizures. International journal of environmental research and public health, 15(10), 2232.
Lowman, D. K., Simons, D. F., Shepherd, J. T., Fiocca, J. T., Ernouf, H. S., & Hundley, B. S. (1999). Occupational therapists in the school setting: Working with students with complex health care needs. The American Journal of Occupational Therapy, 53(5), 519-523.
Nicholson, C., Edwards, M. J., Carson, A. J., Gardiner, P., Golder, D., Hayward, K., ... & Stone, J. (2020). Occupational therapy consensus recommendations for functional neurological disorder. Journal of Neurology, Neurosurgery & Psychiatry, 91(10), 1037-1045.
Pinelopi, V., Aikaterini, T., Anna, T., Alexandrina, N., Theofanis, V., Konstantinos, V., & Ioannis, H. (2022). Changes in the quality of life of persons with epilepsy, after the implementation of an occupational therapy intervention with drama activities Epilepsy & Behavior, 130, 108694.
Rani, A., & Thomas, P. T. (2019). Parental knowledge, attitude, and perception about epilepsy and sociocultural barriers to treatment. Journal of epilepsy research, 9(1), 65.
Sourbron, J., Klinkenberg, S., van Kuijk, S. M., Lagae, L., Lambrechts, D., Braakman, H. M., & Majoie, M. (2020). Ketogenic diet for the treatment of pediatric epilepsy: review and meta-analysis. Child's Nervous System, 36(6), 1099-1109.
Tang, V., Poon, W. S., & Kwan, P. (2015). Mindfulness-based therapy for drug-resistant epilepsy: an assessor-blinded randomized trial. Neurology, 85(13), 1100-1107.
Citation
Nathenson, N. (2024). Understanding seizures and epilepsy in the occupational therapy setting. OccupationalTherapy.com, Article 5706. Available at www.occupationaltherapy.com
