Introduction
Thank you to OccupationalTherapy.com for having me back. I do a lot of research and training, but I am a clinician first. I know how valuable your time is today and am grateful that you all have chosen to spend some of it with me.
International Center for Spinal Cord Injury
- At Kennedy Krieger Institute, Baltimore, MD
- 50 therapists
- Continuum of care
As Fawn mentioned, I work at the Kennedy Krieger Institute in Baltimore, Maryland. Figure 1 is a picture of our outpatient facility.

Figure 1. The outpatient facility at Kennedy Krieger Institute.
We have about 50 therapists across both inpatient and outpatient programs. Our programs serve only patients with spinal cord injury. We see about 1000 unique patients a year with both acute and chronic spinal cord injuries. Kennedy Krieger as a whole sees a variety of diagnoses involving the brain and spinal cord and the nervous system as a whole. My experience and what I will talk about today is spinal cord injury.
The Spinal Cord Following Injury
We will start with a little recap of spinal cord injury and everyone's favorite subject, neuroanatomy. This is your spinal cord following injury in Figure 2.
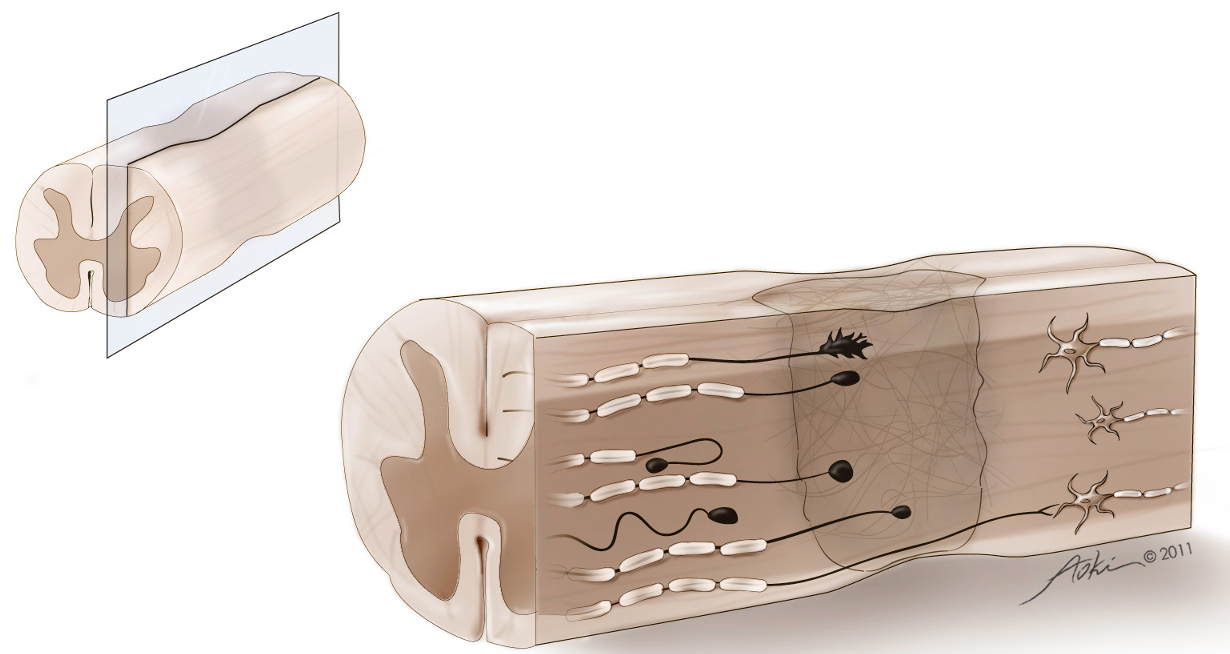
Figure 2. Cross-section of the spinal column showing an area of injury.
Looking at this illustration, imagine the head on the left side of the screen. This is a cross-section of the injury. Within the damage zone, you can see stalled axons or axons that cannot grow through this area. There is cavitation that over time fills in with fluid and is surrounded by a glial scar. These both are mechanical barriers to recovery.
Some axons are demyelinated. Both stalled axons and demyelinated axons represent a conduction block. The information cannot get from the brain to the muscles. We know that the spinal cord, unlike the brain where things are centralized, has segmental innervation.
Levels of Innervation
Depending on the level of injury, there will be different muscles involved. Figure 3 is a schematic of the spinal cord and levels of innervation.
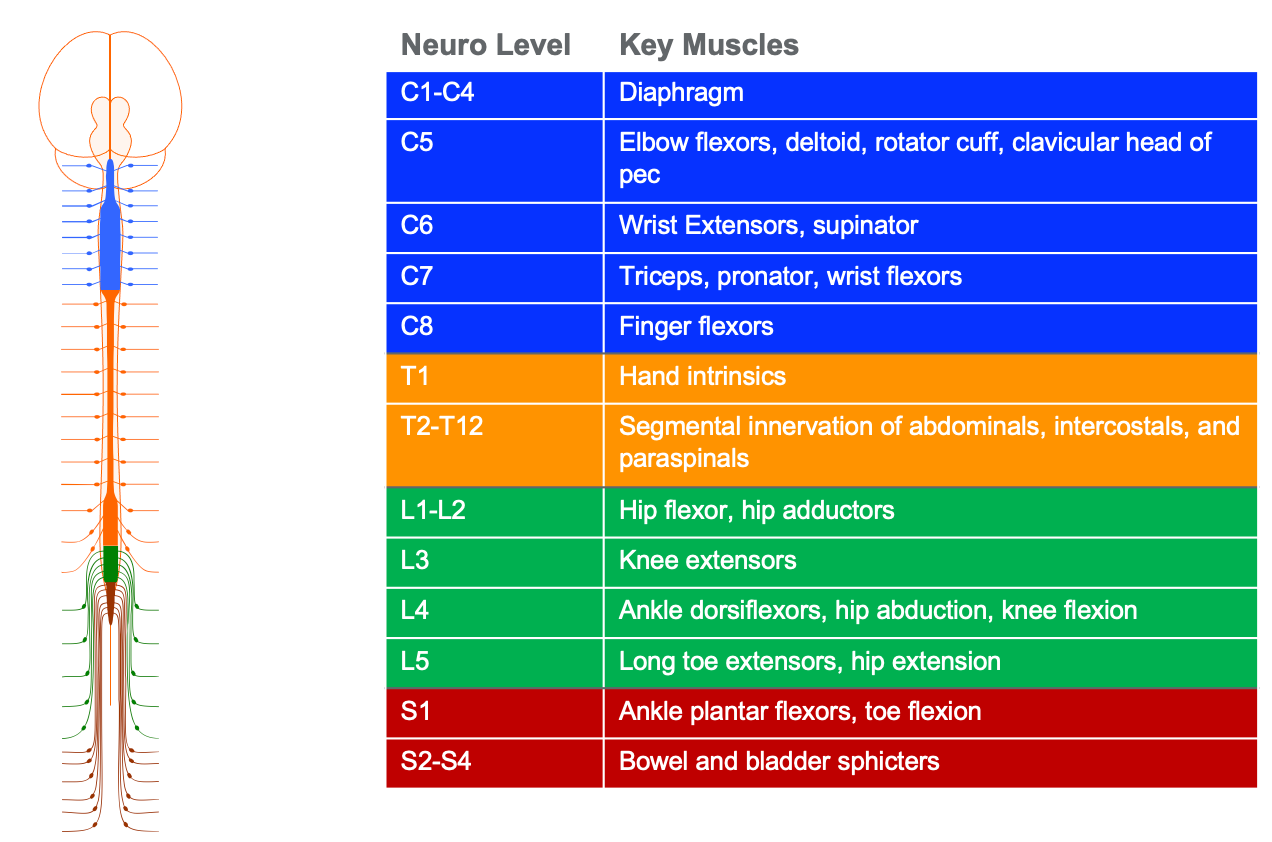
Figure 3. Levels of innervation. Click here to enlarge the image.
There are eight cervical levels of innervation, which we will focus on today as this is where all of the information for the hand and upper extremity are contained. There is segmental innervation of the abdominals, intercostals. and paraspinals through the thoracic spine. Then, the lower extremity musculature is innervated by the lumbar and sacral segments of the spinal cord.
SCI Facts and Figures
How big is this problem?
My husband jokes that "I know everybody in a wheelchair" in a 50-mile radius. Depending on their practice area, many therapists will only see one or two spinal cord injuries a year, and maybe less.
- 17,900 new injuries per year
- 296,000 people living with SCI in the US
It is important to understand the scope of the problem. There are about seven, almost 18,000 new injuries per year in the US. And 296,000 people are living in the US with a spinal cord injury.
We can break this down and look at the level of the lesion. Both incomplete tetraplegia and incomplete paraplegia make up the bulk of nearly two-thirds of injuries.
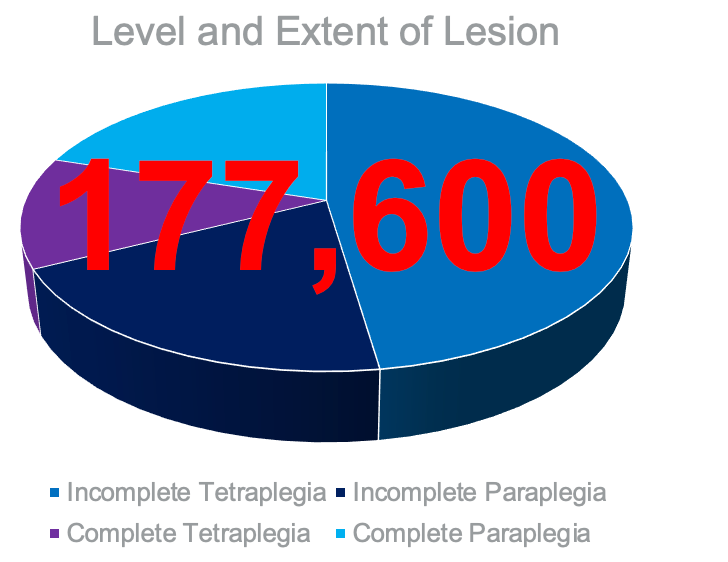
Figure 4. Pie chart showing the level and extent of the lesions (https://www.nscisc.uab.edu/Public/Facts and Figures - 2021.pdf).
Incomplete tetraplegia is the most common injury level, and then complete tetraplegia and complete paraplegic being the other third of our injury levels. Incomplete tetraplegic means some involvement of all four limbs and some hand and upper extremity dysfunction. They are also likely to have some difficulty walking if they can walk at all. In total, about 177,600 patients are living with some form of tetraplegia. This is why we need to examine what we are offering our patients, and how we can help them.
We need to keep in mind that patients with spinal cord injury are living longer. In Figure 5, you can see that although ages 16 to 25 are the most common ages when injuries occur, ages 40 to 49 are the most common ages for people living with spinal cord injury.
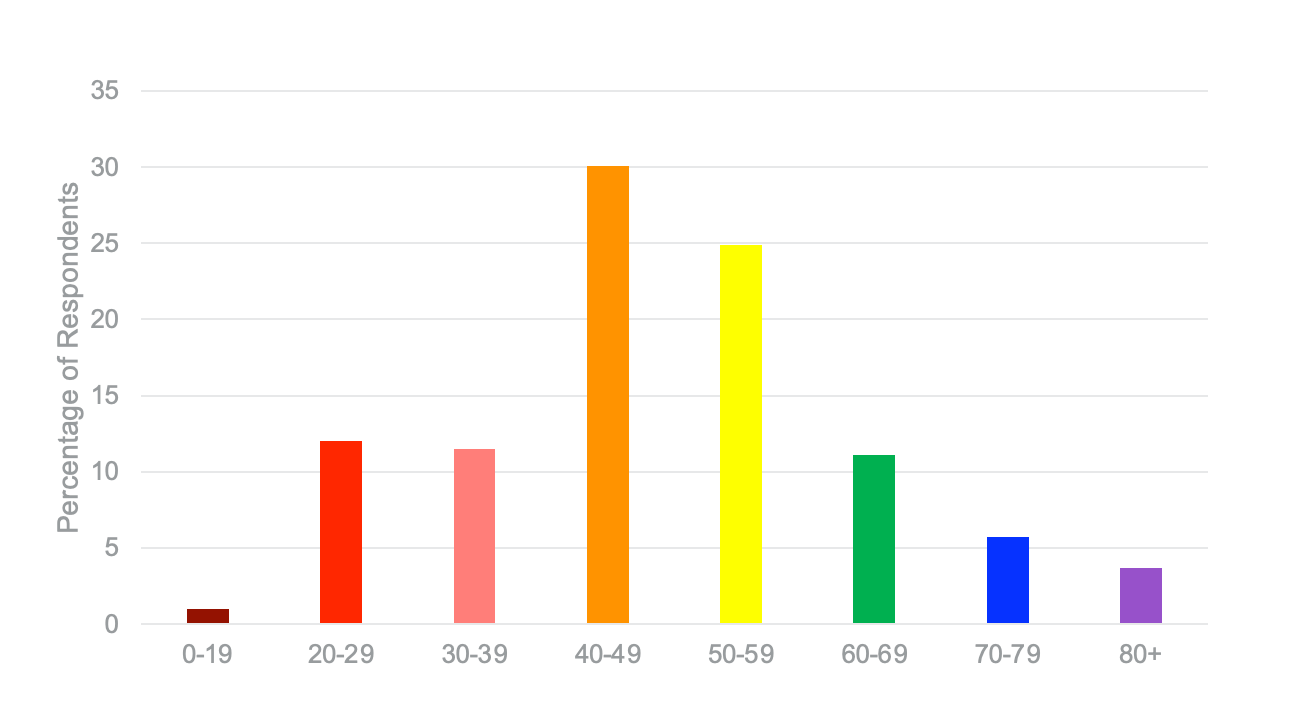
Figure 5. Bar graph showing ages of people living with SCI (http://www.christopherreeve.org/site/c.mtKZKgMWKwG/b.5184255/k.6D74/Prevalence_of_Paralysis.htm).
People are living longer, and they need more help as they get older. This shift is happening.
SCI Levels
While we are on the topic of neuroanatomy, I want to review the cervical levels of innervation to make sure that we are all on the same page as we look at the options for patients.
Level C1-C4
- Relevant Muscles Innervated
- Upper trapezius
- Cervical paraspinals
- Neck accessories
- Diaphragm at C4
- Probable movements
- Neck flexion, extension, rotation
- Scapular elevation, shoulder shrug
- Problems
- No movement in trunk, LE, UE
- Ventilator dependent, low respiratory reserve
First, we have patients who have injuries in C1 to C4 or the highest level of injury possible. C1 is basically referred to as an internal decapitation. This is where the individual's brain is separated from their spinal cord, while the vertebrae, muscles, and the skin that contain the spinal cord remain intact. There is just an internal break. These patients will have a preserved upper traps, cervical paraspinals, and neck accessories. Patients at C4 will have use of their diaphragm. Remember, C4 or C5 keep the diaphragm alive. This is the level at which patients can start to breathe on their own. Patients from C1 to C4 will need some sort of respiratory support, depending on the severity and completeness of their injury. They will also need support for the rest of their body, trunk, and extremities.
These patients will probably have neck flexion, extension, and rotation. They will also have scapular elevation and shoulder shrug, but that is about it. They will have no movement in their trunk, lower extremities, or upper extremities. They most likely will be ventilator dependent and have a low respiratory reserve. As I said, they will need some support in respiration.
According to the Paralyzed Veterans Administration, expected outcomes for these levels are in the chart in Figure 6.
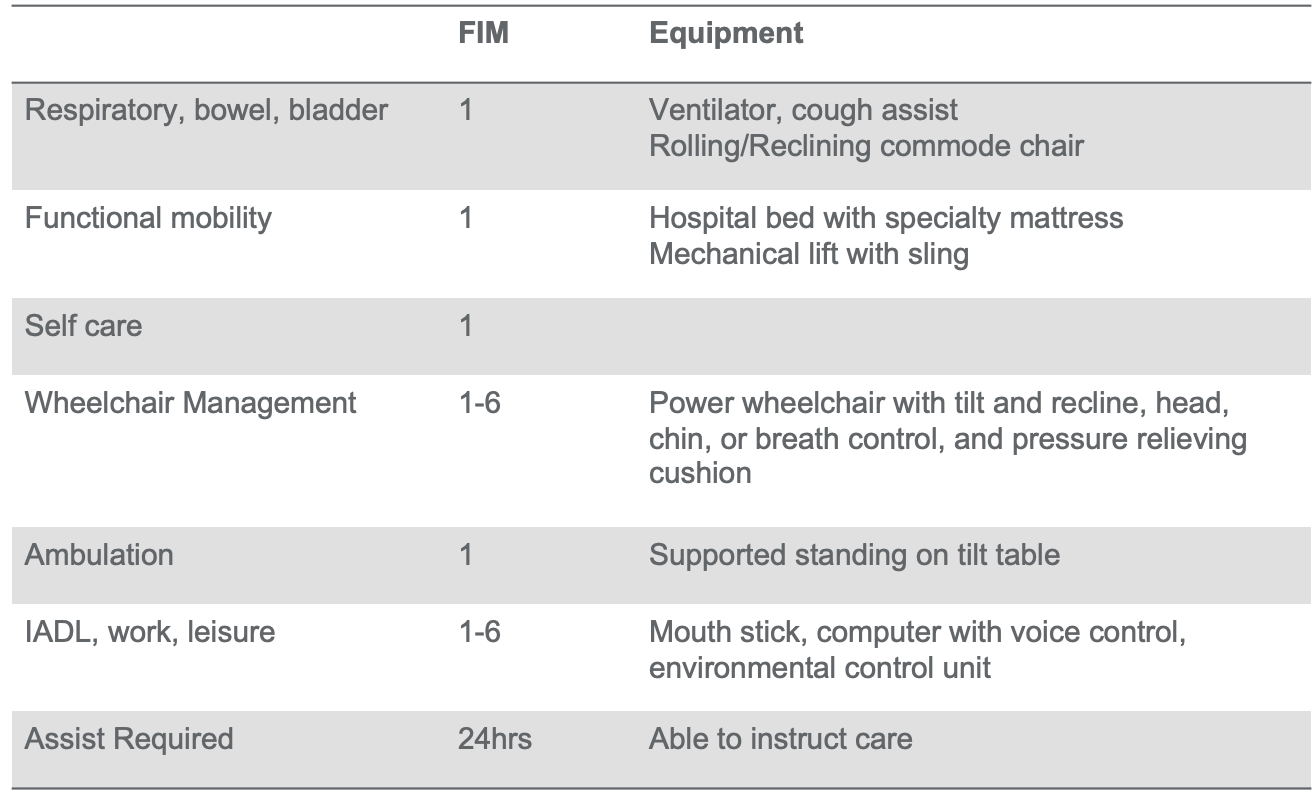
Figure 6. Chart of expected outcomes for a client with an SCI Level C1-C4. Click here to enlarge the image.
This is what a patient with a complete injury at this level can expect long-term. However, I am also going to say that our patients generally are capable of more. This is the maximum level what they are going to need. These patients will be dependent for their respiratory, bowel, and bladder care. They will be dependent for their functional mobility like rolling, transfers, and coming to sit. They will be dependent for all of their self-care activities. They may depend on the style of their wheelchair, achieve some independence with wheelchair management and mobility. Wheelchair driving may be controlled using a sip and puff, a head array, or a chin controller. These patients will require supported standing on a tilt table. They may also achieve some independence in IADLs, work, and leisure tasks using technology. They are likely going to need 24 hours a day of assistance.
Level C5
- Relevant Muscles Innervated
- Deltoid
- Elbow flexors
- Rhomboids and serratus anterior
- Probable movements
- Shoulder flexion, abduction, extension
- Elbow flexion and supination
- Scapular abduction and adduction
- Problems
- No movement in the trunk, LE
- No elbow extension, pronation, scapular depression, wrist or hand movements
Patients at the C5 level of injury will have everything they had before with the C1-C4 levels, but now they will also use their deltoids, elbow flexors, rhomboids, and serratus anteriors. Now, we start to see more function in their upper extremity. They can now do shoulder flexion, abduction, extension, elbow flexion, supination as driven by the bicep, and scapular abduction and adduction. They can bring their hands up towards their mouth through elbow flexion, but they still have no grip, no wrist stability, and no way of extending their elbow.
You can see expected outcomes in Figure 7 (Source: Paralyzed Veterans Association).
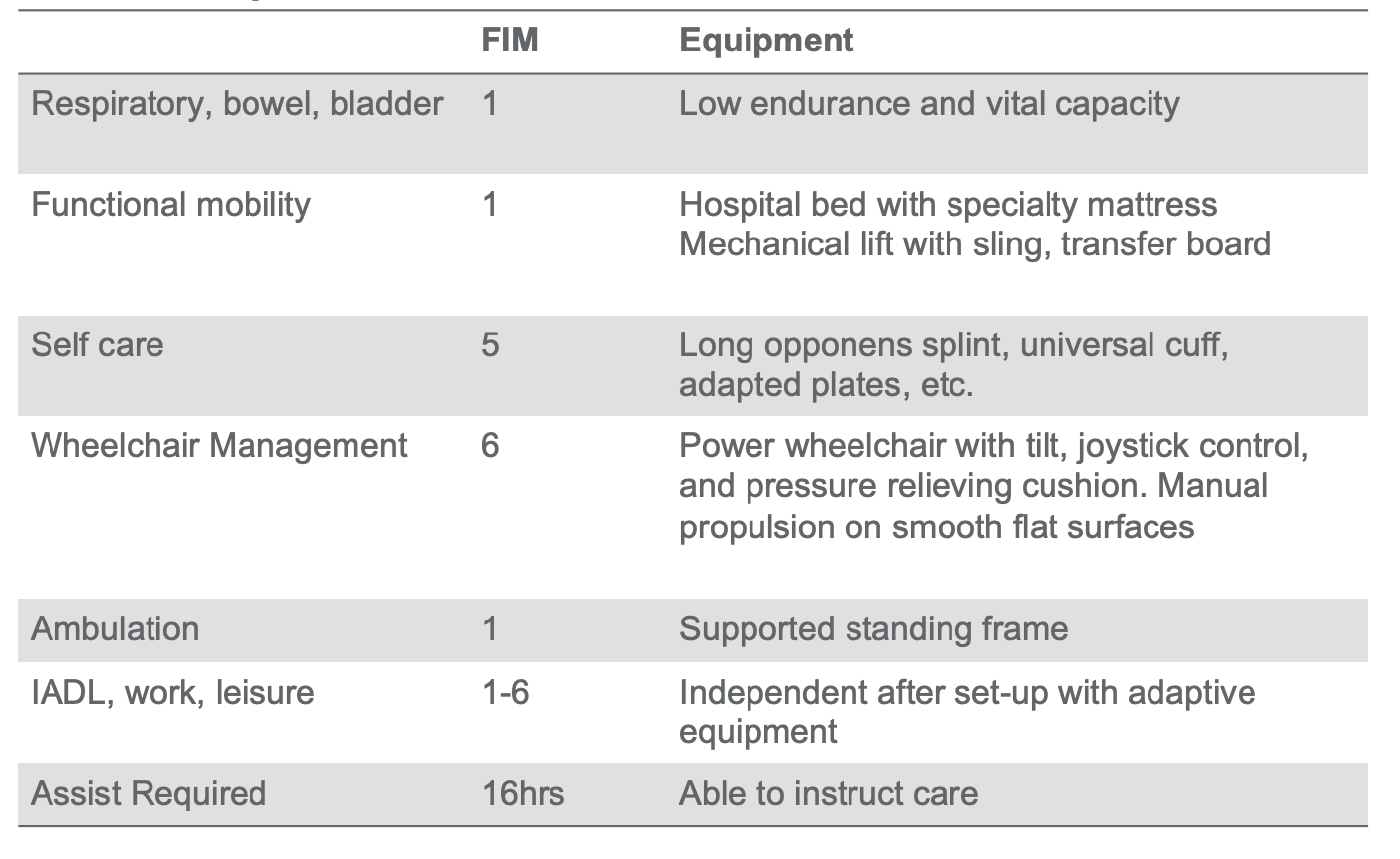
Figure 7. Chart of expected outcomes for a client with an SCI Level C5. Click here to enlarge the image.
These patients will still be dependent for bowel and bladder function, but they can now breathe independently. They will have low endurance and vital capacity. These patients will still be mostly dependent for functional mobility, transfers, coming to sit, and rolling in bed. With some adaptive equipment and strategies, they can achieve independence in some self-care tasks. We often have what we call the "super quads," or now called "super tetras." These are patients who can roll, go from supine to sit and get dressed. However, it is still energy expensive for them to do these activities, so they do not do them often. These patients are likely to be in a power wheelchair, but they can manage them on their own for the most part. With adaptive equipment, they may have some level of independence in IADL, work, and leisure activities. They can instruct their care, but they probably need care for most of their awake hours.
Level C6-C8
- Relevant Muscles Innervated
- Pectoralis
- ECRB and ECRL
- Latissimus dorsi
- Triceps, FCR, FDP, FDS, Extensor communis at C7
- Lumbricals and hypothenar at C8
- Probable movements
- Shoulder horizontal adduction
- Wrist extension
- Wrist and finger flexion, finger extension
- Finger abduction, adduction, and lateral pinch
- Problems
- No movement in the trunk, LE
- Limited dexterity
These patients will add in the following muscles: pectoralis, extensor carpi radialis brevis, extensor carpi radialis longus, and latissimus dorsi. At C7, they get triceps, flexor carpi radialis, flexor digitorum profundus, flexor digitorum superficialis, and extensor communis. These are all a big deal. In fact, C7 is a game-changer. Then at C8, they get lumbricals and hypothenars. At the C8 level, they have a pretty complete upper extremity function. They are missing some intrinsic function as they are innervated at T1, but for the most part, they can do everything they want to do with their upper extremities. They now have shoulder horizontal abduction, wrist extension, wrist flexion, finger flexion, finger extension, finger abduction, finger adduction, lateral pinch, and elbow extension. These are all a big deal.
You can see expected outcomes in Figure 8.
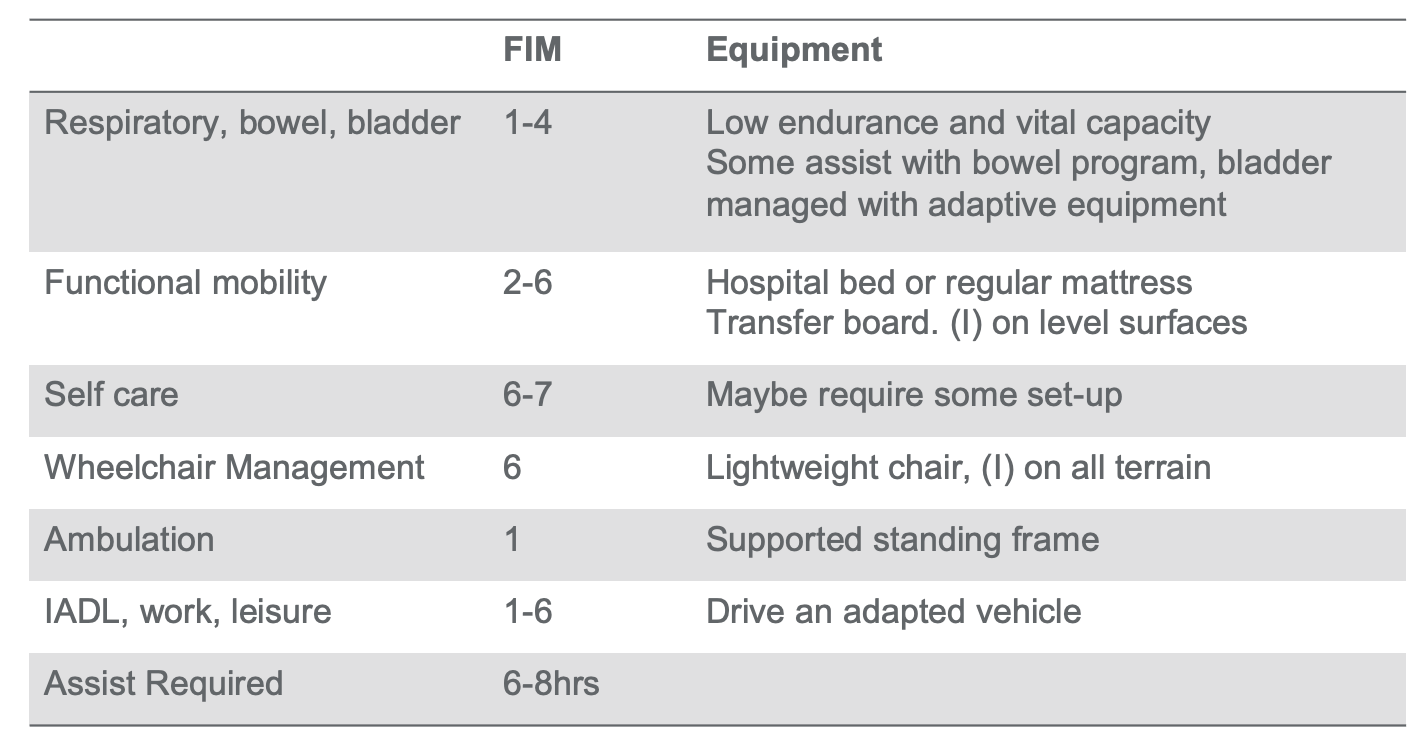
Figure 8. Chart of expected outcomes for a client with an SCI Level C6-C8. Click here to enlarge the image.
Now, they can reach workspaces that are much higher due to elbow extension. They can also manipulate things like tying laces, doing buckles/buttons, and all of those sorts of things. They can cut their own food and have the strength to grip a full glass of something. They no longer have to use long straws. There is a significant change in a patient's quality of life at this level. They are still going to be missing trunk and lower extremity function and some fine motor dexterity.
They start to become much more independent as they move into the six and seven-level range. These patients are likely to manage their own bowel and bladder function through catheterization and bowel programs. They are also likely to get in and out of bed on their own and transfer. They may be able to drive themselves with an adaptive vehicle.
These patients are likely to be in a manual wheelchair, representing a much wider access because now they do not always need ramps. They can pop a wheelie to get up a curb and get into somebody else's car (or their own) because they can transfer into it and fold up their wheelchair. These patients may need some level of assistance during the day, but mostly this has to do with efficiency and energy conservation and less to do with needing somebody to do their care.
I point all of this out to show that even just a little bit of change in their neurological level, in terms of the muscles they have available, makes a big difference in their functional level.
Therapy
Our first line of defense as therapists is always therapy. I mentioned patients are living longer. They are young when they start, but they want to stay more involved and engaged in their lives as they age. There is this shift happening from traditional models of rehab into these more activity-based models of rehab. If this is an area of interest for you, I have lots of courses and papers on this topic because I feel really passionate.
Repetitions in Traditional Rehab (Lang et al., 2009)
- 312 therapy sessions in post-stroke rehab
Average duration (min) | 36 |
UE (functional movement) | 32 |
LE (functional movement) | 6 |
Gait (steps) | 357 |
Transfers | 11 |
Catherine Lang from Washington University in St. Louis did a study several years ago where she watched 312 therapy sessions in post-stroke rehab. Some of you probably work in this environment and know what it is to see these patients. You know what you are doing to get their three hours a day of therapy in to get them home safely. I have worked in this setting. So, I was shocked when I read this. In a 60-minute session, patients are getting on average 36 minutes of therapy. It is not very much. If the session's goal was upper extremity functional movement, patients were only doing 32 repetitions or less than one rep per minute. I get it. Mrs. Jones needs her medication or has to go to the bathroom. You have to convince her to get out of bed and then find her slippers. Then, she is not wearing pants. I get what happens in a therapy session that starts to eat away at your time. For my PT friends, repetitions for lower extremities (gait and transfers) are so low.
- Not enough
- “Amount of practice…is small compared with animal models…Current doses…during rehabilitation are not adequate to drive neural reorganization needed to promote function poststroke optimally.”
These repetitions are just not enough to drive change in the nervous system. We are not giving our patients enough input to make changes in their nervous system. Thus, they are not going to recover or make changes. We might teach them to be more independent or give them some strategies with their skills, but it is not enough to sustain them and make changes.
Feasibility in In-patient Rehab (Waddell et al., 2014)
- 15 pts. with UE paralysis s/p CVA in IRF
- 4 days/week of individually tailored UE training
- Ex: lifting cans to a shelf
- Reaching, grasping, manipulating, releasing
- >/=300 reps in 60 min
- 2 days/week of ADL training
(Waddell et al., 2014)
Catherine Lang's group did a follow-up. This builds on a lot of the work that I do in high-intensity activity. She looked at 15 patients with upper extremity paralysis in the same post-stroke inpatient rehab facility. Four days a week, the patients got individually tailored upper extremity training. These were things like lifting cans to a shelf, reaching, grasping, manipulating, and releasing. The goal was to do 300 repetitions in 60 minutes. Now you will remember, we are going from 32 to 300. This is a big change. Patients were still getting two days a week of ADL training.
- Massed Practice Does Not Inhibit Skill Acquisition
- 289 repetitions/session; 47 min engaged
- Fatigue was a complaint, pain was not
- Sessions were not often missed
- Improvements in ARAT, grip/pinch strength, UE-FIM
- Pts with various UE capacities could participate
- Higher doses were associated with better outcomes
- ADL retraining was not sacrificed.
They found that mass practice did not inhibit skill acquisition. Patients did not quite get 360 minutes, but they did get 289 repetitions and were engaged for 47 minutes. The duration of time from 36 to 47 is not significant, but the intensity of the activity from 32 reps to 289 is very significant. This is the kind of input that the nervous system needs to push change. Surprisingly, fatigue was a complaint (as you would expect), but pain was not. We often worry about overuse injuries and taxing these patients, but the truth is that the patients are capable of more than what we are doing right now.
Patients improved the Action Research Arm Test, which looks at things like strength and range of motion. They also made statistically significant improvements in grip, pinch, and in the upper extremity sections of the FIM. Their FIM score changes were equal to their counterparts who were getting traditional rehab. So, higher doses were associated with better outcomes, and ADL retraining was not sacrificed. You have to get somebody ready to go home. They have to be independent and safe. This is your priority. What I am telling you is that it is possible to do both. In fact, we are sometimes sort of shortsighted in rehab. If we are only looking at the few weeks that a patient is with us and the changes they need to make to go home and be safe, we may miss the potential for more long-term recovery.
Might Take Longer for the UE (Lo et al., 2010)
- 127 pts with mod-to-severe UE impairment, >6 mos post CVA
- Intensive robotic-assisted therapy (RA)
- Intensive therapist-assisted therapy (TA)
- Usual care (UC)
- Outcomes: Fugl-Meyer Assessment, Wolf Motor Function Test, Stroke Impact Scale
- At 12 wks, RA was better than UC but worse than TA. No significant differences
- At 36 wks, RA and TA were significantly better than the UC
This was a study from the University of Washington in Seattle. They looked at patients now and then in outpatient. They got them safe and discharged to home, but now they needed more upper extremity function. These patients were divided into robotic-assisted therapy, therapist-assisted therapy, and usual care (UC) with low-intensity interventions. They found that at 12 weeks, the robotic-assisted therapy was better than the usual care but not as good as the therapist-assisted therapy. So, yay for therapy and high intensity.
Then at 36 weeks, patients did their 12 weeks of therapy and got 36 more weeks at home. The patients who got high-intensity interventions were much better than the usual care. Patients gained small incremental component level skills like a little bit of grip or pinch. They were then able to use those skills to do more at home. This is a feedback system. The grip and pinch got stronger because they were using it more at home. As they can do more, it gets stronger. This is unlike patients who get usual care. If we teach somebody how to eat with a lip plate and a built-up utensil, they may not even use it all the time as it takes effort to set them up. Caregivers may think it is easier to feed them. This causes them to backslide and get worse.
I have seen this, and I have done this. I get it. What I am telling you is that now we know better. Science has shown us that it is possible and that we can do better. And, when we start to add in these surgical interventions, which we are going to talk about, we can see patients make real and lasting changes in their function. However, it is still not good enough for some patients, and we needed another answer.
Surgical Reconstruction
How do we give patients with spinal cord injury, whose nervous system might not be capable of change and recovery, a little bit of function so that they can do more? So far, I have shown you a way to get a little bit more in those component-level skills. I am not talking about going from max assist dressing to independent dressing. I am talking about whether they have the grip to pull up their pants and shoes or hold a hairbrush, toothbrush, or fork. These little component skills, which start to generalize into all your other ADLs, become essential.
International Classification of Surgery of the Hand in Tetraplegia
- Developed in 1979 (Moberg)
- Describes the number of transferable muscles
- Does not include triceps, which are recorded separately
- Also records sensibility, 2pt discrimination of thumb and index pulpa
- >10mm= Occular (O)
- <10mm= Cutaneous (OCu)
We will first discuss how patients are classified and what options are available to them at different levels. The International Classification of Surgery of the Hand in Tetraplegia was developed in 1979. It describes the number of transferable muscles. Depending on the completeness of their injury and whether or not they have a lower motor neuron presentation, a C5 level can look different. A client at a C5 level can be flaccid or spastic at their bicep. A C5 also might have great deltoids on one side and not on the other side. Thus, it becomes a little bit trickier. If we are referring them for surgery, we need to know what is available to them. This classification is more sensitive and more specific than the ISNCSCI classifications.
You can see here on the right of your screen how the muscles break down in Figure 9.
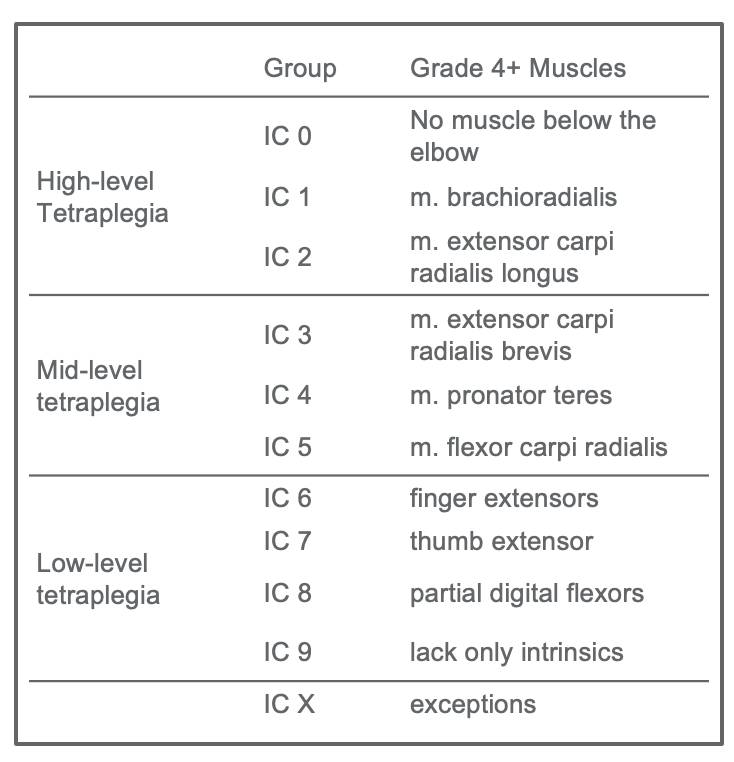
Figure 9. International Classification of Surgery of the Hand in Tetraplegia.
Instead of dividing people into the eight cervical levels, they are divided into these 10 groupings per the international classification. Zero means there are no muscles below the elbow to transfer. Thus, they are not a great candidate for surgery. Whereas if they are one, they have a brachioradialis. For a two, they have extensor carpi radialis longus. As you go through the chart, you can see how the number refers to how many muscles are available at that level. For example, they have finger extensors at level six plus flexor carpi radialis, pronator, ECRP, ECRL, and brachioradialis. You can see how these start to layer in and are more specific than our usual classification.
I do not know if anybody is currently working with surgeons, but they have a different idea than therapists about how things should go. At least, this has been my experience. Excellent surgeons and therapists will recognize that they each bring something to the table and listen to each other to define priorities for patients.
Surgical Hierarchy
- Wrist extension
- Lateral pinch
- Grasp
- Release
According to the International Society for Hand Surgery, there is a hierarchy for reconstruction. The first movement you want to restore is wrist extension. Wrist extension gives you the option for tenodesis and a lateral pinch. This passive flexion of the fingers (tenodesis) can be used to do most things. Last would be active grasp and then active release. You may be thinking, "If they give you this but not this, the balance of the hand is going to be a problem." That is true. In fact, sometimes I find myself having to advocate for a release over an active grasp, particularly if the patient has a lot of spasticity and stiffness in their fingers or a closed hand posture, to begin with. It might be that somebody has an intrinsic minus hand posture, and the release is not as much of a problem because that is the position they want to stay in.
Surgeons always say, "The surgery always wins." If somebody has a lot of shortening, they will go in and do a Z-plasty where they extend the tenodesis while they do the transfers. Or, there might be an option if they move one of the spastic muscles to create more balance if there is tightness in both flexor carpi radialis and flexor carpi ulnaris. If there is flexor tightness at your wrist, they can move the flexor carpi ulnaris to the extensor side to create some balance and then center the radialis. This way, there is more balance at the wrist.
Things to Consider
- Strength and potential excursion of donor
- Maintaining biomechanics of the hand
- Maintenance of action balance
- Long term sequelae
- Patient’s ability to comply with rehabilitation
Therapists and surgeons work together to determine the patient's priorities and what we need to consider in terms of surgical reconstruction. The first thing we want to talk about is the strength and potential excursion of the donor. Muscles generally lose one muscle grade when transferred, although I have seen that come back in patients who work really hard. However, if somebody has only a grade three elbow flexion, taking away one of those elbow flexors to become an extensor is probably not a great choice because they will lose one grade of flexion. There can also be a potential excursion if somebody is really short in their elbow flexors. If they do not have full range, they will not have full range after the transfer either. They might have to combine Z-plasty with either Botox and/or serial casting before the surgery. These are the things that you would talk about in your treatment plan with the surgeon.
Maintaining biomechanics of the hand and action balance is really important to me. Not every surgeon or every therapist will feel the same way. Still, I believe that a simple hand ready for spontaneous movement is ideal, particularly when talking about kids. Kids want to be able to shake hands with grownups, high-five their friends, hold a date's hand, or pick up a glass instead of having to use a straw. So for me, maintaining the action balance and the biomechanics of the hand is really important. I do not want a hand that winds up fisted because all of your transfers have focused on providing grip. They may have no way to release their hand because it is so tight. Even flexion of the wrist should give you passive release. That is something you want to think about.
You also want to look at the long-term sequelae and what the patient will look like down the road. This is especially true if they have a lot of spasticity or limited ability to comply with rehab. These interventions require skilled rehab on the other side. If you have a patient who lives far away, a non-compliant family, or a risk-taker patient, you need to consider this. I had a patient who had a multi-layer reconstruction of his hand because he wanted to go to med school. He recovered grip and pinch via a beautiful series of transfers. Then he decided he would take his wheelchair down a skateboard half-pipe, fell backward, and busted all of his transfers open. This ended up not being a great candidate for the surgery that we had done.
Tendon Transfers
Overview
- Unipolar redirection of a strong, redundant muscle to restore a desired action or balance across a joint
- Examples:
- Biceps to triceps to restore elbow extension
- Brachioradialis to FPL with fusion of thumb IP to restore thumb CMC flexion (lateral pinch)
- Brachioradialis to FDP for grip
- Transposition of ECRB align wrist extension and allow for tenodesis
There are two options for surgical reconstruction. The first is tendon transfers. Tendon transfers are a unipolar redirection of a strong redundant muscle to restore the desired action. For example, three muscles flex the elbow: biceps, brachialis, and brachioradialis. One option for a patient at a C5 level with no active elbow extension is to relocate the insertion of one of those muscles to become a "tricep" and provide elbow extension. The person could lose another muscle at the elbow and transfer brachioradialis to flexor pollicis longus to restore CMC flexion or lateral pinch. Now, we have taken what were three muscles doing one action and separated them. The brachialis maintains elbow flexion, the bicep becomes the elbow extensor, and the brachioradialis is now responsible for the lateral pinch.
Tendon Transfer: Rehabilitation Protocol
- Immobilization: 1-3 weeks post-op, generally cast in desired end range, putting the muscle on slack.
- Mobilization: 3-6 weeks post-op, immobilize at night, protective splinting during the day, increase allowed movement 10-15°/week, no resistive or passive movement, begin edema and scar management, watch for a lag in the desired action
- Strengthening and Functional Retraining: 6-12 weeks post-op, no passive movement before 3 months, continue protective splinting
Here is an overview of the rehabilitation protocol that we will review in detail in a minute.
Reconstructive Options (0-4)
This table (Figure 10) shows the International Classification Levels, likely neurological level, the muscles they have, and what they need.
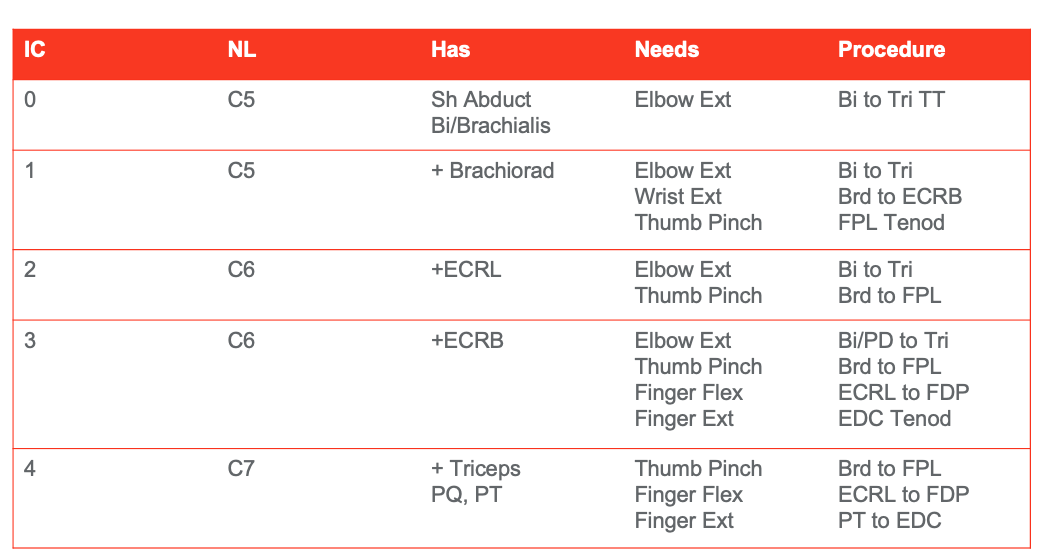
Figure 10. International Classification Level 0-4 options. Click here to enlarge the image.
For example, a patient who has an IC Level 1 is probably a neurological C5. They will have shoulder adduction, biceps, and brachialis but not have elbow extension. As mentioned above, these patients are a good candidate for the biceps to triceps tendon transfer to restore elbow extension. Elbow extension is a big deal because it makes you more independent with transfers, reaching, and functional mobility. My own personal soapbox is that the elbow moves in only one direction (flexion and extension). Moving a muscle in this space does not change the biomechanics of the joint, unlike if you were to do a procedure where all the fingers flex together. "You lose this, but you gain this." It is just a choice. You have to talk it through with your patients and the surgeon, and ultimately, the patient gets to make that decision.
As you start to look through this table, you can see how additional surgical options can be layered in. Patients, for example, who have shoulder abduction, biceps, brachialis, and brachioradialis can now get biceps to triceps and a brachioradialis to ECRB (extensor carpi radialis brevis) or an FPL (flexor pollicis longus) tenodesis transfer. This is when they screw the tendon of the flexor pollicis longus into a carpal bone to tighten up the pinch during wrist extension. There is a combination of things that they can do to change the biomechanics of the hand the more muscles that are added in. It is a long-term trade-off.
Patients at C6 have the addition of ECRL (extensor carpi radialis longus) and ECRB (extensor carpi radialis brevis). The ECRL and ECRB can be used as a flexor digitorum profundus or combined with extensor digitorum communis. Now, we can give patients some additional closure or opening, depending on their original hand posture.
Reconstructive Options (5-9)
Figure 11 is a table of options available for IC levels 5-9.
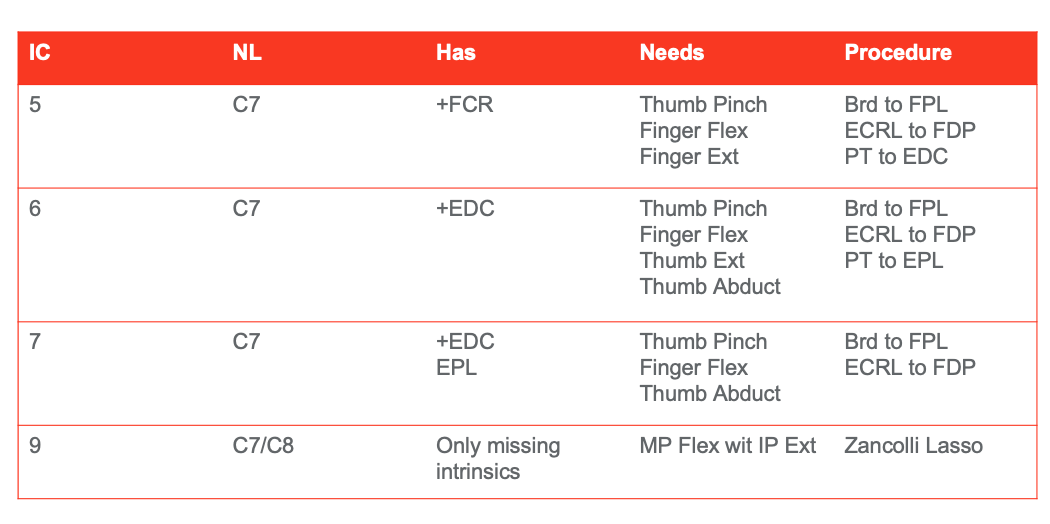
Figure 11. International Classification Level 5-9 options. Click here to enlarge the image.
Somebody at a C7 neurological level may have triceps, pronator quadratus, and pronator teres. These can be used for opening the hand and moving the brachioradialis to the flexor pollicis longus for the addition of a pinch. Patients at an IC level five (that are C7s) also have the addition of flexor carpi radialis. Now, we can do more elegant transfers allowing for some individual finger motions with EDC (extensor digitorum communis) as the donor muscle. Now, they can get greater strength in their flexor digitorum profundus or extensor pollicis longus to differentiate different finger motions.
As we move down the chart, you can see that clients can get more movement and strength in their grip and release all the way down to what they call a Zancolli Lasso procedure in the IC nine level. This is where they take a flexor tendon from the wrist and wrap it around the intrinsics so that it pulls the patient out of that intrinsic minus position (extension at the MCPs and flexion at the IPs). This is difficult to reverse because you have shortening of the collateral ligaments. By pulling forward those intrinsics, you move somebody out of that position for a more useful, normal-looking hand, which is a priority for many patients. Again, you talk through all these options with the surgeons.
Tendon transfers have a pretty well-defined rehab protocol. There is an immobilization phase, where generally, the client is casted, and the muscle that has been transferred is put on slack. For example, let's look at the insertion of the bicep into the tricep. They wrap it around and screw it into the insertion of the tricep. Usually, the tendons are braided together or stitched together, depending on where it is going. In this case, it is inserted into the olecranon so that the bicep will be responsible for elbow extension. The patient is in a cast to put the muscle on slack. You do not want any tension at the site of the co-optation to prevent pulling on the sewn site. Depending on the size of the tendons, the quality of the co-optation, and the patient's age (younger being better), you will move into a mobilization phase somewhere between three and six weeks post-op. A strengthening phase comes later at six to 12 weeks. The key for tendon transfers is to avoid any passive movement before month three because you do not want to put any additional tension on that transfer.
Restoration of Elbow Extension (Mulcahey et al. 2003; Kozin, et al. 2010; Bonds & James, 2009)
- Deltoid to Triceps
- Most frequently used (although losing ground). Higher innervation, more pts will have available.
- Complications:
- Elongation of the tendon s/t early mobilization
- Attenuation
- Graft failure
- Elbow flexion contracture
- Long immobilization phase with demanding rehab
- Biceps to Triceps
- May be a better option, especially if pec is absent. Need to have intact brachialis and supinator.
- Complications:
- Lateral rounding = radial nerve injuries
- Better candidates for early mob—better tendon without external graft
- Graft failure, although less
- Long immobilization with demanding rehab
We are going to talk about post-operative rehab a little more in a little bit. Before that, I want to go over some evidence for the restoration of elbow flexion specifically and generally for tendon transfers. There used to be two approaches, a deltoid to triceps and a bicep to triceps. Depending on the surgeon and location, deltoids to triceps may still be the most common surgery, particularly if the surgeon wants to use the bicep to do something else like an FPL. Also, the deltoid is at a higher innovation thus is more available to somebody with a higher level of injury.
Looking at these two surgeries, they have similar complications. One is that the elongation of a tendon with early mobilization leads to decreased strength over time because you stretch out that tendon. Attenuation or graph failure is where it dissolves or rips apart. You can have elbow flexion contractures that need to be mediated by some sort of additional surgical procedure or Botox plus serial casting. It is important to remember that this immobilization phase can be difficult for caregivers and patients to sustain. This is something you want to think about as you move forward.
Restoration of Elbow Extension (Mulcahey et al., 2003; Kozin et al., 2010)
- Deltoid Outcomes
- Elbow extension was restored
- MMT >3 in 1 out of 8
- No loss of elbow flexion or supination
- Elbow flexion torque loss of -32% at 2 yrs post…not clinically significant
- Improved performance of ADLs and on self-selected goals (COPM)
- Elbow extension was restored
- Biceps Outcomes
- Elbow extension was restored
- MMT >3 in 7 out of 8
- No loss of elbow flexion or supination
- Elbow flexion torque loss of -47% at 2 yrs post…not clinically significant
- Improved performance of ADLs and on self-selected goals (COPM)
- Elbow extension was restored
When we compare their outcomes, the biceps to triceps transfer is slightly superior. This case resulted in a manual muscle test of greater than three in seven out of the eight transfers. In contrast, the deltoid transfer resulted in a manual muscle test greater than three in only one out of the eight transfers. If strength is a problem before then, that is something that you might want to consider. Both sets of patients did not experience any loss of elbow flexion or supination. When you look at the long-term results, neither group lost a lot of flexion torque at the elbow, and both groups improved performance on ADL's and their self-selected goals as measured by the COPM.
Restoration of Elbow Extension: So What?
- Biceps-to-triceps transfers yield better clinical outcomes as compared to deltoid transfers
- Early mobilization
- Maintain integrity at the shoulder
- Better chance of antigravity extension (overhead reaching)
- Good candidates have 4+/5 strength at the biceps, brachialis, and supinator
- Both procedures require diligent rehab
Generally, when we look at the restoration of elbow extension, the bicep is the preferred surgical approach. It has better clinical outcomes and is tolerated more by patients. However, the deltoid may be available to patients who do not have a bicep option.
Nerve Transfers
Nerve Transfer/Grafts
- Transfer of a functional (rostral to the lesion) nerve to a distal irreparable (caudal to lesion) nerve within the “golden period”
- Involves severing of the original nerve, eliminating the chance for “natural” recovery
- Has the potential to innervate more than one muscle, does not change the biomechanics of the joint
- Little to no rehab. Recovery 1cm/month
In nerve transfers, we are transferring a nerve from above the level of the lesion to a distal irreparable nerve during a golden period. Timing is not an issue for tendon transfers. It can be done at any point post-injury. However, timing is an issue for nerve transfers. This is because you want the grafted nerve to reach the neuromuscular junction before the neuromuscular junction has had time to degrade anywhere between six months and 18 months, depending upon the surgeon you talk to. An attendee has asked, "Six months post-injury is not that long, and patients are still changing." You are right, and that is true. This is something that we have to consider when we recommend nerve transfers strongly. The good news is that nerves have the potential to reinnervate more than one muscle group. Thus, you can get a more normal-looking recovery than you can with a tendon transfer.
For a bicep to tricep transfer, the elbow only moves one way. It is going to be fine. However, when we talk about hand transfers like a brachioradialis to an FPL and fuse that IP joint, now we can only do one particular motion. It will look different than normal hand movement. But, if I take a nerve to the flexor pollicis longus, that may innervate other muscle groups to create more movement. It is a different approach that is timing dependent. It is also less of a sure thing than a tendon transfer. A tendon transfer moving a bicep muscle to the triceps will work as it is sewn together. In contrast, taking a musculocutaneous nerve and plugging it into your FPL nerve, this connection has some distance to grow.
Nerves grow at the rate of one centimeter a month, which is the rate at which peripheral nerves recover. This is less of a sure thing. There is also less of a defined postoperative protocol because it is dependent on the growth, the quality of the neuromuscular junction, and the biomechanics of what is available at the joint.
Common Nerve Transfers
Here is a chart outlining common nerve transfers in Figure 12.
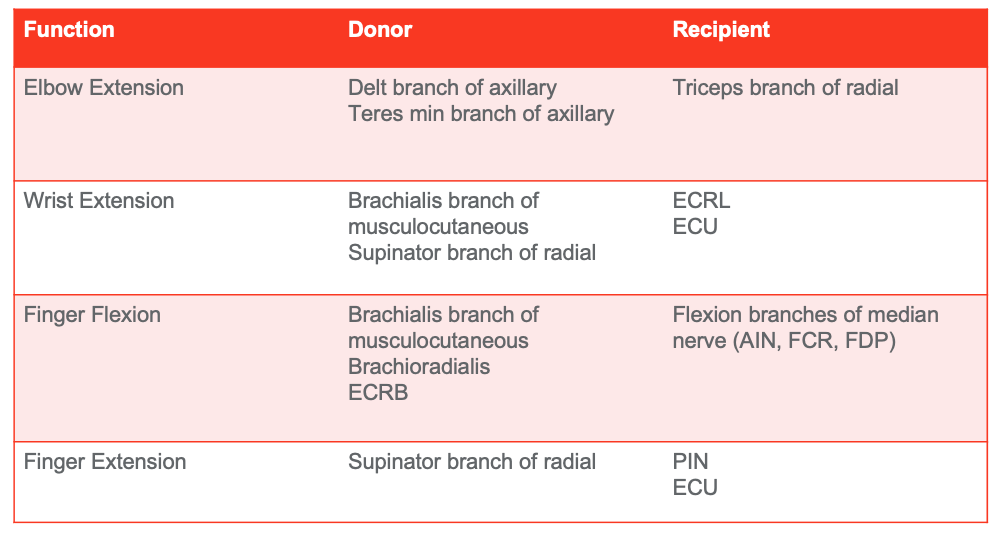
Figure 12. Chart of common nerve transfers based on function, donor, and recipient (Vova & Davidson, 2020). Click here to enlarge the image.
Here are some common nerve transfers to restore particular actions. If we want to restore elbow extension, we have a couple of options. One is the deltoid branch of the axillary to the triceps' nerve. The second is the teres minor branch of the axillary nerve to the triceps' nerve.
To restore wrist extension, we are generally looking at the brachialis branch of the musculocutaneous or the supinator branch of the radial nerve to either ECRL or ECU. In this case, they find the nerve during surgery and separate the different bundles of fascicles. Then they stimulate each of them to see where they are going and what they are doing. When they find the bundles of the musculocutaneous nerve going to the brachialis, they will take one of those to ECRL. Thus, the patient does not lose the donor function. They do not lose the brachialis, unlike in tendon transfers, but there is less surety on the other end knowing if it will actually reinnervate ECRL. Hopefully, that made sense but please ask questions if it did not. Also, I recommend that you Google nerve transfers if you want to see something specific. For instance, you can Google the brachialis branch for the musculocutaneous to ECRL. Use any of these combinations of keywords, and you can pull them up and watch surgeries. Some of these videos will also have pre and post videos of patients' hand functions. I like to show my clients these videos. It is helpful for patients to see it.
We can restore finger flexion with the brachialis branch of the musculocutaneous, the brachioradialis nerve, or this ECRB nerve into the flexion branches of the median nerve. Finger extension is typically restored through the supinator branch of the radial nerve to the posterior interosseous nerve or ECU.
Again, options depend on the patient's injury level and on what the patient has reinnervated. It also depends on timing. If a patient is in the six to 12 months range, this is where you want to have a much more serious conversation with your patient and your surgeon. The other good news is that you could do a nerve early at like six months without any real risk for loss of biomechanics or function down the road. And, you still have options to do tendon transfers down the road, depending on what you have done initially.
Hybrid Procedures
- Bipolar Transfer
- Free Muscle Transfer
- Multi-stage reconstruction
Bipolar Transfers With Microvascular and Nerve Anastomosis
- Transfer of a muscle to another limb location with its blood and nerve supply intact.
- Ex: Rotation of Latisimuss Dorsi to restore elbow extension
- Don’t need to have anything existing (nerve/blood) in deficit location.
- Generally, a bulky muscle is transferred to allow for loss of motor units, but maintain adequate strength.
A bipolar transfer is where they take both ends of the tendon of a muscle and move it to a new space. They can do this with or without the blood supply or the nerve intact. If there is no blood supply and the nerve is not intact, it must be available at the recipient location. For example, they will take two ends of the latissimus dorsi with the blood and nerve supply still intact, and wrap it behind the arm, sort of like reroute it up through the armpit to restore elbow extension. In this case, the nerve and the blood supply remained intact. Usually, they transfer a really bulky muscle into a location like the latissimus dorsi into the elbow extensors to allow for a loss of motor units.
Free Muscle Transfer
- Bipolar transfer of a muscle
- Ex: Gracilis transfer to restore elbow flexion
- Need to have nerve and blood supply available in deficit location
- Used with significant atrophy and suspected degradation of the neuromuscular junction (12-18 months post-injury)
The other option is a free muscle transfer. This is a bipolar transfer of a muscle with nerve and blood supply redirection. For example, they can take the gracilis muscle from a leg (about the size of the biceps), cut off both ends of that, and sew that right on top of the bicep. They also do a nerve transfer as they have taken this from the leg. They may take a lateral pec nerve and place that into the bicep and reroute some blood supply from the original bicep muscle. This free muscle transfer is an option for patients way down the road because the gracilis muscle is not being used. This is pretty risky in terms of outcomes. There are no procedures that I am aware of where they take a donor nerve from somebody else and put it into somebody else's body, even like a cadaver nerve. This is because once a nerve is not being used, then it starts to die. Even if you were to do a nerve graft, where you take two ends of a nerve and move it in, the chances that this takes hold before the neuromuscular junction is available is really low. It is not a great option. However, many people are combining both, the nerve and the tendon transfers, to get optimal outcomes.
Evidence for Nerve and Tendon Transfers
- 10 participants (12 limbs)
- Elbow Extension via teres minor nerve or posterior axillary neve to triceps branch of radial nerve
- Finger/thumb Extension via supinator nerve to the posterior interosseous nerve
- Thumb, index finger, and middle finger flexion via ECRB, brachialis, or supinator nerve to anterior interosseous nerve.
- Some participants had tendon transfers to restore grasp or pinch in one hand to provide two different styles of hand functionality.
- In 3 limbs wrist extension was restored with a brachioradialis to extensor carpi radialis brevis tendon transfer.
(VanZyl et al., 2019)
This study is from Natasha van Zyl, who is in Europe. Again, if you are going to Google people to watch surgery (not during lunch), I would recommend her or Ida Fox. They are my two favorites. All of these are in your reference list. You can look for these articles, and they will have pictures. Some of the articles online will also have a supplemental video, or you can Google these surgeons and watch their surgeries on YouTube.
She had 10 participants for a total of 12 limbs. She looked at elbow extension via the teres minor nerve or the posterior axillary nerve to the tricep branch of the radial nerve. You have to think back to your brachial plexus diagrams. Remember, the radial nerve supplies all of the extensors, but it branches off at different places. So if they plugin either the teres minor nerve or the posterior axillary nerve before the takeoff for the triceps nerve, you get reinnervation of all three heads of the tricep.
They also went after finger and thumb extension via the ECRB, brachialis, or the supinator nerves to the posterior interosseous nerve to the anterior interosseous nerve. Some participants had additional tendon transfers to restore grasp or pinch in one hand to provide two different styles of hand functionality, which is something we do a lot. Perhaps, really early, a client could have a nerve transfer to one hand that looks less functional to see if we can get some restoration there. Then, later on, they have the option to do a tendon transfer in the other hand. I have patients who have a "power" hand because they had a tendon transfer there. They have a precision hand because they had a nerve transfer there. In her study, wrist extension was restored in three limbs with brachioradialis to extensor carpi radialis brevis tendon transfer.
- Nerve + Tendon: Outcomes (24 mos)
- Significant improvements
- ARAT total score (16·5to 34·0, p<0·0001)
- GRT total score (35·0 to125·2, p<0·0001)
- SCIM total score (31.2 to 39.3, >MDC/MCID)
- Strength grades
- Triceps = 3 (IQR 2–3)
- Digital Extension = 4 (IQR 4–4)
- Grip strength
- Distal nerve transfer: 3·2 kg (SD 1·5)
- Proximal nerve transfer: 2·8 kg (3·2)
- Tendon transfer: 3·9 kg (2·4)
She found that at 24 months post-surgery, there were significant improvements in the Action Research Arm Test (ARAT), the Grasp and Release Test (GRT) total score, and the SCIM total score. Patients made improvements in range of motion, strength, and function. They could restore elbow extension via the triceps to a grade three and digital extension/finger extension up to a grade four. There were improvements in grip and strength for all three kinds of surgical interventions (distal nerve transfer, proximal nerve transfer, and tendon transfers).
Role of OT
Poor Rehab Consensus
- Timing
- Intensity
- Immobilization
- Motor retraining
So, maybe I have convinced you. You are going to talk to your surgeons as you have patients in mind. Now, you want to know what your job is. Unfortunately, there is not a great answer because there is poor rehab consensus about these surgeries. There is a lot of variability in the timing, the intensity of therapy, how long immobilization should last, and what motor retraining should be included. I am going to talk to you about today is some data, but I am mostly going to talk about our experience at Kennedy Krieger and the protocols we use with our surgeons.
Pre-operative Phase
- Initiate education in nerve transfer process and phases of rehabilitation
- Strengthening HEP for potential donor muscle groups
- Initiate general education regarding synergistic patterning and visualization exercises
In both nerve and tendon cases, there is a preoperative phase. Your job is to educate the client in the transfer process and the phases of rehabilitation. You want to strengthen potential donor muscle groups and education regarding the synergistic patterns and visualization exercises. The synergistic patterns are super important when it comes to nerve transfers. For example, if we transfer the brachioradialis fascicle of the musculocutaneous nerve to the median nerve for finger and wrist flexion, you will want the client to do elbow flexion, wrist flexion, and finger flexion altogether in your rehab. You want to pair both the donor action and the recipient action together to have them then move towards separating them. We start that education even before they have surgery to get them thinking about that.
Immobilization Phase
- NO PROM proximal to the transfer
- Gentle PROM distal to the transfer only (hand and fingers if not involved)
- Continue with therapy that does not involve the affected UE as directed
- Initiate education with patient regarding synergistic pairings of donor and recipient and include visualization exercises of desired synergistic muscle movements
There is also an immobilization phase for both. It is important not to provide any passive range of motion proximal to the transfer because we do not want to pull it out. Gentle passive range of motion should be provided only distal to the transfer if the hand and the fingers are not involved. You will continue with therapy for the uninvolved parts of the upper extremity or the uninvolved arm if they have only had one side completed.
Splinting for Immobilization
- Sling 90-100deg elbow flexion, cast may be indicated for distal transfers in patients with good proximal strength and stability
- Resting orthosis in intrinsic plus position if hand and fingers are involved
- *Removed 1x/day for bathing and wound care as necessary (incisions sites to not be submerged and immobilized positioning maintained)
There is also splinting during immobilization. Generally, our patients will wear a sling in 90 to 100 degrees of the elbow flexion or are casted if they have good proximal strength and stability. I do not like to put a cast on somebody with an unstable shoulder because it just pulls on that shoulder's nerves and tendons that we are trying to take care of. This is why I often opt for a sling. It is the only time in all my life that I opt for a sling when working with patients with spinal cord injuries. We also put patients in a resting orthosis in an intrinsic plus position if the hand and fingers are involved as we want to maintain the length of these collateral ligaments and put the flexors on slack. This is taken off only once a day for bathing and wound care.
Mobilization Phase (4-8 wks)
- Daily PROM as tolerated, PROM of shoulder limited to 90deg when intercostal/phrenic nerves used as a donor until cleared by a physician.
- Resume weight-bearing positions as tolerated (prone on elbows, walker, etc.)
- Scar management, including desensitization to the surgical site
- Electrical stimulation to the recipient and surrounding musculature
- AAROM of recipient muscle contraction in affected UE within limits of precautions
This is where things get a bit tricky and vary depending on the surgery and the surgeon you have been working with. This is also where the timing starts to diverge for nerve and tendon transfers. Generally, we want daily passive range of motion as tolerated but limited, particularly when their approximal transfer is involved. You can resume weight-bearing positions as tolerated, like prone on elbows and walkers. Isometric contractions are great because you are not going to move through a range of motion. It is going to contract only as much as it is going to contract. We do scar management, including desensitization. We can also start at this point electrical stimulation to the recipient and surrounding musculature. Patients can get an active assistive range of motion of the recipient muscle in the affected upper extremity within the limits of precautions. For a tendon, we still need to protect the co-optation or the area where the tendons were sewn together.
Splinting for Mobilization Phase
- Nerve
- Resting orthosis in intrinsic plus position at night if hand or wrist involvement
- No sling/cast
- Tendon
- Rigid nighttime splinting
- Daytime splinting in a protected range (ex: Bledsoe for elbow)
Generally, they wear rigid nighttime splints, and their daytime splints are in a protected range. For example, they may wear an adjustable orthosis for their elbow and get a defined range of motion each week or every couple of days they will get 10 degrees or so, depending on the size of their tendons during transfer. The nerve option will probably still wear a resting orthosis at night, but they will discontinue their sling or cast during the day. At this point, the nerve is where it will be, and now it just needs to grow. We also diverge later on in the different protocols because, at eight weeks, you should have reanimation via the tendon transfer.
Tendons: Strengthening Phase (8+wks)
- Gradual increases in AROM, no PROM
- Once full AROM AG, can introduce strengthening
- FES may be used once full AROM is achieved
- Splinting to protect coaptation
Patients can now have gradual increases in active range of motion but no passive range of motion. Because again, we do not want to put any stretch on the transfer. Once they have full active range of motion agai
