Editor's note: This text-based course is a transcript of the webinar, Virtual Reality In Brain Injury Rehabilitation, by Jasleen Grewal, Registered Occupational Therapist, PhD Candidate, University of British Columbia, Julia Schmidt, PhD, BSc (Occupational Therapy).
Learning Outcomes
- After this course, participants will be able to identify the components of virtual reality and its use in rehabilitation.
- After this course, participants will be able to recognize how virtual reality can be implemented in neurorehabilitation and identify areas in which virtual reality can improve one's function post-injury.
- After this course, participants will be able to identify the practical and clinical implications of using virtual reality in neurorehabilitation.
Our presentation will focus on implementing virtual reality in neurorehabilitation, specifically in occupational therapy.
Introduction
Jasleen: Before we get into the presentation, here is a quick picture of a virtual reality setup (Figure 1).

Figure 1. Virtual reality setup.
As you can see, there is a person wearing gloves in front of a virtual environment. Do you think something like this can be implemented in therapy? This can be used in treatment, and we will go through different virtual platforms.
What is Virtual Reality?
- "A computer-generated digital environment that can be experienced and interacted with as if that environment was real" (Jerald, 2016)
Before we get into the details of virtual reality and its use in neurorehabilitation, I want to provide a general definition of virtual reality platforms. Virtual reality is a computer-generated digital environment that can be experienced as if the environment is real.
Types of Virtual Reality
- Non-immersive VR
- Semi-immersive VR
- Fully immersive VR
(Ventura et al., 2019)
Non-immersive virtual reality is often overlooked as a virtual reality category because it is so readily used in everyday life. Non-immersive virtual reality platforms have a virtual interface such as a computer or a television screen and input devices such as a keyboard, mouse, or controller. Non-immersive virtual reality platforms allow individuals to control the virtual reality platform, but they also have complete control over their actual environment. An example would be an individual playing a video game.
Semi-immersive virtual reality platforms take it one step further and incorporate things like gloves or goggles. Individuals are more immersed in the virtual environment and feel as if they are in the virtual environment. However, what they are doing physically has no impact on the virtual environment. An example of this would be having a virtual tour of a home.
Fully immersive virtual reality platforms have sensors over the individual's limbs and incorporate both goggles and gloves to create a more immersive experience. The individual feels like they are entirely a part of the virtual environment and have less control over their real environment. They also receive real-time feedback on what they are doing.
Have you guys used virtual reality in your personal life? I have used non-immersive virtual reality platforms but have not delved into semi-immersive or fully immersive virtual reality platforms.
This presentation aims to focus on all different types of virtual reality platforms and how they can be used in neurorehabilitation. Virtual reality in clinical practice has expanded over recent years because technology is becoming more available and advancing very quickly. It can be used in many healthcare areas, such as training healthcare workers. For example, healthcare workers can learn about the human body through virtual cadaver use and the assessment and treatment of patients. Another example is that doctors can perform medical assessments via virtual video platforms.
Virtual Reality in Clinical Practice
- VR has expanded in healthcare
- Training of healthcare workers
- Assessment and treatment of patients (Adamovich et al., 2009).
- Post-traumatic stress disorder, pain management, anxiety and depression, eating disorders, brain injuries
Virtual reality can also be used with various diagnoses, and I have listed a few. Since virtual reality is rapidly evolving into pragmatically usable technology, it can be used to assess and treat individuals in rehabilitation. In a virtual reality system, the complexities of the natural world are simulated in a controlled environment.
Virtual Reality in Rehabilitation
- In rehabilitation, VR has been used to assess and treat (Lee et al., 2003)
Virtual reality provides a rehabilitation environment that allows assessment and the ability for users to repeat the same activities over and over again to increase motivation. Now, I will outline a few examples of how virtual reality has been implemented in research with specific diagnoses and particular environments.
Assessment and Treatment of Mental Health
- Assessment
- Used to assess emotional responses produced by exposure to real food, virtual food, and photographs of food in patients affected by eating disorders (Gorini et al., 2010)
- Treatment
- Treatment of phobias, i.e., fear of heights (Emmelkamp et al., 2001)
Occupational therapists work in various settings, mental health being one of them. Virtual reality has been used to assess individuals experiencing mental health concerns such as eating disorders. In one study, researchers exposed individuals experiencing eating disorders to virtual food, photographs of food, or real food. They found that exposing individuals to virtual and real food elicited the same emotional reaction, and exposing them to virtual food produced more of an emotional response than photographs of food.
In terms of treatment, virtual reality has extensively been researched on phobias in individuals. One study looked at individuals who had a fear of heights. They were exposed either to heights in a real or virtual environment. Individuals exposed to the virtual environment felt more positively towards approaching heights in their everyday lives and had a reduction in anxiety and depression.
Assessment and Treatment of Cognition
- Assessment
- Virtual reality platform to assess attention, decision making, visual processing speed (Horan et al., 2020)
- Treatment
- Virtual reality platforms are used to improve cognitive abilities (visual attention, visuospatial memory) in stroke patients (Kim et al., 2011)
Virtual reality has also been used to assess and treat individuals with brain injuries or neurological concerns. I have briefly outlined how virtual reality can assess and treat cognition, but I will provide more examples throughout the presentation. Researchers developed a cognitive virtual reality assessment battery for assessment that had individuals complete cognitive exercises while in a horse racing environment. They found that this was an excellent way to assess attention, decision-making, and visual processing speed.
For treatment, a study was done with stroke patients who either received traditional rehabilitation or were given rehabilitation via a virtual reality platform. They had sensors over their limbs as well as gloves and a headset. They found that the individuals who took part in the virtual reality therapy improved visual attention and visual-spatial memory.
Assessment and Treatment of Physical Abilities
- Assessment
- Virtual reality platform to assess upper limb function (Gagnon et al., 2014)
- Treatment
- Virtual reality platforms used to improve upper limb function and gait (Assis et al., 2016; Janeh & et al., 2021)
Virtual reality can also be used to assess and treat physical abilities. For this presentation, we will mainly focus on upper limb function, but there are a few examples of how it can be used to assess and treat gait and individuals.
For assessment, there have been a lot of studies that have shown that virtual reality platforms can be used to assess upper limb function in individuals who have experienced neurological concerns. For example, the Gagnon et al. study had an individual complete a virtual peg test where they picked up a peg with a joystick and put it in an appropriate area. Researchers found that this could be an excellent way to assess upper limb strength, prehension, and coordination.
Virtual reality has been used with stroke patients to improve upper limb function. This was an interesting study because they had upper limb deficits post-stroke and used a virtual arm to do different activities. Researchers found that virtual reality improved upper limb function and range of motion even beyond their affected limb in individuals who experienced a stroke. In terms of gait, there have been many virtual walking programs on treadmill-like systems. This setup has been used to assess and treat gait and balance in individuals post-injury or illness.
Treatment At Home
- Virtual reality platform to use at home for rehabilitation (Lange et al., 2010)
A unique environment where virtual reality can be used is at home. Lange et al. looked at a home program for wheelchair users to practice upper limb exercises via a virtual environment. Researchers found that this was a low-cost and immersive way to improve upper limb strength and function in wheelchair users.
All of these examples showcase that virtual reality has been extensively researched with a lot of diagnoses and settings. Now, I will outline specific platforms available to use in a clinical setting.
Virtual Reality Programs
- Saebo-VR (“Saebo VR”, n.d.)
- Virtual ADL practice
- Real-time feedback
- Motek ("The Ultimate Gait-Lab Solution," n.d.)
- Interactive lab for gait analysis
There are many virtual platforms. I have listed a few that have been recently researched and some fully immersive and some non-immersive virtual reality platforms. The first one is a Saebo-VR that allows for virtual activities of daily living practice. It also provides real-time feedback to the individual on how they are doing. There is also the Motek which is treadmill technology that allows individuals to walk in place while a part of a virtual environment for gait analysis. Again, we will watch a video on this.
Often underutilized, clinical gait analysis is a very powerful tool for treatment, planning, and evaluation, but traditionally, it requires a large lab. And collecting and processing data from just a few steps is often a complex or time-consuming process that involves a lot of manual work. It is time to think about better solutions. Treadmill-based gait analysis takes up just 1/3 of the space. And because every step counts, more data can be recorded in a fraction of the time. Add synchronized virtual environments and self-paced algorithms, and you can ensure a natural walking pattern. Intuitive real-time software applications reduce the complexity of the data collection process, while offline software supports some media to analysis and reporting.
Conventional gait analysis can only analyze a single standardized condition, whereas adaptive treadmills can simulate challenging real-life situations such as up and downhill walking, dual tasking, and perturbations, allowing for functional analysis and effective training. But vast improvements can be seen even in overground analysis and training. Integrating a dynamic bodyweight support system enhances both and allows rehabilitation at an earlier stage. Advanced systems support a broad range of locomotor activities like sit-to-stand transfers, turning, and climbing stairs.
New, all-directional 3D technology leaves the natural gait pattern of patients with limited walking functionality unaffected. Challenging balance control training is also safe at all times. Aside from its clinical impact, both treadmill and overground solutions offer unique environments that can transform otherwise limited research into endless exploration opportunities through state-of-the-art technology, and you, creating your very own protocols, more conditions, more patients, more effective and relevant treatments, more research options. It makes you wonder if such solutions already exist. They do.
- NeuronUP ("About NeuronUP", n.d.)
- Non-immersive VR
- Computer-based
- ADL activities
Another virtual reality platform is a non-immersive virtual reality platform called NeuronUP. The NeuronUP is a computer-based rehabilitation program specifically designed for occupational therapists. They can pick activities for their clients that focus on improving cognitive abilities involved in activities of daily living. Figure 2 shows how NeuronUP looks when you sign in.
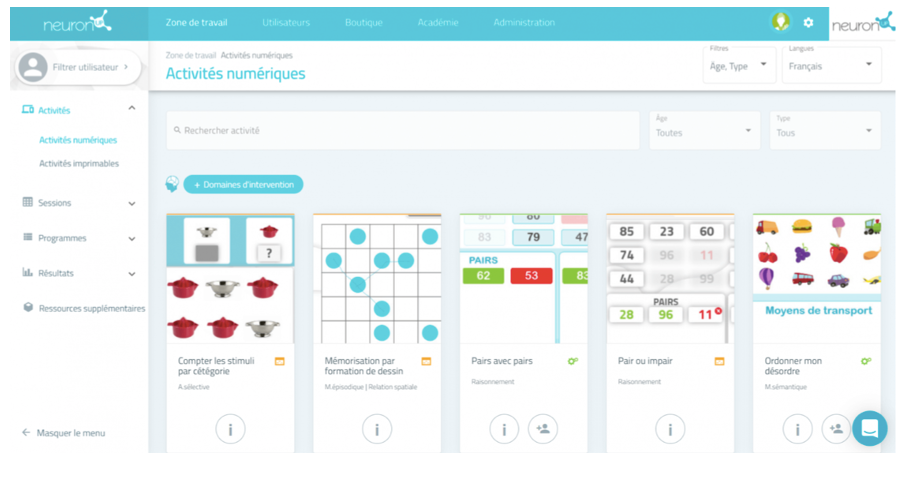
Figure 2. NeuronUP computer program.
Figure 2 shows a screenshot in Spanish, but it is also available in English. You can see a few math and categorization activities.
- Neuro Rehab VR ("About," n.d.)
- Semi-immersive VR
- XR Therapy System
- MIRA platform (Miclaus et al., 2020)
- Exergames
- The Breakfast Task (Craik & Bialystok, 2006)
- And many more!
Another virtual reality platform is Neuro Rehab VR, a semi-immersive virtual reality platform. The client uses a tablet, a handset, and a controller to access the unique program developed by the therapist. The Neuro Rehab VR has improved upper limb function in individuals.
The MIRA platform was recently used with stroke patients to improve upper limb function. The mirror platform combines cognitive and physical tasks into different games presented in a repetitive and motivating manner to improve tasks in daily life.
The Breakfast Task is a smaller-scale virtual reality platform developed for research. The breakfast task allows individuals to prepare different food items at the optimal time, not overcooked or undercooked. It is a button pressing virtual reality platform where they have to start or stop the cooking process. Researchers found that this was an excellent way to assess daily activities such as cooking and daily activities.
Virtual Reality Platforms Considerations
- Design (Baniasadi et al., 2020; Rizzo et al., 2004)
- User-centred (Carroll et al., 2002; Vimarlund et al., 2002)
- Immersion (Bun et al., 2017; Duan et al., 2011; Nunes et al., 2008; Rizzo et al., 2004)
Now that I have outlined specific virtual reality platforms, certain factors need to be considered when implementing virtual reality platforms in clinical practice. Design is essential. Virtual reality platforms should involve the end-user in the design process, including both the clinician and client. The design process should also involve IT experts. It is intuitive and straightforward to use.
As I mentioned, virtual reality should be user-centered, including the clinician and the client. Research has shown that therapists are less likely to implement virtual reality platforms into therapy if the user is not involved, and clients find it less useful when using the equipment.
Immersion is critical so matching it to a real environment is essential. The more realistic the virtual reality environment is, the more immersed the user is.
- Implementation (Garrett et al., 2018)
- Expert opinion (Rizzo et al., 2004; Schulteis et al., 2002)
- Safety (Botella et al., 2009; Nichols et al., 2002)
- Patient fit (Masseti et al., 2018)
The virtual reality platform should be easily implemented in hospitals, clinics, or homes. And, there should be tech support available from the company. If it is being implemented at home, clinicians should support the clients. Virtual reality therapy should only be prescribed by a healthcare professional involved in the individual's care.
Safety is vital as VR applications can be dangerous, especially with individuals who may have difficulty judgment or difficulty distinguishing the real environment from the virtual environment. Keep this in mind. Lastly, the patient fit is critical. The VR platform should be based on their needs, goals, and function.
Virtual Reality and Occupational Therapy
- Occupational Therapy Practice Framework: Domain and Process—Fourth Edition (OTPF-4)
(Boop et al., 2020)
When it comes to any assessment or treatment modality used in occupational therapy, it is crucial to ground the foundations of the specific treatment in an occupational therapy model. I have used the Occupational Therapy Practice Framework to explain why virtual reality can be implemented in occupational therapy assessment and treatment.
Domain
Within the domain are of the OTPF, there are occupations, client factors, performance skills, performance patterns, and context and environment (Figure 3).
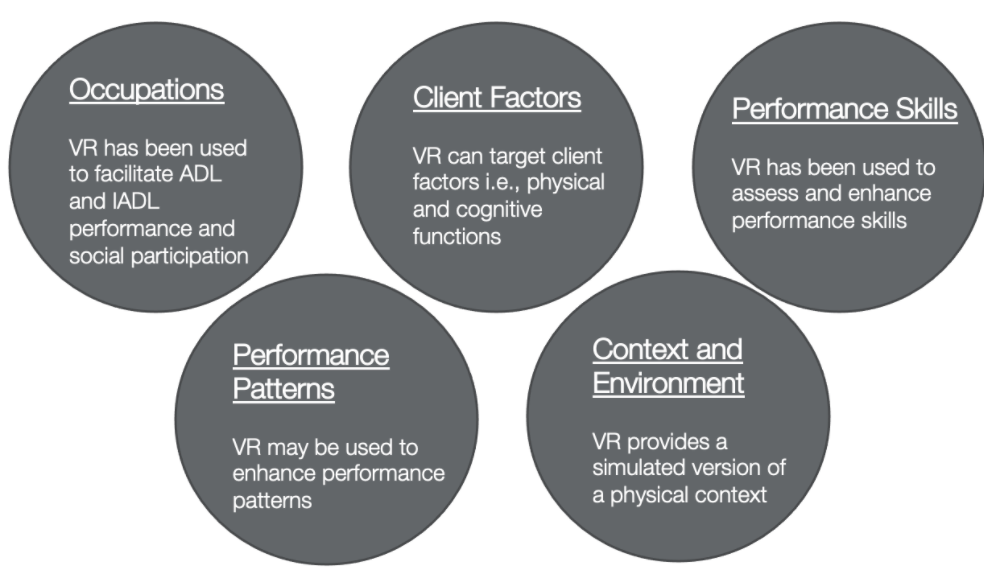
Figure 3. The domain of the OTPF used for VR (Boop et al., 2020)
Virtual reality can facilitate occupational engagement by improving activities of daily living function and social participation. Virtual reality can target specific client factors such as physical and cognitive functions. Within the client factors, it can target particular performance skills such as attention or upper limb function to improve occupational engagement.
Virtual reality can also be used to help an individual rejoin their performance patterns and routines. Additionally, it simulates real contexts and environments. Virtual reality can match the client's needs, goals, and therapy.
Process
- Client-centered assessment and implementation can facilitate occupational engagement.
(Boop et al., 2020)
In terms of process, implementing virtual reality in one's rehabilitation in a client-centered way can facilitate engagement in occupations. You can present clients with scenarios that may be difficult to achieve in a real-world setting or usual care rehabilitation. Virtual reality can be both implemented in assessment and treatment.
- Have you used virtual reality in your practice?
- How did you implement it?
- What did you like, what did you dislike?
- Patient feedback?
Now that I have reviewed the theory supporting the use of VR, I will now give some practical reasons why it can and should be implemented.
Why Use Virtual Reality in Occupational Therapy?
- Naturalistic
- Contextual
- Controlled environment
- Structure
(Davies et al., 1999; Massetti et al., 2018)
Virtual reality provides a naturalistic and contextual environment, which is highly engaging for the individual. It allows control over what details are included in an environment. So if you want to grade the activity to be more difficult, you can add more distractors or take away some distractors to make it easier. It allows structure, and the same activity can be presented to the individual over and over for repetition of tasks if they need more practice.
- Engaging for the user
- Engages sensory system
- Real-time feedback on performance
- Realistic simulated environment, the more immersed the user will be
- Adapted to each user
(Gerber, 2018; LaViola Jr, 2000)
Virtual reality is also engaging for the user. Fully immersive virtual reality platforms can engage all or almost all users' senses. Real-time feedback on performance is also provided with virtual reality. Lastly, it gives a realistic simulated environment that can be adapted to each user.
Virtual Reality in Neurorehabilitation
- Assess and treat individuals who have experienced a neurological disorder such as stroke, spinal cord injury, cerebral palsy, etc. (Massetti et al., 2018)
Virtual reality can be used to assess and treat neurological disorders such as brain injury, stroke, spinal cord injury, cerebral palsy, et cetera. The responsibilities of an occupational therapist include the evaluation and treatment of patients who, due to some functional limitation, find it challenging to complete their daily activities. Those with brain injuries may have cognitive issues with their attention, judgment, and decision-making, as well as physical limitations with their upper extremities, balance, or fine motor skills. Virtual reality can be used to assess and treat these specific performance skills.
Virtual Reality: Assessment
- Assess ADLs
- Assess cognitive functions involved in ADLs such as grocery shopping (Lee et al., 2003)
- Assess meal preparation (Christiansen et al., 1998)
There are specific areas where virtual reality has been used to assess and treat areas applicable to occupational therapy rehabilitation. For example, many studies have been used to evaluate activities of daily living in individuals who have experienced neurological concerns. The first looked at individuals who sustained a brain injury. The participants had to navigate a virtual supermarket environment. The environment was graded so that there were some open refrigerators to allow an individual to have easy access to the groceries and some closed refrigerators where they had to open the refrigerator to get the grocery item. Researchers found that this was an excellent way to assess cognitive functions involved in grocery shopping.
The research example was for meal preparation completed with individuals who sustained a brain injury. They were given a virtual kitchen environment where they prepared a simple meal like canned soup. The researchers graded this task by decreasing or adding cognitive load. For example, they added more choice in the environment to make the task a little more complicated, and they reduced choice to make it a little bit easier. In one instance, different irrelevant cans were added to a cupboard to make it harder for the individual to choose the correct soup can. Researchers found that this was an excellent way to assess meal preparation in individuals who sustained a brain injury.
- Preparing coffee (Davies et al., 1999)
- Task concentration
- Sound
- Controlling the world
- Abstraction
- Making mistakes
Preparing coffee is a standard ADL assessed by occupational therapists. This study had individuals with a neurological deficit prepare coffee in a virtual environment and looked specifically at these five factors.
Individuals who have sustained a brain injury often have difficulty concentrating or removing distractors in the environment. Adding realism like sound can improve function in a natural setting. It is also essential to control the virtual world. It should be simple, easy, simple, and intuitive to use, and there should not be any hidden key presses that cause any differences in the virtual world. Abstraction is the ability to make mistakes that should match the real environment. So, if the individual forgets coffee grounds, they should get hot water instead of coffee. They should be given away to go back and fix their mistakes to prepare a coffee appropriately.
- Assess general cognitive functions such as memory (Rizzo et al., 2002)
- Assess driving (Schiltheis et al., 2001)
Virtual reality has also been used to assess certain cognitive functions such as memory. This was a study completed with individuals who had neurological diagnoses. They were given a virtual office to scan and had to pinpoint any items in the office that did not belong, as research has found that this is an excellent way to assess short-term memory.
Virtual reality has also been used to assess other skills such as driving. This study was completed with individuals who had a brain injury. They were given a stressful driving situation like an emergency or traffic. Researchers found that the virtual reality platform was an excellent way to assess divided attention needed when an individual is driving.
Virtual reality is a great platform for people who are easily distracted. We can control the environment and look at various ADL and IADL tasks.
Virtual Reality: Treatment
- Grocery shopping (Adams et al., 2017)
- Safety in crossing streets (Naveh et al., 2000)
Virtual reality has also been shown to teach specific skills such as those for activities of daily living. In this study, individuals who sustained a stroke were given a continuum of activities of daily living tasks. It started with grocery shopping. Individuals used a virtual supermarket environment where they had to pick groceries. They then had to take these groceries into another in a virtual environment where they had to put them away. Finally, they used these groceries to prepare a simple meal. Researchers found that this was an excellent way to improve ADL function, especially in sequencing food preparation tasks and retrieving and placing items in a kitchen.
Safety and crossing streets are other activities completed in virtual reality. A study looked at safety in crossing streets with stroke patients who had unilateral spatial neglect. They were given usual care rehabilitation like scanning and paper/pencil activities, or a virtual environment where they had to scan the environment to see if it was safe to cross the street. Researchers found that the virtual environment increased scanning and safety for crossing streets in individuals with unilateral spatial neglect.
- Leisure activities
- Goalkeeping in soccer (Kizony et al., 2003)
Virtual reality can also be used to treat leisure activities. We often use virtual reality in our everyday lives, like playing video games or browsing homes on the internet. However, leisure is often overlooked in rehabilitation because there is more of a focus on improving self-care activities and productive occupations. This study was completed with an avid soccer player who sustained a stroke and had attentional deficits. Researchers developed a virtual environment where the individual was part of a soccer game and had to deflect balls from all different directions while also incorporating any distractions in the environment. This environment was very motivating to him. As a result, the individual improved his attention.
Benefits of Using Virtual Reality in Rehabilitation
- Improved balance and gait (Held et al., 2017; Verma et al., 2017)
- Improved range of motion (Assis et al., 2016)
- Improved cognition (Kim et al., 2011)
Here are some benefits associated with virtual reality in neurorehabilitation. It can improve balance and gait, and this is done through treadmill-based walking programs. An individual feels as if they are walking in this virtual environment. As I mentioned previously, if an individual who sustained a stroke is given virtual arm therapy, it can improve the range of motion of the impacted limb and enhance cognition.
- Reduction in depression (Assis et al., 2016; da Silva et al., 2015)
- Motivating (Luque-Moreno et al., 2015; Trombetta et al., 2017)
- Improve participation and autonomy (Gibbons et al., 2016)
It can also lead to a reduction in depression. A study was completed where individuals post-stroke used Nintendo Wii to improve their upper limb function. It improved their upper limb range of motion, strength, and mental health. It also motivated and improved participation as virtual reality platforms were exciting and enjoyable for the patient.
Virtual reality can reduce the boredom and fatigue associated with conventional rehabilitation and keep the individual in a happy mood.
- Possibilities to multitask (Bock et al., 2018)
- Individualized rehabilitation program targeted for different illnesses/diagnoses (Assis et al., 2016; Mousavi et al., 2016)
Virtual reality can provide multitasking. Multitasking is an essential skill in everyday life because we need it to perform many different activities such as driving. A study looked at individuals who sustained a stroke and had difficulty with multitasking. Researchers exposed them to two scenarios where they had to drive a car and pay attention to a street crossing and found that this program was an excellent way to assess and teach multitasking.
Virtual reality can individualize the rehabilitation program based on the person's diagnosis, goals, needs, and wants. It can be different for everyone.
- Telerehabilitation may cost less than in-person rehabilitation (Cikajlo et al., 2012; Dobkin et al., 2017; Maples-Keller et al., 2017)
- Combining VR and usual therapy presented better outcomes (Aminov et al., 2018; Saposnik et al., 2016)
- The possibilities where rehabilitation can go with VR are endless!
Virtual reality may cost less than conventional therapy, especially in telerehabilitation. You can expose individuals to scenarios that may be impossible to achieve in usual care rehabilitation. One example is using virtual reality to work with someone who fears heights or using an airplane.
Virtual reality has been shown via a meta-analysis to have better therapeutic outcomes if combined with usual care rehabilitation. The possibilities of where virtual reality can go are endless, and there are many different platforms out there. Technology is still advancing and becoming more available. It is an area where we might see it utilized more in everyday practice in the future.
Barriers of Using Virtual Reality in Rehabilitation
- Implementation
- Access (Peral-Gomez et al., 2020)
- Safety (Baniasadi et al., 2020; Brassel et al., 2021)
- Large economic investment (Peral-Gomez et al., 2020)
- Motion sickness (Bohil et al., 2011; Garrett et al., 2018; Rizzo et al., 2004)
- Addictive (Baniasadi et al., 2020)
- Research and policy-making needed (Morone et al., 2014)
Access is one barrier. A research study asked occupational therapists why they do not use virtual reality platforms in their practice, and they stated that they do not have access to this type of technology. Safety is also essential. As I mentioned before, virtual reality can be problematic for cognitive issues. It is also a significant economic investment. Saebo VR, Motek, et cetera are costly. Virtual reality systems can cause motion sickness, and those with perceptual concerns can feel sick during and after using them. Motion sickness may be more pronounced if they are on certain medications.
It can also be addictive. While no research proves that virtual reality is addictive in a healthcare setting, it is addictive in a leisure setting. Keep this in mind when prescribing virtual reality platforms to clients.
There is not enough research and policies that are in place to protect clients when using virtual reality platforms. Additionally, the study lacks the treatment end of things, and there needs to be more qualitative and quantitative research.
- Patient and therapist factors
- Age (Casserly et al., 2014; Laver et al., 2014; Nichols et al., 2002; Rizzo et al., 2004; Standen et al., 2015)
- Training (Threaptleton et al., 2016; Wingham et al., 2015)
Some participant factors include age. Many younger individuals are assumed to know about virtual reality platforms when they may not have experienced using them in their everyday lives. Older participants may be less likely to like virtual reality therapy because they do not have experience using it. Much of the research has been done with a population between the ages of 40 to 50, although many neurological concerns happen later in life. It is essential to realize this when going through the literature.
Training is also essential. The clinician needs to use a virtual reality platform appropriately to train the client in turn. Research has shown that if the therapist is not adequately trained, they are less likely to implement it and are less satisfied with using the equipment.
Overall Considerations
- Clinical training (Glegg et al., 2018; Proffitt et al., 2019; Wingham et al., 2015)
- Therapist and team involvement (Glegg et al., 2018)
- Research (Glegg et al., 2018)
Here are some overall considerations of using virtual reality platforms in neurorehabilitation as clinical training. As I mentioned, managers should be aware that clinical training should be available for all conditions and the whole team's involvement.
Therapists should not exclusively use this technology with the client. The team should be involved in implementing virtual reality care as part of a multidisciplinary approach. There need to be more randomized control trials to see if it is effective in neurorehabilitation, specifically in an occupational therapy setting. More qualitative research is required to see if therapists and clients like it.
- Feasibility of implementation
- Safety and Responsibility (Baniasadi et al., 2020; Brassel et al., 2021)
- Patient factors
- "It's far more important to know what person the disease has than what disease the person has"-Hippocrates
It should be feasible as far as costs and resources to implement. Safety and responsibility are essential as there may be risks, as mentioned earlier. It would help if you outlined this to the client so they are making an informed decision about whether they want to use it.
Patient factors are important. I like this quote by Hippocrates. Every person is different despite similar diagnoses. If a virtual reality platform works with one individual who experienced a stroke, it may not work with another. Catering the treatment to the individual is more important than implementing virtual reality.
Summary
- Use of VR fits into the OTPF-4
- Individualized treatment
- Adaptable treatment
- Engaging and motivating environment
- More research needed
Julia: The literature suggests that virtual reality can be one of the tools that we as OTs use in our practice for both assessment and intervention across lots of different populations, pediatrics, adults, neurological injury, mental health, et cetera. And it fits in with our OT Practice Framework that we use. And like any tool, as Jasleen was just mentioning, virtual reality can be used for some people very well, but for others, it might need to be customized or perhaps not even used at all. For instance, people may have vertigo or experience dizziness and not use virtual reality like Oculus. Thus, it is crucial to individualize treatment. Virtual reality is great for this as you can change and customize the platform depending on the person's challenges. They may have a successful shopping experience virtually, whereas, in a typical shop, they may not do well due to unexpected things that might come up. Virtual reality is also engaging and motivating. For those who have used VR in your personal life, you may be able to identify with this. Finally, there more research is needed.
Next Steps
- Future research
- Randomized controlled trials to assess if VR use during neurorehabilitation can improve ADL function
- How do patients feel about using VR?
- How do OTs feel about more implementation of VR?
- Qualitative research to understand the experience of engaging in virtual reality in different populations
It would be helpful to have some clear evidence for virtual reality use with people with brain injury for future research. It would be essential to use this platform for assessment and ADL practice as this is the core bread and butter. We also want to know the perception of patients using this treatment from children to older people. And, how do OTs feel about it? When I was doing clinical practice, I did not want to use technology. However, seeing the benefit of virtual reality changed how I was looked at it.
We will start trying to answer some of these questions in our practice, including Saebo VR and the Motek treadmill. We just submitted a grant to get the Motek VR system. We want to investigate what populations this might be appropriate for, its effectiveness, and the perception of the treatment.
Questions and Answers
Can a person's performance in VR translate to real life? Has the research shown that yet?
The idea of VR is to help clients practice specific areas. We do not necessarily need people to get better at VR, but we want people to get better in real life. Virtual reality can be a tool to practice some aspects of it. There needs to be more research in this area in terms of literature on how their skills translate. Virtual reality is still relatively new, and research needs to see if these skills can be translated from a virtual environment to a real environment.
There are some unexpected stimuli in a real-world situation, while VR, traditionally, is more controlled. What are your thoughts on this?
Different types of virtual reality platforms are out there. Some of these platforms allow tasks to be graded, like adding more distractors in the environment, but of course, it is hard to simulate it entirely in a virtual reality platform.
What are the precautions or contraindications of virtual reality?
Virtual reality may not be appropriate for those with significant perceptual or balance problems. It is always essential to keep the client's safety in mind before implementing novel treatment. We should be clear about what is going to be taking place.
Some VRs have a glove system for fine motor coordination and grasp and release, but other platforms just have shoulder and elbow movement.
It is essential to the aim of the assessment or intervention. Some VR tasks do not look at the complete task or the entire movement of the person but just a portion. Again, we need to use critical reasoning to know the areas we can assess and treat with this modality.
Virtual reality almost seems like a preparatory activity like mental practice where you think through what you will do before you do it.
Imagery is a huge part of therapy and sports. This is the same thing with virtual reality. You are not necessarily doing an activity in real life but using the same neural pathways.
Citation
Grewal, J., & Schmidt, J. (2022). Virtual reality in brain injury rehabilitation OccupationalTherapy.com, Article 5490. Available at www.occupationaltherapy.com

