What We Will Be Covering
- What is a “prop sitter”?
- Clinical Guidelines
- Case Study
Today, we are going to be talking about wheelchair seating and considerations for the prop sitter (Figure 1).

Figure 1. Example of a prop sitter.
First, what is a prop sitter? How does that relate to other types of wheelchair sitters? What are some clinical guidelines when working with this person and determining the most appropriate wheelchair seating? Finally, we will wrap up with a case study to put a face on this category of wheelchair sitter and the solutions we used.
SMS Series
- This is part of a series of webinars designed to prepare the participant for the Seating and Mobility Specialist examination
- And… develop more advanced seating and wheeled mobility skills
This is part of a series of webinars that are primarily designed to help someone who already works in this specialty area of wheelchair seating and mobility to prepare for an examination called the Seating Mobility Specialist exam. This is a certification that is available through RESNA. If this is something that you are interested in pursuing, you should check out this series of webinars. In fact, the first webinar addresses the SMS examination and certification process, what the prerequisites are, et cetera. I hope that this series of webinars will help you to prepare for that and successfully pass and receive this designation. But whether or not you are looking at getting the SMS certification, I hope that this series of webinars will help you develop more advanced seating and wheeled mobility skills so that you can better address the needs of the clients with whom you work.
Seating and Wheeled Mobility
- Every mobility base includes some form of seating
- Primary supports include a seat, back, armrests, and footrests
- Seating interventions vary tremendously depending on the client's age, diagnosis, prognosis, postural needs, pressure risks, etc.
Every mobility base, whether it is an adaptive stroller, a manual chair, or a power chair includes some form of seating, and this is primarily where the client bears weight. These are called the primary support surfaces and include the seat, the back, the armrest, and the footrest and footplates. From there, the specific seating interventions are going to vary quite a bit and depend on the individual client, their age, their diagnosis, prognosis, postural needs, their risk of pressure injury, et cetera.
Postural Needs
- One way of looking at wheelchair seating is by postural support needs:
- Hands-free sitter
- Hands-dependent sitter
- Prop sitter
One way of looking at wheelchair seating is by categorizing the clients that we are working with by the amount of postural support that they require. These categories are referred to as the hands-free sitter, the hands-dependent sitter, and the prop sitter. There are courses available to you on the hands-free sitter and the hands-dependent sitter, and along that continuum, we now address the prop sitter. Let's talk about what each of these terms may mean.
The Hands-free Sitter
- The person is able to lift their hands off of the surface without changing the position of the trunk
- Can also shift weight to the side and return to a midline position
- Good trunk control
As a quick review, a hands-free sitter is a person who is able to lift their hands off of the seating surface without changing the position of their trunk. They are not going to fall over or collapse in their trunk, and they are able to maintain that position. This person can shift their weight to the side a little bit and return to the midline. This person has good trunk control.
The Hands-dependent Sitter
- This person uses one or both hands on a surface to maintain sitting balance
- If hands are lifted, the trunk will collapse
The hands-dependent sitter needs to use one or both hands on the surface to maintain their sitting balance. Otherwise, if they lift a hand or both hands, either the client will fall over or the trunk will collapse into a posterior flexed kyphotic posture or might collapse to the side.
The Prop Sitter
- This person cannot maintain sitting, even with the support of both arms
- External support is required
The prop sitter, who we are talking about today, cannot maintain sitting even with the support of both their arms, as shown in Figure 2. And, some clients cannot get their arms down towards the seating surface. However, even if they could, they need a lot more postural support.

Figure 2. Another example of a prop sitter.
For these types of cases, we need to bring in external support.
The Prop Sitter
Goals
- Provide adequate proximal support for improved function
- Optimize function
- The function may be more basic, such as improved breathing and swallowing, rather than increased participation in MRADLs (mobility-related ADLs)
- Prevent the development of or accommodate asymmetrical postures
- Mitigate pressure issues
What are our goals when we are working with this prop sitter, or someone who needs more significant postural support? We want to provide adequate support proximally, close to the body, to help this person to be as functional as possible. Now, for the prop sitter, this function may be more basic. This person may have enough physical involvement that even with adequate wheelchair seating, this client may not be able to participate in their MRADL. That is a nice Medicare term for mobility-related ADLs. So, when I am working with someone who is in this category, even if I recommend an optimal seating system for them, it does not mean that they now can cook dinner for the family. However, there still can be a functional change. The client may now be able to use their assistive technology, like a communication device or their power wheelchair. It can also be even more basic than that. With the appropriate positioning devices, they may have improved breathing and swallowing. These are very key medical changes that need to be on our radar and certainly can justify the recommendations we are making.
We also want to prevent the development of or accommodate already existing asymmetrical postures. If this person has a tendency towards lateral scoliosis of the spine, we want to provide adequate support of the trunk to minimize the risk of that development. Or, if there is already an asymmetry of the spine, we want to appropriately accommodate that. We want to mitigate any pressure risk for this client as well.
Many prop sitters tend to fall into one of two subcategories; clients that have little or no postural asymmetries or clients that have significant non-reducible asymmetries. Let's start with the first. Some clients need a lot of support from their seating system but do not yet have postural asymmetries. If they fall into an asymmetric position, we can correct it. Everything is reducible or flexible. These clients often have low tone in their trunk. This may be a new diagnosis, an acquired injury, or a younger child, where we are not having to deal with accommodation yet. In these cases, we are looking at providing adequate postural support and prevention. Then, there are the clients who have significant non-reducible asymmetries, as this young man from the earlier picture as shown lying on the mat table (Figure 3).

Figure 3. Example of a fixed deformity.
In this case, one of our goals is to try to help this person keep their head in an upright and aligned position as much as possible, even if this requires a lot of support. This becomes a priority even if the pelvis and trunk are asymmetrical. If we can provide enough support so that this client is aligned at the pelvis and trunk, that is wonderful. However, if the end result of that is a very symmetrical head, then we are going to impact this person's vision, breathing, and swallowing, or basic medical needs. Our priorities change a bit when we are working with this population.
Typical Diagnoses and Presentation
- Little or no postural asymmetry
- Often very low tone in trunk
- A new diagnosis or acquired injury
- Significant, non-reducible asymmetries
- Supporting head in midline even if pelvis and trunk are asymmetrical
- Orthopedic and Neurological impairments
- Asymmetrical alignment of pelvis and spine
- i.e. Muscular dystrophy, cerebral palsy
- Neurological impairments
- Little or no trunk control
- i.e. SCI, ALS
- Other diagnoses, dependent on postural support needs
- MS, DVA, TBI, DD
- Typically, multiple issues including mobility, sensation, and alignment
- Progressive conditions may start as hands-free or hands-dependent
There are many diagnoses and presentations that might need this level of support. These diagnoses include multiple sclerosis, traumatic brain injury, developmental disabilities, et cetera. For the prop sitter, there can be multiple issues including decreased mobility, sensation, and alignment (Figure 4).

Figure 4. A client with multiple issues.
We need to keep all those in mind in our interventions. If someone has a progressive condition, they may start off as a hands-free or hands-dependent sitter, and over time as the person's condition progresses, they may become a prop sitter and require more support.
Assessment Considerations
- Fixed or non-reducible
- Cannot be corrected or even moved without surgery, but can worsen
- Flexible or reducible
- Can be reduced, but not necessarily to neutral
- Even if reducible to neutral, still important to check if more flexible in one direction
Other assessment considerations are whether or not we see concerns in the body that are fixed or non-reducible versus flexible or reducible.
Flexible
Let's say you are working with a client who has lateral scoliosis in their spine. Their spine is shortened on one side as compared to the other. But, if you lay that person down on the mat table on their back, you can move them into alignment. That means that their spinal deformity is flexible or reducible. Reducible is the preferred term. Even if their spine is reducible to neutral, it is still important to check beyond neutral because sometimes what we will see, especially in children or someone with a new diagnosis, is there may be more flexibility on one side versus the other. This is where a potential curvature can develop, and you need to keep that in mind with your recommendations. If you can reduce part of the asymmetry, it is still considered reducible, but I may note in my documentation that it is only partially reducible.
Fixed
Finally, we have fixed or non-reducible. In this case, I cannot correct the curvature or asymmetry in the pelvis. Let's take the example of lateral scoliosis again. Perhaps, I really cannot budge it or even remotely approach neutral, then I would say that it is non-reducible. The reason "non-reducible" is the preferred term over fixed is that even though it cannot be corrected or moved without surgery, it can worsen. I learned this the hard way. I saw a client a number of years ago and recommended a molded back due to non-reducible asymmetries. A number of years later, we needed to remold the back, because unfortunately, the curvature had worsened. The funding source said, "Hey, wait a minute, you said it was fixed." I needed to explain to them that even though I meant fixed as I could not make it better, I did not mean it could not get worse. Unfortunately, it could. So, it is very important to be clear in our documentation.
Mat Examination
- An important measurement in supine is hip flexion which determines seat to back angle
- This is addressed in more detail in the Mat Assessment course
When we take the prop sitter and examine them on the mat, it is important to determine their available hip flexion to recommend the appropriate seat to back angle. This is something that we discuss in more detail in the mat assessment course in the library. This young man (Figure 5), Wyatt, is featured in a couple of videos within that course.
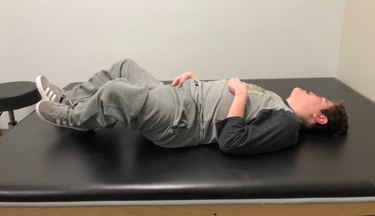
Figure 5. Wyatt.
Here are some considerations when we are assessing the prop sitter, things we need to keep in mind.
Pelvis
- Posterior pelvic tilt leads to
- Trunk flexion
- Forward head position
- Hip internal rotation and adduction, or
- Hip external rotation and abduction
Let's start with the pelvis as this is always where we should focus. The position of the pelvis is going to have a significant impact on the position of the trunk, as well as the lower extremities. Many of our prop sitters show quite a bit of posterior pelvic tilt, as Brett is showing in this picture (Figure 6).

Figure 6. Example of a posterior pelvic tilt.
His pelvis is rocking rearward with a very flexed spine. He is also showing extreme trunk flexion and a forward head position. Along with this collapsed position of the pelvis, we often see hip internal rotation and adduction. While in some clients, we might see the exact opposite. There can be external rotation and abduction along with a posterior tilt.
- Anterior pelvic tilt leads to
- Trunk extension, exaggerated lumbar curve, scapular retraction
- Neck extension
- Hip internal rotation and adduction
We want to address this within the seating system. Some clients may have an anterior pelvic tilt. This is Anderson, and his pelvis tends to tilt forward anteriorly, leading to trunk extension and a more exaggerated lumbar curve (Figure 7).

Figure 7. Example of anterior pelvic tilt.
There can also be an exaggerated lordosis with the shoulders pulled backward into scapular retraction, often in an attempt by the client to remain upright. The neck in conjunction with this scapular retraction may also be in extension. The hips are very frequently internally rotated and abducted in these clients as well.
- Obliquity
- One side of the pelvis is lower
- Named for low side (Left obliquity = left low)
- The opposite side of trunk collapses
Pelvic obliquity is where one side of the pelvis is higher than the other side, and it is typically named for the low side. Thus, a left obliquity means that the low side is on the left side. Now, this is not always consistently used by people, and so in my documentation, I always try to label it more specifically. In the case of this young man, the left side of his pelvis is high. Instead of saying a right obliquity even though that is correct, I might say, "This client has an obliquity that is low on the right side." I want to make sure that everyone is clear. The opposite side of the trunk is going to tend to collapse when we have an obliquity.
- Rotation
- One side of the pelvis is forward
- Named for facing side (Left rotation = right side of the pelvis forward, entire pelvis facing left)
- Legs windswept to facing side
- One leg abducted and externally rotated
- One leg adducted and internally rotated
- At risk of subluxation
We can also see the rotation of the pelvis, where one side of the pelvis is forward of the other. This is usually named for the facing side.
